Abstract
Natural killer (NK) cell belongs to innate lymphoid cell family that contributes to host immunosurveillance and defense without pre-immunization. Emerging studies have sought to understand the underlying mechanism behind NK cell dysfunction in tumor environments, and provide numerous novel therapeutic targets for tumor treatment. Strategies to enhance functional activities of NK cell have exhibited promising efficacy and favorable tolerance in clinical treatment of tumor patients, such as immune checkpoint blockade (ICB), chimeric antigen receptor NK (CAR-NK) cell, and bi/trispecific killer cell engager (BiKE/TriKE). Immunotherapy targeting NK cell provides remarkable advantages compared to T cell therapy, including a decreased rate of graft versus-host disease (GvHD) and neurotoxicity. Nevertheless, advanced details on how to support the maintenance and function of NK cell to obtain better response rate and longer duration still remain to be elucidated. This review systematically summarizes the profound role of NK cells in tumor development, highlights up-to-date advances and current challenges of therapy targeting NK cell in the clinical treatment of hematologic malignancies.
Similar content being viewed by others
Introduction
Recently, a remarkable potential has been demonstrated in immunotherapy for treating tumors, including adoptive cell therapy, CAR, ICB, and bi/trispecific immune cell engagers. Therapeutic strategies targeted immune cells have changed traditional tumor therapeutic regimen, particularly chimeric antigen receptor T (CAR-T) cells that could confer higher specificity and affinity to T cells [1]. Established efficacy profiles of utilizing T cells has led to the emerging impetus to develop T cell-targeted tumor immunotherapy and promoted extensive clinical investigations [2]. However, intolerable toxicities including GvHD and neurotoxicity [3] greatly limit clinical application of T cell therapeutic strategies. Therefore, emerging studies have energized a shift of focus towards clinical utility of different immune cells, especially NK cells.
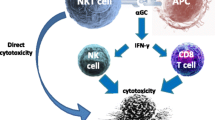
NK cell, identified with absence of surface T cell receptor (TCR) and related cluster of differentiation (CD) 3 molecule, acts as tumor suppressors and contribute to host immune surveillance and defense without pre-immunization [4]. Under healthy conditions, NK cells are damped to protect normal cells from damage due to the interaction between human leukocyte antigen (HLA) of normal nucleated cell and killer cell immunoglobulin-like receptors (KIRs) [5, 6]. NK cells are rapidly activated and then exert cell-killing activity once encounter abnormal cells with decreased expression of HLA molecule, which contribute to the clearance of abnormal cells and the persistence of organism homeostasis [6]. NK cells perform their cytotoxic activity mainly through two ways: I) directly contact with target cells and release perforins and enzymes associated to cell lysis [7]. II) produce immunomodulatory factors including an array of cytokines and chemokines, mainly interferon-γ (IFN-γ), to modulate adaptive immunity and participate in other associated pathways [8, 9].
NK cell immune function is restricted in tumors, which suggests valuable therapeutic targets for tumor treatment. The first application of NK cells in tumor therapy could be traced back to 1985, precleared autologous NK cells were transferred to patients with metastatic cancer and obviously decreased tumor volume (more than 50 percent) [10]. Subsequent strategies for boosting NK cell function including being modified with CAR structures or engagers, and blocking inhibitory receptors with ICB, which attract more and more attention as encouraging anticancer therapeutics. Here, we review biological function and dysfunctional roles of NK cells in hematologic tumors, recent advances and current challenges of NK cell-targeted clinical applications, which might offer novel therapeutic strategies for patients with hematologic malignancies.
The dysfunction of NK cells in hematologic malignancies
Decreased function of NK cells in tumor microenvironment
Abnormal features of receptors on NK cells
Activating, inhibitory and co-stimulatory receptors are needed for NK cell functions, which display obvious abnormalities in tumors. Figure 1 shows classical surface receptors of NK cell. Natural killer group 2 member D (NKG2D) receptor and natural cytotoxicity receptor (NCR) are two prominently stimulatory receptors contributing to NK cell activation [11, 12], decreased expression of them leads to NK cells dysfunction in tumor environment [13]. Previous studies have shown dramatical changes of surface epitopes on tumor cells, such as NKG2D ligand (NKG2DL)-negative could help tumor cells to escape. Increasing NKG2DL levels of tumor cells through genetically or pharmacologically inhibiting poly-ADP-ribose polymerase 1 (PARP1) could suppress leukemogenesis in patient-derived xenotransplant models [14].
General view of surface receptors between NK cell and tumor cell. The anti-tumor functions of NK cell depend on a suite of activating and inhibitory receptors which combined to ligands on tumor cell surface or regulatory cytokines. Dramatical changes of the interaction lead to NK cell dysfunction and then cause tumor escape and progression. Novel agents targeting these special interactions have been explored to augment NK cell-mediated killing effect and recruit them to boost anti-tumor immunity. (1) CD33 CAR molecule; (2) CD-16/IL-15/CD33 TriKE; (3) Anti-CD16/CD19 BiKE; (4) Anti-TIGIT mAb, such as Tiragolumab; (5) Anti-KIR mAb, such as Lirilumab; (6) Anti-PD-1 mAb, such as Pembrolizumab; (7) Anti-NKG2A mAb, such as Monalizumab. BAT-3, HLA-B associated transcript 3; BiKE, bispecific killer cell engager; B7-H6, B7 homolog 6; CAR, chimeric antigen receptor; CD, cluster of differentiation; DAP10, DNAX-activation protein 10; Fas, factor related apoptosis; FcRγ, fragment crystallizable receptor γ; HLA, human leukocyte antigen; ICB, immune checkpoint blockade; IFN-αR, interferon-α receptor; IFN-γ, interferon-γ; IL-R, interleukin receptor; LILRB1, leukocyte immunoglobulin-like receptor B 1; mAb, monoclonal antibody; MICA, human MHC-I chain-related A; MICB, human MHC-I chain-related B; NKG2A, natural killer group 2 member A; NKG2D, natural killer group 2 member D; NKp30, natural killer receptor protein 30; NKp44, natural killer receptor protein 44; NKp46, natural killer receptor protein 46; KIRs, killer cell Ig-like receptors; PD-1, programmed cell death 1; PD-L1, programmed cell death ligand 1; PD-L2, programmed cell death ligand 2; PGDF-DD, platelet derived growth factor DD; TGFβR, transforming growth factor-β receptor; TIGIT, T cell Ig and ITIM domain; TRAIL-R, TNF-related apoptosis inducing ligand-receptor; TriKE, trispecific killer cell engager; ULBPs, ULl6 binding proteins
Published studies have suggested that the impairment of NK cytolytic function derived in part from reduced specific molecules on tumor cell surface. Loss of the mismatched HLA in the genome of the leukemia impaired NK cell-mediated response, representing a vital immune escape mechanism of leukemia relapse after allogeneic hematopoietic cell transplantation [15, 16]. Tumor cells could downregulate the expression of stimulatory ligand through several strategies, including DNA methylation [17], expression pattern alteration of related gene [18, 19] and self-shedding from the cell surface [20]. For example, major histocompatibility complex (MHC)-I chain related protein A (MICA) molecules expressed on malignant cell activated NK cell via binding to NKG2D, while soluble MICA releasing from malignant cell surface impaired NKG2D and facilitated escape of them from immunosurveillance [21, 22]. Inhibition of MICA shedding via antibodies or vaccines were demonstrated to promote anti-tumor immunity of NK cells, providing rationales for exploring novel clinical applications targeting NK cell receptors [23,24,25]. Exosomes, a population of vesicles in biological fluids, were demonstrated to downregulate the expression of NKG2D by inducing its internalization from NK cell surface in microenvironment of leukemia and multiple myeloma (MM) [26,27,28]. Altogether, these findings provide a novel insight that related ligand levels of tumor cells may become a prognostic index, targeting these specific interactions will strengthen the killing effect of NK cells and improve therapeutic outcomes for hematologic malignancies in the future.
Inhibitory receptors on NK cell surface constrain killing capacity of them, which are indispensable for self-tolerance [29]. Natural killer group 2 member A (NKG2A), KIRs family, T cell immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domain (TIGIT) and programmed cell death protein 1 (PD-1) are representative inhibitory receptors. Among them, NKG2A-CD94 complex on NK cell surface transduces inhibitory signals through binding to HLA-E of tumor cells, which rendered the lytic activity of NK cell impaired [13, 30]. Up-regulation of HLA-E was found in some hematologic neoplasms such as chronic lymphocytic leukemia (CLL) and acute myeloid leukemia (AML), indicating a novel strategy to restore cytotoxic ability of NK cell via blocking NKG2A on cell surface [31]. TIGIT expression was demonstrated to be tightly restricted in lymphocytes including T cell subsets and NK cells [32]. Increasing evidence has demonstrated that TIGIT was highly expressed on tumor-infiltrating NK cells in hematological malignancies, such as AML, resulting in tumor progression and poor outcomes [33]. Zhang et al. found that TIGIT expression on tumor-infiltrating NK cells was associated with functional exhaustion of NK cells, and blockade of TIGIT via monoclonal antibodies reversed the exhaustion of anti-tumor immunity [34]. Furthermore, a marked increase level of PD-1 was detected in tumor-infiltrating NK cells of hematologic malignancies [35,36,37,38]. PD-1+ NK cells were proved to have a tendency to exhaust, characterized by reduced proliferative capability and impaired cytotoxicity in tumor microenvironment (TME) [39]. Previous studies focusing on PD-1 and its ligands have found that blockade of the interaction can restore IFN-γ-producing function of NK cells. Besides, soluble programmed cell death ligand 1 (PD-L1) in serum were found to be related to adverse prognosis in lymphoma [40, 41]. Taken together, interactions between inhibitory receptors and the ligands inhibit cytokines release and anti-tumor cytotoxicity of NK cell, which causes immune escape of tumor development. Further detailed research is still needed to explore the intricate network between inhibitory receptors and the ligand in TME of hematologic malignancies.
