Abstract
Background
Hydatid disease, also known as echinococcosis, is a zoonotic parasitic infection caused by the larvae of the Echinococcus tapeworm. It is endemic in various regions worldwide, particularly in rural areas of countries in southern South America, Central Asia, China, parts of Africa, the Mediterranean, and parts of the Middle East. The disease primarily affects the liver (60–70% of cases) and the lungs (10–25% of cases), but it can involve any organ, including the brain, bones, and rarely the pelvic region, as seen in our case report. Hydatid disease typically follows an asymptomatic course in the early stages of the primary infection and may remain so potentially for years or even permanently. If symptoms occur, they depend on various factors, such as the number, size, and location among other factors. Typically, hydatid disease presents with nonspecific symptoms. Common symptoms include abdominal pain, hepatomegaly, as well as anaphylaxis in case of cyst rupture. Extrahepatic intra-abdominal isolated hydatic cyst is a rare finding (6–11%).
Case presentation
In our case, a 70 year-old Asian white male presented with right thigh pain radiating to the lower leg, which is an atypical presentation for an extrahepatic intraabdominal hydatid cyst. Primary intraabdominal hydatid cysts involving the pelvic region are relatively rare, and such cases pose diagnostic and management challenges.
Conclusion
This case report underscores the challenges in diagnosing and managing extrahepatic intraabdominal hydatid cysts, particularly in atypical presentations. A combination of clinical evaluation, serological studies, and imaging techniques facilitates accurate diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Hydatid disease is a parasitic infection caused by the larval stage of the Echinococcus genus. The cystic form of the disease is most commonly caused by the Echinococcus granulosus tapeworm, which infects humans as an accidental intermediate host in its lifecycle. In the lifecycle, canines serve as definitive hosts while ungulates act as intermediate hosts. Definitive hosts become infected by ingesting contaminated meat and shed eggs or gravid proglottids in feces. Intermediate hosts are infected through oral uptake of these eggs, which release larvae in the small intestine and can be transported to various organs, including the liver and lungs. Humans are often infected as intermediate hosts owing to exposure to unwashed vegetables, infected animals, or contaminated soil [1, 2]. Cystic hydatid disease exhibits a global distribution with a prevalence of 1–200/100,000; however, it is endemic in specific regions including South and Central America, the Middle East, and Mediterranean Countries, as well as certain sub-Saharan African countries. Although the disease can potentially manifest in any part of the body, it is predominantly observed in the liver (52–77% of cases) followed by the lungs (10–40%) [1,2,3]. Although rare, isolated extrahepatic intra-abdominal cysts can occur, but extrahepatic intra-abdominal cystic disease commonly coexists with hepatic involvement [2].
The purpose of this case report is to highlight the uncommon occurrence of isolated hydatid cysts in the right pelvic cavity. This rare presentation of the disease warrants consideration of a wide range of differential diagnoses and necessitates exploration of multiple treatment options for managing this potentially life-threatening condition.
Case presentation
A 70 year-old Asian white man presented to the hospital for right thigh pain radiating to the lower leg. The patient was in pain for 1 month and was unable to walk. His past medical history is confined to controlled hypothyroidism with no past surgical history. He is a nonsmoker, nonalcoholic, and denied any drug abuse.
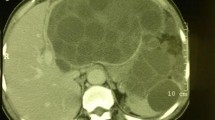
On physical examination the patient was alert, conscious, and oriented. The patient had a regular heartbeat, good bilateral airway entry, and soft abdomen. The physical examination was insignificant except for a right thigh tenderness and a decrease range of motion. Vital signs were within the normal range. The computed tomography (CT) scan showed a large multi-loculated complex cystic lesion on the right pelvic cavity measuring 14 × 10 cm with multiple thick septae [Figure. 1]. The cysts have induced a remodeling of the subjacent right iliac and acetabular bones [Figure. 2]. It was attached to the right iliopsoas muscle. The cyst was extending to the level of the anorectal junction and involving the obturator internus muscle. The large mass was compressing the bladder and the rectosigmoid colon. Laboratory tests showed high anti-echinococcus-HAI level (1/2560), normocytic anemia: (HG: 0.8.4 g/dl, HCT: 25%), and eosinophilia (6%). The diagnosis of hydatid cyst stage CE3B (Gharbi classification) was confirmed. CT-scan of the head and chest was done to rule out the spread of cysts. Albendazole per Oz for 2 weeks was ordered followed by hydatid cyst removal under general anesthesia. An anterior approach with vertical incision from the xiphoid to the umbilicus was made, for optimal exposure and control given the complex and extensive nature of the lesion. The cyst was identified, and the surrounding tissues were covered with cetrimide-soaked pads. Cetrimide (a scolocidal agent) was injected in the cyst cavity and allowed to sit for 10 min, after which it was evacuated, and the cavity was irrigated with isotonic sodium chloride solution. The cyst was then evacuated using a strong suction device, and cetrimide was injected again into the cavity [Figure. 3]. After the second injection of cetrimide, the patient experienced bradycardia (20 heartbeats per minute) and hypotension. The patient was in anaphylactic shock. Surgery was paused and advanced cardiac life support (ACLS) treatment was started. After eight cycles of cardiac massage with the injection of atropine, adrenaline, sodium bicarbonate, and hydrocortisone, the patient resumed his cardiac function but with undetectable arterial pressure. Noradrenaline was started. Then, surgery was resumed rapidly where the cyst was removed, and part of the greater omentum was used to fill the defect (omentoplasty). The Patient was then transferred to the intensive care unit (ICU). In the ICU, the patient still had no detectable blood pressure, although the maximum dose of noradrenaline was given. After about 5 hours, owing to anaphylactic shock, the patient had a cardiac arrest and passed away.
Discussion
Hydatid disease is a parasitic infection caused by the larval stage of the Echinococcus genus. It is endemic in various regions worldwide, particularly in rural areas of countries in southern South America, Central Asia, China, parts of Africa, the Mediterranean, and parts of the Middle East [4]. The disease primarily affects the liver (60–70% of cases) and the lungs (10–25% of cases) [5], but it can involve any organ, including the brain, bones, and rarely, the pelvic region, as seen in our case report [4]. Extra-hepatic intra-abdominal isolated hydatic cyst is a rare finding (6–11%) [5]. It typically follows an asymptomatic course in the early stages of the primary infection and may remain so potentially for years or even permanently. If symptoms were to occur, they would depend on various factors such as the number, size, and location among other factors [6]. Typically, hydatid disease presents with non-specific symptoms. Common symptoms include abdominal pain, hepatomegaly, as well as anaphylaxis in case of cyst rupture [7].
In our case, a 70-year-old man with no significant medical history except controlled hypothyroidism presented with severe right thigh pain, decreased range of motion, and an inability to walk. The CT scan revealed a large multiloculated complex cystic lesion in the right pelvic cavity, measuring 14 × 10 cm, with multiple thick septae. The cyst was attached to the iliopsoas muscle, extending to the anorectal junction, and involving the obturator internus muscle. This extensive involvement resulted in compression of the bladder and the rectosigmoid colon. Laboratory tests demonstrated elevated anti-Echinococcus-HAI levels, normocytic anemia, and eosinophilia, consistent with the diagnosis of hydatid cyst stage CE3B (Gharbi classification) [8, 9].
The diagnosis of hydatid disease relies on a combination of clinical evaluation, serological studies, and imaging techniques. Serological tests, such as enzyme-linked immunosorbent assay (ELISA) and indirect hemagglutination assay (IHA), measure specific antibodies against Echinococcus and can aid in the diagnosis; however, their role is less important than imaging owing to high false negative rates [10].
Imaging modalities, including ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), play a crucial role in the diagnosis and assessment of hydatid cysts. Ultrasound is often the initial imaging modality of choice owing to its widespread availability, cost-effectiveness, and ability to differentiate cystic from solid lesions. Ultrasound is also the gold standard for staging hydatid disease. [10]. On the other hand, computed tomography (CT) scans excel at identifying calcification and involvement of the bones, while MRI may be useful in cases where soft tissue involvement or spinal cord compression is suspected [11].
The management of extrahepatic intraabdominal hydatid disease involves a multidisciplinary approach, integrating medical treatment and surgical intervention. The mainstay of medical treatment is the administration of benzimidazole derivatives, such as albendazole, to reduce the risk of recurrence and systemic dissemination [12]. A typical regimen involves a preoperative course of 2 weeks to minimize the risk of anaphylactic reactions during surgery, followed by a postoperative course for several months with a minimum overall duration of treatment of 3 months [4].
Surgical intervention is essential for the definitive treatment of hydatid cysts [13]. The choice of surgical approach depends on the cyst’s location, size, and involvement of adjacent structures. Pericystectomy, cystectomy, and total organ resection are commonly employed techniques to achieve complete cyst removal while preserving organ function [13]. However, surgical treatment carries potential risks, including infection, cyst rupture, anaphylactic shock, and recurrence. Other modalities of proposed treatments may include percutaneous approaches, such as the PAIR technique, radiofrequency thermo-ablation, or some even proposed a conservative approach where we monitor the disease progression. It is vital to note that a newer approach has emerged in recent years in the form of percutaneous operations, most important of which is the puncture, aspiration, injection, respiration (PAIR) technique. In the PAIR technique, half of the cyst volume is aspirated, 20% hypertonic saline solution is injected as one third of the initial cyst volume. After 20 minutes, the cyst volume is aspirated again. It is merely used for type I and II cysts below the size of 6 cm. Additionally, it is not applicable for cysts that are calcific and solid (15–18). The cysts in type III and those bigger than 6 cm are treated with percutaneous drainage catheter administration [14,15,16].
