Abstract
Background
Trauma poses a significant global health challenge. Despite advancements in the management of severely injured patients, (poly)trauma continues to be a primary contributor to morbidity and mortality worldwide. In the context of trauma resuscitation, supplemental oxygen is commonly administered generously as suggested by guidelines. Yet, it remains uncertain whether the trauma population might derive advantages from a more conservative approach to supplemental oxygen.
Methods
In this retrospective cohort study from two Swiss trauma centers, severely injured adult (> 16 years) trauma patients with an Injury Severity Score (ISS) ≥ 16 were divided into four groups according to the first blood gas analysis taken: hypoxaemia (PaO2 < 10.7 kPa/80 mmHg), normoxaemia (PaO2 10.7–16.0 kPa/80–120 mmHg), which served as reference, moderate hyperoxaemia (PaO2 > 16.0–40 kPa/120–300 mmHg) and severe hyperoxaemia (PaO2 > 40 kPa/300 mmHg). The primary outcome was 28-day mortality. Length of hospital stay (LOS) and length of intensive care unit stay (LOS-ICU) were analyzed as secondary outcomes.
Results
Of 1,189 trauma patients, 41.3% had hyperoxaemia (18.8% with severe hyperoxaemia) and 19.3% had hypoxaemia. No difference was found for 28-day mortality (hypoxaemia: 15.7%, normoxaemia: 14.1%, hyperoxaemia: 13.8%, severe hyperoxaemia: 16.0%, p = 0.846). Patients with severe hyperoxaemia had a significant prolonged LOS (median 12.5 [IQR 7–18.5] days vs. 10 [7–17], p = 0.040) and extended LOS-ICU (3.8 [1.8–9] vs. 2 [1–5] days, p = 0.149) compared to normoxaemic patients. In multivariable analysis, oxygen group was not associated with the primary outcome 28-day mortality or LOS-ICU. Severe hyperoxaemia patients had a tendency towards longer hospital stay (adjusted coefficient 2.23 days [95% CI: − 0.32; 4.79], p = 0.087).
Conclusion
Hyperoxaemia was not associated with an increased 28-day mortality when compared to normoxaemia. However, both moderate and severe hyperoxaemia is frequently observed in trauma patients, and the presence of severe hyperoxaemia showed a tendency with extended hospital stay compared to normoxaemia patients. Robust randomized controlled trials are imperative to thoroughly evaluate the potential correlation between hyperoxaemia and outcomes in trauma patients .
Trial Registration Retrospectively registered.
Similar content being viewed by others
Background
Trauma represents a major global health issue and has been identified as a key concern for health care by the World Health Organization (WHO) [1]. Despite advances in care of severely injured patients, (poly-)trauma remains a leading cause of morbidity and mortality worldwide [2,3,4].
In trauma resuscitation, supplemental oxygen is often administered to treat and prevent hypoxaemia as recommended by the Advanced Trauma Life Support (ATLS) and the Pre-hospital Trauma Life Support (PHTLS) manual [5, 6]. Oxygen is cheap and widely available in the prehospital as well as in the clinical setting. In general, it is believed that oxygen therapy – at least if administered over a short period of time – is of little harm. This leads to a liberal use of supplemental oxygen in trauma patients and results in hyperoxaemia as a common finding in trauma patients [7]. Moreover, it is frequently administered in the prehospital setting even without an indication [8].
A recent systematic review found extremely sparse evidence for or against the use of supplemental oxygen in the trauma population [9]. Knowledge on the use of supplemental oxygen mainly originates from other critical patient populations and not specifically from trauma patients. However, emerging evidence indicates that even modest hyperoxaemia in general might be harmful. In a systematic review and meta-analysis, Chu et al. compared a liberal versus a restrictive oxygen strategy for a broad mix of acutely ill medical and surgical patients and found an association between liberal oxygen administration and increased mortality [10]. In addition to mortality, hyperoxaemia has been associated with major pulmonary complications in the intensive care unit (ICU) as well as in surgical patients [11, 12]. In contrast, a recent study that randomized ICU patients to either low or high oxygenation levels revealed no discernible difference in mortality rates [13].
For trauma patients, a study on 68 traumatic brain injury patients showed that the degree of disability was significantly reduced at six months in the group receiving liberal compared to restrictive oxygen [14]. In contrast, Douin et al. found an association between higher fraction of inspired oxygen (FiO2) administration during periods of hyperoxaemia (saturation 100%) and greater risk of mortality among critically injured patients [15]. It remains uncertain whether the trauma population could benefit from a more restrictive supplemental oxygen approach than recommended by current international guidelines.
