Abstract
Background
The ELCID Trial was a feasibility randomised controlled trial examining the effect on lung cancer diagnosis of lowering the threshold for referral for urgent chest X-ray for smokers and recent ex-smokers, aged over 60 with new chest symptoms. The qualitative component aimed to explore the feasibility of individually randomising patients to an urgent chest X-ray or not and to investigate any barriers to patient recruitment and participation. This would inform the design of any future definitive trial. This paper explores general practice staff insights into participating in and recruiting to diagnostic trials for possible/suspected lung cancer.
Methods
Qualitative interviews were conducted with 11 general practice staff which included general practitioners, a nurse practitioner, research nurses and practice managers.
Interviews were analysed using a framework approach.
Results
Findings highlight general practice staff motivators to participate in the trial as recruiters, practice staff interactions with patients recruited onto the study, methods of organisation staff used to undertake the trial, the general impact of the trial on practice staff, how the trial research team supported the practices and lastly practice staff suggestions for trial delivery improvement.
Conclusions
The integration of a qualitative component focused on staff experiences participating in a lung diagnostic trial has demonstrated the feasibility to recruit for similar future studies within general practice. Although recruitment into trials can be difficult, results from our study offer suggestions on maximising patient recruitment not just to trials in general but also specifically for a lung diagnosis study.
Trial registration
ClinicalTrials.gov, NCT01344005. Registered on 27 April 2011
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Recruitment in general practice clinical trials
The importance of research in general practice (GP) is longstanding
The values of general practice underpin a challenging research agenda spanning: preventive medicine, early diagnosis, acute and chronic disease management, personalised care, and the understanding of beliefs and behaviours relating to health and illness. These areas of focus are of increasing importance to the UK's healthcare agenda which promotes healthy living and pro-active disease management. p. 5 [1].
In 2006, the Royal College of General Practitioners (RCGP) set up its Research Ready Scheme to support general practices to be research active and this scheme has, to date, accredited over 500 UK practices [2]. By 2018/2019, the Primary Care Specialty recruited 160,000 participants into the National Institute of Healthcare Research (NIHR) Clinical Research Network studies [3].
Maximising recruitment of research participants into randomised controlled trials (RCTs) within general practice is of great importance if rigorous research is to be carried out. However, the failure to recruit adequate numbers of participants has long been a major barrier to the completion of RCTs in primary care globally [4,5,6].
The use of qualitative research methods along trials is being increasingly used to bring to light the reasons for recruitment difficulties in trials. In their systematic review of improving the recruitment activity of clinicians in randomised controlled trials, Fletcher and colleagues [7] highlighted the importance of using qualitative research methods alongside trials
‘the most promising intervention identified by this review was the use of qualitative methods embedded in host RCTs to define appropriate methods, targeted at clinicians, relevant to the context of the individual studies’ p.1
Indeed, primary care trials are increasingly using embedded qualitative research methods to uncover important information relating to recruitment onto trials.
The benefits of embedding qualitative research into primary care randomised controlled trials to explore recruitment issues
Donovan and colleagues [8] used in-depth interviews alongside the ProtecT (prostate testing for cancer and treatment) trial carried out on general practice sites to investigate recruitment challenges between recruiting sites and over time. They found that recruiters had difficulty discussing equipoise and presenting treatments equally and that the terminology that recruiters used was also misinterpreted by participants. This information allowed for changes to be made to the content and presentation of the information and ultimately helped to improve the differing levels of recruitment.
Qualitative interviews were also used with trial staff and recruiting clinicians to explore under recruitment of patients to a community trial concerning patients with severe mental illness and supported employment [9]. Reasons included misconceptions about the trial, a perceived lack of study equipoise, misunderstanding of the trial arms and differing interpretations of eligibility and paternalism. Based on this information, the authors advocate clinician and patient involvement in the study design to improve recruitment in future similar trials.
Paramisivan and colleagues [10] also explored reasons for low recruitment during their qualitative recruitment investigation in the SPARE (Selective bladder Preservation Against Radical Excision) feasibility trial. They highlighted problems relating to equipoise, highlighting treatment preferences amongst both participants and staff. They also found that clinicians had difficulties in identifying eligible patients. Trial information was consequently simplified, recruitment pathway focused around lead recruiters, and training sessions were provided for recruiters. Problems with patient eligibility however could not be resolved.
Similarly, Noble and colleagues [11] illustrated important qualitative research findings relating to patient recruitment difficulties. This trial aimed to identify the most clinically and cost-effective length of anticoagulation with low molecular weight heparin (LMWH) in the treatment of cancer associated thrombosis. Although the study could not recruit adequate numbers for the study, interviews with recruiting clinicians highlighted existing beliefs about medication and the length of time patients needed to be anticoagulated. Study equipoise was also questioned. The authors conclude that the lessons learnt from this study offer useful insights pertaining to the design of future similar studies.
The ELCID trial
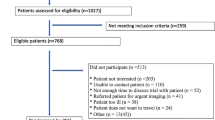
The ELCID feasibility trial [12] (Fig. 1) aimed to improve lung diagnosis by examining the value of lowering the threshold for ordering a chest X-ray for suspected lung cancer symptoms in the primary care setting. Specific outcomes included evaluating trial design, materials, and intervention and the training and recruitment of practices, including the recruitment and randomisation of patients.
The control group reflected NICE referral guidance (at the time) whereby patients were urgently referred if they were experiencing one of a number of chest symptoms present for more than 3 weeks. The trial intervention, termed ‘Extra-Nice’, meant randomised patients received an urgent chest X-ray if they presented with one of a number of chest symptoms of any duration, smoked, or were ex-smokers, and who were over 60 years. Eligibility included patients who were over 60 years of age and were either smokers or ex-smokers with 10 or more pack years of smoking history. They also needed to have presented at a general practice with a new or altered cough of any duration or increased breathlessness or wheezing (whether or not associated with purulent sputum) [13]. In view of recruitment difficulties, however, the eligibility status was revised to be less strict and the criteria changed from receiving only current smokers and non-smokers of 5 years or less to accepting smokers and non-smokers with no time duration associated.
The aim of this trial was to inform the design of a large UK-wide, clinical trial [12] to lower the threshold for investigating patients presenting with symptoms of possible lung cancer. The study involved health economics, quality of life, qualitative and quantitative methods, in order to fully assess feasibility.
The ELCID qualitative study
The integrated qualitative study was carried out with the aim of exploring the feasibility of individually randomising patients to an urgent chest X-ray or not and to investigate any barriers to patient recruitment and participation. A previous paper reported on patient experiences of participating in the trial [14]. This current paper reports on practice staffs’ experiences of participating in the trial. Our paper is the only one to date which has qualitatively explored practice staffs’ experiences of recruiting eligible patients into trials for lung disease diagnosis.
This ELCID qualitative Study is reported in line with the guidelines set out in Consolidated Criteria for Reporting Qualitative Research (COREQ) [15].
The aim of the paper
This paper aims to identify the critical enablers and barriers to recruitment to a lung disease randomised clinical trial that recruited participants through general practices (GP). It reports and discusses selected findings from the ELCID feasibility trial, a diagnostic trial of lung disease in general practice which examines staff attitudes and experiences of participating in a trial of this nature. The paper focuses on experiences of the staff working in general practices who recruited to ELCID. It addresses a gap in evidence regarding factors influencing recruitment to research in general practice. Recommendations from this qualitative study can be used for the design of the further lung diagnostic trials.
Methods
Study design
This was a multicentre, qualitative study which was embedded within a trial.
Recruitment of GP Practices onto the trial
GP practices were recruited into the trial from Wales and Yorkshire with 22 practices ultimately recruiting and randomising 255 patients (Fig. 2). Recruitment of practices was assessed by practice size, known research activity—Primary Care Research Incentive Scheme (PiCRIS) and number of months open to recruitment [12]. Those practices who agreed to take part in the trial also agreed to participate in the embedded qualitative study.
Practices were initially sent a letter to determine their interest in the trial. If they agreed to participate in the trial, the research team would deliver a training day at the practice site which consisted of a PowerPoint presentation covering all aspects of the study.
Staff roles in the trial
Practice staff had individual roles in the study (Fig. 3). GPs recruited eligible patients during patient consultations and discussed the study with patients and provided written informed consent in the form of participant information sheets and consent forms. If patients were interested in participating, they were either consented to the trial or if they preferred, given a future appointment with the GP to consent.
Practice staff also retrospectively searched patient records of previous week’s consultations (where practice resources allowed) to determine eligible patients. These patients were then telephoned by the practice staff and invited to make an appointment with their GP to discuss the study.
When patients were consented onto the study, they were then individually randomised to either an urgent chest X-ray or usual care (NICE 2015). Randomisation took place centrally via the Bristol Randomised Trials Collaboration. Patients were then informed of their allocation and directed to a practice staff member who assisted them with populating the study documentation, a suite of health questionnaires [16,17,18,19,20,21,22] (Table 1). These same questionnaires were also posted to patients 2 months later. Twelve months after the patients’ randomisation, general practices were contacted by the research team for information on the outcomes of any chest X-rays, health service resource use and clinical outcomes.
Practices were reimbursed financially for the time staff spent participating in the trial. Also, occasional prizes were awarded to practices for best or most improved recruitment. During the study, the practices also received newsletters which highlighted information on on-going recruitment between the practices.
Recruitment of practice staff for qualitative interviews and data collection
During the implementation of the trial, practice managers invited staff to volunteer for an interview with the qualitative researcher. The qualitative researcher (HP) introduced herself to the interviewees by visiting or telephoning the practices. Ten interviews were carried out with 4 GPs, 3 research nurses, 3 members of practice management (1 interview with both a manager and a deputy manager) and 1 nurse practitioner (Table 2). Purposive sampling was used according to the demographic breakdown of recruiters and to ensure a range of participants based on practice recruitment levels and staff roles. Participants were recruited from practices with low (0–2 patients recruited), medium (3 to 4 patients recruited) and high (5 or more patients recruited) recruitment levels. This distinction was an arbitrary one and based on researcher experience. Participants were also recruited with both clinical and managerial roles.
The qualitative interviews
The trial and the interviews were carried out simultaneously. The audio-recorded interviews, which lasted between 22 min and 46 min, were carried out by the first author of this paper (HP), a female researcher with a good knowledge of the healthcare system and experienced in qualitative interviewing. The researcher had a clinical background but assumed the researcher role for the interviews. She did not hold any strong views about lung disease diagnosis trials and remained neutral on issues that were discussed with the recruiters. The interviews were carried out at the participants’ place of work, the general practices with only interviewees being present.
The interview guide reflected the aim of the study: to explore the feasibility of individually randomising patients to an urgent chest X-ray or not and to investigate any barriers to patient recruitment and participation. Topics included the following:
-
Feelings about participating in a trial concerning lung disease
-
Reasons for taking part in the trial
-
Experiences of taking part in the trial (including practice training to participate in the trial, the use of trial documentation, the recruitment of patients, the referral process)
-
Motivators/demotivators in participating in the trial
-
Thoughts on the equipoise of the trial
No new topics emerged during the first few interviews so the interview guide remained unchanged. Field notes were carried out by the qualitative researcher immediately following the interview.
Data analysis
Staff interviews were uploaded via digital media for transcription using a standard operating procedure (SOP) to ensure participant confidentiality. These were then transcribed verbatim and anonymised before being uploaded to NVivo 10 software [23] where relevant extracts were isolated and coded. Data analysis was conducted using Framework Analysis [24]. This analysis technique includes familiarisation (where the researcher becomes immersed in the data), developing a theoretical framework (where a hierarchical thematic framework is developed to classify and organise data into key themes, concepts, and categories), indexing (where the framework is applied to the original data transcripts and coded accordingly) and charting (where each theme is charted using a table or matrix using summaries of the data) and mapping and interpretation (where the charts and data are examined for patterns and connections). The main qualitative researcher was assisted by a second qualitative researcher who carried out 10% of the interviews to ensure validity of the analysis and to verify interpretation. A thematic hierarchy was produced and any disagreements were resolved through discussion.
Results
These results reflect the aim of the study and the topics set out in the interview guide. They highlight what motivated practices to participate in the trial as recruiters, how practice staff interacted with patients recruited onto the study, what methods of organisation the practice used to undertake the trial, the general impact of the trial on practice staff, how the trial research team supported the practices and lastly the practice staff suggestions for trial delivery improvement. Table 3 summarises the results of our study, and Table 4 suggests actions to assist patient recruitment into a lung diagnosis trial.
Practice motivation to join the trial as recruiters (Table 5)
A genuine interest in the trial focus
Recruiters’ motivation to take part in the study was largely due to a genuine interest in the focus of the ELCID clinical trial, which was to examine the effect on lung cancer diagnosis of lowering the threshold for referral for urgent chest X-ray for smokers and recent ex-smokers, aged over 60 with new chest symptoms.
Having the required patient population
Many also said that they took part because they believed that they had the appropriate patient population.
Professional and practice development
An additional motivation was the need to develop the practice and improve cancer diagnosis. Others talked of the desire to develop professionally in an individual capacity, for example, it would help with their personal profile and enable them to document the study. Participating in the study was also deemed as evidence of awareness of the NICE guidelines as well as it being advantageous for appraisals. The desire to expand the surgery’s network through making connections with research institutions was also highlighted.
The ‘feel-good’ factor
The feel-good factor of why staff participated in the trial was also highlighted.
The financial incentive
The importance of the financial incentive in relation to trial engagement was hailed as being significant to the extent that participation in the study would have been at stake. It was highlighted that a GP surgery is run as a business which has staffing implications, hence the importance of finance. The financial incentive had allowed one surgery to expand. Similarly, one GP pointed out that if they recruited enough patients onto the trial, then the two healthcare assistants that helped with recruitment would pay for themselves.
Health professionals’ interactions with patients (Table 6)
This theme captured recruiters’ experiences of the recruiting process: problems identifying eligible patients, presenting the trial to the patients, referring patients for chest X-rays and providing patient support.
Problems and disincentives to identifying eligible patients
Although patients with chest infections were presenting at the practices regularly, few patients were being recruited. Recruiting patients onto the trial was a problem for the practice staff. Difficulties recruiting were subsequently highlighted with reports of the eligibility criteria being too narrow as well as overestimation of how many practice patients would fit the eligibility criteria. Ultimately, the eligibility criteria had to be revised. Disincentives to identifying patients for the research study included the fear of patients having unnecessary X-rays and the fear of GPs being overworked and too busy. Confusion surrounding the whole study process led to staff not wanting to identify any patients, as it highlighted to others confusion surrounding the study process. A general indifference to the task of trial recruitment was also noted. Patient lack of time was also proposed if patients were busy. Financial constraints were also highlighted as demotivators to recruit patients.
Presenting the trial to patients
The GPs most commonly had first contact with patients regarding the trial and the research discussion would take place during the consultation. The patient would usually then be referred to another health professional for further information.
It was stated that the study was difficult to carry out if patients had other needs or were pressed for time although recruiting an ex-smoker for a lung diagnosis trial was deemed easy during a consultation. Many practices telephoned patients who may have been eligible for the trial. However, worries about increasing a patient’s anxiety by telephoning them to discuss the study were highlighted. Several methods were used to allay patient anxiety such as choosing one’s language carefully or explaining to the patient that they were not looking for cancer, but rather wanted to help research or change practice. However, most of the recruiters said that patient anxiety had not been a problem because of the current popularity of advertising early chest X-rays.
Completion of patient health questionnaires
Documentation presented a problem because of the lengthy time it took to finish. Helping patients to populate the patient questionnaires was unproblematic for other recruiters. However, one recruiter in particular, highlighted several problems with them for example, some questions not being relevant to the study and patients not understanding the questions and needing help to populate the questionnaires. This same recruiter stated that it is the GP who should be asking the questions to better reassure the patient and felt unprepared and untrained for hearing confidential patient information. Similarly, this awkwardness with asking patients personal questions was reiterated along with querying the relevance of some of the questions.
Explaining study chest X-ray referral to patients
Recruiters initially thought that all patients would want a chest X-ray referral on agreeing to participate in the trial. However, they discovered that patients either did not mind if they received a chest X-ray or preferred not to have a chest X-ray. Patients were reassured however that they would not be deprived of having a chest X-ray if the GP felt that it was necessary.
Patient feedback to health professionals following recruitment
Two recruiters shared feedback on the impact that the trial had on patients’ wellbeing during the trial. They stated that if the patients received a chest X-ray, then they were more likely to be anxious or worried in the period it took to receive their results. For example, a patient came back to the GP Practice following her chest X-ray to ask for her results which she had been worrying about. Moreover, another patient was anxious as following the chest X-ray; she had required additional investigations by way of a CT scan and had to wait for the results which ultimately were fine.
Practice organisation to undertake the trial (Table 7)
To deal with these administrative challenges of running a study, increasing the hours of their practice nurse to compensate for the time it took to fill out the questionnaires with the patients was proposed.
Establishing key staff members responsible for the study to ensure continuity
It was suggested that it was essential to have one person responsible for the trial in the practice to ensure its success. The importance of the continuity of staff working on the trial was also stressed. One practice had had to use locum GPs for 6 months which had not helped the conduct of the trial. Indeed, another practice decided that it would be GPs who worked full time that would work on the study whereas the administration team would not. This was because the latter worked part time hours and would not be able to manage the commitment. This, however, created a lot more work for the GPs. However, a research nurse pointed out that her role is specifically to do research since the GPs at the practice are too busy.
A team effort and a comprehensive recruitment system
Recruiters also discussed the necessity for a clear system to recruit patients including a comprehensive plan for recruiting patients which required a team effort. This practice manager would send a message to the GPs to remind them of the trial eligibility criteria in addition to posting the criteria on their computer screens. If the GP found a suitable patient, the patient was referred to a healthcare assistant or a research nurse for an explanation of the study. In addition, the recruiter also used an online system to check other patients in the practice. If eligible patients were found, the recruiter would call them to ask them to come to the practice. The need to be timely and prompt when recruiting patients retrospectively (searching for patients through practice database lists) was also proposed.
Organisation of the Chest X-ray referral
The recruiters discussed the logistics of patients getting to the hospital for a chest X-ray. Many said that it was an easy trip that the patients could manage. Others however said that it was more difficult as there was a lack of free parking or it was too far to the hospital. Others still talked of paying for a taxi for patients if necessary.
Patients were reported to have been able to access chest X-rays quickly and efficiently. Only one recruiter said that it was difficult to book an ‘urgent’ X-ray and stated that a patient could not get an X-ray appointment for 8–10 days. However, there were also some initial problems of the X-ray department being unaware of the study and accessing the X-ray results.
General impact of the trial on the practice staff (Table 8)
The trial was seen to impact on the level of work which had to be conducted within the practice. A GP from a ‘high’ recruiting practice said that they had had to increase the hours of one of their practice Nurses and also take on a locum nurse. Another level of impact included practice staff anxiety due to waiting for patient chest X-ray results and concern for the patient waiting for the outcome. It was reported that a patient had become very anxious when they were being referred for a chest X-ray, and although the X-ray results were found to be clear, the clinician still felt guilty about invoking unnecessary anxiety for the patient.
However, the most common impact of the trial on practice staff was an increase in medical knowledge for example the length of delay in a possible cancer diagnosis. Another example is knowledge update on the safety of chest X-rays. An additional benefit of the trial related to knowledge of and engagement in research and research methods.
Researcher team support and involvement (Table 9)
Input from the research team
The training day presented by the research team was deemed as being generally very good with the information being presented concisely and appropriately for the audience variety. Some though found the trial detail overwhelming which necessitated too much paperwork. However, the research nurse who had undergone Good Clinical Practice (GCP) training (whilst her two GP colleagues had not) thought she felt more comfortable in the training.
Regarding ongoing support from the study team, the newsletters were described as helpful. Others highlighted the competitive nature of the newsletters which had a positive impact on the practice recruitment activity. The newsletters were also purported to be reassuring as recruiters could see that other practices were struggling to recruit also.
The genial nature of the research team was also highlighted by the practice staff, for example with regard to the support and encouragement that they received during the course of the trial.
Practice staff suggestions for improvement (Table 10)
The most popular suggestion for study improvement was the request for more administrative support. There was a proposal for ‘a workload share’ between the practice staff and the research study team, where the practice staff could scan patient records for eligibility whilst the research study team could explain the study to potential participants. It was even pointed out that the practice would be happy to decrease their study reimbursement if they had someone to help with recruitment. It was acknowledged though that this strategy may not be the best use of resources for the research study as recruitment numbers could be minimal in each individual practice. Furthermore, a nurse recruiter stated that since it is a GP alone that could consent patients, the research study team was limited in helping to conduct the study anyway.
