Abstract
Immune disorders have become one of the public health problems and imposes a serious economic and social burden worldwide. Ginsenosides, the main active constituents of ginseng, are regarded as a novel supplementary strategy for preventing and improving immune disorders and related diseases. This review summarized the recent research progress of ginsenosides in immunomodulation and proposed future directions to promote the development and application of ginsenosides. After critically reviewing the immunomodulatory potential of ginsenosides both in vitro and in vivo and even in clinical data of humans, we provided a perspective that ginsenosides regulated the immune system through activation of immune cells, cytokines, and signaling pathways such as MAPK, PI3K/Akt, STAT, and AMPK, as well as positively affected immune organs, gut flora structure, and systemic inflammatory responses. However, the evidence for the safety and efficacy of ginsenosides is insufficient, and the immune pathways of ginsenosides remain incompletely characterized. We believe that this review will provide a valuable reference for further research on ginsenosides as dietary supplements with immunomodulatory effects.
Similar content being viewed by others
Introduction
Genetic factors, environmental pollution, mental pressure, and unhealthy lifestyles are responsible for immune dysfunction. In addition, with the population aging and the outbreak of various epidemics, diseases caused by immune dysfunction such as allergies, rheumatoid arthritis (RA), rheumatic heart disease and systemic lupus erythematosus (SLE) are emerging [1]. As a research study published by The Lancet showed an increasing trend in the incidence and prevalence of immune diseases, and the world is facing severe economic and social pressures [2]. Immunity is a self-defense function of the human body, and the immune system is a significant system of immune response and immune function. The balance and coordination within the immune system are critical to maintain body health. The response of the immune system can be categorized into two categories: immunoenhancement and immunosuppression. Immunoenhancement refers to an enhanced immune response to pathogenic microbial infections, immunodeficiencies and other diseases. However, the hyperactivity of its function will cause damage to organs or tissues. Many autoimmune diseases, such as RA, SLE and ulcerative colitis (UC), are caused by over-immunization, which requires drug intervention to suppress the body’s immune response. Immunosuppression means that the immune response is downregulated, which can lead to increased susceptibility to infection, even cancers and tumors. Immunomodulation, a treatment strategy that uses natural or synthetic drugs and microorganisms to activate or inhibit the immune system to fight disease, has become a research hotspot and major challenge in the contemporary healthcare area. Immunomodulators are classified as natural and synthetic drugs. The application of immunomodulators has a positive effect on various types of infections, allergies or cancers. These are natural and synthetic agents used to adapt to the immune system response. Clinically, levamisole, cyclophosphamide (CTX), dexamethasone (DEX), methotrexate (MTX), hydrocortisone, and other chemical synthetic drugs are widely used in immunomodulation, the use of such immunomodulators has been controversial due to their typical side effects such as alopecia, diarrhea, hematological diseases, bdelygmia, immune organ failure [3]. Natural agents consisting of botanicals and dietary supplements are known to be comparatively safe but less studied. This review is intended to raise the interest of researchers in the use of ginsenosides as an alternative remedy to traditional therapy, especially in cases where the immune system is partially impaired or specific immunotherapy is needed to minimize adverse events.
Ginseng (Panax ginseng C.A. Meyer) is a widely known medicinal and food plant, that contains more than 100 functional compounds with physiological functions against cancer, viruses, inflammation, aging, diabetes, dementia and fatigue [4]. Ginsenosides are the main active components extracted from the fruits, flowers, leaves, stems and roots of ginseng. QYResearch showed that the global ginseng industry market size stayed above and below $7.9 billion, with China and South Korea being the major ginseng markets, followed by Japan and the EU region. Currently, the global ginsenoside head manufacturers mainly include Folotto, BTGin, Dr. Ginseng, Onstin, and Mkule. On the basis of different product types, it is categorized into capsules, oral liquids, drops, tablets and powders. The price increases with the purity of ginsenosides. Total ginsenoside power costs roughly $166.8/kg, rare ginsenoside Rg3 power costs $69,514.1/kg, and ginsenoside Rh2 power costs $136,247.6/kg. Generally, the more homogeneous the ingredient, the clearer the efficacy. Products in the market have different specifications and advertise different efficacy. Some products confused the concept of total ginsenosides and ginseng powder, and are very vague about the labeling of purity. Emphasis on the development of standardized extracts and quality control can augment consumer reliance. Exploring and elucidating the regulatory mechanisms is a critical step in the development of ginsenosides with immunomodulatory effects as nutritional supplements.
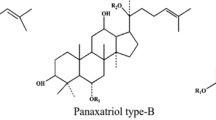
Ginsenosides belong to triterpenoids, which are composed of steroid skeleton (17 carbon) containing sugar. To date, more than 300 natural and transformed ginsenosides have been identified and studied [5]. Depending on the difference between aglycones, ginsenosides can be classified into protopanaxadiol (PPD), protopanaxatriol (PPT), ocotillol and oleanolic acid types (Fig. 1A). Ginsenosides Rb1, Rc, Rb2, Re, Rb3, Rg1 and Rf are considered to be the major ginsenosides as they account for more often than 90% of all ginsenosides. The main ginsenosides could be converted into rare ginsenosides by some factors in the processing process [6,7,8,9] (Fig. 1B and C), and the factors include biological factors such as enzymes and microorganisms, chemical factors such as acid and base, and physical factors such as high temperature and high pressure. The bioactivity and bioavailability of ginsenosides vary with the diversity of their chemical structures [10]. The rare ginsenosides are readily absorbed by the human body and have high bioactivity as the sugar groups are partially removed. Therefore, rare ginsenosides are the main active compounds in the research of immunomodulation.
Extensive in vitro and in vivo studies on ginsenosides have been reported with rewarding results. The details of the immunomodulatory effects of ginsenosides as shown in Fig. 2. Among these studies, researchers used a variety of cell lines, including RAW264.7, PBMC, HepG2, B16F10 and others, and reported both direct cytotoxic effects and indirect cytotoxic effects. A variety of in vivo cancer models including rats, ferrets, BALB/c mice, thymus mice, C57BL/6 mice and several others were stimulated by lipopolysaccharide (LPS), cyclophosphamide (CTX), gemcitabine (GEM) and other drugs were used to establish the animal models of immune enhancement and immunosuppression in vivo study. Therefore, the mechanisms of ginsenosides regulating immune dysfunction can be studied from cellular and organism levels. PPT-type and PPD-type ginsenosides are currently the most studied. Ginsenosides as the main source of nutritional and functional foods with the characteristics of nature, efficiency and security, have developed into an inventive strategy to preclude or improve immune dysfunction under the particular background of chronic diseases and infectious diseases. As a result, it is necessary to elucidate the mechanisms of ginsenoside modulating the immune system.
The details of the immunomodulatory effects of ginsenosides. Various factors can lead to human immune system disorders. Currently, chemical drugs commonly used in clinical practice to improve immune imbalance include levamisole, cyclophosphamide, dexamethasone, etc. However, the natural active ingredient ginsenoside is more advantageous than chemical drugs. Extensive in vivo and in vitro experiments were used to investigate the mechanisms of ginsenosides regulating immunity. A variety of cell lines and animal models were used. Ginsenoside, as a potential immune regulator, has a protective function on human organs and can effectively prevent and alleviate the occurrence and development of a variety of immune diseases
This review focuses on the underlying the current state of knowledge on the potential mechanisms of ginsenosides on immune disorders in the last decade. Literature search was conducted in peer-reviewed and clinical databases, which include PubMed (https://www.ncbi.nlm.nih.gov/pubmed), Scopus (https://www.scopus.com), Web of Science (http://www.webofknowledge.com), Medline (https://www.medline.com), and Clinical Trials (https://clinicaltrials.gov) using the following keywords: Ginsenoside, Ginseng, Immune, Cancer, Tumor, Stress, Liver, Spleen, Intestine, Bone marrow. To provide new insights into the critical path ahead, the immunomodulatory effects, mechanism of action, relevant clinical studies, and innovative applications in combined therapy of ginsenoside were reviewed systemically.
The effects of ginsenosides on innate and adaptive immunity
The effects of ginsenosides on innate and adaptive immunity are summarized and shown in Table 1. During the process of inflammation, injury, infection, and aging, immune cells regulate the availability of various cytokines. Therefore, immune cells were viewed as highly dynamic partners of the immune system. Ginsenoside Rg1 regulated cytokine levels in RAW264.7 cells and enhanced the innate immune response of mouse peritoneal macrophages through differential regulation of phosphoinositide 3-kinase (PI3K)/Akt and nuclear factor kappa-B (NF-κB) signaling pathways [11]. Compound K (CK) and 20S-dihydroprotopanaxadiol (2H-PPD), promoted the innate immune response and motivated macrophages and monocytes by raising the level of phagocyte uptake, cell-to-cell adhesion and the apparent level of CD80 and CD86, costimulatory molecules [12, 13]. Ginsenoside Rg3 intervention inhibited M1-type macrophage marker gene expression and induced M2-type macrophage polarization in LPS-induced mice, suggesting that Rg3 promoted the elimination of inflammation in mouse peritonitis model [14]. Dendritic cells (DCs) are the most potent specialized immunogen-presenting cells in the body, which are essential for initiating adaptive immune responses. Rg1 was effective in promoting phenotypic maturation and eliciting adaptive immune responses in human iDCs [15]. Another study reported that Rg1 raised the number of DCs, B and T cells in DEX-treated mice [16].
Ginsenosides also play a regulatory role in adaptive immunity. A study reported that 20(S)-Rg3 and 20(R)-Rg3 significantly enhanced the secretion of interleukin (IL)-2 and interferon (IFN)-γ by activating the proliferation of lymphocytes and natural killing (NK) cells, which greatly contribute to antitumor effects [17]. Ginsenoside Re activated T and B lymphocytes, and increased the concentration of antibodies in mice [18]. Similarly, ginseng stem-leaf saponins (GSLS) promoted the activation of T and B lymphocytes and the production of IgG and IgG titers in serum, indicating that both cell and humoral immunity responses were enhanced [19]. Oral administration of ginsenoside Rg1 significantly enhanced the expressions of specific antibodies and promoted the proliferation of lymphocytes [20]. Ginsenoside Rd upregulated Foxp3 expression to drive regulatory T cell (Treg) differentiation and induced the generation of IL-10, TGF-β and IL-35 [21]. Rg1 increased the count of neutrophils in the peritoneal cavity and reversed the overexpression of cytokines and suppressed the apoptosis of lymphocytes in septic mice spleen and thymus [22]. CK restored the swollen joint count, polyarthritis index, spleen index and serum antibody (IgG1, IgG2a) and other levels to normal in collagen-induced arthritis (CIA) mice. CK treatment also restored the proliferation of B cells and subsets [23].
Role in cancer
Ginsenosides and cancer immunity
As shown in Fig. 3, ginsenosides were reported to elucidate the immunizing effect against cancer. Ginsenosides exert anticancer effects in hepatocellular carcinoma, colorectal carcinoma, breast carcinoma, and lung carcinoma by inhibiting cell proliferation and migration, angiogenesis, and reversing drug resistance [24,25,26]. Ginsenoside Rh2 inhibited breast cancer cell proliferation and enhanced immunogenicity by down-regulating the expression of hypermethylated genes such as INSL5, CASP1 and OR52A1 and up-regulating hypomethylated genes such as ST3GAL4, C1orf198 and CLINT1 [27]. Rh2 and its octyl derivative Rh2-O increased the levels of TNF-α, IL-2, T lymphocyte and NK cell, and facilitated tumor cell apoptosis by controlling the phosphorylation of caspase and B-cell lymphoma-2 (Bcl-2) [28]. Ginsenoside 20(S)-Rh2 significantly decreased the spleen index in acute lymphoblastic leukemia (T-ALL) mice, and the spleen immunity was enhanced by regulating immune factors. Moreover, 20(S)-Rh2 also weakened the infusion of leukemia cells into the spleen by blocking the PI3K/AKT/mammalian target of rapamycin (mTOR) signaling pathway [29]. Ginsenoside Rh2 significantly improved the survival time in melanoma mice, enhanced the infiltration of CD4+T and CD8+T cells in tumors and triggered cytotoxicity in spleen lymphocytes [30]. Notably, ginsenoside Rk3 blocked the cell cycle in hepatocellular carcinoma (HCC) at the G1 phase to induce autophagy and apoptosis. Meanwhile, Rk3 regulated the expression of PI3K and AKT proteins to inhibit the growth of HCC [31]. 20(S)-Rh2 lowered cancer cell survival and inhibited the phosphorylation of transcription activator 3 (STAT3) and the expression of matrix metalloproteinase (MMP), resulting in suppressing tumor invasion in human colorectal cancer (CRC) cells [32]. Similarly, it was reported that ginsenoside Rg3 could repress the growth and stemness of CRC cells both in vitro and in vivo. Rg3 impaired the migration of CRC cells in vitro. Rg3 repressed the vascularization of CRC xenografts by downregulating the expressions of angiogenesis-related genes. In addition, Rg3 strengthened the cytotoxicity of oxaliplatin and 5-Fluorouracil against orthotopic xenografts in vivo [33]. High expression of Fibroblast growth factors FGF8 is commonly linked to tumor generation and vasculogenesis. Treatment of ovarian cancer mice with Rg5 for one month resulted in a significant reduction of tumor size and restraint of tumor metastasis. Ginsenoside Rg5 significantly reduced FGF8b expression in ovarian cancer cell line OCI-P9a cells, suggesting that anticancer and antimetastatic effects of ginsenoside Rg5 were possibly related to the FGF8b-related pathway [34]. CK inhibited tumor growth by inducing apoptosis and tumor cell differentiation through multiple signaling pathways such as 5’AMP-activated protein kinase (AMPK), c-Jun N-terminal kinase (JNK) and NF-κB. Moreover, CK regulated the tumor microenvironment by inhibiting tumor angiogenesis-related proteins [35].
Ginsenosides modulate cancer immunity. Ginsenosides induced cell-mediated immune response-related pathways, increased uptake of cancer cells by DC cells, increased the cytotoxicity of NK cells, regulated macrophages, T cells and Th1/Th2 balance, so as to reduce organ damage and improve the immune capacity of cancer chemotherapy patients
Ginsenosides as immune modulator
Sorafenib (SFN) and GEM remain the first-line treatment choice for cancer therapy. Ginsenoside Rg3 and combined SFN treatment relieved the hepatocellular carcinoma progression via the mediation of HK2-mediated gluconeogenesis and PI3K/Akt pathway [36]. GEM combined with Rh2 boosted the invasion of DCs to tumors and reduced the expression level of immunosuppressive factors, such as VEGF, IL-6, and TGF-β against trypanic cancer via the NF-κB pathway [37]. Ginsenoside Rg3 increased NK cells’ cytotoxicity via the mitogen activated protein kinase (MAPK) pathway and also raised the expression of NK-activated reactors [38].
Reduction of chemo or radiotherapy-induced side effects
CTX has been widely used as a traditional alkylating chemotherapeutic agent for the treatment of tumors in clinical practice for over 50 years. The use of high doses of CTX during chemotherapy often results in severe allocytopenia, which can lead to life-threatening conditions. CK is a bioactive derivative of ginsenoside Rb1. Ginsenoside CK improved the decline of spleen and thymus indices caused by CTX. CK controlled the apoptosis of BM nucleated cells (BMNCs) by the mitogen-activated extracellular signal-regulated kinase (MEK)/extracellular signal-regulated kinase (ERK) and Bcl-2 assaciated X protein (Bax)/Bcl-2 pathways and promoted the BMNCs to enter the cell cycle, proliferate and differentiate normally [39]. Panaxadiol saponins component (PDS-C) promoted the proliferation and differentiation of hematopoietic progenitor cells in CTX-induced myelosuppressed mice, which mediated by p-MEK and p-ERK, as well as the C-kit and GATA-1 transcription factors [40]. Rg3 intervention significantly increased the body weight, the organ indices of immune organs, thymus and spleen in mice, and alleviated the pathological damage of organs by regulating macrophages and Th1/Th2 balance, suggesting that Rg3 could boost immunity in chemotherapy recipients [41].
Immunomodulators against viruses, bacteria and other parasites
The effects of ginsenosides as immunomodulators against viruses, bacteria and other parasites are shown in Table 2. When humans or animals are infected with a virus, various types of cytokines are known to be activated to prevent the virus from replicating. Ginsenosides Rb1 and Rg3 regulated the expression of immune factors and inflammatory factors, enhancing the phagocytosis of bacteria by phagocytes [42, 43]. Ginsenoside Rg3 inhibited lytic replication and the proliferation of γ herps viral via p38/JNK -related pathways [44]. Ginsenoside Rb1 remarkably reduced the expression of enterovirus 71 (EV71)-induced viral protein-1 (VP-1) [45]. Rg3 attenuated the replication of hepatitis B virus DNA by stimulating TRAF6/TAK1 degradation and repressing JNK/AP-1 signaling. Among them, TRAF6 and TAK1 are adaptor molecules that signal through a toll-like receptor (TLR)-myeloiddifferentiationfactor88 (MyD88)-dependent pathway. Ginsenoside Rg3 dose-dependent inhibited IL-8 and TNF-α levels in HepG2.2.15 cells [46]. Toxoplasma gondii (T. gondii), a neurotropic specialized cytosolic parasite, is responsible for central nervous system disorders. GRh2 inhibited T. gondii infection-induced microglial activation and neuronal damage through the downregulation of the TLR4/NF-κB signaling pathway [47].
Ginsenosides in autoimmune disorders and allergies
Autoimmune disorders and allergic reactions are manifestations of excessive immunity, and ginsenosides gained attention as a hopeful preventive and therapeutic adjuvant in combating excessive response of the immune system. Rh2 significantly attenuated the symptoms of weight reduction, intestinal damage and shortened colon length in dextran sodium sulfate (DSS)-induced ulcerative colitis mice. Rh2 could lower the secretion of IL-6, TNF-α, IL-1β and inhibit STAT3/miR-214 activation induced by IL-6 [48]. Ginsenosides Rb1, Rh1, Rg1 and Rg3 inhibited the proliferation of B cells and the secretion of antibodies (IgG, IgM) by promoting caspase 3 and Fas/FasL expression in SLE mice [49]. The process of allergic immune responses regulated by ginsenosides is closely related to its effects on humoral and cellular immune aspects. Rh2 inhibited the levels of TNF-α, IL-4, IL-1β and IL-8 in ovalbumin (OVA)-induced asthmatic mice, as well as the activation of BCR signaling molecules in lung tissue. Rh2 suppressed the release and degranulation of histamine from IgE-sensitized MCs, which might be related to NF-κB/AKT/Nrf2 and NF-κB/p38 MAPK/Nrf2 pathways [50]. Ginsenoside Rg3 could ameliorate allergic airway oxidative stress and inflammation sensitized with OVA by reducing the levels of ROS, Th2 cytokine and chemokine [51].
Ginsenoside as radioprotectant via immunomodulation
Prolonged exposure to ultraviolet (UV) radiation, especially UVB, can cause damaging effects within cells, involving DNA damage, inflammatory responses and oxidative stress, resulting in skin aging. Ginsenoside Rk1 significantly inhibited the excessive production of ROS and enhanced antioxidant enzyme activity to attenuate oxidative damage. In addition, Masson staining and histological confirmed that Rk1 remarkably improved UVB-induced epidermal thickening, skin roughness, disorganized collagen fiber arrangement and wrinkles in BALB/c nude mice. The above results indicated that ginsenoside Rk1 could be used to develop natural dietary supplements for skin health [52]. Rh2 inhibited mitochondrial mitophagy in UV-exposed normal human dermal fibroblast (NHDF) cells damaged by reinstating membrane electrical potential and mitochondrial ATP production, causing restoration of cell proliferation, extracellular matrix (ECM) and antioxidant capacity [53]. Similarly, ginsenoside Rk1 could reduce intestinal epithelial cells apoptosis in RIII rats by inhibiting PI3K/AKT/mTOR pathway [54].
Immunity modulation in stress
Ginsenoside Rk1 protected human melanocytes from H2O2-induced oxidative stress by modulating the PI3K/Nrf2 pathway [55]. Rg3 regulated the oxidative phosphorylation pathway and augmented CD4+ CD25+ Foxp3 Treg cells function in RA mice [56]. Rg3 improved the immune response of LPS-stressed broilers, inhibiting pro-inflammatory cytokines and inflammatory mediators production [57]. Ginsenoside Rg6 promoted the expression of IL-10 and miR-146a expression in septic mice. The miR-146a is an anti-inflammation operational miRNA and is in charge of suppressing LPS-induced production of pro-inflammatory cytokines [58]. Ginsenoside Rg1 prevented complement-mediated damage to podocytes by repressing MAPK activation and reducing ROS production in membranous nephropathy (MN) podocyte injury mice [59]. Ginsenoside Rb1 reversed the excessive splenic apoptosis induced by Deoxynivalenol (DON) via regulating the mitochondria-mediated apoptosis pathway, down-regulated caspase-3, caspase-9 and Bax in mice. In addition, Rb1 promoted the accumulation of IgA, IgG and IgM [60]. F1-enhanced mixture improved mitotic and endoplasmic reticulum stress-related autophagic fluxes and inhibited apoptosis thus protecting against HFD-induced oxidative damage and cell aging in brain. F1-enhanced mixture declined the secretion of 24 factors in the hippocampus of mouse brain through NF-κB signaling pathway, such as several chemokines, growth factors and pro-inflammatory cytokines. The results provided explicit evidence for its potential as a functional food [61]. The anti-aging gene SIRT1 has a regulatory role in mitochondrial biogenesis, energy homeostasis, and prevention of oxidative stress [62, 63]. Ginsenoside Rh2 ameliorated mitochondrial dysfunction induced by H2O2 by promoting the expression of SIRT1 and PGC-1α genes [64]. Rg1 protected NSCs from OGD-induced oxidative stress by modulating Bax/Caspase3 and p38/JNK phosphorylation [65] (Table 3).
Role in hepatic disorders
Numerous studies showed that systemic inflammation was related to liver immune regulation (Fig. 4). Ginsenosides can inhibit inflammatory molecules and protect liver through ROS, MAPKs, NF-κB/AP-1, Keap1/Nrf2 and HO-1/ARE signaling pathways. Researchers suggested that the pathology of hepatic diseases is closely related to TLR-4 and the immune cascade [66], and a variety of liver injury models have been used to evaluate the immunomodulatory role of ginsenosides in liver diseases. For instance, ginsenoside Re mitigated alcohol hepatic injury by down-regulating TLRs [67]. Ginsenoside Rc relieved the damage of hepatocytes and oxidative stress in alcoholic liver disease (ALD) by up-regulating the SIRT6/NRF2 pathway [68]. Ginsenoside Rg1 could significantly reduce the liver weight and improve the structure of liver lobule in 2, 3, 7, 8-tetrachlorodibenzo-p-dioxin (TCDD)-induced liver injury mice by inhibiting CYP1A1 through the aryl hydrocarbon receptor [69]. 20(R)-Rg3 effectively reduced acetaminophen (APAP)-induced necrosis, apoptosis, and inflammatory infiltration of liver tissue cells by activating the PI3K/AKT signaling pathway [70]. Rg1 significantly reduced APAP-induced oxidative stress and hepatotoxicity by suppressing Keap-1 expression and up-regulating Nrf2 target genes. In addition, Rg1 could inhibit the activity of enzymes in the forming of the APAP toxic metabolite [71]. Similarly, ginsenoside Rg1 promoted the survival rates of hepatocytes and liver repair in carbon tetrachloride-induced acute liver injury mice. Rg1 reduced the levels of AST, ALT, and ALP in serum and increased GSH, SOD and CAT in liver, which were related to the up-regulation of the Nrf2 pathway [72]. Ginsenoside 20(S)-Rh1 maintained the normal levels of FBG and insulin, reducing the apoptosis of liver tissue by inhibiting the activation of the Akt/FoxO1 pathway, effectively improving the liver injury caused by type 2 diabetes [73]. Ginsenoside Rg2 inhibited the expression of liver autophagy-related proteins by triggering the Akt/mTOR signaling pathway, improving liver fibrosis induced by a high-fat diet (CDAHFD). The same results were obtained in vitro experiments [74].
Role in hematopoietic disorders
PDS-C could improve the myelosuppression state of mice and promote the production of BM hematopoietic cells. It found that after the intervention of PDS-C, the counts of white blood cells, platelets, and neutrophils in mice were remarkably increased in a concentration-dependent manner, the myelosuppression state of AA was significantly reduced, and the number of hematopoietic cells in BM was enriched. In addition, PDS-C treatment increased CD4+CD25+FoxP3+ cells. These results indicated that PDS-C has dual activities of boosting hematopoiesis and modulating immunity [75]. Ginsenoside Rg1 could also improve hematopoietic stem cells by inhibiting mitochondrial apoptosis caused by Bax translocation, thereby restoring hematopoietic function [76]. Ginsenoside Rb1 inhibited NLK expression and promoted erythropoiesis in models of diamond-Beckfan anemia (DBA). Among them, NLK is a fragment of the MAPK family, whose activation contributes to the pathogenesis of DBA. Therefore, NLK is considered a potential therapeutic target [77]. These data indicated that ginsenosides can regulate immunity positively to restore hematopoietic function (Fig. 5A).
Ginsenosides promoted the proliferation and differentiation of hematopoietic stem cells in bone marrow, which differentiated into neutrophils and lymphocytes, enhancing the recovery of hematopoietic and immune functions. Ginsenosides participated in the intestinal immune process by regulating the functions of IgG+ plasma cells, macrophages, DC cells and T cells, which effectively improved microbial dysbiosis, dysfunction of tight junctions and impaired mucosal barrier
Role in intestinal disorders
The intestine holds the vast majority of immune cells in the human body. Intestinal ecological disorders can destroy the intestinal epithelial barrier, cause host immune dysfunction, and lead to cancer. Ginsenosides can regulate intestinal immunity through various pathways (Fig. 5B). Ginsenoside Rb1 inhibited inflammatory response and oxidative stress by regulating the PI3K/Akt/Nrf2 pathway in ischemia/reperfusion (IR) damage mice [78]. Rk1 alleviated the apoptosis of intestinal epithelial cells induced by oxidative stress in RIII rats. The pathway of the anti-apoptotic effect may concern the inhibition of PI3K/AKT/mTOR [54]. With the emergence of intestinal flora research, there is no doubt that it provides a new thought to study the immune mechanisms of ginsenosides. Intestinal microbiota cooperate with the immune system to maintain the balance and homeostasis of the internal environment, and normal microbiota can stimulate the host to produce immunity or elimination function. Ginsenoside Rg1 improved effectively the body weight, colon length, change rate of colon mass index and colon mucosal injury in UC mice. Rg1 also increased the variety of colon flora and the proportion of beneficial bacteria [79]. Ginsenoside Rb1 reduced the proportion of Bacteroides and promoted the proportion of phylum Verrucomicrobia and the genus Akkermansia [80]. Rg1 regulated the structure of gut microbiota and increased the relative abundance of gut microbiota in mice, such as Roseburia, Lachnospiraceae, Ruminococcaceae and Alistipes, while the relative abundance of potential pathogens such as Alloprevotella, Helicobacteraceae, Allobaculum, Dubosiella and Mycoplasma was decreased. Meanwhile, Rg1 improved the inflammation of colon tissue and repaired the damaged mucosal barrier. This indicates that Rg1 can enhance immunity by regulating the homeostasis of intestinal microflora in mice [16]. Ginsenoside Rg1 significantly increased the abundance of Bacteroidetes and Firmicutes and reduced the relative abundance of Proteobacteria and Cyanobacteria in morphine-induced intestinal flora dysbiosis mice [81].
Clinical trials about ginsenoside immune modulation
The ameliorative effects of ginsenosides on immune-related diseases have been shown not only in cellular and animal experiments but also in available human data. Clinically, 414 patients suffering from NSCLC improved their symptoms, reduced chemotherapy-induced myelosuppression and prolonged their survival after receiving a combination of Rg3 and chemotherapy [82]. Additionally, Shengmai injection containing ginsenoside Re, Rg1, and Rb1 is used as adjunctive therapy for chronic obstructive pulmonary disease (COPD) in combination with western medications to improve overall clinical effectiveness and lung function according to the results of 23 rationalized controlled trials involving 1804 participants [83]. A study evaluated the effectiveness of ginseng extracts GS-3K8 and GINST in the prophylaxis of acute respiratory illness (ARI), where GS-3K8 was a ginseng extract enriched with PPD-type ginsenosides, and GINST was a pectinase-processed ginseng extract. A total of 45 participants in the study were directed to take two caplets after each meal for 12 weeks, with the incidence of ARI and duration of symptoms as the primary clinical indicators. The results indicated that GS-3K8 and GINST had a preventive effect on ARI [84]. It was reported that ginsenosides alleviated the adverse reactions caused by chemotherapy, and has been prescribed as an adjuvant to TACE for hepatocellular carcinoma (HCC) [85]. A clinical study included 1308 patients and explored the efficacy of TACE combined with ginsenosides Rg3, Rh2, CK and total ginsenoside GS in the treatment of HCC, with the quality of life, tumor response, liver function, survival rates and adverse reactions as the main indicators. The results showed that both short-term and long-term treatment of ginsenosides improved liver function and reduced adverse reactions during TACE treatment. It also showed that ginsenoside was an effective and reliable adjuvant in tumor therapy [86]. PI3K/AKT pathway was thought to play an influential role in inhibiting HCC growth by Rk3. It was reported that Rk3 prolonged the survival of HCC patients by inhibiting PI3K/AKT pathway signaling in clinical samples [31]. The research found a remarkable drop in central and peripheral arterial blood pressure in healthy people after ingesting Rg3 isolated from red ginseng, suggesting that ginsenosides have a preventive effect against cardiovascular disease [87]. Ginsenoside Rg3 restored the morphology and function of normal human dermal fibroblasts under UV irradiation and promoted protein expression related to antioxidant activity and cell proliferation [88].
Although a considerable amount of preclinical information has been available to support the concept that ginsenosides may modulate human immunity through multiple pathways, unfortunately, the efficacy and safety of the clinical application of ginsenosides are still controversial and even contradictory. With disappointment, the translation process from accomplished preclinical results to operative clinical settings, and useful clinical evidence is often missing. Therefore, much work has to be done in this regard to adequately define the potential of ginsenosides as dietary supplements.
Bioavailability of ginsenosides
Absorption, distribution, metabolism and excretion of ginsenosides are crucial for interpreting their immunomodulatory effects. It was reported that ginsenosides could be rapidly absorbed in the gastrointestinal tract [89] and metabolized in liver microsomes [90]. In addition, less than 2% of orally administered ginsenosides were recovered in human urine, suggesting that most ginsenosides are not absorbed in their original form [91]. Ginsenosides come into contact with gastrointestinal fluids containing gastric acid and gastric enzymes, enteric enzymes, and colonic bacteria after oral administration, and most of the intact ginsenosides are metabolized and converted in the gastrointestinal tract to ginsenosides with more biological effects [92]. Taking PPT-type ginsenoside Re as an example, Re was converted to secondary metabolites Rg2, Rh1, F1 and PPT by intestinal flora, and oxidation and deglycosylation were the main metabolic processes of Re. These secondary metabolites could be more readily absorbed into the bloodstream and enter the body circulation. Moreover, Re was hardly detected in the feces of rats, while its metabolites could be detected [93]. Another study reported that PPT-type ginsenoside Rg2 was converted to four metabolites, M1-M4, in rat liver microsomes, and these metabolites had enhanced biological activity [90]. Kang et al. reported that the biotransformation of PPD-type ginsenoside Rb1 was mainly realized by various enzymes secreted by microorganisms in the intestine. Ginsenoside Rb1 was rapidly hydrolyzed by intestinal flora to Rd, which is then mostly deglycosylated to F2. Rd and F2 were further hydrolyzed to CK, a major deglycosylated metabolite readily absorbed into the systemic circulation [94]. Hong et al. proposed a feasible metabolic pathway for PPD-type ginsenoside Rg5. A total of 17 metabolites were detected in biological samples, including rat liver microsomes (13), rat urine (5), feces (5) and plasma (5). Oxidation, deglycosylation, deoxygenation, glucuronidation, demethylation, and dehydration were the major metabolic reactions of Rg5, and fecal clearance was the major excretion route of Rg5 and its metabolites [95].
The dammarane backbone and glycosyl structure of ginsenosides leads to poor cell permeability and low bioavailability in the human body, resulting in limiting the utilization of ginsenosides [96]. Current methods on improvements of the poor oral bioavailability of ginsenosides include pretreatment, structural modification, drug combination, and micro- and nano-delivery. Specifically, the bioavailability of ginsenosides can be effectively improved by using genetic engineering techniques to obtain strains with high deglycosylation activity or heat treatment to pretreat ginsenosides [97, 98]. Cell membranes are mainly composed of lipids, so the structural modification mainly improves the membrane permeability of ginsenosides by increasing the lipophilicity of ginsenosides [99, 100]. Numerous studies have revealed that the combination of ginsenosides with certain drugs, such as prebiotics, borneol and verapamil, could effectively improve their oral bioavailability [101, 102]. Tiny particles are easily absorbed by the body. The tiny droplet size of a micro (or nano)-system have large interfacial surface areas that controls the release and absorption of ginsenoside. In addition, micro- or nano- delivery system also modify the lipophilicity or hydrophilcity of ginsenoside, thereby, enhance the penetrability of ginsenoside [103, 104]. In the context of dietary support and functional foods, these technologies may tremendously improve the effectiveness, safety and bioavailability of ginsenosides, but their anticipated amplification of immune potential, increased utilization and reduced toxicity still need to be optimized and discovered.
Further considerations and conclusive remarks
Recently, many studies have preliminarily elucidated the immunomodulatory activities of ginsenosides, but there are still some problems to be addressed. First of all, the modernization of plant active components is an arduous task. Ginsenosides may vary significantly in nature, active ingredient content, and efficacy due to the use of different extraction, isolation and purification methods. Therefore, professionals must strive to bring about improvements in production and detection systems, and more clinical studies are needed to confirm the efficacy of ginsenosides in modulating the body’s immune system and to explore precise immunomodulatory mechanisms. Secondly, the current research on the immunocompetence of ginsenosides mainly focuses on the detection of immune organs or peripheral blood indicators but does not combine the actual absorption and utilization of different ginsenosides in the human body, which is not conducive to the overall description of the immune pathway of ginsenosides, and it is difficult to conclude a reasonable recommended dosage through such studies. Furthermore, most of the experiments were conducted in young mice over a short period of time and mostly under pathological conditions. However, they are not adequate to elucidate the complex diversity of pathological changes during the evolution of human immune disorders. Large animal models (guinea pigs, rabbits, dogs, and monkeys) due to their significant genetic, physiological, biochemical and metabolic similarities to humans, can close the gap between fundamental research and cautious clinical applications and also facilitate the establishment of an appropriate ginsenoside delivery system, which would alleviate bioavailability barriers. Currently, some investigators provide shallow results, whereas others refuse to offer suitable information related to clinical outcomes or quantify clinical significance. Therefore, more research in this area is urgently needed to eliminate inconsistencies and to contribute worthwhile information for the prospective development of ginsenoside functional foods. Although few studies reported negative effects of ginsenosides, it is crucial to assess their safety. A dose-dependent increase in the toxicity of ginsenosides in animals has been reported [105]. And ginsenosides caused different degrees of toxicity in different experimental animals [106, 107]. Therefore, professionals need to carefully investigate the underlying toxigenicity of ginsenosides, which will help in framing safety and efficacy studies in the future.
The research on the immunocompetence of ginsenosides is still a vast uncultivated land. It is necessary to further explore the specific molecular targets and pathways of ginsenosides from multiple perspectives and in an all-round way, which is of great value for formulating novel dietary strategies to prevent and improve immune disorders.
Availability of data and materials
Data availability is not applicable to this article as no new data were created or analyzed in this study.
References
Huang L, Shen M, Wu T et al (2020) Mesona chinensis Benth polysaccharides protect against oxidative stress and immunosuppression in cyclophosphamide-treated mice via MAPKs signal transduction pathways. Int J Biol Macromol 152:766–774. https://doi.org/10.1016/j.ijbiomac.2020.02.318
Conrad N, Misra S, Verbakel JY et al (2023) Incidence, prevalence, and co-occurrence of autoimmune disorders over time and by age, sex, and socioeconomic status: a population-based cohort study of 22 million individuals in the UK. Lancet 401:1878–1890. https://doi.org/10.1016/S0140-6736(23)00457-9
Bascones-Martinez A, Mattila R, Gomez-Font R, Meurman JH (2014) Immunomodulatory drugs: oral and systemic adverse effects. Med Oral Patol Oral Cir Bucal 19:e24-31. https://doi.org/10.4317/medoral.19087
Zhang J, Ai Z, Wu J et al (2023) Effects of commercial sterilization on non-ginsenoside functional components in fresh ginseng pulps using widely targeted metabolomics. LWT 183:114926. https://doi.org/10.1016/j.lwt.2023.114926
Yang W-Z, Hu Y, Wu W-Y et al (2014) Saponins in the genus Panax L. (Araliaceae): a systematic review of their chemical diversity. Phytochemistry 106:7–24. https://doi.org/10.1016/j.phytochem.2014.07.012
In G, Ahn N-G, Bae B-S et al (2017) In situ analysis of chemical components induced by steaming between fresh ginseng, steamed ginseng, and red ginseng. J Ginseng Res 41:361–369. https://doi.org/10.1016/j.jgr.2016.07.004
Jang GY, Kim MY, Lee YJ et al (2018) Influence of organic acids and heat treatment on ginsenoside conversion. J Ginseng Res 42:532–539. https://doi.org/10.1016/j.jgr.2017.07.008
Simurabiye JB, Yen LTH, Doan ND et al (2022) Optimization of Panax notoginseng root extract hydrolysis by Cordyceps militaris derived glycosidase and bioactivities of hydrolysis products. Sci Afr 15:e01082. https://doi.org/10.1016/j.sciaf.2021.e01082
Zhang J, Ai Z, Hu Y et al (2022) Remarkable impact of commercial sterilizing on ginsenosides transformation in fresh ginseng pulp based on widely targeted metabolomics analysis. Food Chem X 15:100415. https://doi.org/10.1016/j.fochx.2022.100415
Yao F, Sun J, Cao X et al (2020) Steamed ginseng shoot extract rich in less-polar ginsenosides ameliorated the acute hepatotoxicity caused by overdose of acetaminophen in mice. J Funct Foods 73:104155. https://doi.org/10.1016/j.jff.2020.104155
Wang Y, Liu Y, Zhang X-Y et al (2014) Ginsenoside Rg1 regulates innate immune responses in macrophages through differentially modulating the NF-κB and PI3K/Akt/mTOR pathways. Int Immunopharmacol 23:77–84. https://doi.org/10.1016/j.intimp.2014.07.028
Kim M-Y, Cho JY (2013) 20S-dihydroprotopanaxadiol, a ginsenoside derivative, boosts innate immune responses of monocytes and macrophages. J Ginseng Res 37:293–299. https://doi.org/10.5142/jgr.2013.37.293
Yang WS, Yi Y-S, Kim D et al (2017) Nuclear factor kappa-B- and activator protein-1-mediated immunostimulatory activity of compound K in monocytes and macrophages. J Ginseng Res 41:298–306. https://doi.org/10.1016/j.jgr.2016.06.004
Kang S, Park S-J, Lee A-Y et al (2018) Ginsenoside Rg3 promotes inflammation resolution through M2 macrophage polarization. J Ginseng Res 42:68–74. https://doi.org/10.1016/j.jgr.2016.12.012
Huang Y, Zou Y, Lin L, Zheng R (2017) Ginsenoside Rg1 activates dendritic cells and acts as a vaccine adjuvant inducing protective cellular responses against lymphomas. DNA Cell Biol 36:1168–1177. https://doi.org/10.1089/dna.2017.3923
Yousuf S, Liu H, Yingshu Z et al (2022) Ginsenoside Rg1 modulates intestinal microbiota and supports re-generation of immune cells in dexamethasone-treated mice. Acta Microbiol Immunol Hung 69:259–269. https://doi.org/10.1556/030.2022.01881
Wu R, Ru Q, Chen L et al (2014) Stereospecificity of Ginsenoside Rg3 in the promotion of cellular immunity in hepatoma H22-bearing mice: Rg3 stereospecificity in immune response…. J Food Sci 79:H1430–H1435. https://doi.org/10.1111/1750-3841.12518
Su X, Pei Z, Hu S (2014) Ginsenoside Re as an adjuvant to enhance the immune response to the inactivated rabies virus vaccine in mice. Int Immunopharmacol 20:283–289. https://doi.org/10.1016/j.intimp.2014.03.008
Li R, Ma Y, Zhai L et al (2016) Enhanced immune response to foot-and-mouth disease vaccine by oral administration of ginseng stem-leaf saponins. Immunopharmacol Immunotoxicol 38:257–263. https://doi.org/10.1080/08923973.2016.1184680
Bi S, Chi X, Zhang Y et al (2018) Ginsenoside Rg1 enhanced immune responses to infectious bursal disease vaccine in chickens with oxidative stress induced by cyclophosphamide. Poult Sci 97:2698–2707. https://doi.org/10.3382/ps/pey132
Kim J, Byeon H, Im K, Min H (2018) Effects of ginsenosides on regulatory T cell differentiation. Food Sci Biotechnol 27:227–232. https://doi.org/10.1007/s10068-017-0255-3
Zou Y, Tao T, Tian Y et al (2013) Ginsenoside Rg1 improves survival in a murine model of polymicrobial sepsis by suppressing the inflammatory response and apoptosis of lymphocytes. J Surg Res 183:760–766. https://doi.org/10.1016/j.jss.2013.01.068
Zhang M, Hu S, Tao J et al (2019) Ginsenoside compound-K inhibits the activity of B cells through inducing IgD-B cell receptor endocytosis in mice with collagen-induced arthritis. Inflammopharmacology 27:845–856. https://doi.org/10.1007/s10787-019-00608-2
Yuan Z, Jiang H, Zhu X et al (2017) Ginsenoside Rg3 promotes cytotoxicity of Paclitaxel through inhibiting NF-κB signaling and regulating Bax/Bcl-2 expression on triple-negative breast cancer. Biomed Pharmacother 89:227–232. https://doi.org/10.1016/j.biopha.2017.02.038
Xie Q, Wen H, Zhang Q et al (2017) Inhibiting PI3K-AKt signaling pathway is involved in antitumor effects of ginsenoside Rg3 in lung cancer cell. Biomed Pharmacother 85:16–21. https://doi.org/10.1016/j.biopha.2016.11.096
Lu Z, Xu H, Yu X et al (2018) 20(S)-Protopanaxadiol induces apoptosis in human hepatoblastoma HepG2 cells by downregulating the protein kinase B signaling pathway. Exp Ther Med 15:1277–1284. https://doi.org/10.3892/etm.2017.5594
Lee H, Lee S, Jeong D, Kim SJ (2018) Ginsenoside Rh2 epigenetically regulates cell-mediated immune pathway to inhibit proliferation of MCF-7 breast cancer cells. J Ginseng Res 42:455–462. https://doi.org/10.1016/j.jgr.2017.05.003
Chen F, Sun Y, Zheng S-L et al (2017) Antitumor and immunomodulatory effects of ginsenoside Rh2 and its octyl ester derivative in H22 tumor-bearing mice. J Funct Foods 32:382–390. https://doi.org/10.1016/j.jff.2017.03.013
Xia T, Zhang B, Li Y et al (2020) New insight into 20(S)-ginsenoside Rh2 against T-cell acute lymphoblastic leukemia associated with the gut microbiota and the immune system. Eur J Med Chem 203:112582. https://doi.org/10.1016/j.ejmech.2020.112582
Wang M, Yan SJ, Zhang HT et al (2017) Ginsenoside Rh2 enhances the antitumor immunological response of a melanoma mice model. Oncol Lett. https://doi.org/10.3892/ol.2016.5490
Qu L, Liu Y, Deng J et al (2023) Ginsenoside Rk3 is a novel PI3K/AKT-targeting therapeutics agent that regulates autophagy and apoptosis in hepatocellular carcinoma. J Pharm Anal. https://doi.org/10.1016/j.jpha.2023.03.006
Han S, Jeong AJ, Yang H et al (2016) Ginsenoside 20(S)-Rh2 exerts anti-cancer activity through targeting IL-6-induced JAK2/STAT3 pathway in human colorectal cancer cells. J Ethnopharmacol 194:83–90. https://doi.org/10.1016/j.jep.2016.08.039
Tang Y-C, Zhang Y, Zhou J et al (2018) Ginsenoside Rg3 targets cancer stem cells and tumor angiogenesis to inhibit colorectal cancer progression in vivo. Int J Oncol 52:127–138. https://doi.org/10.3892/ijo.2017.4183
Li H, Li H (2020) Ginsenoside-Rg5 inhibits growth and metastasis of ovarian carcinoma via suppressing expression of fibroblast growth factor-8b (FGF8b). J King Saud Univ Sci 32:1162–1167. https://doi.org/10.1016/j.jksus.2019.11.001
Liu J, Wang Y, Yu Z et al (2022) Functional mechanism of ginsenoside compound K on tumor growth and metastasis. Integr Cancer Ther 21:15347354221101204. https://doi.org/10.1177/15347354221101203
Wei Q, Ren Y, Zheng X et al (2022) Ginsenoside Rg3 and sorafenib combination therapy relieves the hepatocellular carcinomaprogression through regulating the HK2-mediated glycolysis and PI3K/Akt signaling pathway. Bioengineered 13:13919–13928. https://doi.org/10.1080/21655979.2022.2074616
Li Q, He J, Li S et al (2023) The combination of gemcitabine and ginsenoside Rh2 enhances the immune function of dendritic cells against pancreatic cancer via the CARD9-BCL10-MALT1 / NF-κB pathway. Clin Immunol 248:109217. https://doi.org/10.1016/j.clim.2022.109217
Lee Y, Park A, Park Y-J et al (2022) Ginsenoside 20(R)-Rg3 enhances natural killer cell activity by increasing activating receptor expression through the MAPK/ERK signaling pathway. Int Immunopharmacol 107:108618. https://doi.org/10.1016/j.intimp.2022.108618
Han J, Wang Y, Cai E et al (2019) Study of the effects and mechanisms of ginsenoside compound K on myelosuppression. J Agric Food Chem 67:1402–1408. https://doi.org/10.1021/acs.jafc.8b06073
Sun X, Zhao Y-N, Qian S et al (2018) Ginseng-derived panaxadiol saponins promote hematopoiesis recovery in cyclophosphamide-induced myelosuppressive mice: potential novel treatment of chemotherapy-induced cytopenias. Chin J Integr Med 24:200–206. https://doi.org/10.1007/s11655-017-2754-8
Liu X, Zhang Z, Liu J et al (2019) Ginsenoside Rg3 improves cyclophosphamide-induced immunocompetence in Balb/c mice. Int Immunopharmacol 72:98–111. https://doi.org/10.1016/j.intimp.2019.04.003
Xin C, Kim J, Quan H et al (2019) Ginsenoside Rg3 promotes Fc gamma receptor-mediated phagocytosis of bacteria by macrophages via an extracellular signal-regulated kinase 1/2 and p38 mitogen-activated protein kinase-dependent mechanism. Int Immunopharmacol 77:105945. https://doi.org/10.1016/j.intimp.2019.105945
Xin C, Quan H, Kim J-M et al (2019) Ginsenoside Rb1 increases macrophage phagocytosis through p38 mitogen-activated protein kinase/Akt pathway. J Ginseng Res 43:394–401. https://doi.org/10.1016/j.jgr.2018.05.003
Kang S, Song MJ, Min H (2018) Antiviral activity of ginsenoside Rg3 isomers against gammaherpesvirus through inhibition of p38- and JNK-associated pathways. J Funct Foods 40:219–228. https://doi.org/10.1016/j.jff.2017.11.011
Kang N, Gao H, He L et al (2021) Ginsenoside Rb1 is an immune-stimulatory agent with antiviral activity against enterovirus 71. J Ethnopharmacol 266:113401. https://doi.org/10.1016/j.jep.2020.113401
Kang L-J, Choi Y-J, Lee S-G (2013) Stimulation of TRAF6/TAK1 degradation and inhibition of JNK/AP-1 signalling by ginsenoside Rg3 attenuates hepatitis B virus replication. Int J Biochem Cell Biol 45:2612–2621. https://doi.org/10.1016/j.biocel.2013.08.016
Jin G-N, Lu J-M, Lan H-W et al (2022) Protective effect of ginsenoside Rh2 against Toxoplasma gondii infection-induced neuronal injury through binding TgCDPK1 and NLRP3 to inhibit microglial NLRP3 inflammasome signaling pathway. Int Immunopharmacol 112:109176. https://doi.org/10.1016/j.intimp.2022.109176
Chen X, Xu T, Lv X et al (2021) Ginsenoside Rh2 alleviates ulcerative colitis by regulating the STAT3/miR-214 signaling pathway. J Ethnopharmacol. https://doi.org/10.1016/j.jep.2021.113997
Yu X, Zhang N, Lin W et al (2018) Regulatory effects of four ginsenoside monomers in humoral immunity of systemic lupus erythematosus. Exp Ther Med 15:2097–2103. https://doi.org/10.3892/etm.2017.5657
Xu C, Li L, Wang C et al (2022) Effects of G-Rh2 on mast cell-mediated anaphylaxis via AKT-Nrf2/NF-κB and MAPK-Nrf2/NF-κB pathways. J Ginseng Res 46:550–560. https://doi.org/10.1016/j.jgr.2021.10.001
Wc H, Th H, Kw Y et al (2021) Ginsenoside Rg3 ameliorates allergic airway inflammation and oxidative stress in mice. J Ginseng Res. https://doi.org/10.1016/j.jgr.2021.03.002
Liu Y, Qu L, Wan S et al (2022) Ginsenoside Rk1 prevents UVB irradiation-mediated oxidative stress, inflammatory response, and collagen degradation via the PI3K/AKT/NF-κB pathway in vitro and in vivo. J Agric Food Chem 70:15804–15817. https://doi.org/10.1021/acs.jafc.2c06377
Lee H, Kong G, Park J, Park J (2022) The potential inhibitory effect of ginsenoside Rh2 on mitophagy in UV-irradiated human dermal fibroblasts. J Ginseng Res 46:646–656. https://doi.org/10.1016/j.jgr.2022.02.001
Wang Y, Su P, Zhuo Z et al (2023) Ginsenoside Rk1 attenuates radiation-induced intestinal injury through the PI3K/AKT/mTOR pathway. Biochem Biophys Res Commun 643:111–120. https://doi.org/10.1016/j.bbrc.2022.12.072
Xiong J, Yang J, Yan K, Guo J (2021) Ginsenoside Rk1 protects human melanocytes from H2O2-induced oxidative injury via regulation of the PI3K/AKT/Nrf2/HO-1 pathway. Mol Med Rep 24:821. https://doi.org/10.3892/mmr.2021.12462
Zhang Y, Wang S, Song S et al (2020) Ginsenoside Rg3 alleviates complete Freund’s adjuvant-induced rheumatoid arthritis in mice by regulating CD4 + CD25 + Foxp3 + Treg cells. J Agric Food Chem 68:4893–4902. https://doi.org/10.1021/acs.jafc.0c01473
Bi S, Shao J, Qu Y et al (2022) Serum metabolomics reveal pathways associated with protective effect of ginsenoside Rg3 on immune stress. Poult Sci 101:102187. https://doi.org/10.1016/j.psj.2022.102187
Paik S, Choe JH, Choi G-E et al (2019) Rg6, a rare ginsenoside, inhibits systemic inflammation through the induction of interleukin-10 and microRNA-146a. Sci Rep 9:4342. https://doi.org/10.1038/s41598-019-40690-8
Zhang M-H, Fan J, Xie X et al (2011) Ginsenoside-Rg1 protects podocytes from complement mediated injury. J Ethnopharmacol 137:99–107. https://doi.org/10.1016/j.jep.2011.04.045
Rajput SA, Shaukat A, Rajput IR et al (2021) Ginsenoside Rb1 prevents deoxynivalenol-induced immune injury via alleviating oxidative stress and apoptosis in mice. Ecotoxicol Environ Saf 220:112333. https://doi.org/10.1016/j.ecoenv.2021.112333
Hou J, Jeon B, Baek J et al (2022) High fat diet-induced brain damaging effects through autophagy-mediated senescence, inflammation and apoptosis mitigated by ginsenoside F1-enhanced mixture. J Ginseng Res 46:79–90. https://doi.org/10.1016/j.jgr.2021.04.002
Di Emidio G, Falone S, Vitti M et al (2014) SIRT1 signalling protects mouse oocytes against oxidative stress and is deregulated during aging. Hum Reprod 29:2006–2017. https://doi.org/10.1093/humrep/deu160
Tatone C, Di Emidio G, Barbonetti A et al (2018) Sirtuins in gamete biology and reproductive physiology: emerging roles and therapeutic potential in female and male infertility. Hum Reprod Update 24:267–289. https://doi.org/10.1093/humupd/dmy003
Liu H, An Z-Y, Li Z-Y et al (2023) The ginsenoside Rh2 protects porcine oocytes against aging and oxidative stress by regulating SIRT1 expression and mitochondrial activity. Theriogenology 200:125–135. https://doi.org/10.1016/j.theriogenology.2023.02.006
Li Y, Suo L, Liu Y, et al (2017) Protective effects of ginsenoside Rg1 against oxygen-glucose-deprivation-induced apoptosis in neural stem cells. J Neurol Sci
Bang CS, Hong SH, Suk KT et al (2014) Effects of Korean Red Ginseng (Panax ginseng), urushiol (Rhus vernicifera Stokes), and probiotics (Lactobacillus rhamnosus R0011 and Lactobacillus acidophilus R0052) on the gut-liver axis of alcoholic liver disease. J Ginseng Res 38:167–172. https://doi.org/10.1016/j.jgr.2014.04.002
Lee I-A, Hyam SR, Jang S-E et al (2012) Ginsenoside re ameliorates inflammation by inhibiting the binding of lipopolysaccharide to TLR4 on macrophages. J Agric Food Chem 60:9595–9602. https://doi.org/10.1021/jf301372g
Pan Z, Guo J, Tang K et al (2022) Ginsenoside Rc modulates SIRT6-NRF2 interaction to alleviate alcoholic liver disease. J Agric Food Chem 70:14220–14234. https://doi.org/10.1021/acs.jafc.2c06146
Li H, Gao Y, Song L et al (2022) Ginsenoside Rg1 protects mice against 2,3,7,8-tetrachlorodibenzo-p-dioxin-induced liver injury by inhibiting CYP1A1 through the aryl hydrocarbon receptor. J Ethnopharmacol 294:115394. https://doi.org/10.1016/j.jep.2022.115394
Zhou Y-D, Hou J-G, Liu W et al (2018) 20(R)-ginsenoside Rg3, a rare saponin from red ginseng, ameliorates acetaminophen-induced hepatotoxicity by suppressing PI3K/AKT pathway-mediated inflammation and apoptosis. Int Immunopharmacol 59:21–30. https://doi.org/10.1016/j.intimp.2018.03.030
Ning C, Gao X, Wang C et al (2018) Ginsenoside Rg1 protects against acetaminophen-induced liver injury via activating Nrf2 signaling pathway in vivo and in vitro. Regul Toxicol Pharmacol 98:58–68. https://doi.org/10.1016/j.yrtph.2018.07.012
Ning C, Gao X, Wang C et al (2018) Hepatoprotective effect of ginsenoside Rg1 from Panax ginseng on carbon tetrachloride-induced acute liver injury by activating Nrf2 signaling pathway in mice. Environ Toxicol 33:1050–1060. https://doi.org/10.1002/tox.22616
Su W-Y, Fan M-L, Li Y et al (2022) 20(S)-ginsenoside Rh1 alleviates T2DM induced liver injury via the Akt/FOXO1 pathway. Chin J Nat Med 20:669–678. https://doi.org/10.1016/S1875-5364(22)60201-2
He Z, Chen S, Pan T et al (2022) Ginsenoside Rg2 ameliorating CDAHFD-induced hepatic fibrosis by regulating AKT/mTOR-mediated autophagy. J Agric Food Chem 70:1911–1922. https://doi.org/10.1021/acs.jafc.1c07578
Zheng Z-Y, Yu X-L, Dai T-Y et al (2019) Panaxdiol saponins component promotes hematopoiesis and modulates T lymphocyte dysregulation in aplastic anemia model mice. Chin J Integr Med 25:902–910. https://doi.org/10.1007/s11655-019-3049-z
Cao H, Wei W, Xu R, Cui X (2021) Ginsenoside Rg1 can restore hematopoietic function by inhibiting Bax translocation-mediated mitochondrial apoptosis in aplastic anemia. Sci Rep 11:12742. https://doi.org/10.1038/s41598-021-91471-1
Wilkes MC, Jung K, Lee BE et al (2021) The active component of ginseng, ginsenoside Rb1, improves erythropoiesis in models of Diamond-Blackfan anemia by targeting Nemo-like kinase. J Biol Chem 297:100988. https://doi.org/10.1016/j.jbc.2021.100988
Chen S, Li X, Wang Y et al (2019) Ginsenoside Rb1 attenuates intestinal ischemia/reperfusion-induced inflammation and oxidative stress via activation of the PI3K/Akt/Nrf2 signaling pathway. Mol Med Rep 19:3633–3641. https://doi.org/10.3892/mmr.2019.10018
Long J, Liu X-K, Kang Z-P et al (2022) Ginsenoside Rg1 ameliorated experimental colitis by regulating the balance of M1/M2 macrophage polarization and the homeostasis of intestinal flora. Eur J Pharmacol 917:174742. https://doi.org/10.1016/j.ejphar.2022.174742
Sung M, Yoon Y, Lee J (2021) Intestinal Lactobacillus species improve immune enhancement by ginsenoside Rb1 and ginsenoside Rb1 increases intestinal Akkermansia proportions. J Funct Foods 86:104730. https://doi.org/10.1016/j.jff.2021.104730
Chen Z, Lin Y, Zhou Q et al (2022) Ginsenoside Rg1 mitigates morphine dependence via regulation of gut microbiota, tryptophan metabolism, and serotonergic system function. Biomed Pharmacother 150:112935. https://doi.org/10.1016/j.biopha.2022.112935
Zhang Y, Wang XQ, Liu H et al (2018) A multicenter, large-sample, randomized clinical trial on improving the median survival time of advanced non-small cell lung cancer by combination of Ginseng Rg3 and chemotherapy. Zhonghua Zhong Liu Za Zhi 40:295–299. https://doi.org/10.3760/cma.j.issn.0253-3766.2018.04.011
Huang X, Duan X, Wang K et al (2019) Shengmai injection as an adjunctive therapy for the treatment of chronic obstructive pulmonary disease: a systematic review and meta-analysis. Complement Ther Med 43:140–147. https://doi.org/10.1016/j.ctim.2019.01.020
Hwang J-H, Park S-H, Choi E-K et al (2020) A randomized, double-blind, placebo-controlled pilot study to assess the effects of protopanaxadiol saponin–enriched ginseng extract and pectinase-processed ginseng extract on the prevention of acute respiratory illness in healthy people. J Ginseng Res 44:697–703. https://doi.org/10.1016/j.jgr.2019.01.002
Zhou B, Yan Z, Liu R et al (2016) Prospective study of transcatheter arterial chemoembolization (TACE) with ginsenoside Rg3 versus TACE alone for the treatment of patients with advanced hepatocellular carcinoma. Radiology 280:630–639. https://doi.org/10.1148/radiol.2016150719
Zhu H, Wang S-Y, Zhu J-H et al (2021) Efficacy and safety of transcatheter arterial chemoembolization combined with ginsenosides in hepatocellular carcinoma treatment. Phytomedicine 91:153700. https://doi.org/10.1016/j.phymed.2021.153700
Jovanovski E, Bateman EA, Bhardwaj J et al (2014) Effect of Rg3-enriched Korean red ginseng (Panax ginseng) on arterial stiffness and blood pressure in healthy individuals: a randomized controlled trial. J Am Soc Hypertens 8:537–541. https://doi.org/10.1016/j.jash.2014.04.004
Lee H, Hong Y, Tran Q et al (2019) A new role for the ginsenoside RG3 in antiaging via mitochondria function in ultraviolet-irradiated human dermal fibroblasts. J Ginseng Res 43:431–441. https://doi.org/10.1016/j.jgr.2018.07.003
Li X, Sun J, Wang G et al (2007) Simultaneous determination of panax notoginsenoside R1, ginsenoside Rg1, Rd, Re and Rb1 in rat plasma by HPLC/ESI/MS: platform for the pharmacokinetic evaluation of total panax notoginsenoside, a typical kind of multiple constituent traditional Chinese medicine. Biomed Chromatogr 21:735–746. https://doi.org/10.1002/bmc.813
Ma L-Y, Zhou Q-L, Yang X-B et al (2016) Metabolism of 20(S)-ginsenoside Rg2 by rat liver microsomes: bioactivation to SIRT1-activating metabolites. Molecules 21:757. https://doi.org/10.3390/molecules21060757
Cui JF, Björkhem I, Eneroth P (1997) Gas chromatographic-mass spectrometric determination of 20(S)-protopanaxadiol and 20(S)-protopanaxatriol for study on human urinary excretion of ginsenosides after ingestion of ginseng preparations. J Chromatogr B Biomed Sci Appl 689:349–355. https://doi.org/10.1016/s0378-4347(96)00304-0
Hasegawa H (2004) Proof of the mysterious efficacy of ginseng: basic and clinical trials: metabolic activation of ginsenoside: deglycosylation by intestinal bacteria and esterification with fatty acid. J Pharmacol Sci 95:153–157. https://doi.org/10.1254/jphs.fmj04001x4
Peng D, Wang H, Qu C et al (2012) Ginsenoside Re: its chemistry, metabolism and pharmacokinetics. Chin Med 7:2. https://doi.org/10.1186/1749-8546-7-2
Kang A, Zhang S, Zhu D et al (2016) Gut microbiota in the pharmacokinetics and colonic deglycosylation metabolism of ginsenoside Rb1 in rats: contrary effects of antimicrobials treatment and restraint stress. Chem Biol Interact 258:187–196. https://doi.org/10.1016/j.cbi.2016.09.005
Hong C, Yang P, Li S et al (2018) In vitro/in vivo metabolism of ginsenoside Rg5 in rat using ultra-performance liquid chromatography/quadrupole-time-of-flight mass spectrometry. Molecules 23:2113. https://doi.org/10.3390/molecules23092113
Hu Q, Hong H, Zhang Z et al (2023) Methods on improvements of the poor oral bioavailability of ginsenosides: pre-processing, structural modification, drug combination, and micro- or nano- delivery system. J Ginseng Res 47:694–705. https://doi.org/10.1016/j.jgr.2023.07.005
Choi I-D, Ryu J-H, Lee D-E et al (2016) Enhanced absorption study of ginsenoside compound K (20-O-β-(D-Glucopyranosyl)-20(S)-protopanaxadiol) after oral administration of fermented red ginseng extract (HYFRG™) in Healthy Korean Volunteers and Rats. Evid Based Complement Alternat Med 2016:3908142. https://doi.org/10.1155/2016/3908142
Hu Q-R, Lai P-W, Chen F et al (2022) Whole mulberry leaves as a promising functional food: from the alteration of phenolic compounds during spray drying and in vitro digestion. J Food Sci 87:1230–1243. https://doi.org/10.1111/1750-3841.16015
Zhang B, Ye H, Zhu X-M et al (2014) Esterification enhanced intestinal absorption of ginsenoside Rh2 in Caco-2 cells without impacts on its protective effects against H2O2-induced cell injury in human umbilical vein endothelial cells (HUVECs). J Agric Food Chem 62:2096–2103. https://doi.org/10.1021/jf404738s
Zhang B, Zhu X-M, Hu J-N et al (2012) Absorption mechanism of ginsenoside compound K and its butyl and octyl ester prodrugs in Caco-2 cells. J Agric Food Chem 60:10278–10284. https://doi.org/10.1021/jf303160y
Zhang X, Chen S, Duan F et al (2021) Prebiotics enhance the biotransformation and bioavailability of ginsenosides in rats by modulating gut microbiota. J Ginseng Res 45:334–343. https://doi.org/10.1016/j.jgr.2020.08.001
Zheng D, Chu Y, Li S et al (2022) Enhancing effect of borneol on pharmacokinetics of ginsenoside Rb1, ginsenoside Rg1, and notoginsenoside R1 in healthy volunteers after oral administration of compound Danshen dropping pills. Biomed Chromatogr 36:e5311. https://doi.org/10.1002/bmc.5311
Yang F, Zhou J, Hu X et al (2017) Preparation and evaluation of self-microemulsions for improved bioavailability of ginsenoside-Rh1 and Rh2. Drug Deliv Transl Res 7:731–737. https://doi.org/10.1007/s13346-017-0402-7
Jin S, Lee CH, Lim DY et al (2021) Improved hygroscopicity and bioavailability of solid dispersion of red ginseng extract with silicon dioxide. Pharmaceutics 13:1022. https://doi.org/10.3390/pharmaceutics13071022
Gao Y, Wang T, Wang G et al (2019) Preclinical safety of ginsenoside compound K: acute, and 26-week oral toxicity studies in mice and rats. Food Chem Toxicol 131:110578. https://doi.org/10.1016/j.fct.2019.110578
Jeong M-K, Cho C-K, Yoo H-S (2016) General and genetic toxicology of enzyme-treated ginseng extract: toxicology of ginseng Rh2. J Pharmacopuncture 19:213–224. https://doi.org/10.3831/KPI.2016.19.022
Gao YL, Liu ZF, Li CM et al (2011) Subchronic toxicity studies with ginsenoside compound K delivered to dogs via intravenous administration. Food Chem Toxicol 49:1857–1862. https://doi.org/10.1016/j.fct.2011.05.003
Acknowledgements
The authors would like to thank Dr. Wang for her guidance through each stage of the process. I am grateful for the support and help from my research partners. We would like to thank the anonymous reviewers for their helpful remarks. We thank the associate editor and the reviewers for their useful feedback that improved this paper.
Funding
This work was supported by the Key R&D Program of Jilin Provincial Department of Science and Technology (20210204040YY).
Author information
Authors and Affiliations
Contributions
PT: investigation and writing-original draft; SL: editing; JZ: editing; ZA: validation; YH: investigation; LC: software; HZ: software; XL: validation; YW: validation; BN: supervision; YW: writing-review, editing and funding acquisition.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This article does not contain any research involving humans or animals. Ethical approval does not apply to this article.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tang, P., Liu, S., Zhang, J. et al. Ginsenosides as dietary supplements with immunomodulatory effects: a review. Appl Biol Chem 67, 27 (2024). https://doi.org/10.1186/s13765-024-00881-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13765-024-00881-y