In our retrospective cohort study, we aimed to assess mid-term mortality (28-day) of stratified oxygen groups of hypoxaemic, normoxaemic, hyperoxaemic, and severe hyperoxaemic trauma patients. We hypothesized that in the trauma population, hypo- and hyperoxaemia are common and associated with increased mortality compared to normoxaemia.
Methods
This retrospective cohort study was performed in two level one trauma centers in Switzerland; Inselspital, University Hospital of Bern and Hospital of Canton St. Gallen (KSSG). The study protocol was approved by the local cantonal ethics committee of the Canton of St. Gallen (approval EKOS 23/178, project number 2023-01801). This report follows the applicable STROBE guidelines [16].
Anonymized patient data from the electronic health records in both hospitals were screened for all patients that presented to Inselspital Bern or KSSG for acute trauma care between 01.01.2017 and 31.12.2022. Screening included coding of free text data through standard trauma scoring systems such as Injury Severity Index (ISS) [17, 18] and abbreviated injury scale (AIS) [19]. Inclusion criteria were primary admission with trauma and ISS ≥ 16, age ≥ 16 years old, and arterial blood gas analysis (aBGA) performed within 3 h after admission. Exclusion criteria was missing PaO2 (arterial partial pressure of oxygen) value in the initial aBGA and missing information on prehospital airway status (intubated or not). Severe trauma to a specific body region was defined as having a maximum AIS of three or higher for that region.. Demographic data, pre-hospital and clinical data as well as details on injury were collected.
Based on the first available result of PaO2 within the first 3 h after admission, patients were divided into four groups [20]:
-
Group 1 hypoxaemia: all patients with PaO2 < 10.7 kPa (80 mmHg)
-
Group 2 normoxaemia: all patients with PaO2 between 10.7 and 16.0 kPa (80–120 mmHg)
-
Group 3 mild hyperoxaemia all patients with PaO2 above 16.0 to 40 kPa (120–300 mmHg)
-
Group 4 severe hyperoxaemia: all patients with PaO2 above 40 kPa (300 mmHg)
Normoxaemic patients (group 2) served as reference group. Demographic data, pre-hospital and clinical data and injury scores were calculated and compared for all four groups.
Statistics
As primary outcome, 28-day mortality was assessed and compared across groups, with group 2 (normoxaemia) as reference. For secondary outcomes, length of ICU stay (LOS-ICU) and length of hospital stay (LOS) were calculated and compared between groups. A predefined set of complications (stroke, myocardial infarction, pulmonary embolism, deep vein thrombosis, pressure ulcer, renal insufficiency, abdominal distension, wound infection, pneumonia, urinary tract infection, sepsis, compartment syndrome (extremity), abdominal compartment syndrome, acute lung injury (ALI) / acute respiratory distress syndrome (ARDS), cardiac arrest, multiorgan failure) were reported.
Data were analyzed with STATA 18.1 (StataCorp, College Station, TX, USA). For primary and secondary endpoints, odds ratios (OR) were calculated in addition to 95% confidence intervals for all point estimates. Depending on normality testing (Shapiro Wilk) median (interquartile range (IQR)) respectively mean (standard deviation (SD)) are shown for continuous variables, p-values obtained by Kruskal–Wallis test (for more than two groups) or Wilcoxon rank sum test (for two groups). Categorical variables are shown with number (%) in each category, p-values obtained by Chi-squared test. No p-value adjustment was performed.
Baseline data was used to derive a multivariable logistic (linear) regression model for the association between the four oxygen groups and the primary (secondary) endpoint as follows:
If binary variables were based on present continuous variables (such as hypotension on systolic blood pressure), the continuous parameter was used only to derive to the final model to avoid collinearity. Furthermore, oxygen saturation and GCS were not included in the multivariable model based on collinearity testing with oxygen group respectively AIS head (Variance Inflation Factor of > 2.5). Missing values were imputed and a stepwise backward regression analysis with a p-value of 0.05 was used to get to the final model. Oxygen group was forced in the final model. Logistic regression associations were presented as adjusted OR (aOR), linear regression associations with the coefficient accompanied with a 95% confidence interval (CI). Last, to explore non-linear associations of PaO2 and 28-day mortality, a fractional polynomial regression was used in one dimension with different powers (− 2, − 1, − 0.5, 0 = ln, 0.5 1, 2, 3) adjusted for the same co-variables as the final model. The proposed model was visualized with an adjusted predicted probability plot.