Suggestions on how the study team could help the practices in the future included the practice managers/non clinical workers being consulted on the design of the trial and delivery of the trial. Also, one participant thought it would be beneficial having the support of a mentor.
Discussion
Our study focused on a lung diagnostic practice in general practice. It is the first to explore the experiences of general practice staff participating in and recruiting to a lung diagnostic trial. However, it also has relevance to the conduct of trials in primary care in general. Tables 3 and 4 set out the practical implications of the study findings. The following discussion reflects on the findings and their associations with existing literature.
The recruitment challenges and enhanced workload associated with a lung diagnosis trial
The issue relating to a strict ELCID patient eligibility status (which consequently needed revising) has been reflected in other studies. In their systematic review on effective recruitment strategies in primary care research, Ngune and colleagues [25] suggested using simple patient eligibility criteria to enhance recruitment. Hange and colleagues [26] too emphasised the importance of scrutinising the inclusion criteria in detail to ensure relevance to practice. In spite of careful consideration to the inclusion and exclusion criteria at the protocol stage of the trial, patient recruitment was quickly identified as a problem and the qualitative interviews highlighted the strict eligibility criteria being the issue. The failure to recruit according to our initial eligibility criteria could be associated with the significant decline in the UK population smoking [27]. Future trials concerning lung cancer diagnosis may therefore need to accept participants who have given up smoking for longer than 5 years, in order to meet the required recruitment target numbers.
Another reason for poor recruitment into the ELCID trial could be due to the clinician’s busy workload. For example, a study clinician admitted to dissuading himself from recruiting a patient if his clinic was busy, and because of this, lacked the motivation to recruit. This could be why one of the practice managers of a low recruiting practice had difficulty in understanding the poor recruitment rates since she had noted many eligible patients to recruit. Time challenges were identified as reasons for reluctance to recruit participants into other primary care studies [4, 26, 28,29,30]. Hange and colleagues [26] highlighted the difficulty that GPs have combining research and clinical work and stress the complicated and time consuming organisational demands of enrolling patients. Foster and colleagues [4] too found that poor recruitment into a study was associated with longer times to recruit the first patients. It is noteworthy that the research nurses in our study had roles that were dedicated to doing research and were both located in the high recruitment bracket (Table 2). Similarly, Potter and colleagues [31] highlighted that the research nurses in their study who had dedicated research time were those who recruited more successfully. Our study also highlighted that assistance with patient documentation was found to be time consuming for some staff, as was the case with other studies [32, 33]. The ELCID staff also had an additional time burden of dealing with X-ray departments.
An additional reason for GP reluctance to recruit was possibly worry over giving unnecessary chest X-rays to patients. For example, one of the GPs stated that he had originally been worried about the safety of the chest X-rays but the ELCID trial training had updated his knowledge and relayed his fears. Other practice staff also exhibited worries that the study could cause patient anxieties being recruited onto a lung diagnostic study which could diagnose cancer. This issue however was largely unfounded as ELCID patient interviews highlighted only a small number of patients being anxious regarding their participation [14]. Staff worries concerning patient reluctance to participate in the study control group, that is, not having the chest X-ray could also have affected clinician recruitment. This worry proved unfounded since although patients stated that they did prefer to have the chest X-ray, they still agreed to participate in the study [14].
Drivers to successful recruitment in a lung disease diagnosis trial
Understanding what motivates staff to recruit participants into trials has shown to be paramount when considering recruitment difficulties in primary care [6, 11, 34,35,36].
The ELCID staff interviews showed that a genuine interest in the topic of lung disease diagnosis helped to motivate staff to recruit. Several studies have shown similar links to improved recruitment in primary care, for example having a special interest in the trial subject area [37], the research question being of relevance [29, 38] and the benefits that the trial is providing [28, 39].
Our study also mirrors several studies with regard to the importance of being reimbursed financially [5, 30, 32, 40]. Several of our study GP practices used this financial incentive to pay for staff to recruit study participants. However, the fact that the most popular suggestion by the practices to improve the study was the request for more administrative support (with one even happy to decrease their financial reimbursement in return for help with recruitment) highlights how busy they were. It is noteworthy that the practice who recruited the most patients employed a research nurse to focus especially on research studies. This nurse had been funded by the Wales Primary Care Research Incentive Scheme (PiCRIS) [41] although this scheme is currently being revised [41]. Schemes like this are imperative if general practice is to continue to play an important role in improving patient care through research and innovation. This scheme also provides the research accreditation status that many staff desire.
Professional staff development and expanding the surgery’s research network as motivators to recruit in the ELCID study mirrored other studies, for example the importance of providing Continuing Professional Development (CPD) points [42], enjoying increased professional satisfaction [43] and having an interest in improving clinical practice [44].
Optimum organisation and continuity of care in a lung diagnosis trial in general practice
In their systematic review of effective recruitment strategies in primary care research, Ngune and colleagues [25] highlighted concepts of good organisational practices. These included the involvement of a discipline champion, having simple patient eligibility criteria and using strategies that reduce practitioner workload. They also point to the active participation of the primary care staff in the design and conduct of the research to enable effective strategies specific to the context of care delivery.