Disruption of killing pathways in NK cells
Activated NK cells take anti-tumor effect mainly through direct or indirect mode. In direct killing mode, immunological synapses forming between tumor cell and NK cell led to release of lysosomes-like molecules such as granzymes and perforins, the perforation of tumor cell membrane, and the induction caspase-dependent or -independent apoptosis [7, 42]. Tumor initiation and metastasis were suppressed by NK cell released perforins, growth of tumor cells was proved to be inhibited by perforin-dependent cytotoxicity of NK cells in mice [43]. It was confirmed that lacking perforin in NK cells contributed to failure in restraining the metastasis of malignant cells to lung [44]. Indirect way mainly refers to the effect of cytotoxic and regulatory cytokines. Factors secreted by NK cells including cytokines, chemokines (such as chemokine CC-chemokine ligand (CCL) 3, CCL4, CCL5), adenosine, and growth factors, exert functions of regulating innate and adaptive immunoreactions [45]. For example, NK cell could facilitate the maturation of DCs through IFN-γ and tumor necrosis factor (TNF), and the initiation of CD4+ T helper cells in the inflamed lymph node also relied on IFN-γ [46].
Metabolic alterations of TME impair NK cell functions
Metabolic reprogramming has been widely revealed in cancer cells with the appearance of increased glycolysis, lipid synthesis and amino acids catabolism, which not only serves as crucial determinant in signal pathways for sustaining tumorigenesis, but also has profound implication to immunocytes [47, 48]. Immune cells including NK cells have been subsequently found in engagement in metabolic manipulation due to competition for fuels with malignant cells in TME. Depletion of nutrients, aberrant accumulation of toxic metabolites and intermediates in TME influence NK cell proliferation and effector function. Clinical applications of targeting tumor metabolism have emerged and achieved remarkable progresses over the past decades, such as using metabolomics-based biomarker for early diagnosis and therapeutic approaches that aim at metabolic enzymes or metabolites [49, 50].
Glucose deficiency
Glucose is a widely described poor fuel in TME attributing to Warburg effect, a main character of tumor cells that avidly utilize and convert glucose to lactate even oxygen is sufficient [51,52,53]. Decreased concentration of extracellular glucose and following reduced glycolysis and oxidative phosphorylation (OXPHOS) attenuate cytotoxic ability of NK cells, for example, by reducing IFN-γ and Fas ligand levels [54]. In addition, rapid growth of malignant cell consumes abundant glucose and creates a high-lactate microenvironment [55, 56]. Studies pointed out gradual loss of IFN-γ production of NK cells during tumor progress, partly attributing to low pH level and accumulation of lactate in TME. Pathophysiological concentrations of lactate could affect levels of nuclear factor of activated T cell (NFAT) in NK cells, causing diminished IFN-γ production [57]. In lymphoid organs the quantity of NK cell and IFN-γ level could be recovered when systemic alkalified by oral delivery of bicarbonate [58]. Similar to the mechanism of elevated lactate in solid tumor environment, tumor cells of hematologic malignancies take up a large amount of glucose and produce lactate via lactate dehydrogenase A (LDHA) due to genetic changes and tumor hypoxia. Lactic acids accumulate in cells and then are exported through monocarboxylate transporters (MCTs) on cell membrane, contributing to an acidic TME [59]. Indeed, this provides us a novel idea for functional reversal of NK cells, as to control balance of glucose levels via crucial targets such as LDHA and MCTs. Reduction of LDHA function by small interfering RNA (siRNA) or a small-molecule inhibitor FX11 was proved to lead to tumor regression [60]. Selective MCTs inhibitors could decrease intracellular pH and impair the proliferation of malignant cells such as leukemia cells, which were expected to become a promising adjunct in tumor treatment strategy [61,62,63]. AZD3965, an orally bioavailable MCT1 inhibitor, has been currently under phase I clinical trial in patients with advanced tumors including lymphoma [NCT01791595] [64]. These findings indicated that targeting glucose metabolism may be an opportunity for novel treatment strategies in hematologic malignancies.
Aberrant lipid accumulation
Malignant cells increase de novo fatty acid synthesis to provide enough energy for anabolic and signaling pathways, leading more aberrant metabolites accumulation such as short-chain fatty acids, which have been confirmed to skew immunocytes towards immunosuppressive phenotypes [65]. Lipid metabolism associated transcriptional reprogramming of NK cells and abnormality signaling mediated immunosuppressive microenvironment were detected in tumors such as in aggressive B cell lymphoma [66, 67]. Cellular metabolism and effector responses of NK cells are potently suppressed when exposed to fatty acids, which mainly due to a significant rewiring of lipid metabolic pathways [66, 68]. Transcriptional and single cell analysis suggested significant upregulation of lipid and glycerol uptake-related genes expression of NK cells when exposed to lipid-enriched TME, leading to impairment and dysfunction of NK cells [69, 70]. Higher cholesterol concentration is also prone to facilitate the expression of ICBs of immune cells, resulting in lower proliferation and cytotoxicity capacity. Metabolites and varieties of physiological substances of cholesterols also contribute to the immunological landscape. For instance, accumulation of 22-hydroxycholesterol can recruit CD11bhighGr1high neutrophils, an important immunosuppressive population in the TME [71]. Adrenal cortex hormones, transformed from cholesterols, can significantly suppress the proliferation and activity of many immune cells including NK cells [72, 73]. NK cells were found to neutralize toxicity of increased lipid levels in TME through upregulating peroxisome proliferator-activated receptor (PPAR) related signaling pathway to improve synthesis of lipid. Previous studies found that employing a specific agonist Rosiglitazone could stimulate PPAR-γ and thus recovered partial function of NK cells [66, 74]. Besides directly alters metabolic pathways of NK cell, the aberrant accumulation of lipid metabolites also contributes to immunosuppressive phenotypes by acting on immunoregulatory cells in TME such as DC and bone marrow derived suppressor cell (MDSC), which create an immunosuppressive microenvironment and impair NK cell activity [75].
Amino acids starvation and enzyme abnormality
Aberrant profile of amino acids metabolism has been found in diverse tumors. For instance, acute lymphoblastic leukemia (ALL) cells need an exogenous source of asparagine, and exhausting the amino acid from blood has been a prominent component of ALL chemotherapy for decades [76]. Solute carrier family 1 member 1 (SLC1A1), a soluble ectopic transporter on tumor cell membrane increased cellular glutamine uptake. Cell proliferation and tumor growth were both accelerated by this glutamine addiction [77]. When glutamine became deficient or L-amino acid transport was systematically blocked, NK cell growth response was impaired rapidly by regulating c-myc protein levels [78]. Arginine (Arg)-starved NK cells show weak viability, decreased NKp46 and NKp30 levels, and reduced intracellular production of IFN-γ [79]. Researchers proved MDSCs expressed arginase I and AML blasts secreted arginase II, both could specifically agitate M2 phenotypes in surrounding monocytes to inhibit NK cell immune response [80]. In addition, Arginase I can convert Arg to ornithine and then limit the proliferation of NK cells. CB-1158, a potent arginase I inhibitor with high affinity, partially restores NK cell function and blunts AML cell immune escape by inhibiting Arg depletion [81]. One of the obstacles is that few amino acids are only confined to tumor cells, systemic blockades raise the likelihood of toxicity to normal cells thus affect organs such as brain and heart [76]. A more intense knowledge of amino acid utilization in both tumor cell and NK cell is still required to develop tumor therapies targeting amino acid metabolism.
Reactive oxygen species (ROS) cytotoxicity
ROS is generally deemed to by-product of oxygen consumption and cell metabolism formed by the partial reduction of molecular oxygen [82]. ROS is certified to be related to tumor initiation and progression as it activates pro-tumorigenic signaling, drives genetic instability and DNA damage, enhances cell proliferation and survival [83]. Tumor cells produce much more ROS than normal cells which damage killing effect of NK cells. For instance, chronic myelogenous leukemia (CML) cells can motivate nicotinamide adenine dinucleotide phosphate (NADPH) oxidase to generate and then paracrine ROS, contributing to the dysfunction of NK cells [84]. Johan Aurelius et al. discovered an original mechanism of NK cells apoptosis depend on triggered PARP1, demonstrating that oxygen radicals could cause NK cells to undergo apoptosis [85]. Previous clinical trial investigated the effect of histamine dihydrochloride, a NADPH oxidase inhibitor, showed notable improvement of leukemia-free survival and AML relapse prevention [86]. Moreover, studies have confirmed that the levels of ROS and the activity of anti-oxidant enzymes are typically increased in drug resistant tumor cells, indicating ROS may become an attractive target for overcoming chemotherapy resistance. Inhibitors targeting ROS production pathway, such as critical redox-regulating enzymes, show bright prospects in immune recovery of NK cells [87].
Other immunosuppressive factors
Hypoxia in TME
Hypoxia, attributed to insufficient oxygen supply and rapid tumor growth, has been demonstrated to play a vital role in tumor progression and resistance to therapy. Similar to solid tumors, hypoxia condition was reported to be important for tumor neovasculogenesis, metastasis and drug resistance in hematologic malignancies [88, 89]. Published studies have revealed that hypoxia reduced the ability of NK cells to release cytokines, such as granulocyte–macrophage colony stimulating factor (GM-CSF), IFN-γ and TNF-α, and decreased the expression of granzyme B and degranulation marker CD107a, thus facilitated tumor immune escape [90]. Teng et al. found that the dysfunction of NK cells under hypoxic condition may be attributed to the activation of protein tyrosine phosphatase SHP-1. Knocking down SHP-1 or using a specific inhibitor TPI-1 was able to partially restore NK cell cytotoxicity under hypoxia [91]. These findings pointed out targeted inhibitors of hypoxia-activated molecules might provide promising therapeutic efficacy for patients with specific profile of hypoxia biomarkers.