With a total of an expected 1200 trauma patients (around 200 patients per year), with 300 patients in each of the four oxygen groups, we would have been able to detect a clinical meaningful difference of 7% in 28-day mortality between normoxaemia (14%) and severe hyperoxaemia (21%).
Results
Study population
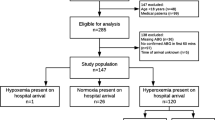
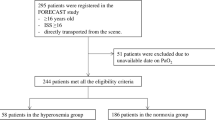
From January 2017 to December 2022, a total of 1,189 adult patients with an ISS of 16 or higher, who were primarily admitted to the two emergency departments, were included in the primary analysis (Fig. 1).
The baseline characteristics according to the oxygen group are shown in Table 1. The median age was 57 [IQR 40–73] years and 27.8% were female in this cohort. Patients in the severe hyperoxaemia group were significantly younger (51.5 [30.5; 68.5] years), and more frequently female (37.0%), overall p-value = 0.001. They presented with a higher median AIS head score (3, [0–5], p = 0.019) and lower GCS (5.5, [3–14], overall p ≤ 0.01). Baseline data for blood pressure and respiratory rate showed statistically significant, clinically negligible differences between the groups. More patients in both the hyperoxaemia (30.8%) and the severe hyperoxaemia (50.0%) group were intubated prehospital compared to normoaemic (20.8%) and hypoxaemic (17.9%) patients. Severe thoracic trauma (AIS thorax > 2) was more prevalent in the normoxaemia and hypoxaemia group (52.8% and 59.4%, respectively) compared to the moderate and severe hyperoxaemia groups (46.4% and 40.0%, supplemental Table 1). The total population is shown in supplement Table 2.
Outcomes and complications
No significant difference was shown for 28-day mortality between the four groups with different oxygen partial pressure (p = 0.846, see Table 2).
Patients exhibiting severe hyperoxaemia experienced a significantly prolonged LOS with a median of 12.5 days (IQR 7–18.5) compared to normoxaemic patients, who had a median LOS of 10 days (7–17, p = 0.040). There was also a significant difference observed in LOS-ICU between the two groups, with 3.8 days (1.8–9) for patients with severe hyperoxaemia versus 2 days [1,2,3,4,5] for normoxaemic patients, yielding a p-value of < 0.001.
In total, 435 (36.6%) experienced complications during their hospitalization. Among all complications, pneumonia was the most common with 10.4%, followed by pulmonary embolism (2.5%) and renal insufficiency (2.4%) (Table 2). Overall, no significant differences were observed when comparing the four groups (Table 2).
In multivariable analysis, oxygen group was not associated with the primary outcome of 28-day mortality (Table 3) or LOS-ICU (supplemental Table 3). Severe hyperoxaemia patients had a statistical tendency towards a longer hospital stay (adjusted beta coefficient 2.23 [95% CI: − 0.32; 4.79], p = 0.087).
Non-linear association for PaO2 and 28-day mortality
The inverse of PaO2 (1/PaO2) was the best predictor of 28-day mortality, based on varying PaO2 levels adjusted on age, ISS, AIS head, systolic blood pressure and prehospital intubation (p = 0.060, Fig. 2).
Visualization of the fractional polynomial regression with inverse-transformed PaO2 (= 1/PaO2); p-value = 0.060. Figure Description: The figure illustrates the relationship between arterial oxygen partial pressure (PaO₂) and adjusted predicted 28-day mortality. The shaded blue area represents the 95% confidence interval for the predicted mortality. At PaO₂ levels below 10 kPa, predicted 28-day mortality is high, indicating a greater risk of death. As PaO₂ increases, predicted mortality decreases rapidly, showing that even small improvements in oxygen levels can significantly reduce mortality risk. Beyond 20–30 kPa, further increases in PaO₂ result in only marginal decreases in mortality, suggesting diminishing returns at higher oxygen levels. Abbreviations aBGA, Arterial Blood Gas Analysis. *adjusted on age, ISS, AIS head, systolic blood pressure (with imputed values), and prehospital intubation
Discussion
In this retrospective multicentre cohort study of 1,189 severely injured patients in Switzerland, both hypoxaemia and hyperoxaemia were frequently observed upon hospital admission. Hyperoxaemia was not associated with an increased 28-day mortality when compared to normoxaemia. However, the presence of severe hyperoxaemia showed a tendency with an extended hospital stay compared to normoxaemia patients.
