Abstract
Background
Septic shock is now the leading cause of mortality in intensive care units (ICUs). Refractory septic shock requires high doses of vasopressors. Some previous studies have revealed that methylene blue could improve hypotension status and help reduce the dosage of catecholamines. This study aims to investigate the clinical effect of methylene blue in septic shock and explore whether it can increase arterial pressure and reduce the usage of vasopressors.
Methods
This study is a multicenter, randomized, placebo-controlled trial planning to include 100 refractory septic shock patients. The protocol is to administer a bolus of 2 mg/kg methylene blue intravenously followed by a continuous infusion of 0.5 mg/kg/h for 48 h. The primary outcome is the total dose of vasopressor required in refractory septic shock in the first 48 h. Secondary outcomes include other hemodynamic parameters, oxygen metabolism indexes, tissue perfusion indexes, major organ function indexes, and certain plasma cytokines and other factors.
Discussion
This protocol aims to evaluate the safety and efficacy of methylene blue as adjuvant therapy for refractory septic shock. The main outcome measure will be vasopressor requirements and hemodynamic parameters. Additionally, bedside ultrasonography, blood gases, and cytokines will be assessed to evaluate perfusion, respiratory, and metabolic effects. The results are intended to provide evidence on the safety and efficacy of methylene blue in refractory septic shock, guiding clinical decision-making.
Trial registration
This clinical trial has been registered at ChiCTR (https://www.chictr.org.cn/) on March 16, 2023. ChiCTR registration number: ChiCTR2300069430.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Background and rationale {6a}
Septic shock is a life-threatening condition characterized by organ dysfunction resulting from infection, with circulatory and cellular/metabolic dysfunction caused by dysregulated host response [1]. Septic shock is a leading cause of mortality in intensive care units (ICUs), with a mortality of 40% according to a meta-analysis [2]. Refractory septic shock is a state of inadequate tissue perfusion despite escalation of vasoactive therapy, recognizable by a requirement for norepinephrine (NE) exceeding 0.5 μg/kg/min or equivalent [3]. Mortality rates for refractory septic shock can reach 60% [4].
Patients with refractory septic shock commonly exhibit vasoplegia with poor response to catecholamine vasopressors. Meanwhile, high catecholamine doses can result in several adverse effects, such as digital ischemia, tachyarrhythmias, bacterial growth stimulation, and metabolic derangements [5]. Therefore, researchers proposed “decatecholaminization” to advocate catecholamine dose reduction, targeted beta-blockade use, and general de-stressing [6]. Methylene blue (MB) is considered to produce catecholamine-sparing effects through several mechanisms. First, MB selectively blocks soluble guanylyl cyclase (sGC) and inhibits inducible nitric oxide (NO) synthase without affecting constitutive NO synthase [7]. Second, MB oxidizes NO to inactive nitrate, reducing NO-mediated vasodilation [8]. Third, low/medium MB doses suppress superoxide production, reducing liver and kidney damage [9]. Finally, MB inhibits sGC [10], reducing NO-sGC binding and cGMP generation.
Several clinical trials have investigated the efficacy and safety of methylene blue in septic shock. Most of these trials suggest that MB can increase mean arterial pressure (MAP) and systemic vascular resistance (SVR) [11,12,13]. Following a bolus MB injection, MAP improves transiently for approximately 2–4 h. Repeated injections every 120 min sustain the pressure-raising effect for over 24 h [11, 14]. MB reduces vasopressor requirements [11, 15], thereby decreasing catecholamine-associated adverse effects. A recent trial demonstrated that MB initiation within 24 h of onset reduced time to vasopressor discontinuation and increased vasopressor-free days at 28 days [15]. Additionally, MB strengthens myocardial contraction, increases ventricular stroke work, and improves cardiac output [11,12,13]. Several studies suggest MB improves oxygen delivery and consumption [11, 13, 16]. Furthermore, MB reduces the serum lactate concentration by improving hemodynamics and redox reactions [12, 14, 16,17,18]. The serum concentration of inflammatory factors remains unchanged after MB administration. Current evidence indicates that MB does not significantly reduce septic shock mortality.
Methylene blue has few adverse effects, with the most common being blue discoloration of urine and skin. A few cases of nausea, vomiting, and diarrhea have been reported. However, higher MB doses (bolus over 5 mg/kg) increase adverse effects, including compromised splanchnic perfusion and transiently increased methemoglobin levels [11, 13, 19]. Overall, MB has been used for decades to treat methemoglobinemia and cyanide poisoning, with clinical applications demonstrating its adverse effects as minor, especially at lower dosages.