Chemotactic environment abnormality
NK cells develop from bone marrow parenchyma and traffic into various tissues to perform specific functions [92]. Previous studies have noted that chemotactic components abnormality in TME could disturb the recruiting and function of NK cells. Dysregulation of C-X-C chemokine receptor 3 (CXCR3) and CXCR4 chemokine receptor-ligand axis was found to induce defective migration and retention of NK cells in MM [93]. Under the influence of CXCR1 and CXCR2 receptor agonists and other chemotactic factors produced by tumors, neutrophils and MDSCs extruded neutrophil extracellular traps, which wrapped tumor cells and shield them from cytotoxicity mediated by NK cells [94]. Beyond the impact of NK cell trafficking, complex receptor-ligand mode in TME also leads to downregulation of cytotoxicity [95]. For example, IFN-γ secretion of NK cells could be activated through the CXCL10/CXCR3 axis when interferon regulatory factor 1 increased [96]. Hence, altering the expression levels of chemotactic factors in TME will help enhance the infiltration and activation of NK cells, possible further strengthen the therapeutic effect of NK cells.
Tumor-secreted immunosuppressive factors
A variety of immunosuppressive factors containing anti-inflammatory cytokines and specific enzymes have been elucidated to play a role in the immune escape of tumor cells in recent studies [17]. In many hematologic malignancies such as AML and CLL, anti-inflammatory cytokines including IL-4, IL-10, and TGF-β produced by tumor cells could render them less immunogenic, thus caused immune escape [97, 98]. Interestingly, Wang et al. found that effector function of bone marrow-derived NK cells in AML patients were impaired by higher levels of TGF-β1 in TME. Galunisertib, TGF-β1 pathway inhibitor, could significantly restore the cytotoxicity and anti-tumor activity of NK cells, providing a potential therapeutic method to improve outcomes in AML patients [99]. Besides, there were hypothetical mechanism that the suppression of proinflammatory growth factors such as granulocyte colony-stimulating factor (G-CSF) and IL-1β also played a role in immune escape [15]. Some immunomodulatory enzymes and metabolites of catalytic reaction were found to be associated with immunosuppressive TME, further impaired NK cell function. Indoleamine 2,3-dioxygenase (IDO) expression was reported in both bone marrow and peripheral blood AML blasts, displayed anti-tumor effect by inducing Treg cells and impairing IFN-γ production of T and NK cells [100, 101]. These results highlighted that the measurement of such specific enzymes may offer utility as prospective prognostic markers, and targeted inhibitors may hold promise for the treatment of tumors.
Targeting NK cells in hematologic malignancies
Flourishing immunotherapy has become the fourth tumor treatment option after chemotherapy, radiotherapy and surgery. With the development of T cell-based immunotherapy including CAR-T, non-specific immunity has also gained attention with better efficacy and fewer side effects. Here follows NK cell-based immunotherapies being gradually explored for hematologic malignancies, of which general view is recapitulated in Fig. 2.
General view of NK cell-based immunotherapies. (1) A number of NK cell sources were explored for infusion in adoptive NK cell therapy, including autologous NK cell from patients themselves, peripheral blood or umbilical cord blood and placenta-derived NK cell from healthy donors, and clonal NK cell lines such as NK-92, NK-YS, KHYG-1. (2) Strategies targeting to enhance anti-tumor activity of NK cell including employing CAR structures, using immune checkpoint blockades to block inhibitory receptors on NK cell surfaces, augmenting NK cells by cytokines, applying BiKEs and TriKEs, and inducing memory-like NK cells. (3) Biologically active agents or the “activated” NK cells were then infused to patients, causing lysis of tumor cells and further improving the clinical outcome. Ag, antigen; BiKE, bispecific killer cell engager; CAR, chimeric antigen receptor; CD, cluster of differentiation; IL, interleukin; ICB, immune checkpoint blockade; ML-NKs, memory-like natural killer cells; NKs, natural killer cells; PB, peripheral blood; TriKE, trispecific killer cell engager; UCB, umbilical cord blood
The source of NK cells for adoptive immunotherapy
Adoptive infusion of NK cells has overcome uncontrolled acute GvHD reaction, the principal barrier of adoptive T cell therapy [102]. The first exploited sources for adoptive NK cell therapy were autologous NK cell as early as 1985. Metastatic cancer patients who had failed in standard therapy were treated with 1.8 to 18.4 × 1010 autologous NK cells, observing objective regression (more than 50 percent of tumor volume) in 11 of the 25 patients [10]. Hareth Nahi et al. demonstrated the feasibility of infusing autologous NK cells in MM patients [103]. Another phase II clinical trial of adoptive transfer of haploidentical NK cells found no decrease of the cumulative incidence of relapse and no improvement of overall survival (OS) in AML patients, which mainly attributed to the limited persistence of alloreactive donor NK cells [104]. Further research discovered that using activating factors such as IL-2 could assist augmentation of NK therapeutic efficacy. However, IL-2 also added toxicity and complication including elevation of creatinine and bilirubin levels, oliguria, hypotension at the same time [105, 106]. Human umbilical cord blood (UCB) and placenta are rich sources for cytotoxic CD56+ NK cell which has high lytic capabilities. It is estimated that around 30% of lymphoid populations in UCB are NK cells, which tend to be younger and have a stronger proliferation potential [107]. Harry Dolstra et al. evaluated the safety and functional effect of NK-cell product derived from HLA partly matched UCB. These NK cells were demonstrated to be well tolerated, and 2 of 4 AML patients became minimal residual disease (MRD) negative in bone marrow after adoptive infusion [108], indicating that immunotherapy based on UCB-derived NK cells has remarkable therapeutic potential. Subsequently, strategies targeting NK cells modification to obtain durable anti-tumor ability experienced great advances. Pluripotent stem cell-derived NK cells engineered with key surface molecules such as high-affinity noncleavable variant of CD16a were demonstrated to improve antibody-dependent cellular cytotoxicity (ADCC) properties of NK cells and contribute to tumor regression in B-cell lymphoma xenograft studies [109, 110]. Clonal NK cell lines containing NK-YS, KHYG-1, NK-92, has become alternative sources for adoptive NK cell therapy [111,112,113]. Due to potentially broad applicability against tumors and little risk potential for GvHD complications, NK-92 cell line has become a popular agent in thriving clinic trials [114, 115]. However, application of clonal NK cell lines still faces challenges. For instance, irradiation is required before cell infusion to prevent further hyper-proliferation, which in turn drastically limits cell persistence after infusion [116].
Chimeric antigen receptor NK cell therapy (CAR-NK)
Clinical achievements and current shortcomings in CAR-T cell therapies consisting neurotoxicity and cytokines release syndrome (CRS) force the improvement of alternative approaches. CAR-NK cells refer to engineered genetically to express specific CAR structures which mainly have three domains: I) extracellular region, containing a single-chain variable fragment (scFv), generally derives from antibodies that recognize surface antigens of tumor cells. II) transmembrane region, anchors CAR to NK cell membrane. III) cytoplasmic domain, transmits activating signals then causes downstream processes and facilitates the killing effects [117,118,119]. Key components of CAR are shown in Fig. 3. NK cells distinct biology allows them to offer alternative, and perhaps even superior immunotherapeutic strategy in comparison with CAR-T cell therapy. First, CAR-NK cells have reduced risk of GvHD due to a non-HLA-restricted modality [120]. Restricted lifespan of CAR-NK cells in circulation allows no requirement for suicide vectors to prevent excessive expansion [121]. Activated NK cells release GM-CSF and IFN-γ, rather than proinflammatory factors consisting IL-1 and IL-6, implying less likely to occur CRS and neurotoxicity and preferable safety profile [120, 122]. Besides, CAR-NK cells exert more killing modes containing executing cell degranulation, activating apoptotic pathways, and mediating ADCC effects [123]. Cancer-initiating cells (CICs) which play a vital part in tumor recurrence are often characterized by resistant to drugs and irradiation therapy. It has been found that CICs were highly sensitive to NK cells, confirming therapeutic CAR-NK cells could become a strategy for recognition and clearance of CICs and thus prevent tumor recurrence [124]. NK cells have been identified with memory-like function in previous studies, which could allow a more rapid and robust response [125]. Moreover, CAR-NK cells also protect against pathogens such as bacteria and virus, helping to prevent concurrent and secondary infections, which plays an essential role in immunocompromised state in cancer patients.
Components and structures of mAb, CAR, BiKE and TriKE. A Taking anti-CD16 antibody for example, it can be divided into several components including Fab, Fab’, scFv and Fc. B CAR contains an antigen recognition domain, a transmembrane domain and a signal domain providing activating signal to NK cell. As above figure shows, extracellular scFv domain of a CD33 CAR molecule is composed of VH and VL anchored to the transmembrane domain by a flexible hinge, and intracellular part includes two signal domains. C A BiKE consists of two scFvs, and a short flexible polypeptide linker joins to prevent dissociation. Take CD16/CD33 BiKE for example, it constructs from VH and VL of anti-CD16 and anti-CD33 antibodies which make it capable of binding both tumor cells and NK cells. AFM is a bispecific, tetravalent chimeric antibody construct that specifically recruits NK cells by two binding sites exclusively for each antigen. D Compared to BiKE, CD16/IL-15/CD33 TriKE adds a novel modified human IL-15 crosslinker which can assist in improvement of NK cell cytotoxicity. TriKE can be also designed with a scFv fragment of anti-CD16 mAb and two scFvs of tumor specific antigens. BiKE, bispecific killer cell engager; CAR, chimeric antigen receptor; CD, cluster of differentiation; Fab, fragment of antigen binding; IL-15, interleukin 15; CH, constant heavy chain; CL, constant light chain; mAb, monoclonal antibody; scFv, single-chain variable fragment; VH, variable heavy chain; VL, variable light chain; TriKE, trispecific killer cell engage
CAR-NK cell therapies have revealed preliminary potential in a large number of animal experiments [126,127,128], which laid a sufficient foundation for human studies. For example, arming cytokine-induced NK cells with a neoepitope-specific CAR significantly enhanced their anti-tumor responses and avoided off-target toxicity in AML models [129]. 30 CAR-NK cell related clinical studies for hematologic malignancies were retrieved on https://beta.clinicaltrials.gov [till Feb. 2023]. Most of them are in early-stage aiming to determine the safety and initial efficacy. In a phase I and II clinical trial performed to assess the safety, relative efficacy and overall response rate (ORR), HLA-mismatched cord blood derived anti-CD19 CAR-NK cells were infused to 11 enrolled patients with relapsed/refractory (R/R) CD19+ tumors. One of three dose-regimes (1 × 105, 1 × 106, or 1 × 107 cells per kilogram of body weight) of CAR-NK cells were administered after chemotherapies. GvHD, CRS and neurotoxicity were not found after infusion and therapeutic evaluation result was encouraging. Among them, 8 achieved a response including 7 (3 with CLL and 4 with lymphoma) achieved complete response (CR) [NCT03056339] [130]. The shortcoming of this trial was that different therapeutic interventions were received before and after adoptive infusion of CAR-NK cells, exact conclusions regarding the efficacy cannot be drawn. Nkarta, a clinical-stage biotechnology company, announced positive preliminary results of NKX101 and NKX019 in Apr 2022. NKX101, engineered to target NKG2D ligands on cancer cells, showed striking early single-agent activity and no dose-limiting toxicities in R/R AML or myelodysplastic syndromes (MDS) patient populations [NCT04623944]. NKX019 is another leader CAR product engineered to target B-cell antigen CD19. Evaluating NKX019 in B cell malignancies found 3 of 6 patients treated with higher dose level of three-dose regimens achieved 50% CR. It was also proved with satisfying tolerance, the most frequent higher-grade adverse events (AEs) were myelosuppression [NCT05020678]. Although therapeutic potential and clinical outcomes may materially change as patient enrollment continues, progression of these candidates is worthy expecting. Details of other current clinical trials about CAR-NK cell therapy in hematologic tumors are concluded in Table 1.
