Abstract
Background
Cardiovascular diseases remain a leading global cause of mortality worldwide especially in older adults. Although it is known that regular exercise reduces cardiovascular diseases incidence, its effects on specific cardiovascular aging parameters considering the influence of sex and different exercise designs are still not fully understood. Therefore, this systematic review and meta-analysis aims to evaluate the effects of different physical exercise protocols on age-related cardiovascular outcomes in older adults.
Methods
This systematic review and meta-analysis will be reported in agreement with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. Articles will be eligible if they are randomized controlled trials with a primary objective of evaluating the chronic effects of exercise interventions on cardiovascular aging parameters. Search strategy will be performed from the inception to September 30th, 2023, in the following electronic databases: MEDLINE (Ovid), SCOPUS (Elsevier), Embase, Sport Discus (EBSCO), Cochrane Central Register of Controlled Trials (CENTRAL), and Web of Science Core Collection (Clarivate Analytics). Data will be extracted and managed through Research Electronic Data Capture (REDCap) software. The Tool for the assEssment of Study qualiTy and reporting in EXercise (TESTEX) will be used to assess the methodological quality of included studies. Additionally, the quality of the findings will be evaluated using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) profiler. Meta-analysis based on the random-effects model will be performed (if deemed suitable, considering the methodological and clinical heterogeneity of the studies) to estimate the effects of exercise training on cardiovascular aging variables (i.e., cardiac output; arterial stiffness; stroke volume; endothelial function; and carotid intima-media thickness). Heterogeneity will be assessed with the I2 statistics, while the publication bias will be assessed based on Egger’s test.
Discussion
To the best of our knowledge, this will be the first systematic review and meta-analysis to investigate the impact of sex and training protocols on the cardiovascular aging parameters. Moreover, the findings of this systematic review and meta-analysis will provide evidence for health professionals in the management of elderly patients in order to optimize the exercise prescription to face the cardiovascular alterations related to the aging process, considering the effects of different protocols according to sex.
Systematic review registration
PROSPERO CRD42023441015 .
Similar content being viewed by others
Background
Cardiovascular disease (CVD) is the leading cause of death worldwide. In 2020, nearly 20 million deaths worldwide (95% uncertainty interval (UI), 17.53–20.24 million) were due to CVD, accounting for 37% of deaths due to non-communicable diseases (NCDs) in people under 70 years of age [1]. Although the age-standardized prevalence of CVD has almost stabilized over the past decade, the crude prevalence has increased by 29.01% (95% UI, 27.73–30.38%), totaling 607.64 million (95% UI, 568.07–644.85 million) cases in 2020 [1]. This increase in crude prevalence can be explained by the increase in life expectancy, as age-related changes in the cardiovascular system are involved in the pathophysiology of all CVD [2, 3].
Cardiac aging is characterized by a decrease in systolic/diastolic ventricular function, increased ventricular stiffness, cardiomyocyte hypertrophy, increased fibrosis, and other alterations [4, 5]. These age-related cardiac changes ultimately lead to a decrease in stroke volume and cardiac output and can lead to coronary artery disease and other CVDs [4, 5]. At the same time, vascular aging is characterized by changes in the functional and structural components of the arterial wall, manifested primarily in arterial stiffness, endothelial dysfunction, and intima thickness [6, 7]. These age-related vascular changes are associated with the development of hypertension, atherosclerosis, stroke, heart failure, and other diseases [6,7,8,9]. With the older population expected to more than double by 2050 [10], global burden of CVD will also increase in the following years [11]. Therefore, strategies to reduce the impact of aging on the cardiovascular system are of paramount importance for the prevention and treatment of CVD as well as for reducing its health and economic consequences.
It is important to note that several environmental and/or lifestyle factors may affect cardiovascular aging [2, 3]. Among lifestyle factors, regular participation in physical activity or exercise programs is well established and is inversely related to the incidence of CVD disease and mortality [1], including in older adults [12]. In this context, regular physical activity through participation in structured exercise programs (mainly aerobic and resistance training programs) is a key recommendation in several guidelines for the prevention and treatment of CVD [13,14,15] and for the health promotion and prevention/treatment of disease in older adults [16]. In relation to cardiovascular aging, there are several systematic reviews showing the effectiveness of exercise interventions on improving cardiac output [17, 18], stroke volume [18], arterial stiffness [17, 19,20,21,22,23,24], endothelial function [25], and carotid intima-media thickness [22]. However, only a few assessed the effects of exercise intervention in older individuals, and only on arterial stiffness [19,20,21, 23], which is an important bias because aging process may affect cardiovascular adaptation to exercise [26]. In addition, these systematic reviews have included only a specific population (i.e., obese) [23] and/or have not assessed the effects of important mediating and moderating variables that may influence the effect of exercise training on cardiovascular aging parameters [19,20,21, 23].
Among the mediating and moderating variables, the adequate representation of women, and the comparison between the sexes should be considered to minimize the under representation of women in cardiovascular disease randomized clinical trials (RCTs) [27], mainly in older age [28]. CVD is highly prevalent in women, and the burden of CVD in women has stagnated during the past decade [27]. In addition, the sex-specific mechanisms of cardiovascular aging and CVD remain poorly understood [27]. It appears that sex chromosomes and hormones influence cardiovascular function and cardiovascular risk factors throughout life [29, 30], leading to poorer outcomes in women, particularly at older ages [31]. In this context, differences between women and men in the effects of physical exercise on cardiovascular outcomes have been reported [30, 31], and sex/gender-specific studies are gaining increasing attention and highlighting crucial implications, including cardiac adaptation to exercise and CVD prevention/rehabilitation [31, 32].
The characteristics of the exercise intervention, defined by the frequency, intensity, type, and time (FITT) principle, are another factor that should be considered when systematically reviewing the effects of exercise interventions on cardiovascular aging. For example, there is limited evidence from systematic reviews with meta-analyzes suggesting that exercise type (aerobic, resistance or combined) may influence the effects of exercise on cardiac output [17] and arterial stiffness [17, 19, 24, 33, 34], while exercise intensity (low-, moderate-, or high-intensity) may influence the effects on arterial stiffness [33] and endothelial function [25]. However, only one study has systematically reviewed the effect of exercise in older adults, and arterial stiffness was the only arterial aging outcome [19]. Furthermore, exercise type cannot be reduced to aerobic, resistance, or combined interventions. There is some evidence that other types of exercise such as stretching, yoga, and dance [21, 35, 36] improve several cardiovascular risk factors in older adults, but their effects on cardiovascular aging, as well as compared with other exercise modalities, remain to be determined. Indeed, the effects of all components of the FITT principle on the effect of exercise on cardiovascular aging parameters in older women and men also remain to be determined.
Our purpose is therefore to perform a systematic review with meta-analysis to assess the effect of exercise training compared with a control intervention on cardiovascular aging parameters (i.e., cardiac output, stroke volume, arterial stiffness, endothelial function, and carotid intima-media thickness) in older individuals. Our specific aim is to quantify the moderating effects of sex (women vs. men) and exercise training characteristics (i.e., FITT principle variables) on cardiovascular aging parameters, to help identify the optimal exercise dose (frequency, intensity, type and time) required to improve cardiovascular aging in older women and men.
Methods
This systematic review will be carried out and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [37]. The present protocol is registered in the PROSPERO repository (CRD42023441015) and follows the PRISMA Protocols statement (Supplement 1) [38].
Eligibility criteria
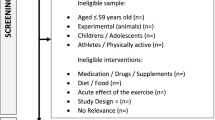
The present review will include only full-text scientific documents of RCTs (i.e., peer-reviewed journal publications, non-peer-reviewed preprints, or PhD/MSc dissertations) investigating the effects of exercise intervention(s) on cardiovascular aging parameters in humans that were written in English, Portuguese, Spanish, Chinese, Polish, Slovak, Azerbaijani, or Turkish. The Population-Intervention-Comparator-Outcomes-Study design (PICOS) criteria will be used to select the studies eligible for inclusion in the review (Table 1).
Population
We will include studies that assessed women and/or men (description of results separated by sex), healthy or with noncommunicable chronic diseases, with a mean age of ≥ 60 years (minimum age ≥ 50 years), that provided a detailed description of the participants (i.e., age, number or percentage of women/men, BMI, healthy status and comorbidities, and medication). The corresponding authors of studies including both men and women, in which participants’ characteristics and results were not presented separately by sex, will be asked to provide the data separately by sex.
Intervention
Studies should have any type of chronic exercise intervention (i.e., repeated exercise sessions during a short or long-term follow-up) to be included in the review. As defined by the American College of Sports Medicine [39], exercise comprises a planned, structured, and repetitive bodily movement done to improve or maintain one or more components of physical fitness and may include aerobic, resistance, and alternative exercise programs, such as Tai Chi, Qigong, dance, exergaming, or balance. Any organ-specific exercise intervention such as respiratory or pelvic muscle training as well as relaxation, meditation, or stretching/flexibility interventions will not be included. Studies assessing only the acute response to exercise or not describing the type, duration and frequency of exercise intervention will not be included.
Comparator
To be included in the review, studies should have a control group with no treatment/intervention, usual care with no exercise interventions (e.g., only medical treatment or healthy habits counseling), sham intervention (e.g., stretching, etc.), or non-active interventions (e.g., health education, recreational activities).
Outcomes
The primary outcomes will be changes between pre- and post-intervention in cardiac output and arterial stiffness. The secondary outcomes will be changes between pre- and post-intervention in stroke volume, endothelial function, and carotid intima-media thickness. To be eligible for this review, studies should have measured, at baseline and at the end of intervention/control follow-up, any of the primary or secondary outcomes, by using a validated method.
Study design
We will include only RCTs.
Search strategy and study selection
Search strategy will be performed from the inception to August 20th, 2024, in the following electronic databases: MEDLINE (Ovid), SCOPUS (Elsevier), Embase, Sport Discus (EBSCO), Cochrane Central Register of Controlled Trials (CENTRAL), and Web of Science Core Collection (Clarivate Analytics). The reference list of the major textbooks, review articles, and all included studies will be hand searched in order to identify other potentially eligible studies. Finally, we will also undertake searches on online gray literature to minimize publication bias (i.e., Google Scholar). The search strategy will include a combination of terms for the key concepts “older adults,” “exercise,” “cardiovascular system,” and “clinical trial.” The full search strategy for MEDLINE and other databases are described in Table 2 and Supplement 2, respectively.
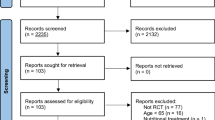
All manuscripts retrieved from each search database will be exported as “.ris” or “.nbiib” files. The files will be imported into Rayyan, a web-based application for systematic review screening (https://rayyan.qcri.org/welcome), and a single researcher will remove the duplicates and duplicates by using the application’s duplicate function. Then, at least two independent reviewers will screen the titles and abstracts of all studies for eligibility. All studies that meet the inclusion criteria, and those with insufficient information in the abstract, will be retrieved for full text screening by two independent reviewers. Disagreements between reviewers, both at abstract or full-text screening, will be discussed with another independent reviewer (E.G.C) to obtain consensus.
Data extraction and management
After study selection, all data will be extracted and managed by using REDCap. The data extraction form will be designed by the review authors, and data extraction will be piloted with a small number of studies (at least 10). If necessary, it will be modified prior to the data extraction of all studies. Data extraction for each individual study will be performed independently by two reviewers. Any disagreement in data extraction will be solved by consensus. If consensus is not achieved, a third reviewer will independently extract the data. The data extraction will include report characteristics (title, first author, study location, year of publication/availability), characteristics of the RCT (study design [parallel group, crossover, number of arms, etc.], total study duration, sequence generation, allocation sequence concealment, blinding, intention to treat, primary and secondary outcomes), participants’ characteristics (health status, sample size at beginning and end of the study, mean age, sex, and physical activity level), intervention(s) characteristics (all FITT variables), control intervention characteristics (type, duration, orientations), outcomes (primary and secondary), and moderators. Outcomes and moderators are detailed below.
In case of missing or unclear data, the authors of the specific study will be contacted by email, up to two times, to provide the required information. If there is no response within 4 weeks, the data we will be considered unobtainable. For data presented in graphs, we will contact the authors to obtain the data or use Web Plot Digitizer (if there is no response within 4 weeks).
Outcomes
The primary outcomes will be cardiac output (both at rest and/or during exercise) and arterial stiffness. The secondary outcomes will be stroke volume (both at rest and/or during exercise), endothelial function, and carotid intima-media thickness. The primary and secondary outcomes should be measured by a validated method, which include:
-
Cardiac output: acetylene rebreathing; bioreactance; cardiac MRI; CO2 rebreathing; echocardiography; finger photoplethysmography; impedance cardiography; inert gas rebreathing; radionuclide ventriculography; or thoracic impedance
-
Arterial stiffness: aortic pulse wave velocity (PWV); carotid-femoral PWV; brachial-ankle PWV; cardio-ankle vascular index (CAVI); or waveform reflection (i.e., augmentation index, and/or augmentation index adjusted to 75 bpm)
-
Stroke volume: acetylene rebreathing; bioreactance; cardiac MRI; CO2 rebreathing; echocardiography; finger photoplethysmography; impedance cardiography; inert gas rebreathing; radionuclide ventriculography; or thoracic impedance
-
Endothelial function: brachial artery flow-mediated dilation (FMD); radial artery FMD; or peripheral arterial tonometry by the reactive hyperemia index (RHI)
-
Carotid intima-media thickness: ultrasound data processing; or echo-tracking
Mean and standard deviation (SDs) at baseline and follow-up will be extracted from intervention(s) and control groups for each primary or secondary outcome. The effect of exercise on primary and secondary outcomes will be first examined without sex separation. Subgroup analyses by sex (women vs. men) will be then conducted to investigate the sex differences in outcomes. Any significant differences in the effects of exercise and physical activity on cardiovascular aging between males and females will be reported, and potential explanations for these differences will be explored.
Moderators
The primary moderators of the present review will be the exercise intervention characteristics (i.e., FITT principle variables). Thus, we will extract information regarding exercise interventions’ frequency (i.e., number of sessions per week), intensity (i.e., absolute and/or relative objective and/or subjective parameters of exercise intensity), type (i.e., exercise modality(ies) performed), and duration (i.e., duration of the exercise sessions, duration of each exercise modality, and duration of the exercise program) as well as about the progression of these variables throughout the follow-up. To try to identify the optimal exercise dose (frequency, intensity, type and time) required to improve cardiovascular aging, we will conduct analyses for the following potential moderators: (1) frequency of exercise sessions, (2) exercise intensity, (3) type(s) of exercise(s), (4) exercise session(s) duration, (5) workload of exercise sessions (e.g., intensity X duration, metabolic costs…), (6) program duration, (7) density of exercise sessions per week (frequency X intensity X volume), (8) progression of exercise frequency/intensity/volume, (9) type of control group, and (10) use of behavioral interventions.
We will also extract information about individual characteristics that are used in previously published systematic reviews and meta-analyses and/or are hypothesized to modulate the effect size of exercise on cardiovascular aging. Possible moderator variables related to this will include the following: (1) population type (e.g., ethnicity, health status, type of comorbidity…), (2) mean age, (3) cardiovascular aging parameters at baseline, (4) fitness and/or physical activity level at baseline, (5) prevention level (e.g., primary, secondary, tertiary…), (6) education, and (7) socioeconomic status. Other possible moderators that will be extracted from the studies will be the type of publication (e.g., peer-reviews journal article, preprint, thesis, etc.) and sample size of intervention(s) and control group.