While the detrimental effects of hypoxaemia are well recognized, the potential risks of hyperoxaemia have received less attention in previous research. Although prior studies have reported hyperoxaemia as a common occurrence in trauma patients [7], a finding in line with our data, its impact on patient outcomes remains insufficiently investigated.
This study revealed that patients with severe hyperoxaemia had prolonged stays both in hospital and in the ICU compared to normoxaemic patients. After adjusting for confounding variables such as the observable differences in baseline characteristics, the difference in LOS disappeared. However, we still observed a trend towards a longer hospital stay in severe hyperoxaemia patients. These findings are consistent with previous studies [15, 21]. For instance, Baekgaard et al. reported an increased mortality for patients with a FiO2 > 60% for more than 2 h within the first 24 h [21], while Douin et al. demonstrated an association between higher administered oxygen fractions during hyperoxaemia and mortality [15]. These results are particularly noteworthy considering that only short periods of hyperoxaemia within the first few hours after trauma may negatively affect outcomes [21]. However, all these studies, including ours, were retrospective analyses.
In contrast, a small randomized controlled trial involving 68 traumatic brain injury patients showed an improved neurological outcome when higher oxygen therapy was administered for the first 6 h after admission [14].
One limitation of this retrospective study is the uneven size of the groups and differences in baseline characteristics (age, gender, head trauma). Further, a notably higher number of hyperoxemic patients, including those with severe hyperoxemia, were intubated prehospital compared to normoxemic patients. It is known that intubated patients typically experience extended stays in the ICU and overall hospitalization duration. However, our study couldn’t discern whether the prolonged ICU and hospital stays resulted from prehospital intubation or were directly linked to hyperoxemia itself. Only patients with an aBGA were included which might have created a potential selection bias as patients without aBGA were notably less severe injured and had lower mortality and shorter hospital and ICU stay (Supplement Fig. 4).
A strength of this retrospective study is the multicentre design encompassing a large general trauma population in Switzerland with a complete dataset for primary outcome data.
This study, along with the diverging current literature highlights the urgent need for a large randomized controlled trial adequately powered to investigate the optimal oxygen administration and address confounders like prehospital intubation in trauma patients. The forthcoming results from the TRAUMOX2 (NCT05146700) and SAVE-O2 (NCT04534959) studies may provide valuable insights into this matter.
Conclusion
This study indicate that hyperoxaemia is not associated with increased 28-day mortality compared to normoxaemia. Nonetheless, both moderate and severe hyperoxaemia are frequently detected in trauma patients, with severe hyperoxaemia exhibiting a tendency towards prolonged hospital stays compared to normoxaemia patients. Given the retrospective nature of our study, comprehensive randomized controlled trials are essential to fully assess the potential correlation between hyperoxaemia and outcomes in trauma patients.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- (a)BGA:
-
(Arterial) blood gas analysis
- AIS:
-
Abbreviated injury scale
- aOR:
-
Adjusted odds ratio
- ATLS:
-
Advanced trauma life support
- CO2 :
-
Carbon dioxide
- FiO2 :
-
Inspired oxygen fraction
- GCS:
-
Glasgow coma scale
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- ISS:
-
Injury severity score
- kPA:
-
Kilopascal
- KSSG:
-
Hospital of Canton St. Gallen, Switzerland
- LOS:
-
Length of hospital stay
- LOS ICU:
-
Length of ICU stay
- mmHg:
-
Millimetre of mercury
- PaCO2 :
-
Arterial partial pressure of carbon dioxide
- PaO2 :
-
Arterial partial pressure of oxygen
- PHTLS:
-
Prehospital trauma life support
- SaO2 :
-
Arterial oxygen saturation
- SD:
-
Standard deviation
- SpO2 :
-
Oxygen saturation
- WHO:
-
World Health Organization
References
WHO. Decade of Action for Road Safety 2011–2020: WHO; 2014 [Available from: https://www.who.int/publications/i/item/decade-of-action-for-road-safety-2011-2020.
van Breugel JMM, Niemeyer MJS, Houwert RM, Groenwold RHH, Leenen LPH, van Wessem KJP. Global changes in mortality rates in polytrauma patients admitted to the ICU-a systematic review. World J Emerg Surg. 2020;15(1):55.
