Abstract
Background
The human endometrium, lining the inner uterus, regenerates over 400 times uniquely during a woman’s reproductive life. Endometrial stem cells (eSCs) enrich the tissue, resulting in a dense vascular network, significant angiogenic potential, and effective regeneration power. Being of natural angiogenic properties and proven effective in the treatment of vascular disorders, eSCs can be considered safe, reliable, and superior to other post-natal stem cells. Cluster of Differentiation 146 (CD146) has emerged as a pivotal marker associated with pericytes and endothelial cells for promoting angiogenesis. Endometrial cells with high CD146 expression could proliferate and differentiate into multiple lineages. This study will explore the role of CD146 in eSCs, focusing on the potential to boost the angiogenic and regenerative functions of the cells. The novelty of this study lies in the investigation of CD146 on eSC function, which may open new possibilities for eSC-based therapy in regenerative medicine and vascular disorders.
Methods
The study involved obtaining endometrial biopsies from active reproducing women to isolate and cultivate eSCs. eSCs were assessed for growth factor secretion pattern, characterized for their mesenchymal properties. Finally, eSCs were tested for their angiogenic potential by angiogenic gene expression profile and in-ovo chick embryo model. As aimed, to check the role of CD146 in eSC angiogenesis, CD146+ cells were magnetically sorted and cultured. The sorted cells underwent various analyses, including flowcytometry to identify mesenchymal markers and human growth factor panel to analyze growth factor secretion profiles The study evaluated the angiogenic potential of CD146 + cells using functional assays, including ring formation, endothelial differentiation, and wound scratch assays, to evaluate cell migration and healing capabilities. Molecular insights were obtained through chemokine and cytokine investigations In-ovo Chick model assay was conducted to check the angiogenic potential and evaluated through macroscopic as well as through immunohistochemistry.
Result
Endometrial stem cells (eSCs) were successfully isolated using a combination of mechanical and enzymatic digestion, followed by culturing in complete DMEM media. The secretion profile of eSCs revealed significant production of various angiogenic growth factors, including Granulocyte macrophage colony-stimulating factor (GM-CSF), granulocyte colony stimulating factor (G-CSF), Vascular endothelial growth factor (VEGF), Fibroblast growth factors (FGF), and Platelet derived growth factor AA (PDGF-AA). The angiogenic gene profile indicated upregulation of several angiogenic genes in eSCs. The mesenchymal nature of eSCs was demonstrated through surface marker analysis (Cluster of differentiation 73, Cluster of differentiation 90, Cluster of differentiation 105) and trilineage differentiation. The in-ovo chick model confirmed the angiogenic potential of eSCs. CD146+ cells, isolated via magnetic sorting, exhibited enhanced angiogenic potential. These cells secreted significant levels of angiogenic growth factors such as VEGF. In Matrigel assays, CD146+ cells formed endothelial ring structures more rapidly and persistently than unsorted eSCs. Semi-quantitative PCR confirmed their endothelial differentiation. CD146+ cells express various angiogenic chemokines such as CXCL5, CXCL8, CCL3, and CCL20 and cytokines such as GM-CSF, Interleukin-1β (IL-1β), Interleukin-6 (IL-6), PDGF AA/BB, Epidermal growth factor (EGF), Endothelin 1, Angiopoietin. In-ovo chick model assay showed that CD146+ cells had superior angiogenesis, with more nodes, junctions, and segments compared to eSCs and controls. Immunohistochemistry confirmed increased expression of endothelial markers (Cluster of differentiation 31, VEGF, Vascular associated protein (VAP), Von Willebrand factor (vWF) in CD146+ cells.
Conclusion
The study highlights the angiogenic potential of endometrial stem cells, particularly the CD146+ cell population. These cells promote angiogenesis, secreting growth factors and forming stable blood vessel structures. CD146+ cells have higher expression levels of VEGF and TGF-α, key factors in angiogenesis. This suggests CD146+ eSCs may be promising for therapeutic applications in vascular diseases requiring angiogenesis. Further research is needed.
Similar content being viewed by others
Background
Endometrial stem cells (eSCs) have emerged as a promising source of cells for regenerative medicine due to their unique properties and therapeutic potential. The endometrium, the inner lining of the uterus, undergoes dynamic changes throughout the menstrual cycle, characterized by cyclic shedding and regeneration. This regenerative capacity is driven by endometrial stem cells, which play a crucial role in tissue repair, regeneration, and homeostasis [1, 2]. Angiogenesis, the formation of new blood vessels, is a fundamental process in endometrial regeneration and repair. eSCs have been shown to possess angiogenic properties, secreting growth factors and cytokines that promote endothelial cell proliferation, migration, and tube formation [3,4,5]. The endometrial stem cells holds emerging therapeutic potential. These cells play a vital role in tissue and cellular regeneration, as demonstrated by their natural function and location within the human body. When compare to the other sources of stem cells, these cells are easily accessible, available throughout a woman’s reproductive age, eSCs possess long term viability and expectational clonogenic property. More importantly, endometrium tissue can be obtained from the uterus that is to be discarded in the hysterectomy procedure, thus circumventing significant ethical issues. Human endometrium contains several types of stem cells and are crucial for regenerative applications. Endometrial epithelial stem cells are found in the basal layer and contribute in endometrial lining regeneration during menstrual cycle. Endometrial mesenchymal stem cells (MSCs) found in stromal region and have potential to differentiate into adipocyte, chondrocytes and osteocytes. Endometrial MSCs are also known for its high regenerative capacity and angiogenesis. There are also side population cells which are known to have long lasting clonogenic potential and also possess multilineage differentiation capacity into different types of endometrial stem cells. Understanding the angiogenic potential of eSCs holds significant clinical implications for treating conditions associated with impaired angiogenesis, such as endometrial dysfunction, infertility, and vascular diseases.
Vascular diseases are mediated by endothelial cell dysfunctions, leading to blockage of vessels. Cardiovascular diseases are the leading cause of mortality in India. The way of treating vascular diseases is temporary. Despite recent advances in surgical and radiological vascular procedures, a large number of patients are not eligible for these revascularization techniques [6]. Besides, exogenous induction of synthetic VEGF for ischemia [7, 8] and myocardial infarctions [9] is expensive, have less half-life and shows minimal or no effect. With the aim to address neovascularization, stem cell therapies have so far been applied to bone marrow, dental pulp, adipose tissue, and circulation; each has its own limitations with regard to cell procurement and therapeutic efficacy [10,11,12,13,14]. Pericytes, the wrapping cells around blood capillaries interact with endothelial cells to promote angiogenesis [15]. CD146 is a pericyte marker and key cell adhesion protein, highly expressed by cells of vascular endothelial cell and pericytes [16]. Endothelial cells were found to be activated by CD146 to boost their survival with increased cell migration, proliferation and capillary formation and regenerative ability under both in-vitro and in-vivo conditions as well by promoting neovascularization in preclinical models [17].
The fresh endometrial stromal cells with a high expression of CD146, a pericyte marker possesses proliferation and multipotent differentiation ability [18, 19]. This signifies the role of CD146 in endometrial stem cells and angiogenesis. Although the significance of CD146 correlating stem cells and pericytes for their angiogenic ability is being investigated in various aspects, until date, there are no Indian Scientist who has explored working on stem cell-pericyte interactions and their molecular mechanism in treating vascular diseases. Thus, the study intended novel and comprehensive examination of the angiogenic potential of CD146+ eSCs. By focusing on a specific subpopulation, employing innovative assay models, and providing detailed mechanistic insights, we contribute significant new knowledge to the field. This study not only advances our understanding of eSC biology but also lays the groundwork for future therapeutic strategies targeting vascular diseases.
Materials and methods
Sample collection
The study subjects were recruited from D. Y. Patil Hospital, Kolhapur with prior approval. The participants were informed about the purpose of sampling and written informed consent from the patients was obtained prior to sampling. All samples were transported to the laboratory in a sterile container with the medium. Human endometrial biopsies were collected from reproductively active women (n = 3) [5, 20] of the age 20, 30 and 45 respectively and in absence of any known endometrial disorders. All the samples were processed within 2 h of collection.
