Abstract
Background
The long-term clinical status of coronavirus disease 2019 (COVID-19) in recovered patients remains largely unknown. This prospective cohort study evaluated clinical status of COVID-19 and explored the associated risk factors.
Methods
At the outpatient visit, patients underwent routine blood tests, physical examinations, pulmonary function tests, 6-min walk test, high-resolution computed tomography (CT) of the chest, and extrapulmonary organ function tests.
Results
230 patients were analyzed. Half (52.7%) reported at least one symptom, most commonly fatigue (20.3%) and sleep difficulties (15.8%). Anxiety (8.2%), depression (11.3%), post-traumatic symptoms (10.3%), and sleep disorders (26.3%) were also reported. Diffusion impairments were found in 35.4% of the patients. Abnormal chest CT scans were present in 63.5% of the patients, mainly reticulation and ground-glass opacities. Further, a persistent decline in kidney function was observed after discharge. SARS-CoV-2-specific antibodies of IgA, IgG, and IgM were positive in 56.4%, 96.3%, and 15.2% of patients, respectively. Multivariable logistic regression showed that disease severity, age, and sex were closely related to patient recovery.
Conclusions
One year after hospital discharge, patients recovered from COVID-19 continued to experience both pulmonary and extrapulmonary dysfunction. While paying attention to pulmonary manifestations of COVID-19, follow-up studies on extrapulmonary manifestations should be strengthened.
Similar content being viewed by others
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the pathogen causing coronavirus disease 2019 (COVID-19). The COVID-19 epidemic has resulted in huge challenges to global public health and heavy economic and social burdens. As of 29 December 2021, SARS-CoV-2 has infected over 281 million individuals, worldwide, and caused over 5.4 million deaths [1]. Over time, most discharged patients have experienced phases of recovery, but the long-term health effects are still emerging [2].
SARS-CoV-2 mainly invades the lungs during the acute stage, manifesting as pneumonia and acute respiratory distress syndrome [3]. Nevertheless, COVID-19 infections are distinguished by multiple system lesions, leading to multiple extrapulmonary manifestations [4], including thrombotic complications [5], heart injury [6], acute kidney injury [7], gastrointestinal symptoms, liver cell injury, metabolic system abnormalities, and neurologic disease [8]. Previous studies have explored the lung function changes in patients with COVID-19 during the recovery period and identified persistent symptoms [9,10,11]. Similar long-term health consequences were reported following infections with the related SARS and Middle East respiratory syndrome (MERS) viruses [12]. However, patients with COVID-19 are more likely to demonstrate multiple organ effects, including in the respiratory, endocrine, neural (psychological), and cardiovascular systems [13,14,15,16,17,18,19]. However, long-term follow-up studies investigating multiple organ function in recovered patients are lacking.
Here, we report a comprehensive evaluation of the pulmonary and extrapulmonary dysfunction, and the associated risk factors, observed in patients with COVID-19 1 year following their discharge from the hospital.
Methods
Study design and participants
This cohort study included patients with COVID-19 admitted to Shenzhen Third People's Hospital, which is the only hospital designated for the treatment of patients with COVID-19 in Shenzhen, Guangdong, China. Between January 11 and April 27, 2020, 462 patients with COVID-19 were hospitalized. Patients were excluded if they were younger than 16 years, died within 1 year of discharge, refused to participate, were lost to contact, and lived outside of Shenzhen city. The research protocol was approved by the Ethics Committee of Shenzhen Third People's Hospital (IRB 2020-021-02). All patients provided written informed consent.
Data collection and follow-up
Demographic characteristics, laboratory data, and acute-phase medical histories were retrospectively collected from hospital electronic medical records. The acute phase of COVID-19 was defined as the period from symptom onset to hospital discharge. Disease severity was classified into the following categories according to the four severity grades from the clinical guidance for COVID-19 pneumonia diagnosis and treatment, issued by the Chinese National Health Commission: (1) mild illness, patients with mild symptoms and without radiological evidence; (2) moderate illness, patients with fever, respiratory tract symptoms, and radiological evidence of confirmed pneumonia; (3) severe illness, patients with one of the following: (a) respiratory distress (≥ 30 breaths/min); (b) oxygen saturation ≤ 93% at rest; (c) arterial partial pressure of oxygen/fraction of inspired oxygen ≤ 300 mmHg; (4) critical illness, patients with one of the following: (a) respiratory failure requiring mechanical ventilation; (b) shock; (c) other organ failure that requires intensive care unit (ICU) [20, 21]. All discharged patients met uniform discharge standards: no fever for three consecutive days, improved respiratory symptoms, obvious recovery of acute lung lesions, and two negative SARS-CoV-2 test results, 24 h apart. Two months before the start of the follow-up, a nurse contacted each patient, by telephone, and invited them to participate in this study. The patients were contacted in the order of their recorded discharge date. Pulmonary and extrapulmonary functions were evaluated in the outpatient clinic between December 26, 2020 and June 19, 2021.