The above-mentioned moderator variables will only be included in the meta-analysis if sufficient studies are available (at least three studies for of each level of a categorical moderator description/analysis and at least eight studies for a meta-regression).
Assessment of study quality, risk of bias, and overall quality of evidence
The methodological quality of the included studies will be assessed by the Tool for the assEssment of Study qualiTy and reporting in EXercise (TESTEX) [40], which has 12 criteria (maximum score of 15 points) pertaining to study quality (i.e., eligibility criteria specified, randomization specified, allocation concealment, groups similar at baseline, and blinding of assessor for the primary outcome) and study reporting (i.e., outcome measures assessed in 85% of patients, intention-to-treat analysis, between-group statistical comparisons reported, point measures and measures of variability for all reported outcome measures, activity monitoring in control groups, relative exercise intensity remained constant, and exercise volume and energy expenditure). A higher score reflects better quality. Two reviewers will assess independently to rate each criterion, and inter-observer agreement will be determined using Kappa statistics [41]. In case of disagreement of rating, the agreement will be solved by two different reviewers. Studies will not be excluded based on their quality.
The overall quality of evidence will be reported using Grading of Recommendations Assessment, Development and Evaluation (GRADE) [42], which is structured in five domains: risk of bias, imprecision, inconsistency, indirectness, and publication bias. Each outcome will be assessed for the overall certainty in evidence and classified into four levels: high, moderate, low, or very low.
Data analysis
Statistical analyses will be performed using Comprehensive Meta-Analysis software (CMA, version 2.2.064, Biostat, NJ, USA). Descriptive data for each of the individual studies will be reported as means ± standard deviations (SD). Continuous outcomes will be used to analyze as post-intervention changes from baseline using mean difference (MD). Standardized mean differences (SMD, i.e., mean weighted difference and its 95% confidence intervals [CI]) will be used if the outcomes were collected using different measurements across studies. Data expressed using the standard error of the mean (SEM) will be first converted to SD. For binary outcomes, the odds ratio (OR) and its corresponding 95% CI will be calculated. The Mantel–Haenszel method will be employed for pooled estimates in binary outcomes, with the choice between a fixed-effect or random-effects model based on the level of heterogeneity. Pooled estimates of the effect of exercise training on cardiac aging outcomes (i.e., cardiac output, arterial stiffness, stroke volume, endothelial function, and carotid intima-media thickness) will be obtained using a random-effects model with significance set at P < 0.05 (two-tailed), as we expected heterogeneity in the methodology of the studies. The random-effects model will use the DerSimonian and Laird method to estimate the heterogeneity variance (τ2), which allows for the assumption that the true effects might vary across studies.
Sub-group analyses, including sensitivity and meta-regression approaches, will be performed to explore potential moderators, such as sex differences, baseline fitness levels, and study design factors, on cardiovascular aging outcomes. Meta-regression will be conducted using a mixed-effects model, where the heterogeneity variance will be estimated using restricted maximum likelihood (REML). Covariates, including age, gender, duration of intervention, and baseline health status, will be examined as potential moderator variables Heterogeneity will be assessed using the I2 statistics where I2 values between 25 and 50% represents small amounts of inconsistency, 50 and 75% represents medium inconsistency, and above 75% represents large amounts of inconsistency [43]. Cochran’s Q test will also be performed to test for heterogeneity. If substantial heterogeneity is detected, sources of heterogeneity will be explored through subgroup analyses and meta-regression.
Publication bias will be examined by visual inspection of the different funnel plots’ asymmetry. The Egger’s test [44] will indicate the presence of a significant publication bias. Duval and Tweedie’s trim and fill procedure will be applied to estimate the effect of publication bias on the results [43]. Sensitivity analyses will be conducted to assess the robustness of the results by excluding studies with high risk of bias, studies with extreme effect sizes, or studies contributing disproportionately to the heterogeneity.
Discussion
Previous systematic reviews have investigated the effects of exercise interventions on several cardiovascular aging parameters, including cardiac output [17, 18], stroke volume [18], arterial stiffness [17, 19,20,21,22,23,24], endothelial function [25], and carotid intima-media thickness [22]. However, in older individuals, there are systematic effects assessing the effect of exercise interventions only on arterial stiffness [19,20,21, 23]. Although these systematic reviews found positive effects of exercise interventions on arterial stiffness of older individuals, they did not investigate if the benefits are different between sexes nor investigated the impact of most moderators that will be investigated in the present review.
According to our knowledge, this is the first systematic review with meta-analysis aiming to assess the effects of chronic exercise on different cardiovascular aging parameters in older individuals. In addition, it will also be the first to investigate the role of sex (men vs. women) and training characteristics (i.e., frequency, intensity, type and time) on the effects of chronic exercise effects on cardiovascular aging. Thus, this review will contribute to the evidence base of exercise on cardiovascular aging, which may help the development of specific exercise recommendations (i.e., frequency, intensity, type and time) to improve cardiovascular aging according to sex.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics—2023 update: a report from the American Heart Association. Circulation. 2023;147(8):e93–621. https://doi.org/10.1161/CIR.0000000000001123.
Fontana L. Interventions to promote cardiometabolic health and slow cardiovascular ageing. Nat Rev Cardiol. 2018;15(9):566–77. https://doi.org/10.1038/s41569-018-0026-8.
Gude NA, Broughton KM, Firouzi F, Sussman MA. Cardiac ageing: extrinsic and intrinsic factors in cellular renewal and senescence. Nat Rev Cardiol. 2018;15(9):523–42. https://doi.org/10.1038/s41569-018-0061-5.
Nakayama H, Nishida K, Otsu K. Macromolecular degradation systems and cardiovascular aging. Circ Res. 2016;118(10):1577–92. https://doi.org/10.1161/CIRCRESAHA.115.307495.
Pandey A, Kraus WE, Brubaker PH, Kitzman DW. Healthy aging and cardiovascular function: invasive hemodynamics during rest and exercise in 104 healthy volunteers. JACC Heart Fail. 2020;8(2):111–21. https://doi.org/10.1016/j.jchf.2019.08.020.
Laurent S. Defining vascular aging and cardiovascular risk. J Hypertens. 2012;30. https://journals.lww.com/jhypertension/Fulltext/2012/06001/Defining_vascular_aging_and_cardiovascular_risk.2.aspx.
Climie RE, Alastruey J, Mayer CC, et al. Vascular ageing - moving from bench towards bedside. Eur J Prev Cardiol Published online. February 2023. https://doi.org/10.1093/eurjpc/zwad028.
Alexander Y, Osto E, Schmidt-Trucksäss A, et al. Endothelial function in cardiovascular medicine: a consensus paper of the European Society of Cardiology Working Groups on Atherosclerosis and Vascular Biology, Aorta and Peripheral Vascular Diseases, Coronary Pathophysiology and Microcirculation, and Thr. Cardiovasc Res. 2021;117(1):29–42. https://doi.org/10.1093/cvr/cvaa085.
Chirinos JA, Segers P, Hughes T, Townsend R. Large-artery stiffness in health and disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;74(9):1237–63. https://doi.org/10.1016/j.jacc.2019.07.012.
United Nations. World population ageing 2019 (st/esa/ser. a/444). Department of Economic and Social Affairs PD, editor New York, USA 2020. Published online 2020. Accessed April 17, 2023. https://www.un.org/development/desa/pd/news/world-population-ageing-2019-0.
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results.; 2020. Accessed April 17, 2023. http://ghdx.healthdata.org/gbd-results-tool.
Cunningham C, O’ Sullivan R, Caserotti P, Tully MA. Consequences of physical inactivity in older adults: a systematic review of reviews and meta-analyses. Scand J Med Sci Sports. 2020;30(5):816–27. https://doi.org/10.1111/sms.13616.
Visseren FLJ, MacH F, Smulders YM, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–337. https://doi.org/10.1093/eurheartj/ehab484.
Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104. https://doi.org/10.1093/eurheartj/ehy339.
Ambrosetti M, Abreu A, Corrà U, et al. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2021;28(5):460–95. https://doi.org/10.1177/2047487320913379.
Izquierdo M, Merchant RA, Morley JE, et al. International Exercise Recommendations in Older Adults (ICFSR): Expert Consensus Guidelines. Journal of Nutrition, Health and Aging. 2021;25(7):824–53. https://doi.org/10.1007/s12603-021-1665-8.
Zhang Y, Qi L, Xu L, et al. Effects of exercise modalities on central hemodynamics, arterial stiffness and cardiac function in cardiovascular disease: systematic review and meta-analysis of randomized controlled trials. PLoS One. 2018;13(7). https://doi.org/10.1371/journal.pone.0200829.
Astorino TA, Causer E, Hazell TOMJ, Arhen BB, Gurd BJ. Change in central cardiovascular function in response to intense interval training: a systematic review and meta-analysis. Med Sci Sports Exerc. 2022;54(12):1991–2004. https://doi.org/10.1249/MSS.0000000000002993.
Lan YS, Khong TK, Yusof A. Effect of exercise on arterial stiffness in healthy young, middle-aged and older women: a systematic review. Nutrients. 2023;15(2). https://doi.org/10.3390/nu15020308.
Manojlović M, Protić-Gava B, Maksimović N, et al. Effects of combined resistance and aerobic training on arterial stiffness in postmenopausal women: a systematic review. Int J Environ Res Public Health. 2021;18(18). https://doi.org/10.3390/ijerph18189450.
Kato M, Green FN, Hotta K, et al. The efficacy of stretching exercises on arterial stiffness in middle-aged and older adults: a meta-analysis of randomized and non-randomized controlled trials. Int J Environ Res Public Health. 2020;17(16):1–15. https://doi.org/10.3390/ijerph17165643.
Huang C, Wang J, Deng S, She Q, Wu L. The effects of aerobic endurance exercise on pulse wave velocity and intima media thickness in adults: a systematic review and meta-analysis. Scand J Med Sci Sports. 2016;26(5):478–87. https://doi.org/10.1111/sms.12495.
Montero D, Roberts CK, Vinet A. Effect of aerobic exercise training on arterial stiffness in obese populations: a systematic review and meta-analysis. Sports Med. 2014;44(6):833–43. https://doi.org/10.1007/s40279-014-0165-y.
Sardeli AV, GáSpari AF, Chacon-Mikahil MP. Acute, short-, and long-term effects of different types of exercise in central arterial stiffness: a systematic review and meta-analysis. J Sports Med Phys Fitness. 2018;58(6):923–32. https://doi.org/10.23736/S0022-4707.17.07486-2.
Ashor AW, Lara J, Siervo M, et al. Exercise modalities and endothelial function: a systematic review and dose–response meta-analysis of randomized controlled trials. Sports Med. 2015;45(2):279–96. https://doi.org/10.1007/s40279-014-0272-9.
Ciolac EG, Roberts CK, Rodrigues Da Silva JM, Guimarães GV. Age affects exercise-induced improvements in heart rate response to exercise. Int J Sports Med. 2014;35(5). https://doi.org/10.1055/s-0033-1351332.
Vogel B, Acevedo M, Appelman Y, et al. The Lancet women and cardiovascular disease Commission: reducing the global burden by 2030. Lancet. 2021;397(10292):2385–438. https://doi.org/10.1016/S0140-6736(21)00684-X.
Daitch V, Turjeman A, Poran I, et al. Underrepresentation of women in randomized controlled trials: a systematic review and meta-analysis. Trials. 2022;23(1). https://doi.org/10.1186/s13063-022-07004-2.
Gerdts E, Sudano I, Brouwers S, et al. Sex differences in arterial hypertension: a scientific statement from the ESC Council on Hypertension, the European Association of Preventive Cardiology, Association of Cardiovascular Nursing and Allied Professions, the ESC Council for Cardiology Practice, and the ESC Working Group on Cardiovascular Pharmacotherapy. Eur Heart J. 2022;43(46):4777–88. https://doi.org/10.1093/eurheartj/ehac470.
Seals DR, Nagy EE, Moreau KL. Aerobic exercise training and vascular function with ageing in healthy men and women. J Physiol. 2019;597(19):4901–14. https://doi.org/10.1113/JP277764.
Vaccarezza M, Papa V, Milani D, et al. Sex/gender-specific imbalance in CVD: could physical activity help to improve clinical outcome targeting CVD molecular mechanisms in women? Int J Mol Sci. 2020;21(4). https://doi.org/10.3390/ijms21041477.
Ghisi GL de M, Kin R. SM, Price J, et al. Women-focused cardiovascular rehabilitation: an International Council of Cardiovascular Prevention and Rehabilitation clinical practice guideline∗. Canadian Journal of Cardiology. 2022;38(12):1786–1798. https://doi.org/10.1016/j.cjca.2022.06.021.
Ashor AW, Lara J, Siervo M, Celis-Morales C, Mathers JC. Effects of exercise modalities on arterial stiffness and wave reflection: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(10). https://doi.org/10.1371/journal.pone.0110034.
Lopes S, Afreixo V, Teixeira M, et al. Exercise training reduces arterial stiffness in adults with hypertension: a systematic reviewand meta-analysis. J Hypertens. 2021;39(2):214–22. https://doi.org/10.1097/HJH.0000000000002619.
Brandani JZ, Mizuno J, Ciolac EG, Monteiro HL. The hypotensive effect of Yoga’s breathing exercises: a systematic review. Complement Ther Clin Pract. 2017;28. https://doi.org/10.1016/j.ctcp.2017.05.002.
Rodrigues-Krause J, Farinha JB, Krause M, Reischak-Oliveira Á. Effects of dance interventions on cardiovascular risk with ageing: Systematic review and meta-analysis. Complement Ther Med. 2016;29:16–28. https://doi.org/10.1016/j.ctim.2016.09.004.
Page MJ, McKenzie JE, Bossuyt PM, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. The BMJ. 2020;2021:372. https://doi.org/10.1136/bmj.n71.
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Revista Espanola de Nutricion Humana y Dietetica. 2016;20(2):148–60. https://doi.org/10.1186/2046-4053-4-1.
ACSM’s guidelines for exercise testing and prescription, 11th Edition. ProtoView. 2021;2021(8).
Smart NA, Waldron M, Ismail H, et al. Validation of a new tool for the assessment of study quality and reporting in exercise training studies: TESTEX. Int J Evid Based Healthc. 2015;13(1):9–18. https://doi.org/10.1097/XEB.0000000000000020.
Viera A, Garrett J. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–3.
Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94. https://doi.org/10.1016/j.jclinepi.2010.04.026.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. https://doi.org/10.1002/sim.1186.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629. https://doi.org/10.1136/bmj.315.7109.629.
Acknowledgements
This publication is based upon work from EU COST Action CA20104 – Network on evidence-based physical activity in old age (PhysAgeNet), supported by COST (European Cooperation in Science and Technology).
Funding
The fees for the publication of the protocol are supported by COST Action CA20104. EGC was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq #310572/2021–5).
Author information
Authors and Affiliations
Consortia
Contributions
EGC coordinated and supervised all activities and participated in the study conception and design, manuscript drafting, and reviewing. JB participated in the study conception and design, manuscript drafting, and reviewing. RMA, SJM, GQ, and VTA participated in the study conception and design and manuscript drafting. BW, AJTF, ZO, FVFF, SCY, and BF participated in the study conception and manuscript drafting. LMR and RG participated in the study conception and manuscript reviewing. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This review does not require approval from an Ethics Committee and any consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ciolac, E.G., Babjakova, J., de Abreu, R.M. et al. Role of sex and training characteristics on exercise effects on cardiovascular aging: protocol for a systematic review with meta-analysis of randomized trials. Syst Rev 13, 234 (2024). https://doi.org/10.1186/s13643-024-02644-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-024-02644-8