Abstract
Background
Prevention of multi-morbidities following non-communicable diseases requires a systematic registration of adverse modifiable risk factors, including low physical fitness. The aim of the study was to establish criterion validity and reliability of a smartphone app (InterWalk) delivered fitness test in patients with type 2 diabetes.
Methods
Patients with type 2 diabetes (N = 27, mean (SD) age 64.2 (5.9) years, BMI 30.0 (5.1) kg/m2, (30 % male)) completed a 7-min progressive walking protocol twice (with and without encouragement). VO2 during the test was assessed using indirect calorimetry and the acceleration (vector magnitude) from the smartphone was obtained. The vector magnitude was used to predict VO2peak along with the co-variates weight, height and sex. The validity of the algorithm was tested when the smartphone was placed in the right pocket of the pants or jacket. The algorithm was validated using leave-one-out cross validation. Test-retest reliability was tested in a subset of participants (N = 10).
Results
The overall VO2peak prediction of the algorithm (R2) was 0.60 and 0.45 when the smartphone was placed in the pockets of the pants and jacket, respectively (p < 0.001). The mean bias (limits of agreement) in the cross validation was−0.4 (38) % (pants) and−0.1 (46) % (jacket). When the smartphone was placed in the jacket a significant intensity dependent bias (r = 0.5, p = 0.02) was observed. The test-retest intraclass correlations were 0.85 and 0.86 (p < 0.001), for the pants and jacket, respectively. No effects of encouragement were observed on test performance.
Conclusion
In conclusion, the InterWalk Fitness Test is accurate and reliable for persons with type 2 diabetes when the smartphone is placed in the side pocket of the pants for. The test could give a fair estimate of the CRF in absence of a progressive maximal test during standardized conditions with the appropriate equipment.
Trial registration
www.clinicaltrials.org (NCT02089477), first registered (prospectively) on March 14th 2014
Similar content being viewed by others
Background
Type 2 diabetes (T2D), along with a range of non-communicable diseases, has become an increasing societal burden [1–3]. Low cardiorespiratory fitness (CRF) is a marker of low health-related physical activity [4, 5] and an independent predictor of some of these non-communicable diseases including T2D and all-cause mortality [6–8]. Modifiable risk factors, such as low CRF, should be identified and targeted in order to implement strategies to prevent the development and consequences of these diseases. CRF is normally assessed in the laboratory by a comprehensive exercise test with expensive equipment, administered by trained test personnel and with the requirement of maximal effort from the participants. Hence, this procedure is not appropriate and feasible in populations selected for large scale testing. A number of field-applicable walking/running-based test protocols have been developed and tested [9]. Although criterion validity has been established for these protocols, they still require the presence of test personal, standardized surroundings, post processing and reporting of test results which makes them difficult to apply in large-scale testing and monitoring within clinical care and rehabilitation. Thus, novel low cost and valid methods to assess VO2peak can improve the detection of people at risk and increase the use of VO2peak as a risk stratification tool.
On-board movement sensors on smartphones allow for registration of exercise intensity. With the increasing use of smartphones, this platform might thus be a feasible tool for estimating CRF on a larger scale. Since new more feasible test for large scale testing and monitoring are needed we developed a smartphone delivered progressive walking CRF test for persons with T2D, as walking is considered safe and feasible, not least for the elderly population [10].
The aim of the study was to establish criterion validity and test-retest reliability of a 7-min progressive sub-maximal CRF test delivered by the smartphone app InterWalk. Secondarily, we aimed to examine the importance of the body location of the smartphone (the side pocket of the pants or jacket), and of therapist encouragement during the test on test performance.
Methods
Study sample
The present article describes a validation study that is a subset of a trial investigating the effect of SMS-prompting on the adherence to IWT (NCT02089477). Participants were recruited using bulletins. Potential participants contacted the project employees by telephone and were orally informed about the study. If no exclusion criteria (see below) were identified through the telephone interview, written material and consent form was mailed to the participant and participants was offered an information meeting. Interested participants screened by telephone was examined at a pre-examination and further informed about the study.