Our ELCID study staff participants highlighted similar concepts including the suggestion of one specific staff member taking responsibility for the trial within each practice. The fact that the research nurses recruited the most participants suggests that they may be the best staff member to take on this role. Continuity of staff member dealing with patient may be a beneficial aspect when a GP practice carries out a lung diagnosis study. The study may require arranging chest X-rays for anxious patients who may need further tests. Moreover, continued communication with a patient may help non-clinical staff feel more comfortable discussing health questions with patients for data collection. This was a problem highlighted by one of the ELCID practice managers.
Support and involvement by research team
Gaglio and colleagues [45] highlighted the importance of a strong rapport between researchers and practice staff in a primary care diabetes behaviour change programme and point out that this focus plays a key factor in research success. Our study staff too emphasised the genial nature of the study team and the good support that they received. Some staff found the study training day overwhelming, thus highlighting the necessity of continuing researcher support in trials. Our use of newsletters has also been used successfully in other studies to provide focus and reminders to staff [31, 46, 47].
Strengths and limitations of the study
Our study was the first to explore general practice participation in a trial to detect possible lung disease. It also used embedded qualitative research methods to enhance learning associated with the trial. A cross section of the staff that were interviewed included practice managers, GPs, practice nurses, research nurses and administrative staff, and this allowed for a more complete picture of staff participation in the study. However, although the study interviewed a variety of staff that worked at the practice, numbers of staff interviewed per group were small. A larger number of interviews of each staff group would have generated a clearer picture of the attitudes and experiences of each staff group.
Conclusion and recommendations
The integration of a qualitative component focused on staff experiences participating in a lung diagnostic trial has demonstrated the feasibility to recruit for similar future studies within general practice. Although recruitment into trials can be difficult, results from our study offer suggestions on maximising patient recruitment not just to trials in general but also specifically for a lung diagnosis study. Table 4 suggests key recommendations to maximise patient recruitment in general practice trials.
Availability of data and materials
Study data will always remain confidential whilst the study is ongoing. Once the study has been completed, the data has been ratified and results published, the data will be made available to external academic researchers. Requests for access to data will be directed to the Marie Curie Research Centre, where the Scientific Director of the Centre will be identified as the data custodian for the trial and will ensure adherence with Marie Curie and University policy. Where the study has been undertaken in conjunction with a Clinical Trials Unit, the request for data release will be made to that trials unit and processed in accordance with their data sharing protocols.
References
The Academy of Medical Sciences. Research in general practice: bringing innovation into patient care. Workshop Report. 2009.
Research Ready. [https://www.rcgp.org.uk/researchready]. Accessed Oct 2020.
Primary Care Speciality Profile: why you should deliver primary care research in the UK. [https://www.nihr.ac.uk/documents/primary-care-specialty-profile/11603]. Accessed Oct 2020.
Foster JM, Sawyer SM, Smith L, Reddel HK, Usherwood T. Barriers and facilitators to patient recruitment to a cluster randomized controlled trial in primary care: lessons for future trials. BMC Med Res Methodol. 2015;15(1):1–9. https://doi.org/10.1186/s12874-015-0012-3.
Pearl A, Wright S, Gamble G, Doughty R, Sharpe N. Randomised trials in general practice-a New Zealand experience in recruitment. N Z Med J. 2003;116(1186):U681.
van der Gaag WH, van den Berg R, Koes BW, Bohnen AM, Hazen LMG, Peul WC, et al. Discontinuation of a randomised controlled trial in general practice due to unsuccessful patient recruitment. BJGP Open. 2017;1(3) https://doi.org/10.3399/bjgpopen17X101085.
Fletcher B, Gheorghe A, Moore D, Wilson S, Damery S. Improving the recruitment activity of clinicians in randomised controlled trials: a systematic review. BMJ Open. 2012;2(1):e000496. https://doi.org/10.1136/bmjopen-2011-000496.
Donovan J, Little P, Mills N, Smith M, Brindle L, Jacoby A, et al. Quality improvement reportImproving design and conduct of randomised trials by embedding them in qualitative research: ProtecT (prostate testing for cancer and treatment) studyCommentary: presenting unbiased information to patients can be difficult. Bmj. 2002;325(7367):766–70. https://doi.org/10.1136/bmj.325.7367.766.
Howard L, de Salis I, Tomlin Z, Thornicroft G, Donovan J. Why is recruitment to trials difficult? An investigation into recruitment difficulties in an RCT of supported employment in patients with severe mental illness. Contemp Clin Trials. 2009;30(1):40–6. https://doi.org/10.1016/j.cct.2008.07.007.
Paramasivan S, Huddart R, Hall E, Lewis R, Birtle A, Donovan JL. Key issues in recruitment to randomised controlled trials with very different interventions: a qualitative investigation of recruitment to the SPARE trial (CRUK/07/011). Trials. 2011;12(1):78. https://doi.org/10.1186/1745-6215-12-78.
Noble SI, Nelson A, Fitzmaurice D, Bekkers M-J, Baillie J, Sivell S, et al. A feasibility study to inform the design of a randomised controlled trial to identify the most clinically effective and cost-effective length of Anticoagulation with Low-molecular-weight heparin In the treatment of Cancer-Associated Thrombosis (ALICAT). Health Technol Assess (Winchester, England). 2015;19(83):vii.
Neal RD, Barham A, Bongard E, Edwards RT, Fitzgibbon J, Griffiths G, et al. Immediate chest X-ray for patients at risk of lung cancer presenting in primary care: randomised controlled feasibility trial. Br J Cancer. 2017;116(3):293–302. https://doi.org/10.1038/bjc.2016.414.
Hurt CN, Roberts K, Rogers T, Griffiths GO, Hood K, Prout H, et al. Protocol for a feasibility clinical trial examining the effect on lung cancer diagnosis of offering a chest X-ray to higher risk patients with chest symptoms. Trials. 2013;14(1):405. https://doi.org/10.1186/1745-6215-14-405.
Prout HC, Barham A, Bongard E, Tudor-Edwards R, Griffiths G, Hamilton W, et al. Patient understanding and acceptability of an early lung cancer diagnosis trial: a qualitative study. Trials. 2018;19(1):419. https://doi.org/10.1186/s13063-018-2803-4.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. https://doi.org/10.1093/intqhc/mzm042.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
Costing psychiatric interventions. Discussion Paper 1536. PSSRU, University of Kent at Canterbury. [http://www.pssru.ac.uk/pdf/dp1536.pdf]. Accessed Oct 2020.
Ridyard CH, Hughes DA. Methods for the collection of resource use data within clinical trials: a systematic review of studies funded by the UK Health Technology Assessment program. Value Health. 2010;13(8):867–72. https://doi.org/10.1111/j.1524-4733.2010.00788.x.
Ridyard CH, Hughes DA, Team D. Development of a database of instruments for resource-use measurement: purpose, feasibility, and design. Value Health. 2012;15(5):650–5. https://doi.org/10.1016/j.jval.2012.03.004.
Coast J, Peters TJ, Natarajan L, Sproston K, Flynn T. An assessment of the construct validity of the descriptive system for the ICECAP capability measure for older people. Qual Life Res. 2008;17(7):967–76. https://doi.org/10.1007/s11136-008-9372-z.
Group TE. EuroQol-a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. https://doi.org/10.1016/0168-8510(90)90421-9.
EQ-5D-3 L user guide. [Available at http://www.euroqol.org/fileadmin/user_upload/Documenten/PDF/Folders_Flyers/EQ-5D-3 L_UserGuide_2015.pdf]. Accessed Oct 2020.
Qualitative data analysis software. [http://qsrinternational.com/nvivo]. Accessed Oct 2020.
Ritchie J. SL, Bryman A, Burgess RG: Analysing qualitative data. London: Routledge; 1994.
Ngune I, Jiwa M, Dadich A, Lotriet J, Sriram D. Effective recruitment strategies in primary care research: a systematic review. Qual Prim Care. 2012;20(2):115–23.
Hange D, Björkelund C, Svenningsson I, Kivi M, Eriksson MC, Petersson E-L. Experiences of staff members participating in primary care research activities: a qualitative study. Int J Gen Med. 2015;8:143. https://doi.org/10.2147/IJGM.S78847.
Adult smoking habits in the UK: 2018. [https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2018]. Accessed Oct 2020.
Ward E, King M, Lloyd M, Bower P, Friedli K. Conducting randomized trials in general practice: methodological and practical issues. Br J Gen Pract. 1999;49(448):919–22.
Van der Windt D, Koes BW, Van Aarst M, Heemskerk M, Bouter LM. Practical aspects of conducting a pragmatic randomised trial in primary care: patient recruitment and outcome assessment. Br J Gen Pract. 2000;50(454):371–4.
Brodaty H, Gibson LH, Waine ML, Shell AM, Lilian R, Pond CD. Research in general practice: a survey of incentives and disincentives for research participation. Mental Health Fam Med. 2013;10(3):163–73.
Potter R, Dale J, Caramlau I. A qualitative study exploring practice nurses’ experience of participating in a primary care–based randomised controlled trial. J Res Nurs. 2009;14(5):439–47. https://doi.org/10.1177/1744987108098228.
Tognoni G, Alli C, Avanzini F, Bettelli G, Colombo F, Corso R, et al. Randomised clinical trials in general practice: lessons from a failure. BMJ Br Med J. 1991;303(6808):969–71. https://doi.org/10.1136/bmj.303.6808.969.
Peto V, Coulter A, Bond A. Factors affecting general practitioners’ recruitment of patients into a prospective study. Fam Pract. 1993;10(2):207–11. https://doi.org/10.1093/fampra/10.2.207.
Schreijenberg M, Luijsterburg P, Van Trier Y, Rizopoulos D, Koopmanschap M, Voogt L, et al. Discontinuation of the PACE Plus trial: problems in patient recruitment in general practice. BMC Musculoskelet Disord. 2018;19(1):146. https://doi.org/10.1186/s12891-018-2063-1.
Bower P, Wilson S, Mathers N. How often do UK primary care trials face recruitment delays? Fam Pract. 2007;24(6):601–3. https://doi.org/10.1093/fampra/cmm051.
Foy R, Parry J, Duggan A, Delaney B, Wilson S. Lewin-van den Broek N, Lassen A, Vickers L, Myres P: How evidence based are recruitment strategies to randomized controlled trials in primary care? Experience from seven studies. Fam Pract. 2003;20(1):83–92. https://doi.org/10.1093/fampra/20.1.83.
Bell-Syer SE, Moffett JAK. Recruiting patients to randomized trials in primary care: principles and case study. Fam Pract. 2000;17(2):187–91. https://doi.org/10.1093/fampra/17.2.187.
Ross S, Grant A, Counsell C, Gillespie W, Russell I, Prescott R. Barriers to participation in randomised controlled trials: a systematic review. J Clin Epidemiol. 1999;52(12):1143–56. https://doi.org/10.1016/S0895-4356(99)00141-9.
McMullen H, Griffiths C, Leber W, Greenhalgh T. Explaining high and low performers in complex intervention trials: a new model based on diffusion of innovations theory. Trials. 2015;16(1):242. https://doi.org/10.1186/s13063-015-0755-5.
Dormandy E, Kavalier F, Logan J, Harris H, Ishmael N, Marteau TM, et al. Maximising recruitment and retention of general practices in clinical trials: a case study. Br J Gen Pract. 2008;58(556):759–66. https://doi.org/10.3399/bjgp08X319666.
Primary Care Research Incentive Scheme (PiCRIS) applications now being accepted. [https://www.healthandcareresearch.gov.wales/news/primary-care-research-incentive-scheme-picris-applications-now-being-accepted/]. Accessed Oct 2020.
Williamson MK, Pirkis J, Pfaff JJ, Tyson O, Sim M, Kerse N, et al. Recruiting and retaining GPs and patients in intervention studies: the DEPS-GP project as a case study. BMC Med Res Methodol. 2007;7(1):42. https://doi.org/10.1186/1471-2288-7-42.
Liu H, Massi L, Eades A-M, Howard K, Peiris D, Redfern J, et al. Implementing Kanyini GAP, a pragmatic randomised controlled trial in Australia: findings from a qualitative study. Trials. 2015;16(1):425. https://doi.org/10.1186/s13063-015-0956-y.
Ellis SD, Bertoni AG, Bonds DE, Clinch CR, Balasubramanyam A, Blackwell C, et al. Value of recruitment strategies used in a primary care practice-based trial. Contemp Clin Trials. 2007;28(3):258–67. https://doi.org/10.1016/j.cct.2006.08.009.
Gaglio B, Nelson CC, King D. The role of rapport: Lessons learned from conducting research in a primary care setting. Qual Health Res. 2006;16(5):723–34. https://doi.org/10.1177/1049732306286695.
Csipke E, Serfaty M, Buszewicz M. Optimizing recruitment from primary care: methods of recruiting older people with depression. Prim Health Care Res Dev. 2006;7(2):116–23. https://doi.org/10.1191/1463423606pc283oa.
Fransen GA, Van Marrewijk CJ, Mujakovic S, Muris JW, Laheij RJ, Numans ME, et al. Pragmatic trials in primary care. Methodological challenges and solutions demonstrated by the DIAMOND-study. BMC Med Res Methodol. 2007;7(1):16.
Acknowledgements
Many thanks to all the general practice staff who agreed to be interviewed for this study and to the practice staff who helped to recruit the patients for interview. Thanks also to the Research Partners and the Marie Curie Palliative Care Research Centre for conducting the qualitative component. The trial was developed on behalf of the National Cancer Research Institute (NCRI) Primary Care and Lung Clinical Studies Groups. It was sponsored by Bangor University.
Funding
This trial including the qualitative sub study was funded by the National Awareness and Early Diagnosis Initiative (NAEDI) Research Call Funding Partners (in alphabetical order): Cancer Research UK (trial reference: C8350/A12199); Department of Health, England; Economic and Social Research Council; Health and Social Care Research and Development Division, Public Health Agency, Northern Ireland; National Institute for Social Care and Health Research, Wales; and the Scottish Government (http://www.naedi.org.uk). Dr Annmarie Nelson’s post was funded by Marie Curie Cancer Care core grant funding (grantreference MCCC-FCO-17-C). Hayley Prout was funded by NAEDI as part of the clinical trial funding.
Author information
Authors and Affiliations
Contributions
AN designed the qualitative study, supervised the qualitative work, contributed to the design of the qualitative study, and was a management group member throughout. HP undertook the qualitative work under AN’s supervision and with advice from AT. HP wrote the first draft of the paper and was a management group member throughout. AT advised on the qualitative study, contributed to the writing of the qualitative paper and was a management group member throughout. RN was the chief investigator of the ELCID trial, contributed to the design of the trial and the writing of the qualitative paper and was a management group member throughout. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
NHS ethics was approved by the North Wales Research Ethics Committee (11/WA/022) on the 25 August 2011. This included the qualitative sub study for all the centres involved. We also obtained informed consent from each participant recruited onto the study.
Consent for publication
This qualitative study used anonymised quotes from study participants. They consented to their anonymised quotes being reported.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Prout, H., Tod, A., Neal, R. et al. Maximising recruitment of research participants into a general practice based randomised controlled trial concerning lung diagnosis—staff insights from an embedded qualitative study. Trials 23, 225 (2022). https://doi.org/10.1186/s13063-022-06125-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-022-06125-y