Further researches are still needed to conquer existing barriers of CAR-NK cell therapy: I) choose more suitable CAR structures, optimize the distance between epitopes and NK cell surface to enhance their effect [131, 132]. II) seek efficient gene transfer approaches. Traditional method for T cells by viral transfection resulted transgene expression of NK cells in low levels and damped their survival [119, 132]. A variety of small molecular compounds have been employed to reduce the repulsion of NK cells to foreign viral particles via charging cells or colocalizing viruses and cells in close proximity [120, 133]. Novel non-viral methods such as electroporation have been also proved to increase transfection efficiency [119]. III) exogenous cytokines are indispensable for survival and proliferation of infused NK cells, while these cytokines cause undesirable AEs like cross stimulating other subpopulation of immunocytes consisting regulatory T cells, which lead immunosuppressive environment for NK cells [134]. Pharmacological interventions, designed CARs targeting NKG2DL-expressing MDSCs and strategies to disrupt TGF-β signaling show the potential to preserve NK cell therapy efficacy [135, 136].
NK cell-based immune checkpoint blockade
Immune checkpoint receptors anchored on cell surface could mediate the delivery of either inhibitory or activating signals, the balance of which decides if NK cells remain in a quiescent state or kill target cells [40, 137]. Targeting these immune checkpoint receptors has exploited a prospective therapeutic strategy for hematologic tumors. ICB serves the role of reactivating anti-tumor immunoreaction through blocking inhibitory molecules on the surfaces of tumor-infiltrating lymphocytes [138]. Marketing approved and well-studied ICBs of NK cells in recent years were concluded in Table 2.
Targeting PD-1 and PD-L1 mAbs are one of the first research hotspots entering people’s vision, which have been observed to treat both hematologic and solid tumors [139, 140]. Genetic analyses identified that RS cells of Hodgkin Lymphoma (HL) exhibited frequent amplification of 9p24.1, leading to overexpression of correlative gene products PD-L1 and PD-L2. The amplification also increased JAK/STAT pathway in turn by acting on JAK2 locus and further drove PD-L1 expression [140]. PD-L1 overexpression of malignant cells lays the groundwork for strengthening the anti-tumor functions of NK cell via blocking PD-1/PD-L1. Pembrolizumab is a humanized IgG4 PD-1 mAb with high-affinity. Philippe Armand et al. reported Pembrolizumab treatment in 31 HL patients, showing only 5 grade 3 drug-related AEs. CR rate was 16% (5/31) and partial response (PR) rate was 48% (15/31), most responses sustained at least 24 weeks with a median follow-up of 17 months [NCT01953692] [141]. The results identified considerable therapeutic outcome on account of blocking inhibitory immune checkpoints. Moreover, application of PD-1 blockades has broken new ground for advanced R/R tumors. Patients with advanced Sezary syndrome (SS) and mycosis fungoides (MF) suffer worse disease progress and poor OS. One phase II trial found 38% (9/24) ORR including 2 CR and 7 PR among 24 enrolled patients with advanced SS or MF in Pembrolizumab treatment regime of 2 mg/kg every 3 weeks [142]. Pembrolizumab also delineated satisfactory therapeutic effect in other hematologic malignancies such as MM and lymphoma [143, 144].
As above mentioned, KIRs are generally expressed on NK cells to preclude normal cells from damaging. Early study found that KIR epitope incompatible transplants could achieve higher engraftment rates [145]. Lacking of interaction between KIR-MHC I was concluded to trigger NK cell activity, suggesting that specifically blocking the recognition and binding between them could rejuvenate NK cells [146]. Relevant clinical trials are booming, early safety evaluation test of anti-KIRs ICBs draw desirable results but the efficacy tests were inconsistent [147,148,149]. And addition of KIR blockade improved meaninglessly in the efficacy over single agent PD-1 blockade in some clinical studies [150]. Heterogeneous results may approximately due to that study populations were too small to overcome the biological heterogeneity within and across disease types. Thus, additional benefits accruing from the combination regimens still require longer follow-up time to assess.
Application of ICBs and the resultant breakthrough strategy of taking advantage of immune system for tumor therapy have displayed profound superiorities. However, there are still varieties of challenges need to be addressed. The major barrier is drug-resistant, either lacking of initial response to treatment or with initial promising response but developed resistance during therapeutic stage [151]. Published studies have revealed the minimal expression of PD-1 on NK cells in several tumors, which may lead to primary drug-resistant to ICBs [152]. Strategic approaches such as the combination of immune checkpoint treatments with other therapies including angiogenesis inhibitors and oncolytic viruses have been demonstrated to improve the responses to ICBs [153]. A complex of checks and balances were observed in human immune system that afford response or preserve tolerance. ICBs have the capacity for this homeostatic balance perturbation, causing immune related AEs (irAEs). IrAEs refer to inflammatory adverse events due to non-specific stimulation of immune system by ICBs, generally involving endocrine glands, skin, gastrointestinal tract [154]. IrAEs have been described in many clinical trials including nausea, vomiting, diarrhea, bilirubin increase, rash et al. [NCT01822509] [155]. Besides acute clinical toxicities of these agents, chronic irAEs (usually refer to > 12 weeks sustaining after ICBs discontinuation) are more prevalent [156]. Long-term potential chronic toxicity may be ignored because clinical studies tend to pay attention to the most frequent treatment-associated adverse effects. A generally limited life expectancy for patients with metastatic tumors constrains long follow-up time to exhibit chronic irAEs. Endocrinopathies and rheumatological toxicities has become the most frequent chronic irAEs, and pneumonitis, neuropathy, dermatitis et al. are relatively low-prevalence events [157]. The onset of irAEs varies widely and is hard to predict. Terminating ICBs therapy and beginning high-dose corticosteroids treatment are most commonly used for irAEs control. But there still remains drawbacks including irAEs-overlapped drug toxicities, serious infections, and the risk of suppressing tumor immunosurveillance [158]. Deeper exploration of intrinsic and extrinsic factors that impact ICB response and standard managements built on these hallmarks are intensively needed.
Cytokine-induced NK cell therapy
Cytokines appear to be critical in many aspects including regulating innate or adaptive immunity, cytogenesis, cell growth, as well as damaged tissue repairment [159]. Earlier results have shown cytokines such as IL-2 could promote the regression of solid tumor models established in animals [160, 161], providing novel insights for augmenting anti-tumor effects of immunocytes containing NK cell by cytokines. Table 3 showed recent applications of cytokine-induced NK cells for treatment of hematological malignancies.
Interleukins
Several interleukin immunotherapies have been permitted by the United States Food and Drug Administration (FDA) such as IL-2 for the treatment of metastatic neoplasms. IL-2 used directly for improving anti-tumor response of NK cell can trace back to 1985, finding that administrating recombinant IL-2 assisted generation of activated lymphokine killer cells [162]. However, there are contradictions between safety and efficacy of IL-2. Low dose can stimulate NK cells expansion, but limited anti-tumor efficacy [163], while high doses enough for efficient anti-tumor response may lead to severe side effects like capillary leak syndrome [164, 165]. IL-2 also assisted to generate and maintain Treg cells to inhibit NK cells via TGF-β and down-regulating surface NKG2D receptors of NK cell [166, 167]. IL-15 was subsequently found to play a critical role in NK cell stimulation with no Treg-mediated immunosuppression. ALT-803 was a super-agonist complex of IL-15, which was evaluated in hematologic malignancies patients relapsed over 2 months, showing well tolerance and remarkable efficacy [168]. IL‐21, with the function of promoting the differentiation and proliferation, increasing IFN-γ production and cytotoxicity of NK cells, is also in exploring process of NK cell-based therapy [169]. A phase I study enrolled 21 patients with B cell malignancies was performed to evaluate the safety, maximum-tolerated dose (MTD) and efficacy of rIL-21 combined with Rituximab, finding toxicities including flu-like symptoms, fatigue, and headache. The MTD was 100 μg/kg and 8 of 19 evaluable patients showed clinical responses after Rituximab-based treatment [170]. This preliminarily confirmed the value of interleukins-based combination treatment regimen.