The inclusion criteria were; confirmed T2D diagnose (fasting glucose ≥7.0 mmol/L, random measured glucose ≥11.1 mmol/L, 2 h oral glucose tolerance test glucose ≥11,1 mmol/L or HbA1c > 48 mmol/mol), age˃30 years and BMI ˃18 but ˂40. Exclusion criteria included pregnancy, insulin dependence, contraindications to physical activity and any evidence of thyroid, liver, lung, heart or kidney disease [11]. Training status was not an in or exclusion criteria, however participant included were characterized with low physical fitness (VO2max/kg = 23,3 (±4,6) ml O2/kg/min) [12]. The sample for this validation study constitutes of participants with available data on VO2peak and smartphone sample accelerometer data. No formal sample size calculation was therefore performed. The participants had either no or 3 months’ experience with the InterWalk app. Participants received oral and written information about the study and informed consent was obtained from all participants. The study is approved by the Regional Ethics Committee of the Capital Region of Denmark (H-1-2013-116).
The Inter Walk app
The development of the InterWalk app and the background for development has been described in details elsewhere [13]. Briefly, the InterWalk app was developed as a vehicle to deliver interval walking training (IWT) for persons with T2D. The intensities during IWT are individualized based on the InterWalk Fitness Test (IWFT)-a standardized 7-min progressive walking test protocol (see below). During IWT and IWFT, on-board accelerometer data are sampled (100 Hz). The vector magnitude (VM) is calculated as the square root of the summed squared acceleration from the x, y and z axes. Subsequently, the data are averaged across 30 s. The data are transmitted to the server through Wi-fi or the mobile data network along with user demographics and central personal registration number [14].
Procedures
Indirect calorimetry (described below) was used as the criterion measure to validate the prediction of VO2peak from the accelerometer data obtained during the IWFT along with other co-variates. To establish test-retest reliability, the IWFT was repeated after 1 week in a subset of the participants (N = 10). Prior to testing, all participants underwent a medical screening including a health status interview and a physical exam, and demographic information was obtained.
The Inter Walk Fitness test (IWFT)
The IWFT protocol consists of 2 minutes of slow, followed by 2 minutes of intermediate, 2 minutes fast and 1 minute of very fast walking. The walking intensities are self-selected, thus what “slow walking”, “fast walking” etc. means is defined by the user. The test protocol is audio guided through earphones. Hence, the app automatically instructs the user to start and change the walking intensities as described above.
After a thorough introduction to the test procedures and the InterWalk app, the participants completed two IWFTs during each visit (see below). The tests were administered by smartphones (Iphone 5C, IOS 7, v 1.18.8/2.0, Apple inc). All IWFTs were performed outside on a standardized course. The course was selected to reflect a free-living situation; i.e. the tests were performed on a side-walk near a major road (incl. traffic noise and other pedestrians) with turns and varying surface.
The first IWFT was self-administered with self-selected pace, performed only by the auditory instructions from the InterWalk app. The second test was conducted with self-selected pace by instruction from the InterWalk app along with verbal encouragement from the examiner to increase the subjects’ walking intensity during the last minute of the test. At both IWFTs the smartphones were placed in the right side pocket of the pants (lower position; LP) and in the right side pocket of the jacket (upper position; UP) (Fig. 1). A resting period of >20 min was employed between the two tests.
Measurement of peak (VO2peak) and maximal oxygen consumption (VO2max)
VO2peak was assessed during both IWTF procedures using indirect calorimetry (Cosmed K4b2, Cosmed, Italy) as indirect calorimetry is considered the gold standard in assessing VO2 in a clinical setting [15]. The device is a lightweight portable system calculating oxygen uptake from breath by breath measurements described in detail elsewhere [16] and has previously been validated [17]. The system was calibrated according to the manufacturer description. VO2peak was defined as the mean oxygen consumption (ml O2) during the last 30 s of the protocol.
VO2max was assessed by a graded walking test protocol on treadmill (Technogym Runrace, Gambettola, Italy). Since the majority of the participants don’t have the capacity to run, the walking test protocol was chosen. This test has previously been used successfully in our laboratory [18]. The participants were allowed to select their own comfortable walking speed ranging from 1.6 to 4.8 km/h at a 1 % incline during a 6-min warm-up. The warm-up was followed by 2 min intervals of increasing inclines (2 % per stage) at individually determined brisk walking, ranging from 2.2 to 5.5 km/h until two of the three following criteria were met: plateauing of VO2 with incremental workloads and/or respiratory exchange ratio˃1,0 and/or at exhaustion (as assessed by the examiner). Oxygen consumption was assessed using continuous indirect calorimetric measurements (CPET, Cosmed, Italy).