Isolation and culture of endometrial stem cells
The process involved carefully scraping the endometrial tissue from the underlying myometrium following the removal of the uterus through a hysterectomy. Subsequently, the curetted tissues underwent rinsing with Dulbecco’s phosphate-buffered saline (DPBS) (Make: Gibco, Cat. No. 10010023) containing antibiotics. The tissues were then incubated with 0.25% trypsin (Make: Gibco, Cat. No. 25200056) at 37 °C for 15 min in a humidified 5% CO2 incubator. To neutralize the enzyme, Dulbecco’s Modified Eagle Medium (DMEM) (Make: Gibco, Cat. No. 11965092) supplemented with 10% fetal bovine serum (FBS) (Make: Gibco, Cat. No. 26140079) was added. After digestion was stopped, the cell suspension was washed twice with DPBS (Make: Gibco, Cat. No. 10010023) by centrifugation at 450 g for 10 min to remove any remaining trypsin and cellular debris. The final cell pellet was re-suspended in a complete DMEM, seeded and cultured on t-25 flask. The cells were incubated in a humidified 5% CO2 incubator at 37 °C [21]. Cells were passaged every 3–5 days. Somatic cell contamination was eliminated when eSCs were cultured in specific growth media supplemented with growth factors such as fibroblast growth factor (FGF) and epidermal growth factor (EGF) to promote their proliferation and maintenance.
Flowcytometry analysis
Following passage five, cells were characterized for the surface marker using flowcytometry. Cells were harvested using trypsin and fixed in IC fixation buffer (make: Invitrogen cat No. 00-8222-49) Subsequently, the cells were thoroughly cleansed and stained by incubating them with specific antibodies at the recommended concentrations in PBS containing 2% BSA. After a period of 45 min of incubation, the cells were analyzed using BD FACS Aria. The antibodies used are mentioned in Table 1 with their appropriate dilutions. FITC conjugated mouse IgG1, PE conjugated mouse IgG1, PE conjugated IgG Mouse IgG2, PE conjugated IgG2 Rat were used as isotype control. Data acquisition and analysis were accomplished by using BD FACS Diva software (BD Biosciences, India). A minimum of 10,000 events were characterized and recorded [22].
Growth factor analysis of eSCs
In this investigation, we utilized the LEGENDplex™ Human Growth Factor Panel (Cat. No. 741282) for a thorough examination of the secretion of growth factors in eSCs. Before collecting the cell culture supernatant, cells were cultured in DMEM without serum for 48 h. Following kit guidelines, cell culture supernatants were prepared and appropriately diluted. Reconstituted beads, detection antibodies, and samples were introduced to a 96-well plate, where they underwent incubation and subsequent washing steps. The analysis was performed with the Attune NxT acoustic focusing cytometer. The kit has been designed for the simultaneous flowcytometry detection of 13 human growth factors: Angiopoietin-2 (Ang-2), EGF, EPO, FGF-basic, G-CSF, GM-CSF, HGF, M-CSF, PDGF-AA, PDGF-BB, SCF, TGF-α and VEGF in a single sample [23].
Angiogenesis PCR array
Angiogenesis PCR array for HUVEC, cultured endometrial cells (eSCs) were performed using Qiagen RT2 profiler PCR array kit (Make: Qiagen, Cat. No. 330231) and RT2 first strand kit (Make: Qiagen, Cat. No. 330404) by following the kit’s protocol. Briefly, The RNA was isolated from Endometrial stromal cells, HUVEC, and Cultured endometrial stromal cells (P3) by using Qiagen miRNeasy Mini Kit (Make: Qiagen, Cat. No. 217004) by following the instruction. The purified RNA, post QC check was subjected to cDNA synthesis using an RT2 first strand kit (Make: Qiagen, Cat. No. 330404) and stored at -20˚C till use. For the array, initially, RT2 SYBR Green Master mix (Make: Qiagen, Cat. No. 330502) was thawed and centrifuged briefly for 10–15 s. to bring the content down at the bottom. PCR components mix was prepared according to the table provided in the kit and the PCR components were mixed into the RT2 Profiler PCR Array 96 well plate, sealed carefully, and subjected to qPCR (QuantStudio 3, Thermo Fisher Scientific). After completion, the CT values were recorded and analysis was done using 2^-delta ct (relative gene expression) using the software. Housekeeping genes GAPDH, ACTB and B2M were incorporated in the plate itself.
Flowcytometry analysis
The detection of cell surface markers CD73, CD90, CD105 is done by MACSQuant®10 analyzer (MiltneyiBiotec, Germany). Cells were harvested using trypsin and fixed in IC fixation buffer (make: Invitrogen cat No. 00-8222-49) Subsequently, the cells were thoroughly cleansed and stained by incubating them with specific antibodies at the recommended concentrations in PBS containing 2% BSA. After a period of 45 min of incubation, the cells were analyzed using BD FACS Aria. The antibodies used are mentioned in Table 2. FITC conjugated mouse IgG1, PE conjugated mouse IgG1, PE conjugated IgG Mouse IgG2, PE conjugated IgG2 Rat were used as isotype control. The data was acquired from 10,000 events using the MACSQuantify™ software. The data analysis was performed by FlowJo™ v10 Software.
Tri-lineage differentiation
Differentiation studies were performed according to the previously published paper [24]. However, a brief protocol for each differentiation is explained below.
Osteogenic differentiation
Upon reaching 80–90% confluence, the complete cell culture media was replaced with an osteogenic induction medium with timely replacements. Osteogenic induction media consisted of DMEM-LG (Make: Gibco, Cat No. 11885084), 10% FBS (Make: Gibco, Cat. No. 26140079), 1% Antibiotic (Make: Gibco, Cat. No. 15240096), Dexamethasone (0.1 μM) (Make: Sigma Aldrich, India, Cat. No: D4902), β-glycerophosphate (10 mM) (Make: Sigma Aldrich, India, Cat. No. G-9422,) and Ascorbic acid (2 mM) (Make: Sigma Aldrich, India, Cat. No. A4544). Osteocytes were confirmed after 21 days of differentiation by Alizarin Red and Von Kossa staining. Stained cells were visualized using a phase contrast microscope.
Adipogenic differentiation
Similarly, adipogenic differentiation was promoted by differentiating the cells under the presence of adipogenic induction media containing DMEM-LG (Make: Gibco, Cat. No. 11885084), 10% FBS (Make: Gibco, Cat. No. 26140079), 1% Antibiotic (Make: Gibco, Cat. No. 15240096), Dexamethasone (1μM) (Make: Sigma Aldrich, India, Cat. No. D4902-25MG), Isobutyl methyl xanthine (0.5 mM) (Make: Sigma Aldrich, India, Cat. No. 15879,), Insulin (10 μg) (Make: HiMedia, Cat. No. TCL035,) and Indomethacin (200 μM) (Make: Sigma Aldrich, India, Cat. No. 17378,). Adipogenic differentiation was assessed on the eighteenth day of culture by staining the MSC monolayer with triglyceride-specific dye, Oil-O-Red.
Chondrogenic differentiation
Cells were incubated for 24 h after seeding at a density of 5000/ cm2 in a 12-well plate. Chondrogenic induction media (DMEM-LG (Make: Gibco, Cat. No. 11885084) with ITS 1X(Make: Gibco, Cat. No. 41400045), sodium pyruvate 1 mM (Make: Gibco, Cat. No. 11360070), dexamethasone 100 nM (Make: Sigma Aldrich, India, Cat. No. D4902), ascorbate-2-phosphate 50 mg/ml (Make: Sigma Aldrich, India, Cat No. 49752-10G), TGF-β3 10 ng/ml (Make: Sigma Aldrich, India, Cat. No. H8791-5UG), and L-proline 40 mg/ml (Make: Sigma Aldrich, India, Cat. No. P0380-10MG) was introduced to the cells. The cells were fed with the induction medium every two days. For the control group, the cells were grown on the plain growth medium alone. To check the chondrogenic differentiation and assess the glycosaminoglycan (GAGs) content, the cells were fixed and stained by using 2% alcian blue (Make: Sigma Aldrich, India, Cat. No. A5268-10G) after 28 days.
RT-PCR of stemness-related genes
Total RNA was isolated Qiagen RNeasy Mini Kit (Make: Qiagen, Cat. No. 74104) according to the manufacturer’s instructions. Total RNA was used for cDNA synthesis using High-Capacity.
cDNA Reverse Transcription Kit (Make: Applied Biosystem, India, Cat. No. 4368814), according to the manufacturer’s instructions (2 μg of RNA; 1 cycle 48° C/30 min; 95° C/5 min) and stored at.
-20° C. The quantification of mRNA expression levels for Oct-4, SOX-2, c-Myc, NANOG, ALDH1A3, PPAR γ, SOX-9, Runx2, and KLF-4 with GAPDH as housekeeping gene was carried out on QuantStudio™ 5 Real-Time PCR System using specific primers (IDT). Power SYBR Green PCR Master Mix (Applied Biosystems, Warrington, UK) was used for real-time monitoring of amplification (2 μl of template cDNA; 40 cycles: 95 ° C/ 15 s; 60° C/ 1 min) with primers. Expressions of target genes were normalized to human GAPDH using the ΔΔCt method. The cycle threshold (CT) values for each gene were corrected using the mean CT value. RT-qPCR data were quantified using the 2-ΔΔCt method and presented as relative gene expression normalized to the average CT for the human β-actin gene. Sequence for the primers are given in Table 3.
In-ovo angiogenic assay
According to the days of the experiment, Yolk Sac Model (YSM) is practiced in the in-Ovo angiogenic assay.
YSM: Yolk Sac Membrane model. (Experimental days 4–6)
Fertilized eggs of Black australorp were obtained from “Government hatchery center, Kolhapur, Maharashtra.” The shells of fertilized eggs were disinfected and incubated at 37.5˚C in humidified egg incubator until day 5–8 based on the experiment.
The experimental group were distributed as Control, Vehicle control (PBS control) and eSCs. Using forceps, a gap was made in the egg by holding the egg at 5 ‘o’ clock position. Albumin was extracted using a 2 ml syringe. The gap was then properly sealed using tape and parafilm. The egg was then carefully broken from the top (blunt end) and the bubbles along with more albumin was removed using pipette. 25,000 eSCs were then injected onto the chick vasculature and sealed with parafilm. Following this, eggs were returned to the incubator. Similarly, 1X PBS was injected on other eggs as vehicle control. The experiment was done in triplicates and surviving embryos were harvested for assessment.
Macroscopic analysis
The eggs were opened carefully to assess the angiogenic effect post 48 h of incubation of treatment. Photographs of the vasculature of both control and treated eggs were obtained with a digital camera and exported to a computer for image analysis using ImageJ software.
Histological preparation
The YSM was surgically removed and fixed in 10% buffered formaldehyde for 10 h, dehydrated in graded alcohol, cleared in xylene, and embedded in paraffin. 5 μm thick sections were cut in a plane parallel to the surface and stained by hematoxylin-eosin which was then observed under a light photomicroscope.
Magnetic cell sorting
The CD146 MicroBead Kit and MACS® Column (Make: Miltenyi Biotec, Cat. No. 130-093-596) were used to isolate CD146+ cells in accordance with the manufacturer’s instructions. In a nutshell, the kit’s CD146 microbeads and FcR blocking agent were used to react with the cells. After that, cells were put into a magnetic field and inserted onto a MACS LS column.
Growth factor analysis of sorted CD146+ cells
In this investigation, we utilized the LEGENDplex™ Human Growth Factor Panel (Cat No. 741282) for a thorough examination of the secretion of growth factors in CD146+ cells and eSCs. Before collecting the cell culture supernatant, cells were cultured in DMEM without serum for 48 h. Following kit guidelines, cell culture supernatants were prepared and appropriately diluted. Reconstituted beads, detection antibodies, and samples were introduced to a 96-well plate, where they underwent incubation and subsequent washing steps. The analysis was performed with the Attune NxT acoustic focusing cytometer. The kit has been designed for the simultaneous flow Cytometry detection of 13 human growth factors: Angiopoietin-2 (Ang-2), EGF, EPO, FGF-basic, G-CSF, GM-CSF, HGF, M-CSF, PDGF-AA, PDGF-BB, SCF, TGF-α and VEGF in a single sample [23].
Ring formation assay in matrigel
The in vitro assay will be carried out by coating 24 well plates with 200 μl of Matrigel (Make: Corning, Cat No. 354234) per well and incubated at 37˚C for an hour to solidify. The plates seeded with eSCs and CD146+ cells at a density of 1 × 103 cells per well and incubated with growth media. Formation of endothelial rings was observed at different time points and qualitatively analysed using a bright field phase contrast microscope (Nikon-Eclipse TE 2000-S) and photographed.
Characterization of differentiated endothelial cells
Differentiated endothelial cells were extracted from the matrigel and RNA isolated using the Qiagen RNeasy Mini Kit (Qiagen, Cat. No. 74104) according to the manufacturer’s instructions. The High-Capacity cDNA Reverse Transcription Kit (Make: Applied Biosystem, India, Cat. No. 4368814) was used to synthesise cDNA using 2 ug of RNA in accordance with the manufacturer’s guidelines. Master mix was prepared for KDR, Tie2, FLT1, vWF and β actin. Reactions were conducted using an Applied Biosystems TM ProFlexTM 96-well PCR equipment. 30 cycles of 5 min at 95 °C, 45 s at 55 °C, and 1 min at 72 °C were programmed in the PCR machine and executed. Meanwhile, a 2% agarose gel was made using EtbR, and once the gel solidified, the PCR product was loaded into the appropriate wells using a DNA ladder in a different well. HUVEC cells were used as positive sample.
Wound scratch assay
To determine the migration potential of CD146+ cells, a wound scratch assay was performed. For the wound scratch assay eSCs and CD146+ cells were seeded at the density of 0.04 × 106 and let it grow until 95% confluency. Cells were wounded by introducing a linear scratch on the monolayer using a 100 μl pipette tip. The area of the wound at selected time points (0, 12 and 24 h) was recorded to assess migration and wound healing using a bright field phase contract microscope and photographs was taken. The wound healing effect was calculated as the percentage of remaining cell-free area (at aforementioned time points) compared with the initial wound area using ImageJ software [30].
Chemokine analysis
A customized panel was designed for desired chemokines from BioLegend reactivity specified to human. Protocol performed as per the manufacture’s instructions. The assay protocol entails prewetting the plate with 100 μL of 1X Wash Buffer per well, then loading standards and samples in duplicate according to a predetermined configuration. After adding mixed beads (25 μL each well), the plate is sealed and allowed to sit at room temperature for two hours. Detection antibodies are added (25 μL per well) and the plate is sealed and incubated for an additional hour after it has been washed twice with 200 μL of 1X Wash Buffer. Next, add SA-PE (25 μL per well) without vacuuming, and continue to incubate for one additional step. Samples are read on a flowcytometer.
Cytokine analysis
Cytokine study was conducted for EGF, Endothelin 1, GM-CSF, IL-1β, IL-6, and Angiopoietin 1 using ELISA kits obtained from Invitrogen. The procedures were carried out in accordance with the manufacturers’ instructions.
In-ovo angiogenic assay
According to the days of the experiment, two models are practiced in the in-ovo angiogenic assay.
YSM: Yolk Sac Membrane model. (Experimental days 4–6)
CAM: Chick Chorioallantoic membrane model (Experimental day 8–10).
Initial procedure was followed as mentioned above. Briefly, the eggs were distributed as per experimental groups viz. Control, eSCs and CD146+ cells. For both of the models, in the case of direct injection, on day 4 of incubation, 2–3 ml of albumin was removed from the tapering end of the egg and the aperture was sealed with sterile adhesive tape. The egg was slightly opened at the blunt end (from the air sac area) with the help of sterile forceps. Cells incorporation was done according to the experimental groups and the opening was sealed with sterile adhesive tape and the procedure was followed as above.
Macroscopic analysis
The eggs were carefully opened to evaluate the angiogenic effect 48 h after treatment incubation (one week after initial incubation). Photographs of the vasculature in both control and treated eggs were taken with a digital camera and transferred to a computer for image analysis.
Histological preparation
The YSM / CAM was surgically removed and fixed in 10% buffered formaldehyde for 10 h, dehydrated in graded alcohol, cleared in xylene, and embedded in paraffin. 5 μm thick sections were cut in a plane parallel to the surface and stained by hematoxylin-eosin which was then observed under a light photomicroscope.
Immunohistochemistry protocol
The intensity of endometrial stem cells along with sorted CD146+ cells were analyzed by immunohistochemistry (IHC). Following deparaffinization and rehydration, antigen retrieval was performed using 0.01 M sodium citrate buffer (pH 6.0) in a pressure cooker at 100 °C for 20 min, followed by a 20-minute cooling period. Tissue sections underwent incubation to block the non-specific binding with the respective serum for 45 min at room temperature. Subsequently, the sections were incubated with CD31, VEGF, VAP and vWF at dilution of 1:200 in a humid chamber, followed by washing with distilled water containing 0.05% Tween 20. This was succeeded by incubating the sections for 60 min at room temperature with a secondary antibody in the dark, as per the manufacturer’s instructions. After washing with distilled water containing 0.05% Tween 20, sections were counterstained with DAPI for 30 s. Finally, the sections were mounted in fluorescent mounting medium. For negative staining, sections were stained with secondary antibody followed by DAPI for aforementioned duration.
Statistical analysis
All statistical analyses were performed using GraphPad prims version 10.2.0 for windows, GraphPad software, San Diego, California, USA. Descriptive statistics, including means, medians, standard deviations, and ranges, were calculated for all relevant variables. Data are presented as mean ± SD. P values < 0.05 were referred to as being significant.
Results
Isolation and culture of endometrial stem cells (eSCs)
The eSCs were isolated using trypsin digestion method and the cells isolated from human endometrium were cultured until P5 (Fig. 1 A). eSCs reached confluency within 5 days P0 and P1 and within 3 days subsequently from P2 onwards.
Flowcytometry characterization
With the fact that eSCs are present in the perivascular niche of endometrium and could be Mesenchymal in nature, endometrial cells were marker characterized using flowcytometry (Fig. 1B). The endometrial cells showed remarkable positivity CD16 and CD140b confirming their perivascular niche origin. Cell differentiation, development, and the determination of cell destiny are all impacted by CD49. It has an impact on polarity, growth, adhesion, migration, survival, and death of cells. eSCs with CD 90, CD 73, and CD 105 indicate that they are mesenchymal. For cell survival, proliferation, and differentiation, CD117 is crucial. A marker called CD13 is expressed on stem cells and in the majority of myeloid cell developmental phases. especially during the early stages of B and T cell development. CD44 marker denotes for transmembrane adhesion molecule for various mesenchymal markers and cell adhesion molecules. HLA-DR is weakly positive determining that, eSCs are originating from the perivascular cells of endometrium, as reported by Gargett. Additionally, the eSCs were negative for hematopoietic markers CD34, CD45, CD14, and CD19, confirming their mesenchymal stem cell identity.
Growth factor analysis
Secretory profile of various factors by eSCs is shown in Fig. 1C. G-CSF and GM-CSF secretion was highest among all. These two factors are majorly known for their immunomodulatory potential. Along with these two, EGF, FGF basic, PDGF-AA and VEGF shows remarkable expression in eSCs. These factors are recognized for promoting cell proliferation, cell migration and/ or promoting tubular morphology. Analysis was done using GraphPad Prism and p value is < 0.0001.
Isolation and culturing eSCs, surface marker analysis and growth factor analysis
Figure 1A; The sample was collected from the hospital (i), trypsin was used to digest it (ii), centrifugation was used to obtain the cell pellet (iii), and the isolated cells were cultured in full DMEM media (iv) image is taken at 10X. Figure 1B; The endometrial cells showed remarkable expression of mesenchymal (CD90, CD105, CD73, CD140b, CD146), cell adhesion molecules (CD29, CD44, CD166). However, the expression of HLA-DR, CD34, CD45, CD14 and CD19 were negative. Figure 1C; In growth factor secretion profile GM-CSF, G-CSF secretion concentration was higher than others. Followed by EGF, FGF basic, PDGF-AA and VEGF (p value: <0.0001)
Gene expression
To analyse the role of various angiogenesis associated gene expression, PCR array was used. The scatter plot Fig. 2 (i) compares the normalized expression of every gene on the array between the two selected groups by plotting them against one another to quickly visualize large gene expression changes. The central line indicates unchanged gene expression. The dotted lines indicate the selected fold regulation threshold. Data points beyond the dotted lines in the upper left and lower right sections meet the selected fold regulation threshold. Figure 2 (ii) is a heat map and shows the gene expression profile of angiogenesis related genes in HUVECs, and endometrial cells. Figure 2 (iii, iv, v and vi) shows upregulated genes and downregulated genes profile.
eSCs exhibited a fold change of 1097 in comparison to HUVEC cells, suggesting a noteworthy overexpression of TIMP3. Following TIMP3, substantial regulation was demonstrated by F3, FGF1, THBS2, IL1β, and LECT1. 660.8, 218.3, 132, 103.3, and 95.7 were their respective fold changes.
On the other hand, SERPINE and CDH5 were downregulated by -93.1 and − 54.2 folds, respectively, and PECAM was severely downregulated in eSCs with a fold change of -252.6.
Gene expression study of endometrial stem cells
(i) shows the scatter plot of the angiogenic gene. the scatter plot compares the normalized expression of every gene on the array between the two selected groups by plotting them against one another to quickly visualize large gene expression changes. The central line indicates unchanged gene expression. The dotted lines indicate the selected fold regulation threshold. Data points beyond the dotted lines in the upper left and lower right sections meet the selected fold regulation threshold. Heat map is shown in (ii) represents gene expression profile of angiogenesis related genes of HUVEC and eSCs. Up and Downregulated genes of eSCs normalized with respect to HUVEC shows in (iii, iv, v and vi)
Endometrial stem cells are mesenchymal in nature
eSCs have tendency to express major MSC surface markers such as CD73, CD90 and CD105 and also to differentiate into differentiation [31]. The nature of eSCs was analyzed and confirmed by flowcytometry and expressed 97.6% CD73, 99.9%CD90 and 100% CD105 (Fig. 3A).
The stemness-related genes in these cells, including Oct-4, SOX 2, c-Myc, NANOG, ALDH1A3, PPAR γ, SOX 9, RUNX2, and KLF4, were then examined. As seen in Fig. 3B, the gene expression emphasized the cells’ stemness. The cells’ strong expression of ALDH1A3 and c-Myc suggested their capacity for proliferation and expansion. High levels of c-Myc expression are associated with the ability of eSCs to proliferate cells, angiogenesis, and cellular metabolism in the endometrial microenvironment. ALDH1A3 is involved in stem cell maintenance, proliferation, and differentiation in addition to retinoic acid synthesis in cells. Prior research has also demonstrated that endometrial cells express more ALDH1A3. Results are significant with p value 0.0012.
moreover, eSCs also revel the differentiation potential. To prove the differentiation efficacy of endometrial stem cells tri-lineage differentiation was carried out. Endometrial stem cells Fig. 3C (a), were differentiated in to Osteocytes Fig. 3C (b), and Chondrocytes Fig. 3C (c) Adipocytes Fig. 3C (d). The differentiation was confirmed using its respective staining. von kossa for osteoblast and oil o red for adipocytes.
eSCs shows angiogenic potential
Figure 3D shows YSM assay, in-ovo, which represents the angiogenic potential of eSCs. The figure shows neoangiogenic effect of eSCs on Yolk Sac Model (YSM) models. Figure 3D (a) are the controls where the egg kept untouched. Figure 3D (b) is vehicle control wherein PBS was injected. Figure 3D (c) represents models, injected with eSCs. Figure 3D (d, e, f) represents the histological staining of the YSM models respectively. As demonstrated by the pattern and density of blood vessel creation (angiogenesis) in the YSM models, eSCs had a pro-angiogenic effect. Using ImageJ’s Angio analyzer plugin, the number of nodes, junctions, and segments was quantified Fig. 3E. results were quantified using GraphPad and results were significant with p value < 0.0001 Histological staining verifies that the models with eSC injections exhibit a branching pattern.
eSCs are mesenchymal in nature, in-ovo angiogenic potential of eSCs
Figure 3 illustrates the characterization and functional assessment of eSCs. Figure 3A shows flowcytometry analysis of mesenchymal stem cell surface markers, revealing that eSCs express CD73 (a), CD90 (b), and CD105 (c) with high positivity. Figure 3B presents the relative gene expression levels of stemness-related genes (Oct4, Sox2, c-Myc, Klf4, ALDH1A3, PPARγ, SOX9, RUNX2) in eSCs, with data shown as mean ± standard deviation. Figure 3C demonstrates the tri-lineage differentiation potential of eSCs, with images showing adipogenic differentiation stained with Oil Red O (a), osteogenic differentiation stained with Alizarin Red S (b), and chondrogenic differentiation stained with Alcian Blue (c) and Safranin O (d). Figure 3D depicts the in-ovo angiogenic assay using a chick embryo model, illustrating the angiogenic potential of eSCs through images of control (a), vehicle control (b), and eSC-treated groups (c), along with histological analysis of vessel formation in these groups (d-f) images were taken at 20X. Finally, Fig. 3E quantifies the number of nodes, junctions, and segments in control, vehicle control, and eSC-treated groups, showing enhanced angiogenesis in the eSC-treated group, with data represented as mean ± standard deviation
CD146+ population of stem cells are highly potent in inducing angiogenesis
After characterizing the isolated cells and identifying growth factors secreted by them and angiogenic genes expressed in these cells, we cultured the eSCs isolated and analysed them further.
The cells isolated from endometrium were analysed and compared with the cultured cells that were isolated from the same source (endometrium). CD146 is a prominent markers of mesenchymal stem cells and is involved in angiogenesis and cell proliferation.
Figure 4A shows the expression of CD146 on the cultured eSCs. The cultured eSCs showed higher expression of CD146 which is 91.6%. This higher expression in cultured cells is probably due to the involvement of CD146 in cell proliferation. A study analysing a similar aspect reported higher expression of CD146 on cultured cells.
From the cultured cells, CD146+ cells were sorted and analysed for their growth factor secretion profile using cytokine bead array and compare with unsorted cells or hetereogeneous cell population.
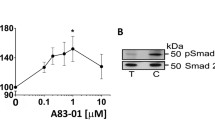
Growth factor analysis
As illustrated in Fig. 4B, M-CSF was predominantly expressed and secreted by unsorted cells, whereas TGF-α and VEGF were primarily secreted by CD146+ cells. This indicates that the CD146+ cell population, or specific stem cell subset, expressed both VEGF and TGF-α. Additionally, VEGF secretion was notably high in eSCs in this study. Given the specialized role of CD146+ cells in angiogenesis and cell proliferation, they were observed to express VEGF and TGF-α. The results were statistically significant, with a p-value of 0.0008.
Endothelial ring formation assay
The ability of CD146+ cells to develop into endothelial lineage was investigated in this study. The Matrigel tube formation test was used for this. At 0 h, 6 h, 10 h, and 15 h, the spontaneous organization of the endothelium ring of eSCs and CD146+ was observed. Within 15 h of incubation, a ring-like structure quickly developed in both CD146+ cells and eSCs. Despite this, eSCs generate persistent endothelial tubes 4 h later than CD146+ cells. Figure 4C show the minuscule pictures were captured at different intervals.
Therefore, sorted CD146+ shows better angiogenic potential than eSCs. This finding is also in line with another wherein authors have highlighted better angiogenic potential than differentiated cells. Other studies have also suggested that CD146+ cells are more responsive to growth factors such as PDGF or platelet derived growth factor [32].
Characterization of endothelial rings
The expression of pro- and angiogenic markers determined for the differentiated endothelial cells at 15 h using an RT-PCR technique allowed for the confirmation that the cells were endothelial. For evaluation, a panel of markers including KDR, Tie2, FLT1, and vWF was employed (Fig. 4D). HUVEC cells served as the reference standard. The outcome accurately indicates the endothelial lineage commitment of CD146+ cells, with HUVEC cell marker expression being unchanged.
Wound scratch assay
Wound scratch assay were performed on unsorted eSCs and sorted CD146+ cells from eSCs to check the migration potential. No significant difference was found in initial scratch width at 0 h in both the groups. The result of cell migration was summarised in Fig. 4E. An additional graph Fig. 4F generated by ImageJ showing datapoints is also provided. At the time point 12 and 24 h post scratch the CD146+ sorted cells group has significantly decrease compared to the eSCs group. Quantification was done using GraphPad Prism p value obtained was 0.0020.
Analysis of CD146+ cells
Characterization and functional assays of endometrial stem cells (eSCs) and CD146+ sorted cells. Figure 4A Flowcytometry shows 91% CD146 expression in sorted eSCs. Figure 4B Growth factor analysis indicates higher levels of VEGF, TGF-α, and others in CD146+ cells compared to eSCs. Figure 4C Endothelial ring formation assay demonstrates enhanced differentiation in CD146+cells over time (0, 6, 10, 15 h) compared to eSCs. Figure 4D Semi-quantitative PCR confirms endothelial differentiation, with endothelial markers (KDR, Tie2, FLT1, VWF) present in differentiated cells (lanes 2, 4, 7, 9, 12) and HUVEC controls (lanes 1, 3, 6, 8, 11). Figure 4E Wound scratch assay shows faster migration and wound closure in CD146+ cells at 0, 12, and 24 h. Images were taken at 4X. Figure 4 F Quantification of the wound scratch assay indicates greater migration distance in CD146+cells compared to eSCs, highlighting their superior regenerative potential
Chemokine analysis
Chemokines are pivotal in recruiting leukocytes to inflammation sites and regulating angiogenesis, the formation of new blood vessels Fig. 5A displays the cytokine analysis of CD146+ and eSCs. Among them, CXCL5 and CXCL8 exhibit pro-angiogenic properties, with significant differences in their levels (P ≤ 0.0001 and P ≤ 0.0001, respectively), indicating their importance in stimulating endothelial cell migration and proliferation. Additionally, CCL3 and CCL20 play crucial roles in angiogenesis and immune cell recruitment, supported by highly significant differences in their levels (P ≤ 0.0001). These findings underscore the intricate involvement of chemokines in the complex molecular regulation of angiogenesis. Whereas, CXCL11 which act as angiostat and CXCL1 are observed downregulated in CD146+ cells.
Cytokine assay
Figure 5B displays the cytokine analysis of CD146+ and eSCs. According to the current study, sorted CD146+ cells express more GM-CSF, IL-1β, IL-6, PDGF AA/BB, EGF, Endothelin 1, Angiopoietin1, and GM-CSF than eSCs. Because it inhibits leukocyte–endothelium interactions and endothelial permeability, angiopoietin-1 (Ang1) is essential for endothelial survival and vascular stabilisation. The proliferation of mesenchymal stem cells (MSCs) is regulated by epidermal growth factor (EGF). A receptor ligand called EGF encourages MSC proliferation and paracrine action. Moreover, EGF can aid MSCs in producing VEGF and HGF, which are critical for tissue regeneration and wound repair. The vasoconstrictor endothelin-1 (ET-1) has the ability to improve the regeneration potential of mesenchymal stem cells (MSCs) generated from human bone marrow. A vital component of haematopoiesis, immunological response, cell survival, and cell proliferation, IL-6 is a pleiotropic cytokine. Results were significant with p value < 0.0001.
Molecular insights and in-ovo assay of CD146+ cells
Figure 5A; Chemokines, including CXCL5, CXCL8, CCL3, and CCL20, play crucial roles in angiogenesis and immune cell recruitment, demonstrating their intricate involvement in inflammation site inflammation and blood vessel formation. Figure 5B; The study reveals that CD146+ cells express more cytokines than eSCs, including GM-CSF, IL-1β, IL-6, PDGF AA/BB, EGF, Endothelin 1, Angiopoietin1, and GM-CSF, crucial for endothelial survival and vascular stabilization. Figure 5C; The study found that CD146+ sorted cells, which are involved in angiogenesis, have a higher number vasculature compared to other groups viz. control and eSCs. Figure 5D; The study found that CD146+ sorted cells, which are involved in angiogenesis, have a higher number vasculature compared to other groups viz. control and eSCs. Figure 5E; In comparison to other groups (control and eSCs), the study discovered that CD146+ sorted cells—which are involved in angiogenesis—had a higher number of vasculatures. Figure 5F; Quantification of the vasculature in terms of nodes, junctions, and segments was done using ImageJ’s Angio Analyzer tool plugin
Immunohistochemistry of YSM
Immunofluorescence staining of tissue sections for endothelial and angiogenic markers at 20X magnification. Panels display CD31 (A-D), VEGF (E-H), VAP (M-L), and vWF (I-P). Negative Control (A, E, M, I) shows minimal background fluorescence. Control (B, F, J, N) shows untreated tissue with CD31 (B), VEGF (F), VAP (J), and vWF (N) expression. eSCs (C, G, K, O) indicates enhanced expression of CD31 (C), VEGF (G), VAP (K), and vWF (O) compared to control. CD146+ cells (D, H, L, P) show increased expression of CD31 (D), VEGF (H), VAP (L), and vWF (P) compared to both control and eSCs sections. Scale bar = 100 μm. Blue indicates DAPI-stained nuclei; green indicates specific antibody staining. (Q) Indicates the bright filed images of cells
In-ovo assay
We analysed the role of CD146 further for their potential to induce angiogenesis. YSM assay was conducted to assess the angiogenic potential of eSCs and to understand the role CD146 in angiogenesis. three groups, control, only eSCs and CD146+ cells were analysed.
In YSM assay, the pattern of vessels formation, density radial symmetry and spatial arrangement are shown in Fig. 5C and its graphical representation is displaced in Fig. 5D. After treatment, the number of junctions, nodes and segments were analysed using ImageJ software.
In the control group of YSM assay, number of nodes was higher than treatment groups. CD146+ sorted cells showed higher number of nodes, junctions and segments than other groups. YSM assays concreted our finding further that CD146+ cells are involved in angiogenesis and are more capable in inducing angiogenesis than other stem cell populations.
Figure 5E depicts the pattern of vessel creation, density, radial symmetry and spatial arrangement in the CAM assay. Figure 5F shows a displaced visual depiction of the CAM assay quantification using ImageJ software in the form of number of junctions, nodes and segments. Quantification of number of nodes, junctions and segment was done and p value obtained was 0.0023 for YSM assay and 0.0016 for CAM assay.
The Immunohistochemistry of yolk sack membrane of chick showing expreesion of endothelial and angiogenic marker is displayed in Fig. 6. We assessed the expression of CD31, VEGF, VAP and vWF in control, eSC treated group as well as in CD146+ cells treated group. In the control group (Fig. 6 A, D, G, J), baseline expression levels of these markers are minimal, as indicated by the sparse staining, reflecting low inherent endothelial and angiogenic activity. In contrast, the endometrial stem cells (eSCs) group (Fig. 6 B, E, H, K) shows moderate expression of CD31, VEGF, VAP, and vWF, evidenced by arrows highlighting areas of positive staining, indicating some degree of endothelial cell presence and angiogenic potential. Most notably, the CD146+ sorted cells group (Fig. 6 C, F, I, L) exhibits significantly higher expression of all four markers. The extensive and intense staining in these panels, as highlighted by the arrows, demonstrates a robust level of endothelial differentiation and angiogenic activity. This stark contrast suggests that CD146+ cells possess a superior capability for promoting endothelial differentiation and vascular formation compared to both the eSCs and control groups, highlighting their potential for use in vascular regeneration and tissue engineering.
Discussion
The present study provides novel insights into the characterization and angiogenic potential of endometrial stem cells (eSCs), particularly CD146+ cells, highlighting their role in tissue regeneration and angiogenesis. The study employed trypsin digestion to isolate eSCs, which were characterized by flowcytometry to express cell adhesion markers, CD146, and CD140b, indicative of their niche-specific properties. These findings align with previous studies that have identified CD146 as a marker of perivascular stem cells with angiogenic potential in various tissues, including the endometrium [33, 34].
The endometrium begins to reach full development at puberty and thereafter exhibits remarkable changes during each menstrual cycle. It undergoes further changes before, during, and after pregnancy, during the menopause, and in old age [35]. Thus, based on this dynamic property of endometrial stem cells undergoes unique tissue remodeling and regeneration, it is ideal that stem cells of the endometrium possess an inherent angiogenic and high regenerative potential as compared to other post-natal stem cells. Hence, with its innate unique qualities coupled with extensive vascualrization potential.
Our results also demonstrated significant expression of angiogenesis-related genes and secretion of angiogenic growth factors, such as GM-CSF, G-CSF and VEGF by eSCs along with EGF, FGF basic, PDGF-AA. These factors have their role mainly in promoting angiogenesis and stability [36]. CD146 is upregulated in endothelial cells during angiogenesis and is implicated in the stabilization of newly formed blood vessels. It acts as a co-receptor for VEGF and contributes to the signaling pathways that promote endothelial cell proliferation and migration [37]. CD146+ pericytes enhance angiogenesis by.
promoting endothelial cell survival, migration, and tube formation. They respond more robustly to PDGF-BB stimulation, which is critical for their angiogenic function. The presence of CD146+ pericytes leads to more effective and sustained endothelial sprouting and vascular stabilization, suggesting that CD146 is a key marker for pericyte-mediated angiogenesis [32].
Angiogenesis is combination of pro and anti- angiogenic marker as Endometrial stem cells undergo dynamic changes in gene expression throughout the menstrual cycle and the differentiation process. The significantly high fold change in TIMP3 expression observed in endometrial stem cells (eSCs) compared to HUVEC cells is noteworthy. Tissue inhibitor of metalloproteinase 3 (TIMP3) is known for its role in regulating extracellular matrix remodeling and angiogenesis [38]. Studies have shown that TIMP3 can inhibit angiogenesis by blocking the activity of matrix metalloproteinases (MMPs), which are involved in the degradation of extracellular matrix components [39]. Therefore, the high expression of TIMP3 in eSCs may suggest a regulatory mechanism to control angiogenesis and maintain tissue homeostasis in the endometrium. The F3 gene, which produces tissue factor, induces angiogenesis in mesenchymal stem cells, binds to integrins α6β1 and αVβ3, increasing FAK, PI3K/AKT, and MAPK signaling [40]. FGF1 promotes angiogenesis, encourages stemness, inhibits senescence and cell death, and aids in the control of cell proliferation [41]. THBS1 slightly enhances endothelial cell length and proliferation in capillary sprouts, indicating its role in stimulating cell differentiation into tip cells for new capillary sprout development [42]. IL-1 beta drives the angiogenesis and also helps in wound healing [43]. PECAM is endothelial haemopoietic marker hence its downregulation confirms the pure population of eSCs and perform angiogenic activity only after they differentiate into endothelial cells. Serpine 1 codes for PAI 1 which involves in clot formation and also it regulates tumor angiogenesis and invasion. Down regulation of SERPINE1 proves that eSCs maintains homeostasis [44]. Besides this CDH5 is adherence junction of endothelial cells. Downregulation of CDH5 also shows the pure population of eSCs. The findings suggest that eSCs have a distinct gene expression profile associated with angiogenesis, with potential implications for understanding the role of eSCs in endometrial physiology and pathology.
Endometrial stem cells are derived from the endometrium, the tissue that lines the uterus. They can be obtained through non-invasive methods such as endometrial biopsy. These cells exhibited the capacity to express crucial stem cell markers such as CD73, CD90, and CD105, confirming their mesenchymal stem cell character (Fig. 3A). Studies have shown that ALDH1A3 is expressed in endometrial cells and tissues and that its expression is often associated with endometrial stem/progenitor cell populations. c-Myc is known to regulate cell proliferation and self-renewal in stem cells. Its overexpression can enhance the proliferation of stem cells, a characteristic shared with endometrial stem cells that actively divide during the menstrual cycle to replenish the endometrial lining [45, 46]. In our study, in accordance with other reports, eMSCs possess large spectrum of differentiation ability. MSCs showed an efficient differentiation towards osteoblast, adipogenic, chondrogenic and beta cell lineages. A chick embryo Yolk Sac Model (YSM) assay was conducted in order to determine the angiogenic properties of eSCs in in-ovo setting. In the in-ovo YSM model, eSCs exhibited a pro-angiogenic effect, as evidenced by increased angiogenesis [47,48,49]. This justifies that eSCs possess angiogenic potential inherently.
In recent years, pericytes have come in the picture as efficient and critical contributors in pathological and physiological angiogenesis. It is thought that they migrate through the basal lamina which is necessary for the activation of stem cell therapy. Pericytes play a key role in stabilization of endothelial cells by regulating the vascular growth, maturation, and remodeling and has a vital role in angiogenesis. CD146, a significant pericyte-endothelial marker has been found to possess angiogenic properties and promote neovascularization. The fresh endometrial stromal cells with a high expression of CD146, a pericyte marker possesses proliferation and multipotent differentiation ability [18, 19]. This signifies the role of CD146 in endometrial stem cells and angiogenesis.
The positively sorted CD146 cells from endometrium showed 90% surface maker expression of CD146 cells at passage 5. CD146+ cells, a specific stem cell population, expressed VEGF and TGF-α, which are known to promote angiogenesis and tissue regeneration [50, 51]. The matrigel tube formation assay showed stable ring formation by CD146+ cells, indicating their superior angiogenic potential compared to unsorted cells. These findings are in line with previous studies demonstrating the pro-angiogenic properties of CD146+ cells in various tissues [32, 33]. The wound scratch assay revealed that CD146+ sorted cells exhibited decreased migration potential compared to unsorted eSCs. This finding suggests that CD146+ cells may play a more significant role in angiogenesis rather than cell migration, highlighting the complexity of stem cell behaviour in different microenvironments [33]. The chemokine analysis of CD146+ cells showed notable differences in CXCL5, CXCL8, CCL3, and CCL20 levels, suggesting their involvement in angiogenesis and immune modulation [52].
In our study, we examined the angiogenic potential of CD146+ endometrial stem cells (eMSCs), focusing on the key molecules responsible for this capability. CD146+ eMSCs have been found to secrete high levels of Vascular Endothelial Growth Factor (VEGF), a critical factor in promoting the formation of new blood vessels. Additionally, these cells express Angiopoietin, bFGF, PDGF which contributes to vascular stability and maturation, thereby enhancing the angiogenic environment.
In the in-ovo assay, CD146+ cells demonstrated superior angiogenic potential compared to other stem cell populations, as evidenced by increased nodes, junctions, and segments in vessel formation. Immunohistochemical analysis further supported these findings, showing higher expression of vascular markers (CD31, VEGF, VAP, vWF) in CD146+ eSCs compared to control and other groups. These results suggest that CD146+ eSCs are highly angiogenic and have the potential to promote tissue regeneration, making them a promising candidate for therapeutic angiogenesis in vascular diseases.
Despite the promising findings, several limitations of this study should be acknowledged. The small sample size and the lack of in vivo validation of the angiogenic potential of eSCs are major limitations. Additionally, the study focused primarily on the angiogenic properties of eSCs and did not investigate other potential therapeutic applications, such as immunomodulation or tissue engineering. Future studies should aim to address these limitations and further elucidate the mechanisms underlying the angiogenic potential of eSCs.
This study highlights the angiogenic potential of eSCs, particularly CD146+ cells, and their role in angiogenesis and tissue regeneration. The findings suggest that CD146+ eSCs exhibit promising potential for therapeutic angiogenesis in vascular diseases. Further in-vivo research is warranted to fully understand the therapeutic implications of eSCs and to explore their potential in other regenerative medicine applications.
Conclusion
The current study elucidates the angiogenic properties of endometrial stem cells (eSCs) and CD146+ cells, highlighting their potential in therapeutic angiogenesis. The angiogenic potential of eSCs primarily operates through the secretion of pro-angiogenic growth factors such as VEGF, FGF, PDGF, and EGF, which facilitate vascular growth through paracrine signalling. Additionally, eSCs’ ability to differentiate into endothelial cells further enhances their pro-angiogenic capabilities. CD146+ cells, sorted from eSCs, serve as perivascular cells in the endometrium, playing critical roles in angiogenesis and endothelial cell stabilization. These cells interact closely with endothelial cells, promoting vessel remodeling and sprout formation. They secrete significant amounts of FGF, VEGF, and pro-angiogenic cytokines such as IL6 and IL8, which collectively support angiogenesis.
However, several challenges and limitations remain in this field. One of the primary challenges is the variability in the isolation and characterization of eSCs, which can affect the reproducibility of results. Additionally, while the in vitro and in ovo models provide valuable insights, they may not fully replicate the in vivo environment of the human uterus. Future studies should aim to validate these findings in more clinically relevant models.
This study provides valuable insights into the mechanisms underlying the angiogenic properties of eSCs and CD146+ cells, suggesting their potential application in treating vascular diseases. Future research should focus on further elucidating these mechanisms and exploring the therapeutic potential of these cells in clinical settings.
Data availability
All data supporting the findings given in this study are available in the paper and its Supplementary Information. There was no data sourced from external repositories.
Abbreviations
- ALDH1A3:
-
Aldehyde dehydrogenase 1A3
- Ang-2:
-
Angiopoietin-2
- ANGPT2:
-
Angiopoietin-2
- c-Myc:
-
Cellular- myelocytomatosis
- CCL20:
-
Chemokine (C-C motif) ligand 20
- CCL3:
-
Chemokine (C-C motif) ligand 3
- CD105:
-
Cluster of Differentiation 150
- CD140b:
-
Cluster of Differentiation 140 b
- CD146:
-
Cluster of Differentiation 146
- CD14:
-
Cluster of differentiation 14
- CD19:
-
Cluster of differentiation 19
- CD31:
-
Cluster of Differentiation 31
- CD34:
-
Cluster of Differentiation 34
- CD45:
-
Cluster of differentiation 45
- CD73:
-
Cluster of Differentiation 73
- CD90:
-
Cluster of Differentiation 90
- CDH5:
-
Cadherin 5
- CXCL5:
-
CXC chemokine ligand 5
- CXCL8:
-
CXC chemokine ligand 8
- DMEM-LG:
-
Dulbecco’s Modified Eagle Medium: Low Glucose
- DMEM:
-
Dulbecco’s Modified Eagle Medium
- DPBS:
-
Dulbecco’s Phosphate Buffered Saline
- EGF:
-
Epidermal growth factor
- EGF:
-
Epidermal growth factor
- EPO:
-
Erythropoietin
- eSCs:
-
Endometrial stem cells
- F3:
-
Coagulation factor III
- FBS:
-
Fetal bovine serum
- FGF-basic:
-
Basic fibroblast growth factor
- FGF1:
-
Fibroblast growth factor 1
- G-CSF:
-
Granulocyte colony-stimulating factor
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- GM-CSF:
-
Granulocyte macrophage colony-stimulating facto
- HGF:
-
Hepatocyte Growth Factor
- HUVEC:
-
Human umbilical vein endothelial cells
- IL-1β:
-
Interleukin-1 beta
- IL-6:
-
Interlukin-6
- ITS:
-
Insulin-Transferrin-Selenium
- KLF4:
-
Krüppel-like factor 4
- LECT1:
-
Leukocyte cell-derived chemotaxin 1
- M-CSF:
-
Macrophage colony-stimulating factor
- Oct4:
-
Octamer-binding transcription factor 4
- PDGF-AA:
-
Platelet-derived growth factor subunit A
- PDGF-BB:
-
Platelet-derived growth factor subunit B
- PPARγ:
-
Peroxisome Proliferator–Activated Receptorγ
- RUNX2:
-
Runt-related transcription factor 2
- SCF:
-
Stem Cell Factor
- SERPINE:
-
Serine protease inhibitor E
- SOX2:
-
Sex determining region Y-box 2
- SOX9:
-
SRY-Box Transcription Factor 7
- TGF-α:
-
Transforming growth factor-alpha
- THBS2:
-
Thrombospondin-1
- TIMP3:
-
Tissue inhibitor of metalloproteinase 3
- VAP:
-
Vascular Associated protein
- VEGF:
-
Vascular endothelial growth factor
- vWF:
-
Von Willebrand factor
References
Gargett CE. Uterine stem cells: what is the evidence? Hum Reprod Update. 2007;13(1):87–101.
Kshersagar J, Pulgam L, Damle MN, Tardalkar K, Sharma R, Joshi MG. Transplantation of human placenta derived mitochondria promotes cell communication in endometrium in a murine model of disturbed endometrium. Stem Cell Rev Rep. 2023;19(5):1384–401.
Schwab KE, Hutchinson P, Gargett CE. Identification of surface markers for prospective isolation of human endometrial stromal colony-forming cells. Hum Reprod. 2008;23(4):934–43.
Cousins FL, Filby CE, Gargett CE. Endometrial stem/progenitor cells-their role in endometrial repair and regeneration. Front Reprod Health. 2022;3:811537.
Hong IS. Endometrial stem cells: orchestrating dynamic regeneration of endometrium and their implications in diverse endometrial disorders. Int J Biol Sci. 2024;20(3):864–79.
Leeper NJ, Hunter AL, Cooke JP. Stem cell therapy for vascular regeneration: adult, embryonic, and induced pluripotent stem cells. Circulation. 2010;122(5):517–26.
Hopkins SP, Bulgrin JP, Sims RL, et al. Controlled delivery of vascular endothelial growth factor promotes neovascularization and maintains limb function in a rabbit model of ischemia. J Vasc Surg. 1998;27:886–94.
Sun Q, Chen RR, Shen Y, et al. Sustained vascular endothelial growth factor delivery enhances angiogenesis and perfusion in ischemic hind limb. Pharm Res. 2005;22:1110–6.
Wang B, Cheheltani R, Rosano J, et al. Targeted delivery of VEGF to treat myocardial infarction. Adv Exp Med Biol. 2013;765:307–14.
Dimmeler S, Burchfield J, Zeiher AM. Cell-based therapy of myocardial infarction. Arterioscler Thromb Vasc Biol. 2008;28:208–16.
Mocini D, Staibano M, Mele L, et al. Autologous bone marrow mononuclear cell transplantation in patients undergoing coronary artery bypass grafting. Am Heart J. 2006;151:192–7.
Higashi Y, Kimura M, Hara K, et al. Autologous bone-marrow mononuclear cell implantation improves endothelium-dependent vasodilation in patients with limb ischemia. Circulation. 2004;109:1215–8.
Onodera R, Teramukai S, Tanaka S, et al. Bone marrow mononuclear cells versus G- CSF-mobilized peripheral blood mononuclear cells for treatment of lower limb ASO: pooled analysis for long-term prognosis. Bone Marrow Transplant. 2011;46:278–84.
Hare JM, Fishman JE, Gerstenblith G, et al. Comparison of allogeneic vs autologous bone MarrowDerived mesenchymal stem cells delivered by transendocardial injection in patients with ischemic cardiomyopathy: the POSEIDON randomized trial. JAMA. 2012;12:308:2369–79.
Gerhardt H, Betsholtz C. Endothelial-pericyte interactions in angiogenesis. Cell Tissue Res. 2003;314:15–23.
Gargett CE, Schwab KE, Deane JA. Endometrial stem/progenitor cells: the first 10 years. Hum Reprod Update. 2016;22(2):137–63.
Harhouri K, Kebir A, Guillet B, et al. Soluble CD146 displays angiogenic properties and promotes neovascularisation in experimental hind-limb ischemia. Blood. 2010;115:3843–51.
Spitzer TLB, Rojas A, Zelenko Z, et al. Perivascular human endometrial mesenchymal stem cells express pathways relevant to self-renewal, lineage specification, and functional phenotype. Biol Reprod. 2012;86:58.
Schwab KE, Gargett CE. Co-expression of two perivascular cell markers isolates mesenchymal stem-like cells from human endometrium. Hum Reprod. 2007;22:2903–11.
Leñero C, Kaplan LD, Best TM, Kouroupis D. CD146 + endometrial-derived mesenchymal stem/stromal cell subpopulation possesses exosomal secretomes with strong immunomodulatory miRNA attributes. Cells. 2022;11(24):4002.
Tavakol S, Azedi F, Hoveizi E, Ai J, Joghataei MT. Human endometrial stem cell isolation from endometrium and menstrual blood. Bio Protoc. 2018;8(2):e2693.
Indumathi S, Harikrishnan R, Mishra R, et al. Comparison of feto-maternal organ derived stem cells in facets of immunophenotype, proliferation and differentiation. Tissue Cell. 2013;45(6):434–42.
Raj AT, Kheur S, Khurshid Z, et al. The growth factors and cytokines of dental pulp mesenchymal stem cell secretome may potentially aid in oral cancer proliferation. Molecules. 2021;26(18):5683.
Marappagounder D, Somasundaram I, Dorairaj S, Sankaran RJ. Differentiation of mesenchymal stem cells derived from human bone marrow and subcutaneous adipose tissue into pancreatic islet-like clusters in vitro. Cell Mol Biol Lett. 2013;18(1):75–88.
Yin X, Li YW, Jin JJ, et al. The clinical and prognostic implications of pluripotent stem cell gene expression in hepatocellular carcinoma. Oncol Lett. 2013;5(4):1155–62.
Sullivan KE, Rojas K, Cerione RA, Nakano I, Wilson KF. The stem cell/cancer stem cell marker ALDH1A3 regulates the expression of the survival factor tissue transglutaminase, in mesenchymal glioma stem cells. Oncotarget. 2017;8(14):22325–43.
Nam DH, Ramachandran S, Song DK, et al. Growth inhibition and apoptosis induced in human leiomyoma cells by treatment with the PPAR gamma ligand ciglitizone. Mol Hum Reprod. 2007;13(11):829–36.
Bernal C, Otalora A, Cañas A, et al. Regulatory role of the RUNX2 transcription factor in lung cancer apoptosis. Int J Cell Biol. 2022;2022:5198203. Published 2022 Dec 3.
Tew SR, Hardingham TE. Regulation of SOX9 mRNA in human articular chondrocytes involving p38 MAPK activation and mRNA stabilization. J Biol Chem. 2006;281(51):39471–9.
Suarez-Arnedo A, Torres Figueroa F, Clavijo C, Arbeláez P, Cruz JC, Muñoz-Camargo C. An image J plugin for the high throughput image analysis of in vitro scratch wound healing assays. PLoS ONE. 2020;15(7):e0232565.
Dominici M, Le Blanc K, Mueller I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The international society for cellular therapy position statement. Cytotherapy. 2006;8(4):315–7.
Manocha E, Consonni A, Baggi F, et al. CD146 + pericytes subset isolated from human micro-fragmented fat tissue display a strong interaction with endothelial cells: a potential cell target for therapeutic angiogenesis. Int J Mol Sci. 2022;23(10):5806.
Sacchetti B, Funari A, Michienzi S et al. Self-renewing osteoprogenitors in bone marrow sinusoids can organize a hematopoietic microenvironment [published correction appears in cell. 2008;133(5):928]. Cell. 2007;131(2):324–336.
Crisan M, Yap S, Casteilla L, et al. A perivascular origin for mesenchymal stem cells in multiple human organs. Cell Stem Cell. 2008;3(3):301–13.
Brosens JJ, Parker MG, McIndoe A, Pijnenborg R, Brosens IA. A role for menstruation in preconditioning the uterus for successful pregnancy. Am J Obstet Gynecol. 2009;200(6):615.e1–615.e6156.
Watt SM, Gullo F, van der Garde M, et al. The angiogenic properties of mesenchymal stem/stromal cells and their therapeutic potential. Br Med Bull. 2013;108(1):25–53.
Epstein SE, Kornowski R, Fuchs S, Dvorak HF. Angiogenesis therapy: amidst the hype, the neglected potential for serious side effects. Circulation. 2001;104(1):115–9.
Lee J, Basak JM, Demehri S, Kopan R. Bi-compartmental communication contributes to the opposite proliferative behavior of Notch1-deficient hair follicle and epidermal keratinocytes. Development. 2007;134(15):2795–806.
Brew K, Nagase H. The tissue inhibitors of metalloproteinases (TIMPs): an ancient family with structural and functional diversity. Biochim Biophys Acta. 2010;1803(1):55–71.
Murphy G. Tissue inhibitors of metalloproteinases. Genome Biol. 2011;12(11):233. Published 2011 Nov 11.
Unruh D, Horbinski C. Beyond thrombosis: the impact of tissue factor signaling in cancer. J Hematol Oncol. 2020;13(1):93. Published 2020 Jul 14.
Prudovsky I. Cellular mechanisms of FGF-stimulated tissue repair. Cells. 2021;10(7):1830.
Herbert SP, Stainier DY. Molecular control of endothelial cell behaviour during blood vessel morphogenesis. Nat Rev Mol Cell Biol. 2011;12(9):551–64.
Ma S, Hirata T, Arakawa T, et al. Expression of ALDH1A isozymes in human endometrium with and without endometriosis and in ovarian endometrioma. Reprod Sci. 2020;27(1):443–52.
Melnik S, Werth N, Boeuf S, et al. Impact of c-MYC expression on proliferation, differentiation, and risk of neoplastic transformation of human mesenchymal stromal cells. Stem Cell Res Ther. 2019;10(1):73.
Fahey E, Doyle SL. IL-1 family cytokine regulation of vascular permeability and angiogenesis. Front Immunol. 2019;10:1426.
As MN, Deshpande R, Kale VP, Bhonde RR, Datar SP. Establishment of an in ovo chick embryo yolk sac membrane (YSM) assay for pilot screening of potential angiogenic and anti-angiogenic agents. Cell Biol Int. 2018;42(11):1474–83.
Nowak-Sliwinska P, Segura T, Iruela-Arispe ML. The chicken chorioallantoic membrane model in biology, medicine and bioengineering. Angiogenesis. 2014;17(4):779–804.
Tardalkar K, Desai S, Adnaik A, Bohara R, Joshi M. Novel approach toward the generation of tissue engineered heart valve by using combination of antioxidant and detergent: a potential therapy in cardiovascular tissue engineering. Tissue Eng Regen Med. 2017;14(6):755–62.
Leker RR, Toth ZE, Shahar T, et al. Transforming growth factor alpha induces angiogenesis and neurogenesis following stroke. Neuroscience. 2009;163(1):233–43.
Tu T, Zhang C, Yan H, et al. CD146 acts as a novel receptor for netrin-1 in promoting angiogenesis and vascular development. Cell Res. 2015;25(3):275–87.
Addison CL, Daniel TO, Burdick MD, et al. The CXC chemokine receptor 2, CXCR2, is the putative receptor for ELR + CXC chemokine-induced angiogenic activity. J Immunol. 2000;165(9):5269–77.
Acknowledgements
Dr. Meghnad G. Joshi and Prof. Rakesh Kumar Sharma acknowledges the research funding support from the D.Y. Patil Education Society, Institution Deemed to be University, Kolhapur (DYPES/DU/R&D/2023/261 and DYPS/DU/R&D/2023/259).
Funding
This study was funded by the D.Y. Patil Education Society, Institution Deemed to be University, Kolhapur (DYPES/DU/R&D/2023/261 and DYPS/DU/R&D/2023/259).
Author information
Authors and Affiliations
Contributions
M. J. conceived the study and designed the experiments. PH, AB, DP, GT and IS performed the experiments, AM helped in histology analysis. PH., AB., TM, SI and MJ reviewed, analyzed and interpreted the data. PH, TM and MJ wrote the manuscript. All authors contributed to the analysis of the data and discussed the manuscript. All authors whose names appear on the manuscript, agreed with the content and all gave explicit consent to submit.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was conducted following the guidelines outlined by the Institutional Review Board (IRB) and approved by Institutional Ethics Committee (IEC) of D. Y. Patil Education Society, Deemed to be University, Kolhapur. The approval was obtained on 14/05/2018 for ‘Role of CD146 in Endometrial Stem Cells and Angiogenesis under Normal and Diseased Conditions’ with number DMCK/ i59/ 2018.
Written informed consent was obtained from all participants prior to their inclusion in study. Participants were informed about the objective of the study, procedures and potential benefits. All procedures were performed in accordance with the principles of the Declaration of Helsinki.
Consent for publication
On behalf of all authors, the corresponding authors states that all authors have consent for publication.
Competing interests
The authors declare that they have no financial or non-financial competing interests that could be perceived to influence the conduct or reporting of this research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hilage, P., Birajdar, A., Marsale, T. et al. Characterization and angiogenic potential of CD146+ endometrial stem cells. Stem Cell Res Ther 15, 330 (2024). https://doi.org/10.1186/s13287-024-03918-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-024-03918-7