Pfeifer R, Tarkin IS, Rocos B, Pape HC. Patterns of mortality and causes of death in polytrauma patients–has anything changed? Injury. 2009;40(9):907–11.
Aboyans V, Collaborators CoD. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet (British edition). 2015;385(9963):117–71.
Brun S. ATLS Advanced Trauma Life Support 10th Edition Student Course Manual. ATLS Advanced Trauma Life Support 10th Edition Student Course Manual: American College of Surgeons; 2018.
NAEMT NAoEMT. Phtls: Prehospital Trauma Life Support: Prehospital Trauma Life Support: Jones & Bartlett Pub Inc; 2019.
Eskesen TG, Baekgaard JS, Christensen RE, Lee JM, Velmahos GC, Steinmetz J, et al. Supplemental oxygen and hyperoxemia in trauma patients: A prospective, observational study. Acta Anaesthesiol Scand. 2019;63(4):531–6.
McMullan J, Rodriquez D, Hart KW, Lindsell CJ, Vonderschmidt K, Wayne B, et al. Prevalence of prehospital hypoxemia and oxygen use in trauma patients. Mil Med. 2013;178(10):1121–5.
Eskesen TG, Baekgaard JS, Steinmetz J, Rasmussen LS. Initial use of supplementary oxygen for trauma patients: a systematic review. BMJ Open. 2018;8(7): e020880.
Chu DK, Kim LH, Young PJ, Zamiri N, Almenawer SA, Jaeschke R, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391(10131):1693–705.
Staehr-Rye AK, Meyhoff CS, Scheffenbichler FT, Vidal Melo MF, Gatke MR, Walsh JL, et al. High intraoperative inspiratory oxygen fraction and risk of major respiratory complications. Br J Anaesth. 2017;119(1):140–9.
Six S, Jaffal K, Ledoux G, Jaillette E, Wallet F, Nseir S. Hyperoxemia as a risk factor for ventilator-associated pneumonia. Crit Care. 2016;20(1):195.
Schjorring OL, Klitgaard TL, Perner A, Wetterslev J, Lange T, Siegemund M, et al. Lower or Higher Oxygenation Targets for Acute Hypoxemic Respiratory Failure. N Engl J Med. 2021;384(14):1301–11.
Taher A, Pilehvari Z, Poorolajal J, Aghajanloo M. Effects of Normobaric Hyperoxia in Traumatic Brain Injury: A Randomized Controlled Clinical Trial. Trauma Mon. 2016;21(1): e26772.
Douin DJ, Anderson EL, Dylla L, Rice JD, Jackson CL, Wright FL, et al. Association Between Hyperoxia, Supplemental Oxygen, and Mortality in Critically Injured Patients. Crit Care Explor. 2021;3(5): e0418.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800–4.
Baker SP, O’Neill B. The injury severity score: an update. J Trauma. 1976;16(11):882–5.
Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96.
Medicine AftAoA, editor The Abbreviated Injury Scale 2015 revision. Des Plaines: AAAM; 2015.
Robba C, Battaglini D, Cinotti R, Asehnoune K, Stevens R, Taccone FS, et al. Individualized Thresholds of Hypoxemia and Hyperoxemia and their Effect on Outcome in Acute Brain Injured Patients: A Secondary Analysis of the ENIO Study. Neurocritical care. 2023.
Baekgaard J, Siersma V, Christensen RE, Ottosen CI, Gyldenkaerne KB, Garoussian J, et al. A high fraction of inspired oxygen may increase mortality in intubated trauma patients - A retrospective cohort study. Injury. 2022;53(1):190–7.
Acknowledgements
None.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
WH designed the project. MI, WH, DJ, CM, MM, UP, GK performed the study. MI, WH, MM analysed and interpreted the data. MI, WH, MM drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the local cantonal ethics committee of the Canton of St. Gallen (approval EKOS 23/178, project number 2023–01801).
Consent for publication
Not applicable.
Competing interests
JS holds a professorship that is funded by The Norwegian Air Ambulance foundation. The other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Iten, M., Pietsch, U., Knapp, J. et al. Hyperoxaemia in acute trauma is common and associated with a longer hospital stay: a multicentre retrospective cohort study. Scand J Trauma Resusc Emerg Med 32, 75 (2024). https://doi.org/10.1186/s13049-024-01247-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-024-01247-5