Unlike vasopressin, which acts primarily on V1A and V2 receptors, and angiotensin-2, which acts on angiotensin receptors, methylene blue exhibits a broader mechanism inducing vasoconstriction. Its potential mechanism of selectively inhibiting inducible nitric oxide synthase likely contributes to its fewer adverse effects. Existing clinical studies support methylene blue’s efficacy and safety. This clinical trial aims to further explore the application of MB in treating septic shock patients receiving norepinephrine exceeding 0.5 µg/kg/min, hopefully informing novel protocols for refractory septic shock.
Objectives {7}
Primary objective
To evaluate the effect of methylene blue on total vasopressor dose in refractory septic shock (time frame: 48 h. Epinephrine, phenylephrine, and dopamine doses will be converted to norepinephrine equivalents based on the following conversions: 100 mg dopamine equivalent to 1 mg norepinephrine, 1 mg epinephrine equivalent to 1 mg norepinephrine, and 2.2 mg phenylephrine equivalent to 1 mg norepinephrine).
Secondary objectives
To evaluate the effect of methylene blue on other hemodynamic parameters (such as mean arterial pressure and heart rate), oxygen metabolism indexes, tissue perfusion indexes, major organ function indexes, and certain plasma cytokines and other factors in septic shock.
Trial design {8}
This study is a randomized, multicenter, single-blind, and placebo-controlled trial that will be conducted in five centers across Guangdong Province, China. This study is a randomized, parallel-group trial with an allocation ratio of 1:1. The framework of the trial is designed to test for superiority.
The trial design follows SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) 2013 guidelines [20]. The trial report will adhere to CONSORT (Consolidated Standards of Reporting Trials) guidelines [21]. The protocol conforms to the Declaration of Helsinki principles and Good Clinical Practice standards.
Methods: participants, interventions, and outcomes
Study setting {9}
The trial will be conducted in five experienced ICUs in China with extensive expertise treating septic shock patients. The main research center has established collaborations with the participating sites to ensure a rigorous, coordinated, and high-quality study conforming to ethical and scientific standards. The study is scheduled from April 2023 to February 2024.
Eligibility criteria {10}
Inclusion criteria
-
(1)
Aged ≥ 18 years.
-
(2)
Diagnosis of septic shock based on the Sepsis-3 definition (2021 international consensus [1]). This definition includes suspected or confirmed infections, an increase in Sequential Organ Failure Assessment (SOFA) score by 2 or more points, the requirement for vasopressor therapy due to hypotension, and a lactate level greater than 2 mmol/L.
-
(3)
Septic shock requiring continuous norepinephrine infusion ≥ 0.5 μg/kg/min, or equivalent alternative vasopressors dose, to maintain mean arterial pressure (MAP) above 65 mmHg during and after the initial fluid resuscitation with at least 30 mL/kg IV crystalloid fluid.
-
(4)
Initially refractory septic shock diagnoses in participating hospitals.
Exclusion criteria
-
(1)
Pregnancy or lactation.
-
(2)
Allergy to methylene blue.
-
(3)
Glucose-6-phosphate-dehydrogenase deficiency.
-
(4)
Terminal cancer. (referring to patients with advanced-stage malignancies who have a prognosis of 6 months or less to live, as determined by their treating oncologist based on current medical assessments and standards)
-
(5)
Noninfectious risk factors leading to imminent death (e.g., uncontrollable hemorrhage, brain herniation).
-
(6)
Irreversible disease or terminal stage.
-
(7)
Refusing active treatment or planning to leave ICU within 48 h.
-
(8)
Enrollment in other clinical trials.
Who will take informed consent? {26a}
Patients developing refractory septic shock during hospitalization will be screened for eligibility. Attending physicians will report eligible patients to the central research group, which will confirm alignment with inclusion criteria. Legitimate informed consent will be obtained from the patients or legal representatives in participating centers. After completing informed consent procedures, eligible patients will be formally enrolled and randomized.
Patients will be screened to determine alignment with predefined inclusion and exclusion criteria. Written informed consent will be obtained from all participants or their legal representatives. In cases where participants are unable to provide consent due to septic shock, a suitable surrogate or legal representative will provide consent on behalf of the patient. If the participant regains capacity, consent will be requested from them as soon as possible to ensure their continued participation is voluntary and informed.