There is no global gold standard of a go-to treatment for hydatid disease, but rather the treatment choice should be individualized to each case with a discussion of the treatment options available with the patient [12]. The extraperitoneal approach with partial cystectomy to avoid damage to nervous structures is recommended for primary intraabdominal extra-hepatic cysts of the abdomen that involve the psoas muscle [5].
In our case, an anterior approach with a vertical incision from the xiphoid to the umbilicus was made. The cyst was identified and surrounded by cetrimide-soaked pads to minimize the risk of cyst rupture. Cetrimide, a scolicidal agent, was injected into the cyst cavity, and after evacuation, the cavity was irrigated with isotonic sodium chloride solution. However, the patient experienced an anaphylactic shock following the second injection of cetrimide. Prompt management restored cardiac function, and the cyst was removed. The patient, unfortunately, suffered a cardiac arrest and passed away 3 hours after the procedure.
Cetrimide is a potent disinfectant and effective scolicidal agent used to sterilize the cyst and prevent intraoperative dissemination of its contents [17]. Numerous scolicidal agents with different concentrations have been proposed for treatment in literature, but no guidelines to date exist on the acceptable volume and concentration that can be used safely. The present uncertainties in the use of scolicides, the difficulty of accurately estimating the volume of the hydatid cyst in situ, urge upon the surgeon the employment of the most potent safe scolicide available [18]. Although cetrimide is effective in very low concentrations, it is not devoid of complications. Dreadful side effects have been reported in literature, including methemoglobinemia and deep cyanosis that may ensue [19], chemically induced peritonitis with massive adhesions and bowel obstruction postoperatively [20], increasingly severe metabolic acidosis that can lead to cardiovascular collapse with vasoplegic collapse, low central venous pressure, oliguria, and abdominal tension, all attributed to third spacing [21], convulsions, and coma.
The recurrence rate of hydatid disease varies depending on several factors, including cyst characteristics and the extent of surgical resection. Reported recurrence rates for intraabdominal hydatid cysts range from 2 to 30% [4]. Regular follow-up, including clinical evaluation and imaging, is crucial for the early detection of recurrence. The follow-up typically involves the use of imaging at 3 month intervals for 3 years at least to detect the recurrence of cysts with monitoring of cyst size among other cyst characteristics. [4]
Postoperative events following hydatid cyst surgery can include pain, wound infection, cystic fluid collection, and abscess formation. In our case, anaphylactic shock during surgery was the major complication encountered, which was appropriately managed. However, the subsequent cardiac arrest led to the patient’s unfortunate demise.
On the basis of our experience, future cases of extrahepatic intraabdominal hydatid cysts should maintain a high index of suspicion for the disease, even in the absence of typical symptoms. The risks and benefits of scolicidal agents, including cetrimide, should be carefully considered, and alternative agents or approaches should be explored to minimize the risk of anaphylactic reactions. A multidisciplinary approach involving infectious disease specialists, surgeons, anesthesiologists, and critical care teams remains crucial for optimal patient management.
Conclusion
In conclusion, this case report underscores the challenges in diagnosing and managing extrahepatic intraabdominal hydatid cysts, particularly in atypical presentations. A combination of clinical evaluation, serological studies, and imaging techniques facilitates accurate diagnosis. The treatment approach involves a multidisciplinary strategy with medical therapy and surgical intervention, aiming for complete cyst removal while minimizing complications. Further research is needed to refine diagnostic and therapeutic strategies, improve patient outcomes, and reduce the burden of this rare but significant disease.
Availability of data and materials
Not applicable yet until it gets published.
References
Nunnari G, Pinzone MR, Gruttadauria S, Celesia BM, Madeddu G, Malaguarnera G, Pavone P, Cappellani A, Cacopardo B. Hepatic echinococcosis: clinical and therapeutic aspects. World J Gastroenterol. 2012;18(13):1448–58. https://doi.org/10.3748/wjg.v18.i13.1448.
Sayek I, Tirnaksiz MB, Dogan R. Cystic hydatid disease: current trends in diagnosis and management. Surg Today. 2004;34(12):987–96. https://doi.org/10.1007/s00595-004-2830-5.
Ewnte B. Hydatid cyst of the foot: a case report. J Med Case Rep. 2020;14(1):6. https://doi.org/10.1186/s13256-019-2337-8.
Moro P, Schantz PM. Echinococcosis: a review. Int J Infect Dis. 2009;13(2):125–33. https://doi.org/10.1016/j.ijid.2008.03.037.
Makni A, Jouini M, Kacem M, Safta ZB. Extra-hepatic intra-abdominal hydatid cyst: which characteristic, compared to the hepatic location? Updates Surg. 2013;65(1):25–33. https://doi.org/10.1007/s13304-012-0188-6.
Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev. 2004;17(1):107–35. https://doi.org/10.1128/CMR.17.1.107-135.2004.
Ferrer Inaebnit E, Molina Romero FX, Segura Sampedro JJ, González Argenté X, MorónCanis JM. A review of the diagnosis and management of liver hydatid cyst. Rev Esp Enferm Dig. 2022;114(1):35–41. https://doi.org/10.17235/reed.2021.7896/2021.
Ilica AT, Kocaoglu M, Zeybek N, Guven S, Adaletli I, Basgul A, Coban H, Bilici A, Bukte Y. Extrahepatic abdominal hydatid disease caused by Echinococcus granulosus: imaging findings. AJR Am J Roentgenol. 2007;189(2):337–43. https://doi.org/10.2214/AJR.07.2255.
WHO Informal Working Group. International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop. 2003;85(2):253–61. https://doi.org/10.1016/s0001-706x(02)00223-1.
Stojkovic M, Rosenberger K, Kauczor HU, Junghanss T, Hosch W. Diagnosing and staging of cystic echinococcosis: how do CT and MRI perform in comparison to ultrasound? PLoS Negl Trop Dis. 2012;6(10): e1880. https://doi.org/10.1371/journal.pntd.0001880.
Srinivas MR, Deepashri B, Lakshmeesha MT. Imaging spectrum of hydatid disease: usual and unusual locations. Pol J Radiol. 2016;26(81):190–205. https://doi.org/10.12659/PJR.895649.
Siracusano A, Teggi A, Ortona E. Human cystic echinococcosis: old problems and new perspectives. Interdiscip Perspect Infect Dis. 2009;2009:474368. https://doi.org/10.1155/2009/474368.
Martel G, Ismail S, Bégin A, Vandenbroucke-Menu F, Lapointe R. Surgical management of symptomatic hydatid liver disease: experience from a Western centre. Can J Surg. 2014;57(5):320–6. https://doi.org/10.1503/cjs.024613.
Özdil B, Keçe C, Ünalp ÖV. An alternative method for percutaneous treatment of hydatid cysts: PAI technique. Turkiye Parazitol Derg. 2016;40(2):77–81. https://doi.org/10.5152/tpd.2016.4264.
Ben Amor N, Gargouri M, Gharbi HA, Ghorbel A, Golvan YJ, Hammou-Jeddi H, et al. Treatment of hepatic hydatid cyst in sheep by echographic puncture. Tunis Med. 1986;64:325–31.
Akhan O, Dincer A, Gököz A, Sayek I, Havlioglu S, Abbasoglu O, et al. Percutaneous treatment of abdominal hydatid cysts with hypertonic saline and alcohol: an experimental study in sheep. Invest Radiol. 1993;28:121–7.
Ahrari H. L’emploi de Cétrémide dans la chirurgie des kystes hydatiques [Use of Cetremide in the surgery of hydatid cysts]. Bull Soc Pathol Exot Filiales. 1978;71(1):90–4.
Meymerian E, Luttermoser GW, Frayha GJ, Schwabe CW, Prescott B. HOST-parasite relationships in echinococcosis: x. laboratory evaluation of chemical scolicides as adjuncts to hydatid surgery. Ann Surg. 1963;158(2):211–5. https://doi.org/10.1097/00000658-196308000-00008.
Baraka A, Wakid N, Yamout F. Methemoglobinemia during surgical excision of hydatid cyst. Middle East J Anaesthesiol. 1980;5(8):509–13.
Gilchrist DS. Chemical peritonitis after cetrimide washout in hydatid-cyst surgery. Lancet. 1979. https://doi.org/10.1016/s0140-6736(79)92862-9.
Momblano P, Pradere B, Jarrige N, Concina D, Bloom E. Metabolic acidosis induced by cetrimonium bromide. Lancet. 1984;2(8410):1045. https://doi.org/10.1016/s0140-6736(84)91147-4.
Acknowledgements
No acknowledgements.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Author information
Authors and Affiliations
Contributions
NB, HB, and AN performed the research; NB, MC, HB, and AH designed the research study; MAM, MC, and GAS contributed essential tools; HB, AH, MAM, AN, and MC analyzed the data; NB, MAM, and HB wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This case report was approved by the administration committee of ethics at St. Charles Hospital. The patient consent to participate in the research project.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bazzi, N., Baalbaki, H., Njeim, A. et al. Extrahepatic intraabdominal hydatid cyst: a case report. J Med Case Reports 18, 399 (2024). https://doi.org/10.1186/s13256-024-04733-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-024-04733-7