Interferon
Interferons (IFN) are one of the first cytokines to be discovered and have been used therapeutically for decades. The recombinant human IFNs has been approved for treating several tumors such as CML [171], and gradually appeared to be a vital component of combination anti-tumor treatment. Type I IFNs could activate IFN-γ generated of NK cell when combined with IL-12 [172]. Moreover, IFN has proved to be a potential candidate for boosting efficacy of tyrosine kinase inhibitor (TKI) treatment. Mechanism can be concluded that application of TKIs inhibited the degradation of IFN-α receptor on tumor cells, thus increased induction of pro-apoptotic genes and proteins [173, 174]. Combination therapy of IFN-α and Dasatinib in 40 newly diagnosed CML patients demonstrated a steep increase in acceptable tolerability and response rates compared to using Dasatinib only [174]. Engineered interferons in combined treatment regimen have shown promising therapeutic effect in leukemia and lymphoma [174,175,176], supporting further exploration for potential therapeutic value of IFN.
NK cell engagers
Bi- and tri-specific antibodies are designed to build efficient immunological synapses between immune cells and malignant cells, specifically recruiting immune cells and forming more densely interconnected to tumor cells. Bispecific antibodies targeting CD3 and specific tumor epitopes to recruit T cells developed rapidly over the past decades. Blinatumomab is one FDA approved CD3/CD19 bispecific T cell engager (BiTE) in Dec. 2014 for adult leukemia. Both CAR T cell therapy and BiTE applications are limited by severe toxicities [177], leading partial study focus more and more turn to NK cell engagers. BiKEs or TrikEs are formed by single variable heavy (VH) and light chain (VL) of certain antibody, of which a flexible polypeptide linker joined to keep from dissociating [178]. Structures of BiKEs or TrikEs are visualized in Fig. 3. Current NK cell engagers are mainly designed with CD16 and tumor epitopes like CD33 simultaneously, which have several additional advantages compared to mAbs. They are non-immunogenic so that could alleviate many complications of their CAR counterparts [179]. Size of NK cell engagers are small, mainly among 50–80 kDa, which allows efficient tumor penetration and increased biodistribution of the agents. Small size of these fragments allows rapidly elimination through kidneys, contributing to maintain appropriate serum concentration levels and limit associated toxicities [180].
BiKE
The engagers targeting CD16 have been chosen in the first generation to trigger NK cell cytotoxicity [181], cooperated with the recognition of different epitopes of tumor cell surface including CD33 or CD33/CD123 on AML cells [182, 183], CD33 on MDS cells [184], CD30 on HL cells [185, 186], CD19/CD20 or HLA-II on B cell lymphomas cells [187, 188]. Dual targeting molecules stand out to recruit NK cells to malignant cells with superior specificity and stronger lysis than traditional mono targeting agents, which extremely attracts further clinical development.
Early back to 1997, F Hartmann et al. had reported a phase I/II clinical research for 15 refractory HL patients with HRS-3/A9, a CD16/CD30 BiKE, finding no explicit dose-side effect till the highest dose administered with 64 mg/m2 [185]. AFM13 is a tetravalent chimeric antibody structure that designed to specifically recruit NK cells by combining to CD16A with two binding sites for each epitope but without Fc domain. A dose-escalation trial of AFM13 with administration doses from 0.01 to 7 mg per kilogram of body weight only found mild to medium AEs like headache, nausea, nasopharyngitis, fever, chills and infusion reaction [NCT01221571] [189]. Addition of AFM13 to Pembrolizumab regime in R/R HL patients showed generally well tolerance, and 88% (21/24) ORR at the highest treatment dose [NCT02665650] [190]. Latest research demonstrated that UCB-derived NK cells loaded with AFM13 opening up promising prospects for treatment of RR CD30+ lymphoma patients [191]. Clinical trials about AFM13 in patients with other hematologic tumors like T cell lymphoma are in progress [NCT03192202, NCT04074746, NCT04101331].
The platform of BiKE designing is flexible, which enables varieties of alterative components to be assembled. Adding components to BiKE such as scFvs against KIRs, TIGIT, NKG2A and PD-1 receptors provides ability to circumvent inhibitory immune checkpoints therefore drives NK cell associated anti-tumor reactions. Addition of a scFv fragment of TGF-β blocking has also been proved to decrease negative signals in TME [192]. The function of engineered bi-specific antibody combining an anti-CS1 (tumor-specific antigen on MM cells) scFv and an anti-NKG2D scFv was tested in a MM mouse model. The result revealed intensive immune synapse formed between NKG2D+ effector cells and CS1+ MM cells, promoting NK cells to improve clearance of tumor cells [193].
TriKE
Cytokines with activating role such as IL-15, have been cooperated into NK cell engagers to further increase cytotoxicity. When compared with CD16 and CD33 BiKE, addition of IL-15 crosslinker induced superior cytotoxicity, degranulation, and cytokines release of NK cells. It was confirmed that in the immunodeficient mouse model where CD16/IL-15/CD33 TriKE induced maintain and survival of NK cells and exhibited superior anti-tumor effect [194]. C-type lectin domain family 12 member A (CLEC12A) is a specific epitope of AML cells. CD16/IL-15/CLEC12A TriKE was proved to specifically boost proliferation and enhance stimulation of NK cells in vitro experiments. In addition, off-target toxicities were minimized due to absence of CLEC12A on normal cells [195]. Laurent Gauthier et.al reported the generation of tri-functional engagers based on NKp46 and CD16, two activating receptors on NK cell surface, and a tumor-specific surface epitope. This TriKE was more potent in vitro and had similar pharmacokinetics to full IgG antibodies in vivo. It had no off-target effect and effectively inhibited tumor development in the mouse model [196]. They further explored the efficacy of a TriKE targeting NKp46, CD16a on NK cells and CD123 on AML blasts, finding that it had prolonged anti-tumor pharmacodynamic effects and very low inflammatory cytokine induction [197].
NK cell engagers have shown highly efficient anti-tumor functions in vitro and preclinical experiments. It has also provided profound preliminary results that the engagers are safe due to their low possibility of non-specific cytokine release, and their activation only occurs with the presence of tumor cells [198]. However, challenges still remain in this field. Chronic stimulation of NK engager therapies may cause NK cell exhaustion, plausible injection protocols need attempt to limit constant NK cell activation [198]. Antigen-low or -negative malignant cells appear to emerge after killer engagers therapy which could contribute to tumor escape and disease relapse. Thus, additional approaches are required containing combining different engagers and increasing response at lower antigen levels [195]. BiKEs and TriKEs have significant potential for clinical applications with these improved functional characteristics, further explorations are still needed to endow NK cells with superior anti-tumor activities.
Memory-like NK (ML NK) cells
It was previously believed innate immunocytes consisting NK cells lack antigen-specificity and immunologic memory because their receptor genes cannot undergo somatic rearrangements. However, “ML NK cells” were subsequently observed in mice, NK cells possessing expression of Ly49H receptors had ability to drive the expansion during infectious phase. Expanded effector NK cells then established a pool of long-lived antigen-specific cells with a unique transcriptional signature [199, 200]. NK cells pre-activated through cytokines and then adoptive transferred into vivo showed enhanced proliferation and exhibited restimulation responses to cytokines [201]. Effector function and persistence of syngeneic IL-preactivated NK cells were observed, which also markedly reduced the growth of established mouse tumors [202]. A phase I study observed 5 clinical responses of 9 evaluable AML patients adoptively transferred ML NK cells, demonstrating robust responses of these immunocytes to leukemia cells [203]. An innovative proposal to enhance tumor-specific recognition of ML NK cells by modifying with CARs was come up to increase IFN-γ generation, degranulation and cytotoxicity of NK cells. For instance, ML NK cells derived from lymphoma patients engineered with anti-CD19 CAR reduced lymphoma burden and thus obtained survival improvement in human xenograft models [204]. Han Dong et al. found that arming ML NK cells with a neoepitope-specific CAR significantly enhanced anti-tumor response and avoided off-target toxicity in AML, suggesting that ML NK cells represented a promising cellular platform for modified adoptive cell therapy [129]. CAR-ML NK cells offer apparent advantages including inducing response to NK cell-resistant tumor targets through an obvious synergistic cooperation of CAR-mediated effects and “memory”, representing a powerful tumor immunotherapy approach.
Conclusions
The roles of NK cell in hematologic malignancies have been revealed in emerging studies, providing scientific basis for novel approaches of immunotherapy. Approaches targeting to combat immunosuppression of NK cells in TME including modifying NK cell with CAR structures or specific engagers, activating NK cell via cytokines or ICBs, inducing ML NK cells, are in different phases of clinical trials and some have been permitted to clinical use already. These immunotherapies have performed encouraging results in safety, persistence and efficiency, especially for patients with tumor relapse and metastasis.
Nevertheless, poor or even no response to these innovative therapies is still remained in a relevant percentage of patients due to dropped expressions of tumor antigen after treatment or complicated immunosuppressive components in TME. Additional explorations are constantly needed to strengthen efficacy of immune therapy based on NK cells. For instance, choose purified, active and low-immunogenic NK cell sources for adoptive infusion to endow superior anti-tumor functions and circumvent detrimental AEs. When designing CAR or engager structure on diverse platforms, it is essential to balance details of different components to ensure high specificity and sensitivity. Moreover, efficacy of combination regimen based on NK cells and other wide-used agents expects for evaluation in more studies. In conclusion, immunotherapy targeting NK cell has become a potential armamentarium and will continually add powerful tools to improve the prognosis of intricate patients with hematologic malignancies in the future.
Availability of data and materials
Not applicable.