General symptom and psychological symptom
Participants completed a 21-item symptom questionnaire to report new and persistent symptoms and any symptoms that were more severe than before COVID-19 onset. Patients participated in face-to-face interviews with an experienced psychologist and were asked to complete four psychological questionnaires: anxiety symptoms were assessed using the Generalized Anxiety Disorder 7-item (GAD-7) scale, depression symptoms using the Patient Health Questionnaire-9 (PHQ-9), post-traumatic stress symptoms (PTSS) using the Post-traumatic Stress Disorder (PTSD) Checklist (PCL-5), and sleep disorders using the Pittsburgh Sleep Quality Index (PSQI). Psychological abnormalities were determined using generally the accepted cut-off values (PHQ-9 ≥ 7, GAD-7 ≥ 7, PCL-5 ≥ 33, and PSQI ≥ 7) [22].
Pulmonary function test and exercise capacity
Pulmonary function tests were performed using a flow spirometer and the lung diffusing capacity for carbon monoxide (DLCO) was measured using the single breath method. Pulmonary function parameters included forced vital capacity (FVC), forced expiratory volume in one second (FEV1), FEV1/FVC, DLCO, total lung capacity (TLC), and residual volume (RV). Diffusion dysfunction was diagnosed when the DLCO was less than 80% of predicted. The 6-min walk test was performed according to the established protocol [23].
Chest CT scan
High-resolution chest computed tomography (CT) scans were performed with the patient in the supine position at end-inspiration using a uCT 760 scanner (United Imaging, Shanghai, China). The following characteristics of the chest CT scan were recorded: ground-glass opacity (GGO), crazy paving, reticulation, honeycombing, parenchymal bands, consolidation, air trapping, and bronchiectasis. The distribution of pulmonary lesions was described as peripheral, random, or diffuse. To quantify the severity of the lung involvement, a severity score for each lung lobe was determined as the percentage of involvement [24, 25]: no involvement, less than 5% involvement, 5–25% involvement, 26–49% involvement, 50–75% involvement, more than 75%, with corresponding scores of 0, 1, 2, 3, 4, or 5, respectively. The total CT severity score was calculated by summing the scores for all five lung lobes (range, 0–25).
Extrapulmonary organ function test
Participants underwent a series of extrapulmonary organ function tests, including kidney function tests, serological marker measurements, and ultrasound evaluations of the abdomen and deep veins of the lower limbs. Kidney abnormalities were evaluated using blood and urine laboratory indicators related to renal function, including estimated glomerular filtration rate (eGFR), blood urea nitrogen (BUN), proteinuria, urea α1-microglobulin (A1M), and urea β2-microglobulin (B2M). The calculation of eGFR was based on the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation. The serological markers related to disease severity determined were the levels of C-reactive protein (CRP), interleukin 6 (IL-6), lactate dehydrogenase (LDH), and D-dimer.
SARS-CoV-2 antibody test
Plasma samples collected during the acute and follow-up phases were analyzed to assess anti-SARS-CoV-2 total immunoglobulin (i.e., IgA, IgM, and IgG) levels. Commercial enzyme-linked immunosorbent assays (Wantai, Beijing, China), involving magnetic particles coated with receptor-binding domain (RBD) antigens, were performed on the Caris200 automatic chemiluminescence instrument, according to the manufacturer’s protocol. The sample’s cut-off index (COI) = RLU/CO, where RLU is the specimen’s chemiluminescence reaction signal value, and CO is the cut-off value. Specimen’s COI ≥ 1was considered to be positive.
Statistical analysis
Categorical variables are reported as frequencies and percentages. Continuous variables are expressed as means (standard deviation, SD) or medians (interquartile range, IQR). To compare between-group demographic and clinical variables, Chi-squared tests or Fisher’s exact tests were used for each categorical variable. Student’s t-test, Wilcoxon signed-rank test, or analysis of variance was used for continuous variables, as appropriate. Associations between two continuous variables were explored using Pearson or Spearman correlation analyses. Multivariable logistic regression models were used to determine the risk factors associated with the presence of clinical status, and corresponding odds ratios (ORs), with 95% confidence intervals (95% CIs), were calculated by adjusting for age, sex, and disease severity. Statistical significance was defined as a two-sided P value < 0.05. Statistical analyses were performed using R (Version 3.5.1).
Results
Patient characteristics
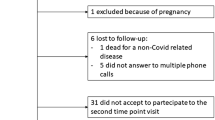
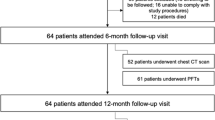
A total of 230 underwent follow-up assessments in the outpatient clinic between December 26, 2020 and June 19, 2021 (flowchart shown in Fig. 1, Additional file 1: Table S1). Overall, the numbers of included patients with mild, moderate, severe, and critical disease were 12 (5.2%), 166 (72.2%), 45 (19.6%), and 7 (3.0%), respectively. The mean age of the 230 included patients was 46.2 years, and 114 (49.6%) were female. The median follow-up time was 385 days, post-discharge. Comorbidities were present in 50 (21.7%) patients. The median length of hospital stay was 21 days, with 14 (6.1%) patients having severe disease spending time in the ICU (median stay, 12 days). Compared with patients having non-severe disease, patients with severe disease were more likely to be male, older, have longer hospitalization, and have more comorbidities (Table 1).
General symptoms and psychological symptoms
General symptoms were assessed in 222 patients at the 1-year follow-up; 52.7% (117 of 222) reported at least one symptom (Additional file 1: Table S2). The most commonly reported symptom was fatigue (20.3%), followed by sleep difficulties (15.8%). Among patients in the severe group, 62.5% of (31 of 50) patients reported ongoing or new symptoms compared with 50.0% (86 of 176) in the non-severe group (Fig. 2). Additionally, chest tightness and cough were significantly more common in patients in the severe group than in those in the non-severe group. Psychological symptoms were evaluated in 194 patients (Additional file 1: Table S2); 70 (36.1%) reported at least one psychological symptom. The prevalences of anxiety, depression, PTSS, and sleep disorders were 8.2%, 11.3%, 10.3%, and 26.3%, respectively, with no statistically significant differences between the non-severe and severe groups.
Pulmonary assessment
Pulmonary function tests were performed in 113 patients at the 1-year follow-up (Table 2, Additional file 1: Table S3). Diffusion impairment was the most common pulmonary function abnormality, and was 40 (35.4%) patients and 10 (8.8%) had DLCO and DLCO/alveolar volume (VA) below 80% of predicted values. FVC (3.5% of patients), FEV1 (8.0%), TLC (8.0%), and RV (1.8%) abnormalities were also observed. A borderline significant difference in DLCO was found between patients in the severe and non-severe group, with a mean value of 86% of predicted in the non-severe group and 80% of predicted in the severe group. Between-group differences were not observed for FEV1, FVC, or FEV1/FVC; however, there were significant between-group differences in DLCO/VA, TLC, and RV. A total of 187 patients completed the 6-min walking test at follow-up, walking a median distance of 478 (IQR, 333–580) meters. The 6-min walking distance for patients in the severe group (415 m) was shorter than that for those in the non-severe group (499 m).
Follow-up chest CT scans were performed on 208 patients (Table 2, Additional file 1: Table S3), with pulmonary abnormalities (bilateral involvement and peripheral and diffuse distribution) observed in 132 (63.5%) patients. The most common CT findings were reticulation (40.4%) and GGO (39.4%). The mean total CT score was 2.29 in the patients with severe disease, which was significantly higher than that for patients in the non-severe group. The total CT score showed a linear increase that was observed to correspond with the incremental increase in disease severity (Fig. 3). The total CT score was negatively correlated with pulmonary parameters (Additional file 1: Fig. S1), including FEV1/FVC, DLCO, DLCO/VA, and RV. There was no difference in total CT score in patients with DLCO < 80% and those with DLCO ≥ 80% (3.18 vs 1.85, P = 0.056) (Additional file 1: Table S4).
Extrapulmonary organ assessment
Kidney function tests were evaluated in 214 patients (Additional file 1: Table S5). At the 1-year follow-up, 28.5% of patients had decreased eGFR (< 90 mL/min/1.73 m2) and fewer patients (19.5%) had proteinuria. A comparison of kidney function parameters between the non-severe and severe patient groups showed a significant difference in the proportions of patients with decreased eGFR (patients in severe group, 45.7%; patients in non-severe group, 23.8%; P = 0.006). Kidney function parameters, including BUN, proteinuria frequency, and urea A1M and B2M levels, were significantly elevated in patients in the severe group. A dynamic analysis of eGFR revealed that kidney function decreased from 1 to 6 months follow-up for patients in both the non-severe and severe groups (Fig. 4). Lower limb deep vein thrombosis was not observed in the 106 participants who underwent ultrasound examinations. Biomarkers related to COVID-19 severity, such as CRP, D-dimer, LDH, and IL-6 levels, were higher in patients in the severe group than in those in the non-severe group (Additional file 1: Table S6).
SARS-CoV-2 antibody
SARS-CoV-2 antibody results were obtained for 222 patients at the 1-year follow-up (Additional file 1: Table S7); 126 (56.8%) patients were positive for IgA antibodies, 213 (95.9%) for IgG antibodies, and 34 (15.4%) for IgM antibodies. Among the 222 patients, antibody results from both the acute phase (average detection time, 6.87 days, post-admission) and 1-year follow-up were available for 163 patients. Compared with the acute-phase concentrations, the titers for all three antibody types were significantly decreased at the follow-up assessment (Fig. 5A). The 49 patients in the severe group had significantly higher IgA and IgG levels than did the 173 patients in the non-severe group (Fig. 5B).
SARS-CoV-2 RBD-specific antibody levels in recovery patients with COVID-19. A Levels of anti-RBD IgA, IgG, and IgM antibodies in 163 recovery patients at acute phase and 1-year follow-up. The difference was determined by the paired samples Wilcoxon test. B Levels of anti-RBD IgA, IgG, and IgM between 173 non-severe patients and 49 severe patients at 1-year follow-up. The difference between two groups was determined by the Wilcoxon test. COI, cut-off Index. ns, P > 0.05; **, P ≤ 0.01; ***, P ≤ 0.001
Risk factors associated with health status
Multivariable logistic regression models were applied to assess associations between demographic and clinical factors and health-related status (Additional file 1: Table S8). Age greater than 50 years was positively associated with anxiety, depression, PTSS, and sleep difficulties. Female sex and severe illness were independent risk factors of diffusion impairment. Age and severe illness were associated with radiological abnormalities. Age and male sex were associated with a higher risk of decreased eGFR (< 90 mL/min/1.73 m2). Disease severity was a significant indicator of decreased IgG levels (> 50%).
Discussion
This long-term follow-up study assessed multiple system damage in patients with COVID-19, 1 year after their hospital discharge. We found that more than half of the patients reported at least one symptom. A considerable percentage of patients demonstrated continuing abnormal pulmonary functions, especially diffusion impairment and radiological abnormalities. Moreover, extrapulmonary organ manifestations were also observed in recovered patients, the decline in kidney function is particularly pronounced. SARS-CoV-2-specific IgG antibodies remained positive in most patients.
This study revealed that a wide range of physical and psychological symptoms persist in patients for at least 1 year after being hospitalized due to COVID-19. Specifically, 51% of patients had at least one symptom, with fatigue (20.7%) and sleeping difficulties (15.0%) being the most common. These results are consistent with short-term follow-up studies assessing the prevalence of post-acute COVID-19 syndrome [15, 26, 27]. For example, a prospective cohort study that included patients from Wuhan, China, 6 months after their hospital discharge, demonstrated that 76% of the patients reported at least one symptom; 63% reported fatigue (or muscular weakness) and 26% reported sleep difficulties [2]. Our study found that mental health problems were common among discharged patients at the 1-year follow-up. Similarly, a recent systematic review reported a pooled prevalence of 31% for sleep disturbances, 23% for anxiety, and 12% for depression, and revealed an increased prevalence of psychiatric symptoms between mid- and long-term follow-up [28]. Thus, these studies suggest that discharged patients with psychological symptoms may benefit from early psychological support.
The present study found that a considerable proportion of patients had reduced diffusion capacity at the 1-year follow-up. This was consistent with previous results for patients discharged from hospital for 6 months after recovering from COVID-19, where the prevalence of reduced diffusion capacity was 16–52% [2, 29,30,31]. A recent study reported that a third of patients demonstrate reduced gas transfer, as measured by DLCO, 12 months after discharge [9]. Similarly, decreased lung diffusion function was observed in patients who recovered from SARS and MERS infections, after hospitalization or ICU admission, based on the results of a meta-analysis; a pooled prevalence of 24.35% was reported at 6 months [32]. Furthermore, we observed that a considerable proportion of patients demonstrated chest CT scan abnormalities, with reticulation and GGO being most frequent. This is consistent with an earlier study that showed two-thirds of patients having residual radiological abnormalities, predominantly residual GGO and reticulation, 100 days after COVID-19 onset [27].
This study also investigated long-term clinical status in extrapulmonary organs. We and others have shown that angiotensin I converting enzyme 2, the host cell receptor of SARS-CoV-2, is highly expressed in multiple organs, including the lung, heart, kidney, gastrointestinal tract, liver, pancreas, nervous system, and skin [33, 34]. Accordingly, extrapulmonary organ dysfunction have been reported during both the acute and recovery phases [4, 35]. Our kidney function study demonstrated that 28.5% of patients had decreased eGFR (< 90 mL/min/1.73 m2), and 18.9% had proteinuria. This is consistent with earlier findings that 35% of patients have decreased eGFR at their 6-month, post-discharge follow-up assessments [2]. Moreover, a trajectory analysis, using our data and those from a previous study, showed that the eGFR continued to decrease after hospital discharge [36]. The decline of eGFR may partly be due to loss of weight explaining the increase in eGFR at 1 months and then patients recovered, gained weight and muscle increasing plasma creatinine and by such lowering eGFR. Because of the lack of kidney assessment before COVID-19 and a follow-up cohort of health controls, the clinical significance of the decline of eGFR after COVID-19 can be further addressed in longer observational studies. The pathogenic mechanism of the decline of the persistent renal function after recovery from COVID-19 is unclear, possibly related to ongoing inflammation, intrinsic tubular injury, maladaptive repair or regaining muscle after discharge. A previous study demonstrated that the SARS-CoV-2 virus can directly infect human renal tubules, causing renal tubule damage and acute kidney injury [37]. According to a urinary microprotein examination, our study found that indicators of renal tubular damage, such as A1M and B2M, were significantly elevated in the patients in the severe group compared with those in the non-severe group. These data suggest that patients who have recovered from COVID-19 may be at risk of persistent renal dysfunction after hospital discharge.
In this study, we reported SARS-CoV-2-specific antibodies in the convalescent serum of patients at the 1-year follow-up assessment, suggesting that anti-SARS-CoV-2 IgG antibodies are detectable in the majority of patients. This finding corresponds with a recent report that indicated that SARS-CoV-2 infection induces humoral immune responses that remain detectable for at least 11 months [38]. Compared with the concentrations during the acute phase, IgG antibodies were significantly decreased at the follow-up visit. Thus, the durability of the IgG antibodies is questionable; however, evidence from another study of SARS-CoV-1 infections showed that IgG antibodies remained detectable for 36 months [39]. Similarly, the seropositivity rate (50.7–56.1%) persisted for up to 4 years after MERS infection, significantly dropping during the 5th year [40]. Our study also showed that the concentrations of IgG antibodies in patients with non-severe disease were significantly lower than in those who had severe disease; the nine patients who had reverted to being IgG-negative for the SARS-CoV-2 antibodies were in the non-severe group. Thus, the decline in antibodies among patients who have recovered from non-severe disease raises concerns of reinfection after repeated exposure to SARS-CoV-2. Continuous monitoring is warranted to confirm the longevity and potency of the anti-SARS-CoV-2 antibody response.
This study has some limitations. First, our study had a single-center design. However, all patients in Shenzhen city with confirmed COVID-19 were admitted to our hospital, facilitating the generalization of these findings. Second, even though some patients were lost to follow-up, there was no significant difference in the clinical characteristics between included and excluded patients. Third, the baseline patient data, such as pulmonary function tests, were unavailable during hospitalization because of preventing cross infection. Fourth, the results should be interpreted with caution because of the missing data of assessments, such as the missing data on pulmonary function tests and the lack of data on dyspnea at follow-up. Finally, a possible limitation was that we cannot rule out that some of them did not attend outpatient clinics, even if all patients diagnosed with COVID-19 in Shenzhen city were required to be evaluated.
Conclusions
In summary, 1 year after hospital discharge, more than half and one-third of the patients recovering from COVID-19 continued to experience physical and psychological symptoms. Patients continued to experience both pulmonary and extrapulmonary dysfunction. These dysfunctions were more frequent among patients with severe disease.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article and its additional file.
Abbreviations
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- COVID-19:
-
Coronavirus disease 2019
- MERS:
-
Middle East respiratory syndrome
- GAD-7:
-
Generalized Anxiety Disorder 7-item scale
- PHQ-9:
-
Patient Health Questionnaire-9
- PTSS:
-
Post-traumatic stress symptoms
- PCL-5:
-
Post-traumatic Stress Disorder Checklist
- PSQI:
-
Pittsburgh Sleep Quality Index
- D LCO :
-
Diffusing capacity for carbon monoxide
- FVC:
-
Forced vital capacity
- FEV1 :
-
Forced expiratory volume in one second
- TLC:
-
Total lung capacity
- RV:
-
Residual volume
- GGO:
-
Ground-glass opacity
- eGFR:
-
Estimated glomerular filtration rate
- BUN:
-
Blood urea nitrogen
- A1M:
-
Urea α1-microglobulin
- B2M:
-
Urea β2-microglobulin
- CRP:
-
C-reactive protein
- IL-6:
-
Interleukin 6
- LDH:
-
Lactate dehydrogenase
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
WHO. WHO coronavirus disease (COVID-19) dashboard.
Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, Kang L, Guo L, Liu M, Zhou X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220–32.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395(10223):497–506.
Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, Bikdeli B, Ahluwalia N, Ausiello JC, Wan EY, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26(7):1017–32.
Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost JTH. 2020;18(6):1421–4.
Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):811–8.
Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, Li J, Yao Y, Ge S, Xu G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–38.
Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, Collange O, Boulay C, Fafi-Kremer S, Ohana M, et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382(23):2268–70.
Wu X, Liu X, Zhou Y, Yu H, Li R, Zhan Q, Ni F, Fang S, Lu Y, Ding X, et al. 3-month, 6-month, 9-month, and 12-month respiratory outcomes in patients following COVID-19-related hospitalisation: a prospective study. Lancet Respir Med. 2021. https://doi.org/10.1016/S2213-2600(21)00174-0.
Guler SA, Ebner L, Aubry-Beigelman C, Bridevaux PO, Brutsche M, Clarenbach C, Garzoni C, Geiser TK, Lenoir A, Mancinetti M, et al. Pulmonary function and radiological features 4 months after COVID-19: first results from the national prospective observational Swiss COVID-19 lung study. Eur Respir J. 2021. https://doi.org/10.1183/13993003.03690-2020.
Gonzalez J, Benitez ID, Carmona P, Santisteve S, Monge A, Moncusi-Moix A, Gort-Paniello C, Pinilla L, Carratala A, Zuil M, et al. Pulmonary function and radiologic features in survivors of critical COVID-19: a 3-month prospective cohort. Chest. 2021;160(1):187–98.
Hui DS, Wong KT, Ko FW, Tam LS, Chan DP, Woo J, Sung JJ. The 1-year impact of severe acute respiratory syndrome on pulmonary function, exercise capacity, and quality of life in a cohort of survivors. Chest. 2005;128(4):2247–61.
Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, Banerjee A. Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ. 2021;372: n693.
Bellan M, Soddu D, Balbo PE, Baricich A, Zeppegno P, Avanzi GC, Baldon G, Bartolomei G, Battaglia M, Battistini S, et al. Respiratory and psychophysical sequelae among patients with COVID-19 four months after hospital discharge. JAMA Netw Open. 2021;4(1): e2036142.
van den Borst B, Peters JB, Brink M, Schoon Y, Bleeker-Rovers CP, Schers H, van Hees HWH, van Helvoort H, van den Boogaard M, van der Hoeven H, et al. Comprehensive health assessment three months after recovery from acute COVID-19. Clin Infect Dis: Off Publ Infect Dis Soc Am. 2020. https://doi.org/10.1093/cid/ciaa1750.
Moreno-Perez O, Merino E, Leon-Ramirez JM, Andres M, Ramos JM, Arenas-Jimenez J, Asensio S, Sanchez R, Ruiz-Torregrosa P, Galan I, et al. Post-acute COVID-19 syndrome Incidence and risk factors: a mediterranean cohort study. J Infect. 2021;82(3):378–83.
Huang L, Yao Q, Gu X, Wang Q, Ren L, Wang Y, Hu P, Guo L, Liu M, Xu J, et al. 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. Lancet. 2021;398(10302):747–58.
Liu T, Wu D, Yan W, Wang X, Zhang X, Ma K, Chen H, Zeng Z, Qin Y, Wang H, et al. Twelve-month systemic consequences of COVID-19 in patients discharged from hospital: a prospective cohort study in Wuhan, China. Clin Infect Dis Off Publ Infect Dis Soc Am. 2021. https://doi.org/10.1093/cid/ciab703.
Heesakkers H, van der Hoeven JG, Corsten S, Janssen I, Ewalds E, Simons KS, Westerhof B, Rettig TCD, Jacobs C, van Santen S, et al. Clinical outcomes among patients with 1-year survival following intensive care unit treatment for COVID-19. JAMA. 2022;327(6):559–65.
National Health Commission of the People’s Republic of China. Handbook of prevention and treatment of the pneumonia caused by the novel coronavirus (2019-nCoV) (in Chinese) updated, 2020. http://en.nhc.gov.cn/2020-02/06/c_76295.htm, Accessed on 2020.
National Health Commission of the People’s Republic of China. Chinese clinical guidance for COVID-19 pneumonia diagnosis and treatment, updated: 2020. http://kjfy.meetingchina.org/msite/news/show/cn/3337.html, Accessed on 2020.
Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2021;126:252–64.
Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, McCormack MC, Carlin BW, Sciurba FC, Pitta F, et al. An official European respiratory Society/American thoracic society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1428–46.
Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology. 2020;295(3):715–21.
Francone M, Iafrate F, Masci GM, Coco S, Cilia F, Manganaro L, Panebianco V, Andreoli C, Colaiacomo MC, Zingaropoli MA, et al. Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. Eur Radiol. 2020;30(12):6808–17.
Morin L, Savale L, Pham T, Colle R, Figueiredo S, Harrois A, Gasnier M, Lecoq AL, Meyrignac O, et al. 4-Month clinical status of a cohort of patients after hospitalization for COVID-19. JAMA. 2021;325(15):1525–34 (Writing Committee for the CSG).
Sonnweber T, Sahanic S, Pizzini A, Luger A, Schwabl C, Sonnweber B, Kurz K, Koppelstatter S, Haschka D, Petzer V, et al. Cardiopulmonary recovery after COVID-19: an observational prospective multicentre trial. Eur Respir J. 2021. https://doi.org/10.1183/13993003.03481-2020.
Premraj L, Kannapadi NV, Briggs J, Seal SM, Battaglini D, Fanning J, Suen J, Robba C, Fraser J, Cho SM. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis. J Neurol Sci. 2022;434: 120162.
Mo X, Jian W, Su Z, Chen M, Peng H, Peng P, Lei C, Chen R, Zhong N, Li S. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. European Respir J. 2020. https://doi.org/10.1183/13993003.01217-2020.
Shah AS, Wong AW, Hague CJ, Murphy DT, Johnston JC, Ryerson CJ, Carlsten C. A prospective study of 12-week respiratory outcomes in COVID-19-related hospitalisations. Thorax. 2021;76(4):402–4.
Zhao YM, Shang YM, Song WB, Li QQ, Xie H, Xu QF, Jia JL, Li LM, Mao HL, Zhou XM, et al. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors 3 months after recovery. E Clin Med. 2020;25: 100463.
Ahmed H, Patel K, Greenwood DC, Halpin S, Lewthwaite P, Salawu A, Eyre L, Breen A, O’Connor R, Jones A, et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: a systematic review and meta-analysis. J Rehabil Med. 2020. https://doi.org/10.2340/16501977-2694.
Qi F, Qian S, Zhang S, Zhang Z. Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses. Biochem Biophys Res Commun. 2020;526(1):135–40.
Trypsteen W, Van Cleemput J, Snippenberg WV, Gerlo S, Vandekerckhove L. On the whereabouts of SARS-CoV-2 in the human body: a systematic review. PLoS Pathog. 2020;16(10): e1009037.
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, Cook JR, Nordvig AS, Shalev D, Sehrawat TS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–15.
Nugent J, Aklilu A, Yamamoto Y, Simonov M, Li F, Biswas A, Ghazi L, Greenberg J, Mansour S, Moledina D, et al. Assessment of acute kidney injury and longitudinal kidney function after hospital discharge among patients with and without COVID-19. JAMA Netw Open. 2021;4(3): e211095.
Diao B, Wang C, Wang R, Feng Z, Zhang J, Yang H, Tan Y, Wang H, Wang C, Liu L, et al. Human kidney is a target for novel severe acute respiratory syndrome coronavirus 2 infection. Nat Commun. 2021;12(1):2506.
Turner JS, Kim W, Kalaidina E, Goss CW, Rauseo AM, Schmitz AJ, Hansen L, Haile A, Klebert MK, Pusic I, et al. SARS-CoV-2 infection induces long-lived bone marrow plasma cells in humans. Nature. 2021. https://doi.org/10.1038/s41586-021-03647-4.
Cao WC, Liu W, Zhang PH, Zhang F, Richardus JH. Disappearance of antibodies to SARS-associated coronavirus after recovery. N Engl J Med. 2007;357(11):1162–3.
Cheon S, Park U, Park H, Kim Y, Hai Nguyen YT, Aigerim A, Rhee JY, Choi JP, Park WB, Park SW, et al. Longevity of seropositivity and neutralizing antibodies in recovered MERS patients: a 5-year follow-up study. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2021. https://doi.org/10.1016/j.cmi.2021.06.009.
Acknowledgements
We thank all patients who participated in this study and all of the staff from Shenzhen Third People’s Hospital. We also appreciate the input from Jinghua Wang and Xianjia Ning to the study.
Funding
This study was supported by the National Science Fund for Distinguished Young Scholars (82025022), the Central Charity Fund of Chinese Academy of Medical Science (2020-PT310-009), the Science and Technology Innovation Committee of Shenzhen Municipality (JSGG20200225152848007, JSGG20200207155251653, and JSGG20220226090002003), and the Emergency Key Program of Guangzhou Laboratory (EKPG21-29). The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
LL, ZZ, GL and QH designed this study; ZM, LZ, JD, GZ, MZ, and WP collected the data; DL, XL, LW, ZL, YK, LW, DL, FW analyzed and interpreted the data; DL and XL wrote the manuscript; LL, ZZ, GL and QH revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Shenzhen Third People's Hospital (IRB 2020-021-02). All patients provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors have declared no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Fig S1. Correlation between total CT score and pulmonary function parameters. Table S1. Baseline characteristics of discharged patients with COVID-19 who were followed up compared with who were not. Table S2. General symptoms and psychological symptoms in recovery patients with COVID-19 at 1-year follow-up. Table S3. Pulmonary function test, 6-min walking test, and CT scan at 1-year follow-up. Table S4. Comparison of CT finding according to diffusion capacity of the lung for carbon monoxide. Table S5. The kidney function in recovery patients with COVID-19 at 1-year follow-up. Table S6. Laboratory biomarkers in recovery patients with COVID-19 at 1-year follow-up. Table S7. SARS-CoV-2 RBD-specific antibody levels and seropositive rate in recovery patients with COVID-19 at 1-year follow-up. Table S8. Risk factors associated with psychological symptoms, diffusion impairment, radiological abnormalities, decreased eGFR, and decreased IgG.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, D., Liao, X., Ma, Z. et al. Clinical status of patients 1 year after hospital discharge following recovery from COVID-19: a prospective cohort study. Ann. Intensive Care 12, 64 (2022). https://doi.org/10.1186/s13613-022-01034-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-022-01034-4