Anthropometry
Height and weight were determined using standard procedures. Height was measured barefooted to the nearest 0.1 cm by a stadiometer (The Leichester Height Measure, Tanita). The weight was assessed during dual-energy X-ray absorptiometry scan (Lunar Prodigy Advance; GE Healthcare, Madison, WI).
Prediction of VO2peak during the IWFT
Tri-axial accelerometry has previously shown to predict energy expenditure (EE) during walking when the monitor was attached to the body [19–22]. Thus, the on-board accelerometer of the smartphone was used as predictor of VO2peak during the IWFT. The remaining predictor variables were chosen a priory. As EE increases during walking with higher body weight and height, these parameters were included as co-variates in the prediction model along with sex [23]. We chose not to include other predictor variables due to consideration of feasibility, as the users of the InterWalk app provide this information during set up of the InterWalk app [13]. As the relationship between VO2 and acceleration has previously been shown to be linear during walking [19–22], we chose to build our prediction model using a linear regression model as described below;
Where Yi is VO2peak (ml/min) during the last 30 s. of the test, Xi1 is the mean VM (g) during the last 30 s of the test, Xi2 is the body weight, Xi3 is the body height (cm), Xi4 is a sex indicator (0 for women, 1 for men) and εi is the error term. Standard linear regression diagnostics, including examining linearity, homoscedasticity, multi-collinearity and normal distribution of the residuals were performed. No indications of violations of the linear regression assumptions of the prediction equations were observed.
Statistical analyses
To established criterion validity we correlated the product–moment correlation coefficient (r) between the VM and oxygen consumption [24]. In order to obtain an un-biased estimate of the precision and accuracy of the predicted VO2peak, we calculated the predicted VO2peak using the leave-one-out cross validation (LOOCV). Agreement between the predicted values from the LOOCV and the observed values are evaluated using Bland-Altman plots with mean bias and limits of agreement (LOA) [25].
Reproducibility (test-rest) was expressed as the intraclass correlation coefficient (ICC) of the predicted values across 1 week. The interpretation of the reproducibility was based on the size of the ICC and classified as good to excellent (1.00–0.76), fair to good (0.75–0.41) and poor (0.41–0.00) [26]. Furthermore, we calculated the minimal detectable change (MDC) not due to measurement error of the predicted VO2peak. The MDC was calculated as 1.96*√2*(Standard deviationMD (1week follow-up and baseline)/√2) [27, 28]. All analyses were performed using STATA IC 13.1 (Stata Corp, Texas, USA). Statistical significance was set at α˂ 0,05 (two tailed).
Results
Sample characteristics
A total of 27 participants (31 % with previous InterWalk app experience) completed the protocol. Sample characteristics are described in Table 1. Participants with and without previous experience with the InterWalk app did not differ in VO2max and VO2peak. However, participants with previous experience were heavier (MD [95 % CI]) (12.1 kg [1.0;23.1]), had a higher BMI (4.1 [0.5;7.5]) kg/m2 and a higher HbA1c (ratio of geometric mean [95 % CI] 1.11 [1.08;1.16]). The participants reached (mean [95 % CI]) 85 % [79.0 to 90.0] of their VO2max during the IWFT.
Effects of encouragement and placement of the smartphone on VO2peak and vector magnitude
Table 2 describes the observed VO2peak and VM during the last 30 s of the 7-min IWFT. No difference in VO2peak was observed when the test was completed with encouragement compared with completion without encouragement (p = 0.70). Nor did the VM differ between tests (p = 0.40 and 0.12 for differences between encouragement and no encouragement, when the smartphone was placed in the LP and UP, respectively). However, a lower VM was observed when the smartphone was placed in the UP, compared to the LP, when the test was performed without (MD [95 % CI]) (−0.17 G [−0.22;−0.11]) as compared to encouragement (MD [95 % CI]) (−0.18 G [−0.23;−0.12]).