Additional consent provisions for collection and use of participant data and biological specimens {26b}
On the consent form, participants will be asked if they agree to the use of their data should they choose to withdraw from the trial. Participants will also be asked for permission for the research team to share relevant data with participating hospitals. This trial involves collecting biological specimens to measure the changes in hemodynamic parameters, oxygen metabolism indexes, major organ function indexes, and the changes in plasma cytokines and factors in 48 h.
Interventions
Explanation for the choice of comparators {6b}
The trial uses blank comparison to better assess the effects of the intervention and isolate the specific impact of methylene blue treatment without the influence of other variables. Besides, due to the special blue-green color of methylene blue, we have difficulty in finding a visually identical placebo. So this trial uses the solvent of methylene blue (5% glucose solution) as placebo.
Intervention description {11a}
After confirming eligibility, a 12-h timeframe is allocated to complete necessary procedures, including obtaining informed consent, preparing medications, collecting baseline data, and implementing necessary medical measures such as central venous catheter insertion and PICCO monitor placement. The attending physicians will initiate the interventions within 12 h of eligibility confirmation. The methylene blue group (MBG) will receive methylene blue injection plus standard therapy, while the placebo control group (PCG) will receive glucose injection plus standard therapy.
MBG patients will receive a 2 mg/kg methylene blue injection. Methylene blue injection (10 mg/ml) will be diluted with 5% glucose injection into a 50 ml solution. PCG patients will receive 50 ml of 5% glucose solution as a placebo.
The initial methylene blue injection will be administered intravenously via an injection pump over 20 min. Subsequent doses will be administered continuously at 0.5 mg/kg/h for 48 h. The PCG will receive 5% glucose solution intravenously via an injection pump over 20 min for the first dose. Subsequent doses will also be administered with 5% glucose solution continuously at 0.5 mg/kg/h for 48 h.
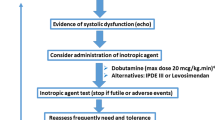
Regarding the vasopressor administration strategies, norepinephrine will be initiated first-line for both groups. Once the norepinephrine dose reaches ≥ 0.5 μg/kg/min, vasopressin will be added at a dose of 0.03 U/min. If hypotension persists despite maximal norepinephrine (3 μg/kg/min) and vasopressin doses, epinephrine will be administered and titrated up to 3 μg/kg/min. In addition to study interventions, patients will receive standard therapy administered by the attending physician in accordance with the “Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021” [1].
Criteria for discontinuing or modifying allocated interventions {11b}
-
(1)
If a participant experiences significant adverse events that outweigh the potential benefits of the intervention, the intervention will be discontinued.
-
(2)
If a participant or their legal representative requests to discontinue the intervention for any reason, the intervention will be discontinued.
-
(3)
If significant protocol deviations occur that impact the safety or efficacy of the intervention, the intervention may be modified or discontinued.
Strategies to improve adherence to interventions {11c}
We provide comprehensive education about the importance of adherence, the intervention protocol, potential benefits, and risks. This includes initial education sessions and ongoing reinforcement throughout the study. And the intervention regimen is simple for participants to follow.
Relevant concomitant care permitted or prohibited during the trial {11d}
Participants may continue with standard treatments for their condition that do not interfere with the study protocol. But patients’ enrollment in other clinical trials or experimental therapies is excluded from the trial and participants are not allowed to take experimental therapies.
Provisions for post-trial care {30}
Participants will receive follow-up care for a specified period after the trial concludes, ensuring that any ongoing health needs related to the trial are addressed.
Outcomes {12}
-
1.
Primary outcome
The primary outcome is the total vasopressor dose in refractory septic shock patients within 48 h. The total dose of norepinephrine, epinephrine, phenylephrine, and dopamine will be recorded from the start of the trial and converted into norepinephrine equivalents as previously described.
-
2.
Secondary outcomes
-
The changes in hemodynamic parameters in 48 h including mean arterial pressure (MAP), central venous pressure (CVP), heart rate (HR), global end-diastolic index (GEDI), cardiac index (CI), global ejection fraction (GEF), systemic vascular resistance index (SVRI), extravascular lung water index (ELWI), pulmonary vascular permeability index (PVPI), and stroke volume variation (SVV).
-
The changes in oxygen metabolism indexes in 48 h including fraction of inspired oxygen (FiO2), pH, arterial oxygen pressure (PaO2), arterial carbon dioxide pressure (PaCO2), arterial oxygen saturation (SaO2), alveolar-arterial gradient (P(A-a)O2), serum lactate level, oxygen delivery (DO2), oxygen consumption (VO2), oxygen extraction ratio (ERO2), and capillary refill time (CRT).
-
The changes in major organ function indexes in 48 h including hemoglobin, methemoglobin, total bilirubin, direct bilirubin, alanine transaminase, aspartate transaminase, creatinine, blood urea nitrogen, white blood cell count, blood platelet count, length of mechanical ventilation, length of continuous renal replacement therapy, and urine output.
-
The changes in plasma cytokines and factors in 48 h including nitric oxide, cGMP, IL-1, IL-1β, IL-2R, IL-6, IL-8, IL-10, TNF-α, reactive oxygen species (ROS), superoxide dismutase (SOD), nitrate, and nitrite.
-
-
3.
Safety outcomes
All adverse events, including severe adverse events, will be recorded and evaluated.
Participant timeline {13}
Time schedule of enrolment, interventions is shown in the schematic diagram (Fig. 1).
Sample size {14}
Based on the primary outcome of total vasopressor dose in refractory septic shock over 48 h, the sample size was determined by referring to a study by Lu et al. [18], which reported a mean norepinephrine dose of 11.4 (SD 5.8) μg/kg/min in the methylene blue continuous infusion group and 13.5 (SD 3.8) μg/kg/min in the control group within 24 h after the first bolus. Assuming a two-sided alpha of 0.05, 90% power, and a 10% dropout rate, a minimum of 28 patients in total is needed (PASS 15.0.5 software). The target sample size was increased to 100 patients (50 per group) to account for possible attrition and improve precision of the treatment effect estimate.
Recruitment {15}
The ICU healthcare providers (doctors, nurses) have been well trained to identify potential participants. And clear information about the trial’s purpose, procedures, potential risks, and benefits are provided to both patients (when possible) and their families to help them make informed decisions.
Assignment of interventions: allocation
Sequence generation {16a}
After obtaining informed consent, eligible patients will be enrolled and randomized using a computer-generated randomized allocation sequence (SPSS 26.0). Patients will be randomized 1:1 into two groups as enrolled at each site.
Concealment mechanism {16b}
Allocation information will be recorded on 100 identical cards, sealed in 100 opaque envelopes labeled with the admission sequence number. Envelopes will be securely stored by a designated research team member. Upon admission, the corresponding envelope will be opened to determine group assignment.
Implementation {16c}
The allocation sequence is generated by an independent statistician using a computer-generated randomized allocation sequence. Trained research staff will be responsible for enrolling participants. They will assess eligibility criteria, obtain informed consent, and ensure that all necessary baseline data is collected. The assignment of participants to interventions will be done by the independent statistician using the pre-generated allocation sequence.
Assignment of interventions: Blinding
Who will be blinded {17a}
This is a single-blind randomized controlled trial. Due to the distinct blue-green color of methylene blue solution, light-proof syringes, and extension tubing will be utilized. Syringes, tubing, urine collection containers, and urinary tubing will be concealed with aluminum foil to maintain blinding. Patients will remain blinded until study completion and database lock.
Procedure for unblinding if needed {17b}
Unblinding will occur if a related serious adverse event necessitates knowing the intervention.
Data collection and management
Plans for assessment and collection of outcomes {18a}
Baseline information
Age, gender, underlying diseases, infection site(s), pathogen type, SOFA score, and APACHE II score on admission will be collected and evaluated.
Blood pressure and vasopressors
Systolic and diastolic blood pressure, heart rate, and vasopressor dose will be recorded every hour.
Hemodynamics and blood gas analysis
Before administration and at 20 min, 2 h, 6 h, 12 h, 24 h, 2 days, 3 days, 5 days, and 7 days after the first bolus of methylene blue, the hemodynamics and blood gas analysis parameters will be recorded, which include CVP, HR, GEDI, CI, GEF, SVRI, ELWI, PVPI, SVV, FiO2, pH, PaO2, PaCO2, SaO2, P(A-a)O2, serum lactate level, DO2, VO2, ERO2, and CRT.
Organ function parameters
Before administration, at 12 h, 24 h, 2 days, 3 days, 5 days, 7 days, and 28 days after the first bolus of methylene blue, the following parameters will be collected:
-
Laboratory parameters: Hemoglobin, methemoglobin, total bilirubin, direct bilirubin, alanine transaminase, aspartate transaminase, creatinine, blood urea nitrogen, white blood cell count, and blood platelet count.
-
Length of mechanical ventilation, length of continuous renal replacement therapy, and urine output.
-
Inferior vena cava respiratory variation and ejection fraction evaluated by ultrasonography.
-
Glasgow coma scale (GCS), analgesic, and sedative medication.
Cytokines and other mediators
Blood samples will be collected before administration and at 20 min, 2 h, 6 h, 12 h, 24 h, 2 days, 3 days, 5 days, and 7 days after the first bolus. These samples will be tested for nitric oxide, cGMP, IL-1, IL-1β, IL-2R, IL-6, IL-8, IL-10, TNF-α ROS, SOD, nitrate, and nitrite.
Other data
At the study endpoint, infection sites, pathogen type, 24-h, 48-h, 72-h, and 7-day mortality, length of stay in ICU, and length of stay in hospital will be recorded (Fig. 1).
Data quality assurance processes
All data collectors and assessors received training on the study protocols, data collection procedures, and the use of instruments to ensure consistency and accuracy. Critical measurements will be performed in duplicate to verify accuracy and reliability.
Plans to promote participant retention and complete follow-up {18b}
We will provide support and education about the importance of follow-up and how it contributes to the overall success of the study. For participants who choose to discontinue the intervention early, we attempt to conduct a final follow-up visit to collect key outcome data.
Data management {19}
Data will be recorded on paper case report forms, entered into a database, and uploaded to the ResMan website (www.medresman.org.cn). The paper case report forms will be properly stored by research group members, and the ResMan website data will be kept confidential until the end of the trial.
Confidentiality {27}
We will assign unique participant codes, removing names, and other direct identifiers from data set. There is limited access to personal information to authorized study personnel only. And personal information is stored in secure, password-protected cabinet.
Plans for collection, laboratory evaluation, and storage of biological specimens for genetic or molecular analysis in this trial/future use {33}
Blood samples are collected at specified time points according to the collection plan. Blood samples will be centrifuged, aliquoted, and appropriately labelled. Then the samples will be stored in − 80n the samples will be st.
Statistical methods
Statistical methods for primary and secondary outcomes {20a}
Statistical analysis will be performed using SPSS 26.0 software. Continuous data will be presented as the mean (standard deviation) or median (interquartile ranges) for non-normal distributions. Categorical data will be presented as rates or proportions. For normally distributed continuous data with equal variance between the two groups, Student’s t-test will compare groups. If the data do not meet the normal distribution assumption, the Mann–Whitney U test will be applied. One-way ANOVA will be performed for measurement data within groups if the data follow a normal distribution and have an equal variance. Otherwise, the Kruskal–Wallis test will be used. Multiple comparisons will be made using the LSD method. Chi-square analysis will be conducted for enumeration data. The significance level α will be set at 0.05 (two-sided) with a power of 90%. Differences with P < 0.05 will be considered statistically significant.
Interim analyses {21b}
This trial will include one interim analysis to be conducted after 50% of the participants have been enrolled and have completed the primary outcome assessment. The interim analysis will be performed by an independent Data Monitoring Committee (DMC) to evaluate safety, efficacy, and futility.
The trial will be stopped early if the intervention clearly causes harm or shows significant benefit over the control group. The trial may also be stopped for futility if interim results suggest that it is unlikely to achieve the desired outcome.
Methods for additional analyses {20b}
This trial may conduct analyses on subgroups of patients based on different age ranges or SOFA scores.
Methods in analysis to handle protocol non-adherence and any statistical methods to handle missing data {20c}
Statistical analysis will follow the intention-to-treat (ITT) principle. Missing data will be addressed using last observation carried forward (LOCF) imputation.
Plans to give access to the full protocol, participant-level data, and statistical code {31c}
The full trial protocol will be made available in ChiCTR. A detailed version of the protocol will be published.
Oversight and monitoring
Composition of the coordinating center and trial steering committee {5d}
The coordinating center includes the principal investigator (PI), project manager, clinical research coordinator, data manager, and biostatistician. Principal investigator provides overall leadership and ensures protocol adherence. Project manager manages daily trial operations, coordinates with study sites, and oversees the study timeline. Clinical research coordinator assists in patient recruitment, ensures protocol compliance at study sites, and manages site communications. Data manager manages data collection, entry, and integrity. Biostatistician develops statistical analysis plans, performs data analyses, and interprets results. The coordinating center team meets weekly to review study progress, address issues, and ensure smooth trial operations.
The trial steering committee includes independent experts in clinical trials and senior members of the research team. The trial steering committee provides overall supervision of the trial, reviews and approves major protocol amendments, and monitors trial conduct and patient safety. The trial steering committee meets quarterly throughout the trial, with additional meetings as necessary.
Composition of the data monitoring committee, its role and reporting structure {21a}
The data monitoring committee includes a statistician, clinical experts, and ethics representative. They regularly review safety data, including adverse events and serious adverse events, assess the quality and integrity of the data being collected, and identify and evaluate potential risks to participants. The data monitoring committee provides regular reports to the trial steering committee detailing their findings and recommendations.
Patient and public involvement
There is no patient and public involvement.
Adverse event reporting and harms {22}
All AEs occurring during the study will be carefully recorded, including the worsening of original symptoms, the appearance of new symptoms or signs, the development of new diseases, and changes in laboratory parameters. In the interest of patients’ safety, any AEs will be addressed and resolved promptly. The research team will assess the causal relationship between the AEs and the intervention. AEs that result in death, life treat, prolonged hospital stay, or disability/incapacity will be reported as SAEs to the ethics committee within 24 h.
Frequency and plans for auditing trial conduct {23}
Regular audits will be conducted every 6 months. Additional audits may be conducted at any time if there are concerns about trial conduct, such as reports of protocol deviations or adverse events.
Plans for communicating important protocol amendments to relevant parties {25}
Trial participants will receive updated information sheets and consent forms explaining the amendments. If changes directly affect their involvement, they will be asked to reconfirm their consent. For significant changes, direct communication through meetings or phone calls will be arranged to ensure clear understanding.
Amendments of the protocol will be formally submitted by the PI to all participating centers and relevant ethical committees for review and approval. The submission will include a cover letter that outlines the changes, the rationale behind them, and their impact on the study. Implementation of changes will only occur after receiving approval from these committees. The revised protocol will be sent to the PI, who will ensure that a copy is added to the Investigator Site File at each participating center. Any deviations from the protocol will be fully documented using a breach report form. This form will detail the nature of the deviation, the reasons for it, and any corrective actions taken.
Dissemination plans {31a}
This clinical trial will be reported according to the CONSORT guidelines. We aim to publish a manuscript with the results in a peer-reviewed journal. Our goal is to disseminate the findings of this trial to the scientific community and contribute to the advancement of medical knowledge on treating refractory septic shock.
Trial status
The protocol version is Version 1.0, March 1st. The date recruitment began on April 19th, 2023. The approximate date when recruitment will be completed is June 30th, 2024.
Availability of data and materials {29}
Data will be uploaded to the ResMan website (www.medresman.org.cn). The final dataset will be kept confidential until the end of the trial. Any data required to support the protocol can be supplied on request. The public have access to the final trial dataset after the end of trial.
References
Evans L, Rhodes A, Alhazzani W, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063–143. https://doi.org/10.1097/CCM.0000000000005337.
Lei S, Li X, Zhao H, Xie Y, Li J. Prevalence of sepsis among adults in China: a systematic review and meta-analysis. Front Public Health. 2022;10:977094. https://doi.org/10.3389/fpubh.2022.977094.
Bassi E, Park M, Azevedo LCP. Therapeutic strategies for high-dose vasopressor-dependent shock. Crit Care Res Pract. 2013;2013:654708. https://doi.org/10.1155/2013/654708.
Nandhabalan P, Ioannou N, Meadows C, Wyncoll D. Refractory septic shock: our pragmatic approach. Crit Care. 2018;22(1):215. https://doi.org/10.1186/s13054-018-2144-4.
Singer M. Catecholamine treatment for shock–equally good or bad? Lancet. 2007;370(9588):636–7. https://doi.org/10.1016/S0140-6736(07)61317-8.
Singer M, Matthay MA. Clinical review: Thinking outside the box–an iconoclastic view of current practice. Crit Care. 2011;15(4):225. https://doi.org/10.1186/cc10245.
Puntillo F, Giglio M, Pasqualucci A, Brienza N, Paladini A, Varrassi G. Vasopressor-sparing action of methylene blue in severe sepsis and shock: a narrative review. Adv Ther. 2020;37(9):3692–706. https://doi.org/10.1007/s12325-020-01422-x.
Jang DH, Nelson LS, Hoffman RS. Methylene blue in the treatment of refractory shock from an amlodipine overdose. Ann Emerg Med. 2011;58(6):565–7. https://doi.org/10.1016/j.annemergmed.2011.02.025.
Salaris SC, Babbs CF, Voorhees WD. Methylene blue as an inhibitor of superoxide generation by xanthine oxidase. A potential new drug for the attenuation of ischemia/reperfusion injury. Biochem Pharmacol. 1991;42(3):499–506. https://doi.org/10.1016/0006-2952(91)90311-r.
Keaney JF, Puyana JC, Francis S, Loscalzo JF, Stamler JS, Loscalzo J. Methylene blue reverses endotoxin-induced hypotension. Circ Res. 1994;74(6):1121–5. https://doi.org/10.1161/01.res.74.6.1121.
Kirov MY, Evgenov OV, Evgenov NV, et al. Infusion of methylene blue in human septic shock: a pilot, randomized, controlled study. Crit Care Med. 2001;29(10):1860–7. https://doi.org/10.1097/00003246-200110000-00002.
Park BK, Shim TS, Lim CM, et al. The effects of methylene blue on hemodynamic parameters and cytokine levels in refractory septic shock. Korean J Intern Med. 2005;20(2):123–8. https://doi.org/10.3904/kjim.2005.20.2.123.
Juffermans NP, Vervloet MG, Daemen-Gubbels CRG, Binnekade JM, de Jong M, Groeneveld ABJ. A dose-finding study of methylene blue to inhibit nitric oxide actions in the hemodynamics of human septic shock. Nitric Oxide. 2010;22(4):275–80. https://doi.org/10.1016/j.niox.2010.01.006.
Preiser JC, Lejeune P, Roman A, et al. Methylene blue administration in septic shock: a clinical trial. Crit Care Med. 1995;23(2):259–64. https://doi.org/10.1097/00003246-199502000-00010.
Ibarra-Estrada M, Kattan E, Aguilera-González P, et al. Early adjunctive methylene blue in patients with septic shock: a randomized controlled trial. Crit Care. 2023;27(1):110. https://doi.org/10.1186/s13054-023-04397-7.
Xiong X, Jin L, Wang L, Zhu T, Peng Y, Lin L. Effect of methylene blue on oxygen metabolism in patients with septic shock. Chin J Anesthesiol. Published online 2010:1239–1242.
Donati A, Conti G, Loggi S, et al. Does methylene blue administration to septic shock patients affect vascular permeability and blood volume? Crit Care Med. 2002;30(10):2271–7. https://doi.org/10.1097/00003246-200210000-00015.
Lu Y, Yu H, Liu Q, Yao M, Zhu J. Efficacy of methylene blue continuous intravenous infusion in patients with septic shock. Natl Med J China. 2019;99(11):868–71. https://doi.org/10.3760/cma.j.issn.0376-2491.2019.11.015.
Memis D, Karamanlioglu B, Yuksel M, Gemlik I, Pamukcu Z. The influence of methylene blue infusion on cytokine levels during severe sepsis. Anaesth Intensive Care. 2002;30(6):755–62. https://doi.org/10.1177/0310057X0203000606.
Chan AW, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200–7. https://doi.org/10.7326/0003-4819-158-3-201302050-00583.
Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. https://doi.org/10.1136/bmj.c332.
Acknowledgements
We would like to express our gratitude to Medical Intensive Care Unit in General Hospital of Southern Theater Command for providing the necessary infrastructure and resources for this research.
Funding
This work was self-funded.
Author information
Authors and Affiliations
Contributions
JJ and ZL conceived and designed the initial trial concept. JJ developed the trial design and wrote the protocol. JJ contributed to the development of the trial design, provided important intellectual content, and critically revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate {24}
The study has been approved by the Ethics Committee of General Hospital of Southern Theatre Command. The approval number is NZLLKZ2022183. Written, informed consent to participate will be obtained from all participants.
Consent for publication {32}
We are willing to provide a model consent form and other related documentation on request.
Competing interests {28}
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jia, J., Ji, J. & Liu, Z. Efficacy of methylene blue in refractory septic shock: study protocol for a multicenter, randomized, placebo-controlled trial. Trials 25, 630 (2024). https://doi.org/10.1186/s13063-024-08439-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-024-08439-5