Abbreviations
- ADCC:
-
Antibody-dependent cell mediated cytotoxicity
- AEs:
-
Adverse events
- ALL:
-
Acute lymphoblastic leukemia
- AML:
-
Acute myeloid leukemia
- Arg:
-
Arginine
- BiKE:
-
Bispecific killer cell engager
- BiTE:
-
Bispecific T cell engager
- CAR-NK cell:
-
Chimeric antigen receptor natural killer cell
- CAR-T cell:
-
Chimeric antigen receptor T cell
- CCL:
-
Chemokine CC-chemokine ligand
- CD:
-
Cluster of differentiation
- CICs:
-
Cancer-initiating cells
- CLEC12A:
-
C-type lectin domain family 12 member A
- CLL:
-
Chronic lymphocytic leukemia
- CML:
-
Chronic myelogenous leukemia
- CR:
-
Complete response
- CRS:
-
Cytokines release syndrome
- CXCR3:
-
C-X-C chemokine receptor 3
- Fc:
-
Fragment crystallizable
- FDA:
-
The United States Food and Drug Administration
- G-CSF:
-
Granulocyte colony-stimulating factor
- GM-CSF:
-
Granulocyte–macrophage colony stimulating factor
- GvHD:
-
Graft versus-host disease
- HLA:
-
Human leukocyte antigen
- ICB:
-
Immune checkpoint blockade
- IDO:
-
Indoleamine 2,3-dioxygenase
- IFN:
-
Interferon
- IFN-γ:
-
Interferon-γ
- irAEs:
-
Immune related adverse events
- KIRs:
-
Killer cell immunoglobulin-like receptors
- LDHA:
-
Lactate dehydrogenase A
- MCTs:
-
Monocarboxylate transporters
- MDS:
-
Myelodysplastic syndromes
- MDSC:
-
Bone marrow derived suppressor cell
- MF:
-
Mycosis fungoides
- MHC:
-
Major histocompatibility complex
- MICA:
-
MHC-I chain related protein A
- ML NK cell:
-
Memory-like NK cell
- MM:
-
Multiple myeloma
- MRD:
-
Minimal residual disease
- MTD:
-
Maximum-tolerated dose
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate
- NCR:
-
Natural cytotoxicity receptor
- NFAT:
-
Nuclear factor of activated T cell
- NK cell:
-
Natural killer cell
- NKG2A:
-
Natural killer group 2 member A
- NKG2D:
-
Natural killer group 2 member D
- NKG2DL:
-
NKG2D ligand
- PARP1:
-
Poly-ADP-ribose polymerase 1
- PD-1:
-
Programmed cell death protein 1
- PD-L1:
-
Programmed cell death ligand 1
- PPAR:
-
Peroxisome proliferator-activated receptor
- PR:
-
Partial response
- ORR:
-
Overall response rate
- OS:
-
Overall survival
- OXPHOS:
-
Oxidative phosphorylation
- ROS:
-
Reactive oxygen species
- R/R:
-
Relapsed/refractory
- scFv:
-
Single-chain variable fragment
- siRNA:
-
Small interfering RNA
- SLC1A1:
-
Solute carrier family 1 member 1
- SS:
-
Sezary syndrome
- TCR:
-
T cell receptor
- TIGIT:
-
T cell immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domain
- TKI:
-
Tyrosine kinase inhibitor
- TME:
-
Tumor microenvironment
- TNF:
-
Tumor necrosis factor
- TriKE:
-
Trispecific killer cell engager
- UCB:
-
Umbilical cord blood
- VH :
-
Variable heavy chain
- VL :
-
Variable light chain
References
June CH, O’Connor RS, Kawalekar OU, Ghassemi S, Milone MC. CAR T cell immunotherapy for human cancer. Science. 2018;359:1361–5.
Wang J, Gu T, Hu Y, Huang H. Novel cellular immunotherapies for hematological malignancies: recent updates from the 2021 ASH annual meeting. Exp Hematol Oncol. 2022;11:61.
Qu C, Zhang H, Cao H, Tang L, Mo H, Liu F, et al. Tumor buster—where will the CAR-T cell therapy ‘missile’ go? Mol Cancer. 2022;21:201.
Vivier E, Artis D, Colonna M, Diefenbach A, Di Santo JP, Eberl G, et al. Innate lymphoid cells: 10 years on. Cell. 2018;174:1054–66.
Yawata M, Yawata N, Draghi M, Little AM, Partheniou F, Parham P. Roles for HLA and KIR polymorphisms in natural killer cell repertoire selection and modulation of effector function. J Exp Med. 2006;203:633–45.
Anfossi N, Andre P, Guia S, Falk CS, Roetynck S, Stewart CA, et al. Human NK cell education by inhibitory receptors for MHC class I. Immunity. 2006;25:331–42.
Orange JS. Formation and function of the lytic NK-cell immunological synapse. Nat Rev Immunol. 2008;8:713–25.
Vivier E, Raulet DH, Moretta A, Caligiuri MA, Zitvogel L, Lanier LL, et al. Innate or adaptive immunity? The example of natural killer cells. Science. 2011;331:44–9.
Roda JM, Parihar R, Magro C, Nuovo GJ, Tridandapani S, Carson WR. Natural killer cells produce T cell-recruiting chemokines in response to antibody-coated tumor cells. Cancer Res. 2006;66:517–26.
Rosenberg SA, Lotze MT, Muul LM, Leitman S, Chang AE, Ettinghausen SE, et al. Observations on the systemic administration of autologous lymphokine-activated killer cells and recombinant interleukin-2 to patients with metastatic cancer. N Engl J Med. 1985;313:1485–92.
Bauer S, Groh V, Wu J, Steinle A, Phillips JH, Lanier LL, et al. Activation of NK cells and T cells by NKG2D, a receptor for stress-inducible MICA. Science. 1999;285:727–9.
Long EO, Burshtyn DN, Clark WP, Peruzzi M, Rajagopalan S, Rojo S, et al. Killer cell inhibitory receptors: diversity, specificity, and function. Immunol Rev. 1997;155:135–44.
Sandoval-Borrego D, Moreno-Lafont MC, Vazquez-Sanchez EA, Gutierrez-Hoya A, Lopez-Santiago R, Montiel-Cervantes LA, et al. Overexpression of CD158 and NKG2A inhibitory receptors and underexpression of NKG2D and NKp46 activating receptors on NK Cells in acute myeloid leukemia. Arch Med Res. 2016;47:55–64.
Paczulla AM, Rothfelder K, Raffel S, Konantz M, Steinbacher J, Wang H, et al. Absence of NKG2D ligands defines leukaemia stem cells and mediates their immune evasion. Nature. 2019;572:254–9.
Zeiser R, Vago L. Mechanisms of immune escape after allogeneic hematopoietic cell transplantation. Blood. 2019;133:1290–7.
Steidl C, Shah SP, Woolcock BW, Rui L, Kawahara M, Farinha P, et al. MHC class II transactivator CIITA is a recurrent gene fusion partner in lymphoid cancers. Nature. 2011;471:377–81.
Baragano RA, Martin-Palanco V, Fernandez AF, Rodriguez RM, Fraga MF, Lopez-Larrea C, et al. Methylation of NKG2D ligands contributes to immune system evasion in acute myeloid leukemia. Genes Immun. 2015;16:71–82.
Szczepanski MJ, Szajnik M, Welsh A, Whiteside TL, Boyiadzis M. Blast-derived microvesicles in sera from patients with acute myeloid leukemia suppress natural killer cell function via membrane-associated transforming growth factor-beta1. Haematologica. 2011;96:1302–9.
Sauer M, Schuldner M, Hoffmann N, Cetintas A, Reiners KS, Shatnyeva O, et al. CBP/p300 acetyltransferases regulate the expression of NKG2D ligands on tumor cells. Oncogene. 2017;36:933–41.
Huergo-Zapico L, Gonzalez-Rodriguez AP, Contesti J, Gonzalez E, Lopez-Soto A, Fernandez-Guizan A, et al. Expression of ERp5 and GRP78 on the membrane of chronic lymphocytic leukemia cells: association with soluble MICA shedding. Cancer Immunol Immunother. 2012;61:1201–10.
Danier AC, de Melo RP, Napimoga MH, Laguna-Abreu MT. The role of natural killer cells in chronic myeloid leukemia. Rev Bras Hematol Hemoter. 2011;33:216–20.
Rebmann V, Schutt P, Brandhorst D, Opalka B, Moritz T, Nowrousian MR, et al. Soluble MICA as an independent prognostic factor for the overall survival and progression-free survival of multiple myeloma patients. Clin Immunol. 2007;123:114–20.
Alves DSP, Xing S, Kotini AG, Papapetrou EP, Song X, Wucherpfennig KW, et al. MICA/B antibody induces macrophage-mediated immunity against acute myeloid leukemia. Blood. 2022;139:205–16.
Ferrari DAL, Tay RE, Pan D, Luoma AM, Ito Y, Badrinath S, et al. Antibody-mediated inhibition of MICA and MICB shedding promotes NK cell-driven tumor immunity. Science. 2018;359:1537–42.
Badrinath S, Dellacherie MO, Li A, Zheng S, Zhang X, Sobral M, et al. A vaccine targeting resistant tumours by dual T cell plus NK cell attack. Nature. 2022;606:992–8.
Clayton A, Mitchell JP, Court J, Linnane S, Mason MD, Tabi Z. Human tumor-derived exosomes down-modulate NKG2D expression. J Immunol. 2008;180:7249–58.
Hong CS, Muller L, Boyiadzis M, Whiteside TL. Isolation and characterization of CD34+ blast-derived exosomes in acute myeloid leukemia. PLoS ONE. 2014;9: e103310.
Moloudizargari M, Redegeld F, Asghari MH, Mosaffa N, Mortaz E. Long-chain polyunsaturated omega-3 fatty acids reduce multiple myeloma exosome-mediated suppression of NK cell cytotoxicity. Daru. 2020;28:647–59.
Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27:450–61.
Liu X, Song J, Zhang H, Liu X, Zuo F, Zhao Y, et al. Immune checkpoint HLA-E:CD94-NKG2A mediates evasion of circulating tumor cells from NK cell surveillance. Cancer Cell. 2023;41:272–87.
McWilliams EM, Mele JM, Cheney C, Timmerman EA, Fiazuddin F, Strattan EJ, et al. Therapeutic CD94/NKG2A blockade improves natural killer cell dysfunction in chronic lymphocytic leukemia. Oncoimmunology. 2016;5: e1226720.
Stanietsky N, Simic H, Arapovic J, Toporik A, Levy O, Novik A, et al. The interaction of TIGIT with PVR and PVRL2 inhibits human NK cell cytotoxicity. Proc Natl Acad Sci USA. 2009;106:17858–63.
Liu G, Zhang Q, Yang J, Li X, Xian L, Li W, et al. Increased TIGIT expressing NK cells with dysfunctional phenotype in AML patients correlated with poor prognosis. Cancer Immunol Immunother. 2022;71:277–87.
Zhang Q, Bi J, Zheng X, Chen Y, Wang H, Wu W, et al. Blockade of the checkpoint receptor TIGIT prevents NK cell exhaustion and elicits potent anti-tumor immunity. Nat Immunol. 2018;19:723–32.
Chen C, Liang C, Wang S, Chio CL, Zhang Y, Zeng C, et al. Expression patterns of immune checkpoints in acute myeloid leukemia. J Hematol Oncol. 2020;13:28.
Korkmaz S, Erdem S, Akay E, Tasdemir EA, Karaman H, Keklik M. Do PD-1 and PD-L2 expressions have prognostic impact in hematologic malignancies? Turk J Med Sci. 2019;49:265–71.
Guan J, Wang R, Hasan S, Tao L, Wazir M, Jain AG, et al. Prognostic significance of the dynamic change of programmed death-ligand 1 expression in patients with multiple myeloma. Cureus. 2019;11: e4401.
Yamamoto R, Nishikori M, Kitawaki T, Sakai T, Hishizawa M, Tashima M, et al. PD-1-PD-1 ligand interaction contributes to immunosuppressive microenvironment of Hodgkin lymphoma. Blood. 2008;111:3220–4.
Pesce S, Greppi M, Tabellini G, Rampinelli F, Parolini S, Olive D, et al. Identification of a subset of human natural killer cells expressing high levels of programmed death 1: a phenotypic and functional characterization. J Allergy Clin Immunol. 2017;139:335–46.
He R, Ding W, Viswanatha DS, Chen D, Shi M, Van Dyke D, et al. PD-1 expression in chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and large B-cell richter transformation (DLBCL-RT): a characteristic feature of DLBCL-RT and potential surrogate marker for clonal relatedness. Am J Surg Pathol. 2018;42:843–54.
Xie M, Huang X, Ye X, Qian W. Prognostic and clinicopathological significance of PD-1/PD-L1 expression in the tumor microenvironment and neoplastic cells for lymphoma. Int Immunopharmacol. 2019;77: 105999.
Prager I, Liesche C, van Ooijen H, Urlaub D, Verron Q, Sandstrom N, et al. NK cells switch from granzyme B to death receptor-mediated cytotoxicity during serial killing. J Exp Med. 2019;216:2113–27.
van den Broek MF, Kagi D, Zinkernagel RM, Hengartner H. Perforin dependence of natural killer cell-mediated tumor control in vivo. Eur J Immunol. 1995;25:3514–6.
Street SE, Cretney E, Smyth MJ. Perforin and interferon-gamma activities independently control tumor initiation, growth, and metastasis. Blood. 2001;97:192–7.
Morandi F, Horenstein AL, Chillemi A, Quarona V, Chiesa S, Imperatori A, et al. CD56brightCD16- NK cells produce adenosine through a CD38-mediated pathway and act as regulatory cells inhibiting autologous CD4+ T cell proliferation. J Immunol. 2015;195:965–72.
Vivier E, Tomasello E, Baratin M, Walzer T, Ugolini S. Functions of natural killer cells. Nat Immunol. 2008;9:503–10.
Tumino N, Nava LC, Tiberti S, Besi F, Martini S, Fiore PF, et al. The tumor microenvironment drives NK cell metabolic dysfunction leading to impaired antitumor activity. Int J Cancer. 2023;152:1698–706.
Yu Z, Zhou X, Wang X. Metabolic reprogramming in hematologic malignancies: advances and clinical perspectives. Cancer Res. 2022;82:2955–63.
Hu F, Wang Y, Wang WD, Gale RP, Wu BY, Liang Y. Improving prediction accuracy in acute myeloid leukaemia: micro-environment, immune and metabolic models. Leukemia. 2021;35:3073–7.
Mondal S, Roy D, Sarkar BS, Jin L, Jung D, Zhang S, et al. Therapeutic targeting of PFKFB3 with a novel glycolytic inhibitor PFK158 promotes lipophagy and chemosensitivity in gynecologic cancers. Int J Cancer. 2019;144:178–89.
Akers LJ, Fang W, Levy AG, Franklin AR, Huang P, Zweidler-McKay PA. Targeting glycolysis in leukemia: a novel inhibitor 3-BrOP in combination with rapamycin. Leuk Res. 2011;35:814–20.
Moreno C. Chronic lymphocytic leukemia and the Warburg effect. Blood. 2015;125:3368–9.
Panchabhai S, Schlam I, Sebastian S, Fonseca R. PKM2 and other key regulators of Warburg effect positively correlate with CD147 (EMMPRIN) gene expression and predict survival in multiple myeloma. Leukemia. 2017;31:991–4.
Wu SY, Fu T, Jiang YZ, Shao ZM. Natural killer cells in cancer biology and therapy. Mol Cancer. 2020;19:120.
De Raes EA, Benoit DD, Depuydt PO, Offner F, Nollet J, Vantilborgh AK, et al. Early recognition of malignant lactic acidosis in clinical practice: report on 6 patients with haematological malignancies. Acta Clin Belg. 2012;67:347–51.
Geng H, Tsang M, Subbaraj L, Cleveland J, Chen L, Lu M, et al. Tumor metabolism and neurocognition in CNS lymphoma. Neuro Oncol. 2021;23:1668–79.
Brand A, Singer K, Koehl GE, Kolitzus M, Schoenhammer G, Thiel A, et al. LDHA-Associated Lactic Acid Production Blunts Tumor Immunosurveillance by T and NK Cells. Cell Metab. 2016;24:657–71.
Potzl J, Roser D, Bankel L, Homberg N, Geishauser A, Brenner CD, et al. Reversal of tumor acidosis by systemic buffering reactivates NK cells to express IFN-gamma and induces NK cell-dependent lymphoma control without other immunotherapies. Int J Cancer. 2017;140:2125–33.
Payen VL, Mina E, Van Hee VF, Porporato PE, Sonveaux P. Monocarboxylate transporters in cancer. Mol Metab. 2020;33:48–66.
Le A, Cooper CR, Gouw AM, Dinavahi R, Maitra A, Deck LM, et al. Inhibition of lactate dehydrogenase A induces oxidative stress and inhibits tumor progression. Proc Natl Acad Sci U S A. 2010;107:2037–42.
Saulle E, Spinello I, Quaranta MT, Pasquini L, Pelosi E, Iorio E, et al. Targeting lactate metabolism by inhibiting MCT1 or MCT4 impairs leukemic cell proliferation, induces two different related death-pathways and increases chemotherapeutic sensitivity of acute myeloid leukemia cells. Front Oncol. 2020;10: 621458.
Intasai N, Pata S, Tragoolpua K, Tayapiwatana C. Recombinant multivalent EMMPRIN extracellular domain induces U937 human leukemia cell apoptosis by downregulation of monocarboxylate transporter 1 and activation of procaspase-9. Appl Biochem Biotechnol. 2015;176:1781–90.
Pivovarova AI, MacGregor GG. Glucose-dependent growth arrest of leukemia cells by MCT1 inhibition: Feeding Warburg’s sweet tooth and blocking acid export as an anticancer strategy. Biomed Pharmacother. 2018;98:173–9.
Halford S, Veal GJ, Wedge SR, Payne GS, Bacon CM, Sloan P, et al. A phase I dose-escalation study of AZD3965, an oral monocarboxylate transporter 1 inhibitor, in patients with advanced cancer. Clin Cancer Res. 2023;29:1429–39.
Cheng C, Geng F, Cheng X, Guo D. Lipid metabolism reprogramming and its potential targets in cancer. Cancer Commun (Lond). 2018;38:27.
Kobayashi T, Lam PY, Jiang H, Bednarska K, Gloury R, Murigneux V, et al. Increased lipid metabolism impairs NK cell function and mediates adaptation to the lymphoma environment. Blood. 2020;136:3004–17.
Wang X, Guo W, Shi X, Chen Y, Yu Y, Du B, et al. S1PR1/S1PR3-YAP signaling and S1P-ALOX15 signaling contribute to an aggressive behavior in obesity-lymphoma. J Exp Clin Cancer Res. 2023;42:3.
Poznanski SM, Singh K, Ritchie TM, Aguiar JA, Fan IY, Portillo AL, et al. Metabolic flexibility determines human NK cell functional fate in the tumor microenvironment. Cell Metab. 2021;33:1205–20.
Michelet X, Dyck L, Hogan A, Loftus RM, Duquette D, Wei K, et al. Metabolic reprogramming of natural killer cells in obesity limits antitumor responses. Nat Immunol. 2018;19:1330–40.
Lv J, Sun H, Gong L, Wei X, He Y, Yu Z, et al. Aberrant metabolic processes promote the immunosuppressive microenvironment in multiple myeloma. Front Immunol. 2022;13:1077768.
Raccosta L, Fontana R, Maggioni D, Lanterna C, Villablanca EJ, Paniccia A, et al. The oxysterol-CXCR2 axis plays a key role in the recruitment of tumor-promoting neutrophils. J Exp Med. 2013;210:1711–28.
Perrone F, Minari R, Bersanelli M, Bordi P, Tiseo M, Favari E, et al. The prognostic role of high blood cholesterol in advanced cancer patients treated with immune checkpoint inhibitors. J Immunother. 2020;43:196–203.
Baek AE, Yu YA, He S, Wardell SE, Chang CY, Kwon S, et al. The cholesterol metabolite 27 hydroxycholesterol facilitates breast cancer metastasis through its actions on immune cells. Nat Commun. 2017;8:864.
Huang J, Das SK, Jha P, Al ZW, Schauer S, Claudel T, et al. The PPARalpha agonist fenofibrate suppresses B-cell lymphoma in mice by modulating lipid metabolism. Biochim Biophys Acta. 2013;1831:1555–65.
Xia L, Oyang L, Lin J, Tan S, Han Y, Wu N, et al. The cancer metabolic reprogramming and immune response. Mol Cancer. 2021;20:28.
DeBerardinis RJ. Tumor microenvironment, metabolism, and immunotherapy. N Engl J Med. 2020;382:869–71.
Xiong J, Wang N, Zhong HJ, Cui BW, Cheng S, Sun R, et al. SLC1A1 mediated glutamine addiction and contributed to natural killer T-cell lymphoma progression with immunotherapeutic potential. EBioMedicine. 2021;72: 103614.
Loftus RM, Assmann N, Kedia-Mehta N, O’Brien KL, Garcia A, Gillespie C, et al. Amino acid-dependent cMyc expression is essential for NK cell metabolic and functional responses in mice. Nat Commun. 2018;9:2341.
Lamas B, Vergnaud-Gauduchon J, Goncalves-Mendes N, Perche O, Rossary A, Vasson MP, et al. Altered functions of natural killer cells in response to l-Arginine availability. Cell Immunol. 2012;280:182–90.
Mussai F, De Santo C, Abu-Dayyeh I, Booth S, Quek L, McEwen-Smith RM, et al. Acute myeloid leukemia creates an arginase-dependent immunosuppressive microenvironment. Blood. 2013;122:749–58.
Steggerda SM, Bennett MK, Chen J, Emberley E, Huang T, Janes JR, et al. Inhibition of arginase by CB-1158 blocks myeloid cell-mediated immune suppression in the tumor microenvironment. J Immunother Cancer. 2017;5:101.
Gorrini C, Harris IS, Mak TW. Modulation of oxidative stress as an anticancer strategy. Nat Rev Drug Discov. 2013;12:931–47.
Moloney JN, Cotter TG. ROS signalling in the biology of cancer. Semin Cell Dev Biol. 2018;80:50–64.
Mellqvist UH, Hansson M, Brune M, Dahlgren C, Hermodsson S, Hellstrand K. Natural killer cell dysfunction and apoptosis induced by chronic myelogenous leukemia cells: role of reactive oxygen species and regulation by histamine. Blood. 2000;96:1961–8.
Aurelius J, Thoren FB, Akhiani AA, Brune M, Palmqvist L, Hansson M, et al. Monocytic AML cells inactivate antileukemic lymphocytes: role of NADPH oxidase/gp91(phox) expression and the PARP-1/PAR pathway of apoptosis. Blood. 2012;119:5832–7.
Brune M, Castaigne S, Catalano J, Gehlsen K, Ho AD, Hofmann WK, et al. Improved leukemia-free survival after postconsolidation immunotherapy with histamine dihydrochloride and interleukin-2 in acute myeloid leukemia: results of a randomized phase 3 trial. Blood. 2006;108:88–96.
Cui Q, Wang JQ, Assaraf YG, Ren L, Gupta P, Wei L, et al. Modulating ROS to overcome multidrug resistance in cancer. Drug Resist Updat. 2018;41:1–25.
Muz B, de la Puente P, Azab F, Luderer M, Azab AK. The role of hypoxia and exploitation of the hypoxic environment in hematologic malignancies. Mol Cancer Res. 2014;12:1347–54.
Ohyashiki JH, Umezu T, Ohyashiki K. Exosomes promote bone marrow angiogenesis in hematologic neoplasia: the role of hypoxia. Curr Opin Hematol. 2016;23:268–73.
Solocinski K, Padget MR, Fabian KP, Wolfson B, Cecchi F, Hembrough T, et al. Overcoming hypoxia-induced functional suppression of NK cells. J Immunother Cancer. 2020;8: e000246.
Teng R, Wang Y, Lv N, Zhang D, Williamson RA, Lei L, et al. Hypoxia Impairs NK Cell Cytotoxicity through SHP-1-Mediated Attenuation of STAT3 and ERK Signaling Pathways. J Immunol Res. 2020;2020:4598476.
Ran GH, Lin YQ, Tian L, Zhang T, Yan DM, Yu JH, et al. Natural killer cell homing and trafficking in tissues and tumors: from biology to application. Signal Transduct Target Ther. 2022;7:205.
Ponzetta A, Benigni G, Antonangeli F, Sciume G, Sanseviero E, Zingoni A, et al. Multiple myeloma impairs bone marrow localization of effector natural killer cells by altering the chemokine microenvironment. Cancer Res. 2015;75:4766–77.
Teijeira A, Garasa S, Gato M, Alfaro C, Migueliz I, Cirella A, et al. CXCR1 and CXCR2 chemokine receptor agonists produced by tumors induce neutrophil extracellular traps that interfere with immune cytotoxicity. Immunity. 2020;52:856–71.
Susek KH, Karvouni M, Alici E, Lundqvist A. The Role of CXC chemokine receptors 1–4 on immune cells in the tumor microenvironment. Front Immunol. 2018;9:2159.
Yan Y, Zheng L, Du Q, Yazdani H, Dong K, Guo Y, et al. Interferon regulatory factor 1(IRF-1) activates anti-tumor immunity via CXCL10/CXCR3 axis in hepatocellular carcinoma (HCC). Cancer Lett. 2021;506:95–106.
DiLillo DJ, Weinberg JB, Yoshizaki A, Horikawa M, Bryant JM, Iwata Y, et al. Chronic lymphocytic leukemia and regulatory B cells share IL-10 competence and immunosuppressive function. Leukemia. 2013;27:170–82.
Alhakeem SS, McKenna MK, Oben KZ, Noothi SK, Rivas JR, Hildebrandt GC, et al. Chronic lymphocytic leukemia-derived IL-10 suppresses antitumor immunity. J Immunol. 2018;200:4180–9.
Wang D, Sun Z, Zhu X, Zheng X, Zhou Y, Lu Y, et al. GARP-mediated active TGF-beta1 induces bone marrow NK cell dysfunction in AML patients with early relapse post-allo-HSCT. Blood. 2022;140:2788–804.
Curti A, Trabanelli S, Onofri C, Aluigi M, Salvestrini V, Ocadlikova D, et al. Indoleamine 2,3-dioxygenase-expressing leukemic dendritic cells impair a leukemia-specific immune response by inducing potent T regulatory cells. Haematologica. 2010;95:2022–30.
Caforio M, Sorino C, Caruana I, Weber G, Camera A, Cifaldi L, et al. GD2 redirected CAR T and activated NK-cell-mediated secretion of IFNgamma overcomes MYCN-dependent IDO1 inhibition, contributing to neuroblastoma cell immune escape. J Immunother Cancer. 2021;9: e001502.
Chakraverty R, Sykes M. The role of antigen-presenting cells in triggering graft-versus-host disease and graft-versus-leukemia. Blood. 2007;110:9–17.
Nahi H, Chrobok M, Meinke S, Gran C, Marquardt N, Afram G, et al. Autologous NK cells as consolidation therapy following stem cell transplantation in multiple myeloma. Cell Rep Med. 2022;3: 100508.
Nguyen R, Wu H, Pounds S, Inaba H, Ribeiro RC, Cullins D, et al. A phase II clinical trial of adoptive transfer of haploidentical natural killer cells for consolidation therapy of pediatric acute myeloid leukemia. J Immunother Cancer. 2019;7:81.
Rosenberg SA, Lotze MT, Muul LM, Chang AE, Avis FP, Leitman S, et al. A progress report on the treatment of 157 patients with advanced cancer using lymphokine-activated killer cells and interleukin-2 or high-dose interleukin-2 alone. N Engl J Med. 1987;316:889–97.
West WH, Tauer KW, Yannelli JR, Marshall GD, Orr DW, Thurman GB, et al. Constant-infusion recombinant interleukin-2 in adoptive immunotherapy of advanced cancer. N Engl J Med. 1987;316:898–905.
Parkhurst MR, Riley JP, Dudley ME, Rosenberg SA. Adoptive transfer of autologous natural killer cells leads to high levels of circulating natural killer cells but does not mediate tumor regression. Clin Cancer Res. 2011;17:6287–97.
Dolstra H, Roeven M, Spanholtz J, Hangalapura BN, Tordoir M, Maas F, et al. Successful Transfer of Umbilical Cord Blood CD34(+) Hematopoietic Stem and Progenitor-derived NK Cells in Older Acute Myeloid Leukemia Patients. Clin Cancer Res. 2017;23:4107–18.
Zhu H, Blum RH, Bjordahl R, Gaidarova S, Rogers P, Lee TT, et al. Pluripotent stem cell-derived NK cells with high-affinity noncleavable CD16a mediate improved antitumor activity. Blood. 2020;135:399–410.
Meng F, Zhang S, Xie J, Zhou Y, Wu Q, Lu B, et al. Leveraging CD16 fusion receptors to remodel the immune response for enhancing anti-tumor immunotherapy in iPSC-derived NK cells. J Hematol Oncol. 2023;16:62.
Tsuchiyama J, Yoshino T, Mori M, Kondoh E, Oka T, Akagi T, et al. Characterization of a novel human natural killer-cell line (NK-YS) established from natural killer cell lymphoma/leukemia associated with Epstein-Barr virus infection. Blood. 1998;92:1374–83.
Suck G, Branch DR, Smyth MJ, Miller RG, Vergidis J, Fahim S, et al. KHYG-1, a model for the study of enhanced natural killer cell cytotoxicity. Exp Hematol. 2005;33:1160–71.
Tam YK, Martinson JA, Doligosa K, Klingemann HG. Ex vivo expansion of the highly cytotoxic human natural killer-92 cell-line under current good manufacturing practice conditions for clinical adoptive cellular immunotherapy. Cytotherapy. 2003;5:259–72.
Boyiadzis M, Agha M, Redner RL, Sehgal A, Im A, Hou JZ, et al. Phase 1 clinical trial of adoptive immunotherapy using “off-the-shelf” activated natural killer cells in patients with refractory and relapsed acute myeloid leukemia. Cytotherapy. 2017;19:1225–32.
Williams BA, Law AD, