Abstract
Background
Numerous studies have explored care interventions to improve the psychological outcome of intensive care unit (ICU) patients, but inconclusive evidence makes it difficult for decision-makers, managers, and clinicians to get familiar with all available literature and find appropriate interventions. This umbrella review aimed to analyze the relationship between care intervention and psychological outcomes of ICU patients based on existing systematic reviews.
Methods
An umbrella review of evidence across systematic reviews and meta-analyses published between 1987 and 2023 was undertaken. We systematically searched reviews that examined the association between care intervention and the improvement of adverse psychological outcomes in ICU patients using PubMed, EMBASE, Web of Science, Cochrane Library, and manual reference screening. The measurement tool (AMSTAR 2) was applied to evaluate the methodological quality of included studies. The excess significance bias, between-study heterogeneity expressed by I2, small-study effect, and evidence class were estimated.
Results
A total of 5110 articles were initially identified from the search databases and nine of them were included in the analysis. By applying standardized criteria, only weak evidence was observed in 13 associations, even though most included reviews were of moderate to high methodological quality. These associations pertained to eight interventions (music therapy, early rehabilitation, post-ICU follow-up, ICU diary, information intervention, preoperative education, communication and psychological support, surrogate decision-making) and five psychological outcomes (post-intensive care syndrome, transfer anxiety, post-traumatic stress disorder, anxiety, and depression). Weak or null association was shown among the rest of the associations (e.g., weak association between music therapy and maternal anxiety or stress level).
Conclusions
The evidence of these eight supporting interventions to improve the adverse psychological outcomes of ICU patients and caregivers was weak. Data from more and better-designed studies with larger sample sizes are needed to establish robust evidence.
Similar content being viewed by others
Background
Advanced technologies, instruments, and education systems used in intensive care unit (ICU) have significantly reduced the mortality of critically ill patients [1]. However, the physical and mental abilities of the surviving critically ill patients to resume normal life are impaired to a certain extent [2]. They will suffer from symptoms that affect their physical, mental, and cognitive health for a long time [3].
Several mental disorders including post-intensive care syndrome (PICS) [4], transfer anxiety [5], post-traumatic stress disorder (PTSD) [6], anxiety [7], and depression [8] are commonly found among critically ill survivors. PICS is a new syndrome that is characterized by new or deteriorated physical, cognitive, or mental health impairment after critical illness, and it could persist after acute care hospitalization [4, 9]. “Transfer anxiety” refers to the psychological and physical problems encountered by patients and their families when they are transferred from the intensive care environment to the general ward environment [5, 10]. These persistent physical, cognitive, and mental disorders experienced by ICU survivors might prevent them from returning home after being discharged from the hospital. This means that it is difficult for them to resume normal daily life when they return home. It may also further cause psychological problems such as anxiety and depression in caregivers, which will subsequently affect their ability to recover from severe diseases.
A substantial amount of literature exists on care interventions to improve psychological outcomes among patients admitted to ICU [11, 12]. Each review evaluates its own specific interventions, making it difficult for policymakers, managers, and clinicians to familiarize themselves with all available literature and to determine which interventions should be applied. Therefore, a comprehensive review of the literature is needed to identify and evaluate evidence and then select effective care interventions to improve the psychological status of patients in the ICU, as well as provide more effective suggestions to decision-makers, managers, and clinicians to improve ICU survivors’ health quality.
To achieve this, an “umbrella review” was designed to describe this approach by synthesizing the evidence of published system reviews and selecting reviews based on pre-determined criteria without an in-depth study of the quality of individual major studies included in the original system review [13]; thus, it is defined as “an overview of existing system review” [14]. A systematic review is conducted by systematically searching, evaluating, and synthesizing evidence in accordance with specific guidelines [15]. Therefore, this umbrella review aims to help managers and clinicians find solutions to problems in an evidence-based manner by summarizing the evidence from the systematic reviews and meta-analyses and improving the psychological outcomes of ICU patients.
Methods
We performed this umbrella review systematically to collect and evaluate information from systematic reviews and meta-analyses focusing on care intervention on psychological outcomes among patients admitted to ICU. The umbrella review was carried out under the guidelines for Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). This study was not prospectively registered at the PROSPERO due to unawareness at the beginning of the study.
Search strategy
Two reviewers independently performed a comprehensive search in four electronic databases: PubMed (from 1996 to present), EMBASE (from 1910 to present), Web of Science (from 1956 to present), and the Cochrane Library (from 1995 to present) by using the comprehensive search strategies (Table S1) from inception to January 3, 2023. We limited the search to humans and the English language. Each literature was first reviewed for title and abstract, followed by full-text retrieval of potentially eligible articles. Reference lists of eligible reviews and meta-analyses were searched for additional citations. For gray literature, we searched them through OpenGrey and Google Scholar or directly contacted the author if necessary.
Eligibility criteria and study selection
Two reviewers independently carried out the study selection from the eligible studies based on the following criteria: (1) full-text systematic reviews and meta-analysis published in the English language; (2) searched at least two electronic databases, such as PubMed, EMBASE, Web of Science, and Cochrane Library; and (3) assessing the relationship between care intervention and poor psychological outcome of ICU patients. After removing the duplicated records from screening the title, two reviewers read the full texts independently and removed studies that did not meet the inclusion criteria. For several kinds of literature focusing on the same interventions or including duplicated primary studies, only the latest reviews or meta-analyses with the largest sample size were considered to be included.
Data extraction and quality appraisal
Two reviewers (ZY and ZL) separately extracted the data from the included literature. Data extracted included the following: author, publication time, research type, exposures, exposure contrast, study design, population, main psychological outcomes, number of primary studies selected in the reviews, number of participants, specific relative risk estimates (risk ratio [RR], odds ratio [OR], mean difference [MD], standardized mean difference [SMD], standard error of measurement [SEM], as reported by the authors of the meta-analysis) together with the corresponding 95% confidence intervals (95% CIs), heterogeneity, bias, and evidence class (Table 1). Any disagreement was resolved in consensus with the rest of the team.
Data analysis
According to the criteria for classification of the credibility of the evidence used in the previous umbrella reviews [16, 17], we classified the strength of evidence in the following categories: class I (convincing)—statistical significance at P < 10−6, > 1000 cases (or > 20,000 participants for continuous outcomes), the highest weighted study reported a significant effect (P < 0.05); the 95% prediction interval excluded the null, no large heterogeneity (I2 < 50%), no evidence of small-study effects (P > 0.10), and excess significance bias (P > 0.10); class II (highly suggestive)—significance at P < 10−6, > 1000 cases (or > 20,000 participants for continuous outcomes), the largest component study reported a significant effect (P < 0.05); class III (suggestive)—statistical significance at P < 10−3, > 1000 cases (or > 20,000 participants for continuous outcomes); and class IV (weak)—the remaining significant associations at P < 0.05.
The results were presented based on each intervention and psychological outcomes. For each meta-analysis, we estimated the effect size and its 95% CI using fixed and random effect models [18, 19]. Between-study heterogeneity was estimated by calculating the I2 measure: ≥ 50% values represented high heterogeneity, while > 75% values represented very high heterogeneity [20, 21]. In addition, we used the regression asymptotic test developed by Egger et al. to calculate the evidence of small research effects [22]. We estimated the standard deviation (SD) of the effect size in each meta-analysis to determine if the SD was less than 0.10 in the largest study. Both the small study and excess significance tests were considered significant at P < 0.05, which evaluated whether there were too many studies with significant results (i.e., P < 0.05) based on the effect power sets at α = 0.05 [23]. Statistical analyses were conducted by Stata version 12.1 and P values were two-tailed.
The MeaSurement Tool to Assess Systematic Reviews 2 (AMSTAR 2) checklist [24] was used to evaluate the methodological quality of the included systematic reviews and meta-analyses (Table 2). AMSTAR 2 used sixteen items to assess the methodological quality of systematic reviews based on the validity of review design, literature screening, data extraction, and individual study quality assessment. Among these items, AMSTAR 2 designated seven “critical domains” that can critically affect the validity of a review (e.g., items 2, 4, 7, 9, 11, 13, and 15). Meta-analyses were considered as “high quality” if they met all “critical domains” with other items satisfied ≥ 8, and other meta-analyses that met all “critical domains” were regarded as “medium quality.” Besides, meta-analyses with one unsatisfied critical domain were assigned to “low quality,” and meta-analyses with more than one unsatisfied critical domain were considered as “critically low quality” [24].
Results
Results of the search process
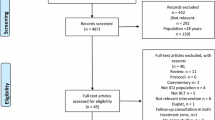
A total of 5110 articles were retrieved from four databases. Of them, 2514 duplicates were removed, and 2317 articles were excluded after screening the titles and abstracts (1624 traditional reviews, reviews, and academic reports; 693 animal and other unrelated studies). Assessment of full-text screening resulted in the exclusion of 270 articles, including 188 articles excluded due to missing psychiatric outcomes, 69 lacking important relevant data, 11 studies investigating duplicate interventions [33,34,35,36,37,38,39,40,41,42,43], and 2 publications being a protocol [44, 45]. Subsequently, 9 articles were included in the umbrella review (Table S2). The flow chart of the study selection is depicted in Fig. 1.
Description of included systematic reviews
The publication dates of the 9 reviews ranged from 2012 to 2022. The publication dates of the reviews ranged from 1987 to 2020. There were 127 trials. The participant numbers were up to 55,000. The general characteristics of the systematic reviews are presented in Table 1. The majority of the reviews were graded as “medium” to “high quality” based on the AMSTAR 2 score. However, the evidence class of most reviews included was weak. A summary of the quality appraisals of the reviews and the AMSTAR 2 scores are presented in Table 2.
Review findings
The 9 systematic reviews evaluated 8 interventions: music therapy, early rehabilitation, post-ICU follow-up, ICU diary, information intervention, preoperative education, communication and psychological support, and surrogate decision-making.
Music therapy
Music therapy refers to the use of music-based interventions within a therapeutic relationship to accomplish individualized goals [25]. Two reviews previously examined the effectiveness of music on intensive care patients [25, 29]. Of them, Yue et al. [25] reviewed the impact of music therapy on neonates in ICU and found that music therapy had a significant influence on preterm infants’ heart rate and respiratory rate and exerted a beneficial effect on oral feeding volume. In addition, music therapy was also found to play a role in reducing maternal anxiety [25]. However, due to the heterogeneity across studies in some outcomes, further studies with larger sample sizes and more stringent designs are needed [25]. Another review was to explore the impact of music therapy on the physiological and psychological stress response of patients in ICU [29]. Music was found to significantly reduce anxiety scores with an SMD of − 1.97 (95% CI = − 3.66 to − 0.28; n = 6) compared to standard care (P = 0.02), but there was no significant change in anxiety scores in comparison with the noise cancellation group (P = 0.14) [29]. It was found that multiple music sessions reduced the anxiety level better than a single music session [29].
Intensive care unit diaries
Intensive care unit diaries include the daily events of patients and may allow patients to reconstruct their experience [3]. A review conducted by Gazzato et al. included 7 RCTs and examined the effect of ICU diaries on PTSD, anxiety, and depression [3]. They found patients who received a diary during the ICU admission had a reduced rate of PTSD (78/432 [18%] vs. 106/422 [25%]; RR = 0.73 [95% CI, 0.57 to 0.94; n = 6]; P = 0.02; I2 = 0%; trial sequential analysis-adjusted CI, 0.55 to 0.97), compared to patients who did not receive a diary [3].
Early rehabilitation
One review included six randomized controlled trials (RCTs) examining the effectiveness of early rehabilitation for the prevention of PICS, which was characterized by an impaired physical, cognitive, or mental health status, among survivors of critical illness [9, 26]. This review found that early rehabilitation significantly improved short-term physical-related outcomes, as indicated by an increased Medical Research Council scale score (SMD = 0.38 [95% CI, 0.10 to 0.66; n = 3], P = 0.009, qualify of evidence [QoE]: low) and a decreased incidence of ICU-acquired weakness (OR = 0.42 [95% CI, 0.22 to 0.82; n = 2], P = 0.01, QoE: low), compared with standard care or no early rehabilitation [26]. However, these two groups did not differ in terms of cognitive-related delirium-free days (SMD = − 0.02 [95% CI = − 0.23 to 0.20; n = 2], QoE: low) and the mental health-related hospital anxiety and depression scale score (OR = 0.79 [95% CI = 0.29 to 2.12; n = 2], QoE: low) [26].
Post-ICU follow-up
Post-ICU follow-up aimed to minimize post-ICU burden for patients, families, and the health care system. Based on 26 studies, one review synthesized data on subject outcomes associated with post-ICU follow-up [27]. In an RCT, post-ICU follow-up models focusing on physical therapy were associated with fewer depression symptoms (MD = − 1.21 [95% CI, 2.31 to − 0.11; n = 4]; I2 = 0%) and better mental health-related quality of life scores (SMD = 0.26 [95% CI, 0.02 to 0.51; n = 4]; I2 = 6%) in the short term [27]. Post-ICU follow-up models focusing on psychological or medical management interventions were associated with fewer PTSD symptoms (SMD = − 0.21 [95% CI, − 0.37 to − 0.05; n = 4]; I2 = 0%) in the medium term [27].
Information intervention
Information intervention means providing patients and their families with disease-related information or future medical environmental information. Brooke et al. [30] undertook a comprehensive systematic review on the efficacy of information intervention, which might reduce anxiety in patients and family members during the time when patients were transferred from a critical care setting to a general ward. They found family members’ transfer anxiety was significantly reduced in the intervention group of information provision (OR = 1.70 [95% CI, 1.15 to 2.52; n = 4]; P = 0.01), related to those who received standard care (OR = 0.42 [95% CI, 0.28 to 0.63; n = 3]; P < 0.001) [30].
Communication and enhancing psychological support
One review evaluated the efficacy of interventions to improve symptoms for ICU surrogates at the highest risk of developing psychological distress [31]. This study showed that communication and enhancing psychological support from the ICU could alleviate the anxiety, depression, and posttraumatic stress of ICU surrogates facing end-of-life decisions to some extent. Significant improvement was seen at 3 months (depression: MD = − 0.68 [95% CI, − 1.14 to − 0.22; n = 5], moderate certainty; posttraumatic stress: SMD = − 0.25 [95% CI, − 0.49 to − 0.01; n = 6], very low certainty) and 6 months (anxiety: MD = − 0.70 [95% CI, − 1.18 to − 0.22; n = 4], moderate certainty) [31].
Preoperative education interventions
Preoperative education was defined as the basic element to enhance the postoperative recovery path, which aims to provide patients with psychological support information, set health expectations, and promote rehabilitation [46]. Preoperative education was known to positively alter people’s perceptions, and emotions, and mitigate surgical distress [47]. One review examined this intervention’s effectiveness in improving perioperative outcomes among patients undergoing cardiac surgery [28]. They found that preoperative education exerted greatly significant effects on reducing post-intervention preoperative anxiety (P = 0.02) and improving knowledge (P < 0.001), but they also found small significant effect sizes on lowering postoperative anxiety (P < 0.001), depression (P = 0.03), and enhancing satisfaction (P = 0.04) [28].
Surrogate decision-making intervention
Surrogate decision-making (SDM) intervention refers to making important decisions on behalf of critically ill patients during the time when ICU patients’ lose decision-making ability. One review conducted by Bibas et al. [32] determined the association of SDM interventions with patient- and family-centered outcomes and resource use. This review screened 3735 studies, comprising a total of 10,453 patients from 13 RCTs. It includes 4 types of interventions: care professional-led, ethics consultation, palliative care consultation, and media. There was no consistent difference in SDM-related outcomes, including satisfaction with care or perceived quality of care (n = 6) and incident psychological comorbidities (depression: ratio of means = − 0.11 [95% CI, − 0.29 to 0.08; n = 5], P = 0.26; anxiety: ratio of means = − 0.08 [95% CI, − 0.25 to 0.08; n = 5], P = 0.31; or PTSD: ratio of means = − 0.04 [95% CI, − 0.21 to 0.13; n = 4], P = 0.65) [32].
Discussion
Summary of main findings
This umbrella review provided an overview of reported findings on the impact of care intervention on the psychological outcome of ICU patients. Overall, eight classes of interventions have been identified for the association, including ICU diary intervention, music therapy/interventions, early rehabilitation, post-ICU follow-up, preoperative education, information interventions, communication and psychological support interventions, and surrogate decision-making interventions. Most of the selected reviews were of “medium” to “high” methodological quality. After assessing the strength direction, we found that each type of care intervention can improve the psychological outcomes of ICU patients, but this finding was supported by evidence with low epidemiological credibility, as expressed by small sample size and large heterogeneity. Among these studies, one study is not suggestive due to the small-study effect.
On the basis of the results of this umbrella review, ICU diary intervention could reduce the incidence of PTSD symptoms in ICU patients [3]. Communication and psychological support intervention in ICU have made minor but significant improvements in improving the psychological symptoms of relatives who took the place of ICU patients to make terminal decisions [31]. However, our assessment failed to show an overall level of evidence class of this study, and its small-study effect and the medium methodological quality suggested that this evidence should be treated with caution.
Compared with standard daily care, music therapy could not only improve the infant’s eating behavior in ICU premature infants but also alleviate their mother’s anxiety [25]. This may be explained by the influence of music on the periphery and autonomic nervous system of premature infants [48]. Prior research showed that music could help coordinate the function of the cerebral cortex, thereby improving the physiological function of the brain [49]. Ranger et al. also found that music intervention could reduce mothers’ anxiety [50]. Additionally, music intervention involving multiple sessions could be used as a care intervention to control the anxiety level of ICU patients [29]; this might be ascribed to the fact that sound signals might reduce noise and improve harmony more than verbal signals [51]. However, the included meta-analysis did not find a statistically significant effect of music therapy on improving the oxygen saturation or behavioral status of premature infants [25]. This may be related to the kangaroo care effect, which was reported by two experiments that combined kangaroo care and music therapy as intervention measures [52]. The effect of this combined intervention might be partly explained by that thermal stimulation could significantly weaken or mask other stimuli, including various types of music. However, our study suggested that there was probably genuine heterogeneity (92.3%) in the association of music therapy with behavior stats in infants. This high heterogeneity might be not only related to the potential bias in the original studies but also related to the differences across studies included in this meta-analysis. Furthermore, being graded as medium methodological quality, these associations were both supported by a weak level of evidence; thus, more studies are needed to further document the effect of music therapy on mental health in ICU patients.
Providing information to the ICU patients and their caregivers about the future ward environment could significantly reduce their anxiety when transferring patients from the intensive care environment [30]. Despite this study being graded as having high methodological quality, the level of research evidence was weak due to the small number of subjects included in the study. When patients and their families cannot understand the information provided by ICU physicians or get less information, their uncertainty would increase, which would further cause them anxiety. Research showed that uncertainty accounted for 30.2% of the factors that cause family members’ transfer anxiety, and providing information was a key factor in reducing uncertainty and anxiety [52, 53].
With the medium methodological quality, preoperative education was found to be helpful in improving the prognosis of patients undergoing cardiac surgery [28] because it may enhance patients’ knowledge; besides, meeting their information needs could also mitigate their distress [54]. However, our umbrella-shaped review shows that information intervention cannot effectively reduce patients’ transfer anxiety, which may be related to our use of quantitative rather than qualitative methods to investigate transfer anxiety. This indicates that more high-quality systematically conducted studies are needed to better understand the associations between providing information and adverse outcomes in ICU patients.
With high methodological quality, early rehabilitation was found to be effective in the improvement of short-term physical outcomes in critically ill patients [49]. Kayambu et al. [55] consistently found a similar conclusion that physiotherapy in the ICU could improve muscle strength, body function, quality of life, and days without convulsion and reduce ICU hospitalization time and hospitalization time. However, a study has inversely shown that acute rehabilitation may cause great physical pressure and fatigue to ICU patients, thus increasing mortality in the ICU [56]. Nonetheless, the results of the study by Fuke et al. [26] showed that early rehabilitation did not significantly improve the cognitive and mental state of patients. The possible reason for this discrepancy might be that the review shed light on studies that implemented multiple “early rehabilitation” programs, and further analysis of large-scale trials was still needed in the later stage, with detailed records and grouping analysis made on the time, type, and intensity of early rehabilitation. Therefore, whether early rehabilitation contributed to the recovery of intensive care syndrome still needs further research.
Post-ICU follow-up focusing on physical therapy could improve depressive symptoms and mental health-related quality of life in the short term, while post-ICU follow-up focusing on psychological or medical management intervention can improve PTSD symptoms in the medium term [27]. However, the evidence supporting these findings was mainly of weak evidence class, though this association originated from a review with high methodological quality. It may be attributable to the fact that the individual risk factors of ICU patients were not considered when the subjects were included in the study. The high heterogeneity of the ICU population, therefore, may offset the potential benefits of nursing intervention on the adverse psychological outcomes of ICU patients and their caregivers. Optimizing the inclusion criteria for follow-up patients after ICU and conducting specific treatments for subjects, who may benefit from specific rehabilitation strategies, may lead to more accurate intervention effects. Given that these results are mainly from non-randomized studies, which may also be the reason for the low evidence class, carefully designed randomized trials were still needed to further verify the impact of follow-up in ICU on the psychological outcomes of patients and their families.
Alternative SDM itself could only shorten the stay time of dead patients in the ICU, but it would not affect the overall mortality of ICU patients [32]. It might be ascribed that surrogate decision-making is a complex task in the ICU environment, and the prognosis judgment of ICU doctors may be wrong. Thus, the surrogate decision-making interventions may cause patients to lose life support prematurely; otherwise, this part of patients may survive for a longer time [57]. In addition, personal characteristics related to SDM, such as coping strategies and competitive responsibilities, may also affect the effect of this intervention. People who have faced similar situations before tend to do the job better than those who have served as SDM for the first time [58, 59]. With the high methodological quality, the assessments of these meta-analyses related to alternative decision-making intervention had high between-study heterogeneity, as well as their null evidence class, suggesting that there is no clear scientific evidence to support the link between alternative decision-making intervention and adverse outcomes in ICU patients.
Limitation of the overview
This umbrella review has several limitations. Firstly, this review was conducted based on the results of the published systematic review and meta-analysis; thus, it is inevitable to suffer from missing data from the original literature and their relevant literature. However, our result was not greatly affected because the evaluation of repeated meta-analysis led to similar results. Secondly, the statistical method we used to test the existence of bias could only indicate the existence of bias, but could not prove its exact source. Finally, our estimation method was relatively conservative, but the detection showed no bias, which did not rule out the possibility of its existence.
Conclusion
The evidence reviewed here indicates that ICU diary intervention, music therapy, early rehabilitation, post-ICU follow-up, preoperative education, information intervention, communication and psychological support intervention, and alternative decision-making may be beneficial to ICU patients and caregivers. However, further high-quality population experiments are still needed to further demonstrate these associations because the evidence supporting our finding was mainly of null or weak evidence class.
Availability of data and materials
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Abbreviations
- 95% CIs:
-
95% Confidence intervals
- AMSTAR-2:
-
Assessment of Multiple Systematic Reviews 2
- ICU:
-
Intensive care unit
- MD:
-
Mean difference
- OR:
-
Odds ratio
- PICS:
-
Post-intensive care syndrome
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTSD:
-
Post-traumatic stress disorder
- RR:
-
Risk ratio
- SMD:
-
Standardized mean difference
References
Bemis-Dougherty AR, Smith JM. What follows survival of critical illness? Physical therapists’ management of patients with post-intensive care syndrome. Phys Ther. 2013;93(2):179–85.
Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–94.
Gazzato A, Scquizzato T, Imbriaco G, Negro A, CaballoGarrido MC, Landoni G, et al. The effect of intensive care unit diaries on posttraumatic stress disorder, anxiety, and depression: a systematic review and meta-analysis of randomized controlled trials. Dimens Crit Care Nurs. 2022;41(5):256–63.
Lee M, Kang J, Jeong YJ. Risk factors for post-intensive care syndrome: a systematic review and meta-analysis. Aust Crit Care. 2020;33(3):287–94.
Brodsky-Israeli M, DeKeyser GF. Risk factors associated with transfer anxiety among patients transferring from the intensive care unit to the ward. J Adv Nurs. 2011;67(3):510–8.
Levi P, Patrician PA, Vance DE, Montgomery AP, Moss J. Post-traumatic stress disorder in intensive care unit nurses: a concept analysis. Workplace Health Saf. 2021;69(5):224–34.
Lai VKW, Ho KM, Wong WT, Leung P, Gomersall CD, Underwood MJ, et al. Effect of preoperative education and ICU tour on patient and family satisfaction and anxiety in the intensive care unit after elective cardiac surgery: a randomised controlled trial. BMJ Qual Saf. 2021;30(3):228–35.
Liao KM, Ho CH, Lai CC, Chao CM, Chiu CC, Chiang SR, et al. The association between depression and length of stay in the intensive care unit. Medicine. 2020;99(23):e20514.
Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40(2):502–9.
McKinney AA, Deeny P. Leaving the intensive care unit: a phenomenological study of the patients’ experience. Intensive Crit Care Nurs. 2002;18(6):320–31.
Jensen JF, Egerod I, Bestle MH, Christensen DF, Elklit A, Hansen RL, et al. A recovery program to improve quality of life, sense of coherence and psychological health in ICU survivors: a multicenter randomized controlled trial, the RAPIT study. Intensive Care Med. 2016;42(11):1733–43.
Ettenberger M, Maya R, Salgado-Vasco A, Monsalve-Duarte S, Betancourt-Zapata W, Suarez-Cañon N, et al. The effect of music therapy on perceived pain, mental health, vital signs, and medication usage of burn patients hospitalized in the intensive care unit: a randomized controlled feasibility study protocol. Front Psych. 2021;12:714209.
De Freitas L, Goodacre S, O’Hara R, Thokala P, Hariharan S. Interventions to improve patient flow in emergency departments: an umbrella review. Emerg Med J. 2018;35(10):626–37.
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13(3):132–40.
Muka T, Glisic M, Milic J, Verhoog S, Bohlius J, Bramer W, et al. A 24-step guide on how to design, conduct, and successfully publish a systematic review and meta-analysis in medical research. Eur J Epidemiol. 2020;35(1):49–60.
Sterne JA, Smith GD. Sifting the evidence—what’s wrong with significance tests? BMJ. 2001;322(7280):226–31.
Ioannidis JP, Tarone R, McLaughlin JK. The false-positive to false-negative ratio in epidemiologic studies. Epidemiology. 2011;22(4):450–6.
Campbell M, Katikireddi SV, Sowden A, Thomson H. Lack of transparency in reporting narrative synthesis of quantitative data: a methodological assessment of systematic reviews. J Clin Epidemiol. 2019;105:1–9.
Armstrong M, Kupeli N, Flemming K, Stone P, Wilkinson S, Candy B. Complementary therapy in palliative care: a synthesis of qualitative and quantitative systematic reviews. Palliat Med. 2020;34(10):1332–9.
Zhang C, Chen M, Wang X. Statistical methods for quantifying between-study heterogeneity in meta-analysis with focus on rare binary events. Stat Interface. 2020;13(4):449–64.
Ioannidis JP, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ. 2007;335(7626):914–6.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Marx W, Veronese N, Kelly JT, Smith L, Hockey M, Collins S, et al. The Dietary Inflammatory Index and human health: an umbrella review of meta-analyses of observational studies. Adv Nutr (Bethesda, Md). 2021;12(5):1681–90.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Yue W, Han X, Luo J, Zeng Z, Yang M. Effect of music therapy on preterm infants in neonatal intensive care unit: systematic review and meta-analysis of randomized controlled trials. J Adv Nurs. 2021;77(2):635–52.
Fuke R, Hifumi T, Kondo Y, Hatakeyama J, Takei T, Yamakawa K, et al. Early rehabilitation to prevent postintensive care syndrome in patients with critical illness: a systematic review and meta-analysis. BMJ Open. 2018;8(5):e019998.
Rosa RG, Ferreira GE, Viola TW, Robinson CC, Kochhann R, Berto PP, et al. Effects of post-ICU follow-up on subject outcomes: a systematic review and meta-analysis. J Crit Care. 2019;52:115–25.
Ng SX, Wang W, Shen Q, Toh ZA, He HG. The effectiveness of preoperative education interventions on improving perioperative outcomes of adult patients undergoing cardiac surgery: a systematic review and meta-analysis. Eur J Cardiovasc Nurs. 2022;21(6):521–36.
Erbay Dalli Ö, Bozkurt C, Yildirim Y. The effectiveness of music interventions on stress response in intensive care patients: a systematic review and meta-analysis. J Clin Nurs. 2023;32(11-12):2827–45.
Brooke J, Hasan N, Slark J, Sharma P. Efficacy of information interventions in reducing transfer anxiety from a critical care setting to a general ward: a systematic review and meta-analysis. J Crit Care. 2012;27(4):425.e9-15.
DeForge CE, George M, Baldwin MR, South K, Beauchemin M, McHugh ME, et al. Do interventions improve symptoms among ICU surrogates facing end-of-life decisions? A prognostically-enriched systematic review and meta-analysis. Crit Care Med. 2022;50(11):e779–90.
Bibas L, Peretz-Larochelle M, Adhikari NK, Goldfarb MJ, Luk A, Englesakis M, et al. Association of surrogate decision-making interventions for critically ill adults with patient, family, and resource use outcomes: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(7):e197229.
Bieleninik L, Ghetti C, Gold C. Music therapy for preterm infants and their parents: a meta-analysis. Pediatrics. 2016;138(3):e20160971.
Mohan A, Gokulakrishnan G, El-Saie A, Brickley A, Hagan J, Pammi M. Music therapy for preterm neonates in the neonatal intensive care unit: an overview of systematic reviews. Acta Paediatr. 2021;110(12):3180–200.
Standley JM. A meta-analysis of the efficacy of music therapy for premature infants. J Pediatr Nurs. 2002;17(2):107–13.
van der Heijden MJ, OliaiAraghi S, Jeekel J, Reiss IK, Hunink MG, van Dijk M. Do hospitalized premature infants benefit from music interventions? A systematic review of randomized controlled trials. PLoS ONE. 2016;11(9):e0161848.
Sabnis A, Fojo S, Nayak SS, Lopez E, Tarn DM, Zeltzer L. Reducing parental trauma and stress in neonatal intensive care: systematic review and meta-analysis of hospital interventions. J Perinatol. 2019;39(3):375–86.
Nydahl P, Fischill M, Deffner T, Neudeck V, Heindl P. Diaries for intensive care unit patients reduce the risk for psychological sequelae: systematic literature review and meta-analysis. Med Klin Intensivmed Notfmed. 2019;114(1):68–76.
Sun X, Huang D, Zeng F, Ye Q, Xiao H, Lv D, et al. Effect of intensive care unit diary on incidence of posttraumatic stress disorder, anxiety, and depression of adult intensive care unit survivors: a systematic review and meta-analysis. J Adv Nurs. 2021;77(7):2929–41.
McIlroy PA, King RS, Garrouste-Orgeas M, Tabah A, Ramanan M. The effect of ICU diaries on psychological outcomes and quality of life of survivors of critical illness and their relatives: a systematic review and meta-analysis. Crit Care Med. 2019;47(2):273–9.
Barreto BB, Luz M, Rios MNO, Lopes AA, Gusmao-Flores D. The impact of intensive care unit diaries on patients’ and relatives’ outcomes: a systematic review and meta-analysis. Crit Care. 2019;23(1):411.
Kynoch K, Chang A, Coyer F, McArdle A. The effectiveness of interventions to meet family needs of critically ill patients in an adult intensive care unit: a systematic review update. JBI Database System Rev Implement Rep. 2016;14(3):181–234.
Castro-Avila AC, Serón P, Fan E, Gaete M, Mickan S. Effect of early rehabilitation during intensive care unit stay on functional status: systematic review and meta-analysis. PLoS One. 2015;10(7):e0130722.
Li D, Yao Y, Chen J, Xiong G. The effect of music therapy on the anxiety, depression and sleep quality in intensive care unit patients: a protocol for systematic review and meta-analysis. Medicine (Baltimore). 2022;101(8):e28846.
Zhou C, Ma H, Qi X, Xu C, Liang Z. The effect of music therapy on delirium in patients receiving mechanical ventilatory support in the Intensive Care Unit: a protocol for systematic review and meta-analysis. Medicine (Baltimore). 2023;102(24):e33956.
Bumin Aydın G, Sakızcı UB. Mothers level of education and preoperative informative story book reading helps reduce preoperative anxiety in children in Turkey. J Pediatr Nurs. 2021;60:e19–23.
Zilla P, Yacoub M, Zühlke L, Beyersdorf F, Sliwa K, Khubulava G, et al. Global unmet needs in cardiac surgery. Glob Heart. 2018;13(4):293–303.
Anderson DE, Patel AD. Infants born preterm, stress, and neurodevelopment in the neonatal intensive care unit: might music have an impact? Dev Med Child Neurol. 2018;60(3):256–66.
Vuust P, Heggli OA, Friston KJ, Kringelbach ML. Music in the brain. Nat Rev Neurosci. 2022;23(5):287–305.
Ranger A, Helmert E, Bott TS, Ostermann T, Als H, Bassler D, et al. Physiological and emotional effects of pentatonic live music played for preterm neonates and their mothers in the newborn intensive care unit: a randomized controlled trial. Complement Ther Med. 2018;41:240–6.
Arya S, Naburi H, Kawaza K, Newton S, Anyabolu CH, Bergman N, et al. Immediate “kangaroo mother care” and survival of infants with low birth weight. N Engl J Med. 2021;384(21):2028–38.
Guan T, Santacroce SJ, Chen DG, Song L. Illness uncertainty, coping, and quality of life among patients with prostate cancer. Psychooncology. 2020;29(6):1019–25.
Xia BY, Yu JM, Wu XY. Illness uncertainty and its associated factors in coronary heart disease patients with heart stent implantation: a cross-sectional study. Annals of palliative medicine. 2022;11(7):2410–21.
DurmazEdeer A, Vural F, TurhanDamar H, Yasak K, Damar M. The effect of web-based preoperative and postoperative patient care education on nursing students: a randomized controlled study. Comput Inform Nurs. 2019;37(10):541–7.
Kayambu G, Boots R, Paratz J. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med. 2013;41(6):1543–54.
Greening NJ, Williams JE, Hussain SF, Harvey-Dunstan TC, Bankart MJ, Chaplin EJ, et al. An early rehabilitation intervention to enhance recovery during hospital admission for an exacerbation of chronic respiratory disease: randomised controlled trial. BMJ. 2014;349:g4315.
Detsky ME, Harhay MO, Bayard DF, Delman AM, Buehler AE, Kent SA, et al. Discriminative accuracy of physician and nurse predictions for survival and functional outcomes 6 months after an ICU admission. JAMA. 2017;317(21):2187–95.
Bakke BM, Feuz MA, McMahan RD, Barnes DE, Li B, Volow AM, et al. Surrogate decision makers need better preparation for their role: advice from experienced surrogates. J Palliat Med. 2022;25(6):857–63.
Majesko A, Hong SY, Weissfeld L, White DB. Identifying family members who may struggle in the role of surrogate decision maker. Crit Care Med. 2012;40(8):2281–6.
Acknowledgements
The authors thank all investigators and supporters involved in this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
QM Wu and JX Zheng: study concepts and design; SH Ma, B Wu: investigation and data searching; PP Chen, Y Xu: data extraction and quality appraisal; YF Zheng, LJ Zhang: data analysis and manuscript preparation; WT Tan, HZ Li: manuscript editing and review.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval and patient consent are not required since this is an overview based on published studies.
Consent for publication
All authors approved the final publication of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Search strategy for the identification of systematic reviews and meta-analyses for PubMed. Table S2. The details of five reviews being excluded due to the duplication.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, Y., Zhang, L., Ma, S. et al. Care intervention on psychological outcomes among patients admitted to intensive care unit: an umbrella review of systematic reviews and meta-analyses. Syst Rev 12, 237 (2023). https://doi.org/10.1186/s13643-023-02372-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-023-02372-5