Accuracy and precision of the predicted VO2peak
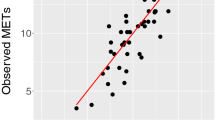
The correlations between VO2peak and VM during the last 30 s of the test for the LP and UP are depicted in Fig. 2. Data from the tests with and without encouragement were pooled as no differences between the r-values were observed between the LP (rencouragement [95 % CI] = 0.63 [0.33;0.82], rno encouragement [95 % CI] = 0.54 [0.20;0.76]) or the UP (rencouragement [95 % CI] = 0.31 [−0.08;0.63], rno encouragement [95 % CI] = 0.42 [0.05;0.70]). To account for the repeated measurements in the pooled analysis, we adjusted the standard errors for within-participant clustering (using VCE cluster option, Stata IC 13). The regression equation for prediction of VO2peak during the last 30 s. of the 7-min IWFT for the LP was described as;
The partial correlations between VO2peak and vector magnitude during the last 30 s of the test when the smartphone was placed in the lower position, smartphone placement in the right side pocket of the pants (Panel a) and in upper position, smartphone placement in the right side pocket of the jacket (Panel b). The dotted line is the best fit line. Triangles (▲) represent observations during the test with encouragement and crosses (X) are observations during the test without encouragement. The grey shaded area is the 95 % confidence interval
And for the UP as;
Figure 3 describes the accuracy and precision of the predictions algorithms for the LP (Fig. 3a) and for the UP (Fig. 3b) from the leave-one-out cross validation. The precision was [LOA ± 46.8 %] for the UP and [LOA ± 35.5 %] for the LP.
The accuracy (mean bias) and precision (±1.96 Standard deviation (SD)) of the VO2peak prediction algorithms for the lower (panel a) and the upper (panel b) position of the smartphone placement in the ‘leave-on-out cross validation’. The dotted line is the best fit line and represents the bias of the predicted values. Triangles (▲) represent the predicted values from the VM derived from the smartphone when placed in the upper position and crosses (X) are predicted values from the lower position
Reliability and the minimum detectable difference of the predicted VO2peak
The reliability (ICC [95 % CI)]) was 0.86 [0.64; 0.96] of the predicted VO2peak for the LP. For the UP the reliability (ICC [95 % CI)]) was 0.85 [0.60; 0.96]. The MDC was 298 ml O2 for the LP and 203 ml O2 for the UP.
Prediction of VO2max
The predicted VO2peak correlated with the measured VO2max (rLP = 0.70, p < 0.001 and rUP = 0.56, p = 0.004). The predicted VO2peak underestimated the VO2max by 15.5 % (p < 0.001) for the LP and 14.2 % (p < 0.001) for the UP. The mean bias [LOA] was 308 [215 to 401] ml O2 for the LP and 272 [118 to 427] ml O2 for the UP. The equations for both positions (LP and UP) underestimated the VO2max for participants with higher VO2max values and underestimated for the participants with lower values. The correlation between the bias and the mean of the VO2max and the VO2peak values was r = 0.36 (p < 0.01) for the LP and r = 0.46 (p < 0.02) for the UP.
Discussion
The aim of this study was to present a VO2peak protocol delivered by a smartphone app (InterWalk) and to establish criterion validity and test-retest reliability of a 7-min progressive fitness test. In addition we examined whether validity was influenced by the body location of the smartphone and if the test performance was affected by therapist encouragement. The accuracy and precision of the predicted VO2peak were dependent on body location, i.e. higher when the smartphone was placed in the LP. Furthermore, encouragement during the last minute of the test did not seem to affect test performance in this sample.
Differences between body locations
The VO2peak was predicted with a high accuracy for both body locations (LP and UP) along with comparable reliability. However, when the smartphone was placed in the UP, the VO2peak was overestimated at the higher intensities and underestimated at the lower intensities and the LOAs were wider. The partial correlation coefficients revealed that the algorithm was less dependent on the only dynamic test parameter in the algorithm (VM) for the UP compared to the LP and the recorded acceleration was generally lower. This would make the prediction algorithm less sensitive to variation herein. Differences in the validity for predicting VO2 between the placements of the accelerometer-based physical activity monitors are consistent with previous studies [29–31]. When the smartphone was placed in the UP, the accelerometer is closer to the centre of mass as observed when accelerometers are fixed on the hip or lower back. In contrast to the use of research physical activity monitors, the type of jackets, worn by the participants in the present study, was not standardized. Thus, some participants wore loosely fitted jackets and others wore jackets more closely attached to the body, all with different size pockets. The lower accuracy and higher variation of the IWFT when the smartphone was placed in the UP, might be due to movements of the jacket not corresponding to the actual movement of the body and therefore induce measurement error. When the smartphone was placed in the LP the accelerometer where close to the thigh/hip following the movement of the leg during walking closely and thus, the measurement error would be lower, explaining the narrower LOA for the LP. As the acceleration is the only body movement intensity-dependent variable in the equation, it could be speculated that the underestimation at higher VO2peak values is due to low sensitivity to capture the body acceleration. If increases in the observed acceleration on the smartphone either do not reflect or underestimate the concomitant acceleration in body, i.e. centre of mass, an underestimation would be observed at higher intensities. However, we did not measure the actual acceleration of the body during this study. The acceleration signal was un-filtered, i.e. all movement frequencies of the smartphone were included. The VM used in the IWFT was calculated as an average across a 30 s. epoch, and thus would suppress high frequency noise components to some extent. It is possible that high and low frequency acceleration components, not related to body movement per se, could explain the low precision of the estimates across both body locations.
Several field-based walking tests have been developed and validated. In a recent meta-analysis Mayorga-Vega et al. (2016) reported low-to-moderate (r = 0.42–0.79) criterion-related validity for walk/run field tests to estimate VO2max across 123 studies [9]. This is comparable to the IWFT, when the smartphone was placed in the LP. However, the studies reported on did not include patients. When compared to the criterion validity for the commonly used six minute walking test (6MWT) in patient groups characterized with low VO2peak, the criterion-related validity was slightly better for the IWFT [32, 33].
Clinical feasibility
The performance during field-based walking tests may be affected by encouragement from test personnel, increasing the resources needed to implement them in clinical care. [33, 34]. Differences in walking distance have been observed in elderly people [32, 33, 35] and in patients with pulmonary limitations [36, 37] when the 6MWT is performed repeatedly. No differences in VO2peak were observed, neither when the IWFT was performed self-conducted, nor with encouragement during the test. In view of the similar performance with and without encouragement and the high reproducibility (ICC; LP 0.86 and UP 0.85), the IWFT can be performed without the presence of professional test personnel, which will increase feasibility of the test in clinical and rehabilitation programs. Moreover, the high reliability indicates that the test has a very high consistency across from one test administration to the next [38], making it feasible to implement. The MDC not due to measurement error indicates the sensibility of the measurement to detect a change in the parameter of interest. Thus, the MDC indicates that the IWFT is able to detect changes in VO2 larger than ±18 % and ±13 % for the LP and UP, respectively. The exercise-induced magnitude of improvements in fitness level is related to the initial fitness level. Thus, only small changes (~5%) in CRF are observed in well trained individual (VO2max ≥ 3500 ml O2/min) with training programs of high intensity [39, 40]. In contrast high intensity exercise interventions in T2D patients with low initial VO2max have shown larger improvements in CRF. For example, improvements in CRF of 16-25 % were observed after 5 months of IWT [18, 41] and improvements of the same magnitude (18–46 %) were demonstrated in other patient groups undergoing high intensity exercise interventions [42, 43]. Therefore, the IWFT could be used as a tool to evaluate these types of exercise programs.
We performed a post hoc analysis to assess the relative validity [38]. The sensitivity and specificity of the predicted VO2peak values to classify the participants into low/intermediate and high risk as compared to the observed VO2peak values were thus calculated. The cut off values were based on reference values published by Kodoma et al. [8]. High risk participants were characterized with a VO2peak <7.9 metabolic equivalents. The sensitivity was 98 % and 94 % for the LP and UP, respectively. The specificity was 77 % for both positions. Thus, to stratify individuals at risk, the post hoc analysis indicated a similar performance across body locations. However, the sample was very homogenous and characterized by poor fitness as compared to the normal population [12]. In view of the small sample size, the interpretation of the relative validity should thus be done with caution.
Strengths and limitations
The main strengths of the study include the direct measurement of VO2peak, the well-characterized sample and an objective indirect measure of intensity. The validity and reliability of the IWFT were furthermore tested in a non-laboratory condition, increasing feasibility of usage in clinical care and rehabilitation without access to a laboratory. Finally, the independence of therapist encouragement on test performance enables patients to perform the test by themselves. With the online data upload the patients’ performance can be monitored over the distance, enabling use in large scale health surveillance programs as well as decreasing the workload of clinicians and therapists.
Some limitations to the study need to be addressed. First, the homogeneity of the sample and the relatively small sample size could limit the generalizability of the findings. However, the cross-validation demonstrated high accuracy and reliability of the equations. Therefore, we are confident that the equations can be employed in other populations with similar characteristics without loss of accuracy. Furthermore, we did not base the sample size on a formal sample size calculation, thus the study might have been under powered to detect statistically significant differences between the predicted and measured VO2peak values. However, the difference was very low (<10 ml O2*min−1), and within the measurement error of the criterion measure Cosmed K4b2 (Cosmed, Italy) [16]. Second, the estimation of VO2 with accelerometers used during incline walking is not accurate [44]. The IWFT was performed on level surface, thus limiting the performance of the equations to surfaces without incline. Third, many studies do indeed observe an association between e.g. VO2max rather than VO2peak [8] as predicted by our equations. However, this association is still present when using VO2peak as a predictor [8]. Fourth, due to the short resting period (20 min) between the paced and non-paced protocol and the lack of a randomized order of the administration of the protocol, fatigue could have prohibited the participants to reach a higher VO2peak during the paced protocol. However, no difference in the RER-values was observed (mean difference [95 % CI] 0.02 [−0.03; 0.07], p = 0.44 between the paced and the non-paced protocols). Thus, we do not believe that the resting period and the lack of randomization explains the lack of effect of pacing the participants during the protocol. Fifth, the IWFT is a measure of VO2peak during walking and thus might not be feasible for exercise prescription for other exercise modalities.
Conclusion
In conclusion the IWFT is a valid and reliable tool in estimating VO2peak in persons with similar characteristics as this sample, i.e. patients with a low VO2max, during walking. The IWFT displays similar criterion validity as other commonly used field-based walking tests. In order to obtain the highest accuracy and precision, the smartphone should be placed in the side pocket of the pants. The fact that no effect of encouragement on test performance was observed with high reliability indicates that the IWFT is feasible for self-administration as well as for use in the clinic. With the automatic transmission of test results, the IWFT makes it possible to test large groups of people over distance in a time-saving and economical manner. The test could give a fair estimate of the CRF in absence of a progressive maximal test during standardized conditions with the appropriate equipment.
Abbreviations
- 6MWT:
-
6-min walking test
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- Cm:
-
Centimeter
- CRF:
-
Cardio respiratory fitness
- EE:
-
Energy expenditure
- HbA1c:
-
Glycolated haemoglobin 1 ac
- ICC:
-
Intra class correlation
- IWFT:
-
InterWalk fitness test
- IWT:
-
Interval walking training
- Kg:
-
Kilogram
- LOA:
-
Limits of agreement
- LOOCV:
-
Leave one out cross validation
- LP:
-
Lower position
- MD:
-
Mean difference
- MDC:
-
Minimal detectable difference
- T2D:
-
Type 2 diabetes
- UP:
-
Upper position
- VM:
-
Vector magnitude
References
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14.
Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–223.
De Cock KM, Simone PM, Davison V, Slutsker L. The new global health. Emerg Infect Dis. 2013;19:1192–7.
Aadahl M, Kjaer M, Kristensen JH, Mollerup B, Jorgensen T. Self-reported physical activity compared with maximal oxygen uptake in adults. Eur J Cardiovasc Prev Rehabil. 2007;14:422–8.
Garber CE, Blissmer B, Deschenes MR, Franklin BA, LaMonte MJ, Lee IM, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–59.
Gulati M, Black HR, Shaw LJ, Arnsdorf MF, Merz CN, Lauer MS, et al. The prognostic value of a nomogram for exercise capacity in women. N Engl J Med. 2005;353:468–75.
Hainer V, Toplak H, Stich V. Fat or fit: what is more important? Diabetes Care. 2009;32 Suppl 2:S392–7.
Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301:2024–35.
Mayorga-Vega D, Bocanegra-Parrilla R, Ornelas M, Viciana J. Criterion-Related Validity of the Distance-and Time-Based Walk/Run Field Tests for Estimating Cardiorespiratory Fitness: A Systematic Review and Meta-Analysis. PLoS ONE. 2016;11, e0151671.
Pollock ML, Carroll JF, Graves JE, Leggett SH, Braith RW, Limacher M, et al. Injuries and adherence to walk/jog and resistance training programs in the elderly. Med Sci Sports Exerc. 1991;23:1194–200.
Pedersen BK, Saltin B. Evidence for prescribing exercise as therapy in chronic disease. Scand J Med Sci Sports. 2006;16 Suppl 1:3–63.
Edvardsen E, Scient C, Hansen BH, Holme IM, Dyrstad SM, Anderssen SA. Reference values for cardiorespiratory response and fitness on the treadmill in a 20–to 85–year-old population. Chest. 2013;144:241–8.
Ried-Larsen M, Thomsen RW, Berencsi K, Brinkløv CF, Brøns C, Valentiner L, et al. Implementation of interval walking training in patients with Type 2 diabetes in Denmark; Rationale, design and baseline characteristics. In: Clinical Epidemiology. 2015.
Frank L. Epidemiology. When an entire country is a cohort. Science. 2000;287:2398–9.
Haugen HA, Chan LN, Li F. Indirect calorimetry: a practical guide for clinicians. Nutr Clin Pract. 2007;22:377–88.
Pinnington HC, Wong P, Tay J, Green D, Dawson B. The level of accuracy and agreement in measures of FEO2, FECO2 and VE between the Cosmed K4b2 portable, respiratory gas analysis system and a metabolic cart. J Sci Med Sport. 2001;4:324–35.
Hausswirth C, Bigard AX, Le Chevalier JM. The Cosmed K4 telemetry system as an accurate device for oxygen uptake measurements during exercise. Int J Sports Med. 1997;18:449–53.
Karstoft K, Winding K, Knudsen SH, Nielsen JS, Thomsen C, Pedersen BK, et al. The effects of free-living interval-walking training on glycemic control, body composition, and physical fitness in type 2 diabetic patients: a randomized, controlled trial. Diabetes Care. 2013;36:228–36.
Brage S, Wedderkopp N, Franks PW, Andersen LB, Froberg K. Reexamination of validity and reliability of the CSA monitor in walking and running. Med Sci Sports Exerc. 2003;35:1447–54.
Vaha-Ypya H, Vasankari T, Husu P, Manttari A, Vuorimaa T, Suni J, et al. Validation of Cut-Points for Evaluating the Intensity of Physical Activity with Accelerometry-Based Mean Amplitude Deviation (MAD). PLoS ONE. 2015;10, e0134813.
Vaha-Ypya H, Vasankari T, Husu P, Suni J, Sievanen H. A universal, accurate intensity-based classification of different physical activities using raw data of accelerometer. Clin Physiol Funct Imaging. 2015;35:64–70.
Yamazaki T, Gen-No H, Kamijo Y, Okazaki K, Masuki S, Nose H. A new device to estimate VO2 during incline walking by accelerometry and barometry. Med Sci Sports Exerc. 2009;41:2213–9.
Bouchard C, Daw EW, Rice T, Perusse L, Gagnon J, Province MA, et al. Familial resemblance for VO2max in the sedentary state: the HERITAGE family study. Med Sci Sports Exerc. 1998;30:252–8.
Lee I-M, Blair S, Manson J, Paffenberger RS. Establishing Validity and Reliability of Physical Activity. In: Epidemiological methods in physical activity studies. 1st ed. Oxford: Oxford University Press; 2009. p. 34–55.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Fleiss JL. The Design and Analysis of Clinical Experiments. New York: John Wiley & Sons, Inc; 1986.
Jorgensen R, Ris I, Falla D, Juul-Kristensen B. Reliability, construct and discriminative validity of clinical testing in subjects with and without chronic neck pain. BMC Musculoskelet Disord. 2014;15:408.
De Vet HC, Terwee CB, Knol DL, Bouter LM. When to use agreement versus reliability measures. J Clin Epidemiol. 2006;59:1033–9.
Kim DY, Jung YS, Park RW, Joo NS. Different location of triaxial accelerometer and different energy expenditures. Yonsei Med J. 2014;55:1145–51.
Swartz AM, Strath SJ, Bassett Jr DR, O’Brien WL, King GA, Ainsworth BE. Estimation of energy expenditure using CSA accelerometers at hip and wrist sites. Med Sci Sports Exerc. 2000;32:S450–6.
Yngve A, Nilsson A, Sjostrom M, Ekelund U. Effect of monitor placement and of activity setting on the MTI accelerometer output. Med Sci Sports Exerc. 2003;35:320–6.
Kervio G, Carre F, Ville NS. Reliability and intensity of the 6-min walk test in healthy elderly subjects. Med Sci Sports Exerc. 2003;35:169–74.
Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, et al. The 6-min walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–23.
Aadahl M, Zacho M, Linneberg A, Thuesen BH, Jorgensen T. Comparison of the Danish step test and the watt-max test for estimation of maximal oxygen uptake: the Health2008 study. Eur J Prev Cardiol. 2013;20:1088–94.
Troosters T, Gosselink R, Decramer M. Six minute walking distance in healthy elderly subjects. Eur Respir J. 1999;14:270–4.
Jenkins S, Cecins NM. Six-minute walk test in pulmonary rehabilitation: do all patients need a practice test? Respirology. 2010;15:1192–6.
Osadnik CR, Borges RC, McDonald CF, Carvalho CR, Holland AE. Two 6-minute Walk Tests Are Required during Hospitalisation for Acute Exacerbation of COPD. COPD. 2015;7:1–5.
Kelly P, Fitzsimons C, Baker G. Should we reframe how we think about physical activity and sedentary behaviour measurement? Validity and reliability reconsidered. Int J Behav Nutr Phys Act. 2016;13:32.
Billat V, Demarle A, Paiva M, Koralsztein JP. Effect of training on the physiological factors of performance in elite marathon runners (males and females). Int J Sports Med. 2002;23:336–41.
Breil FA, Weber SN, Koller S, Hoppeler H, Vogt M. Block training periodization in alpine skiing: effects of 11-day HIT on VO2max and performance. Eur J Appl Physiol. 2010;109:1077–86.
Jakicic JM, Jaramillo SA, Balasubramanyam A, Bancroft B, Curtis JM, Mathews A, et al. Effect of a lifestyle intervention on change in cardiorespiratory fitness in adults with type 2 diabetes: results from the Look AHEAD Study. Int J Obes (Lond). 2009;33:305–16.
Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115:3086–94.
Rognmo O, Hetland E, Helgerud J, Hoff J, Slordahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil. 2004;11:216–22.
Terrier P, Aminian K, Schutz Y. Can accelerometry accurately predict the energy cost of uphill/downhill walking? Ergonomics. 2001;44:48–62.
Acknowledgements
The authors would like to thank the participants for their time. We would furthermore like to acknowledge the foundations supporting the work. The study is part of the DD2, acronym for ‘The Danish Centre for Strategic Research in Type 2 Diabetes’ that is supported by grants from The Danish Strategic Research Council (grant no. 09–067009 and 09–075724). DD2 funding and partners are listed at www.dd2.nu. The Centre for Physical Activity Research (CFAS) is supported by a grant from Trygfonden. The CopenRehab is supported by a grant from the Municipality of Copenhagen. Furthermore, this study is supported by a postdoc grant from The Danish Diabetes Academy (supported by the Novo Nordic Foundation) and grants from the Augustinus Foundation, Fonden for Lægevidenskabens fremme and Viggo og Krista Pedersens Foundation. Finally, the authors would like to thank Prof. Lars Bo Andersen for his valuable input to the data analysis and interpretation.
Availability of data and materials
Data and materials are available upon request. Please contact the corresponding author.
Authors’ contributions
All authors made substantial contributions to study conception and design and revised the manuscript critically for important intellectual content and have given their final approval of the manuscript to be published. CFB and MR-L drafted the manuscript. CFB, IKT and MR-L collected and processed the data. MR-L performed the statistical analyses. CFB and MR-L had full access to all data and takes the full responsibility for data integrity. All read and approved the final manuscript.
Competing interests
The authors declare no competing interests.
Consent for publication
Consent to publish the image (Fig. 1) was obtained prior to submission.
Ethics approval and consent to participate
Participants received oral and written information about the study and informed consent was obtained from all participants. The study is approved by the Regional Ethics Committee of the Capital Region of Denmark (H-1-2013-116).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Brinkløv, C.F., Thorsen, I.K., Karstoft, K. et al. Criterion validity and reliability of a smartphone delivered sub-maximal fitness test for people with type 2 diabetes. BMC Sports Sci Med Rehabil 8, 31 (2016). https://doi.org/10.1186/s13102-016-0056-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-016-0056-7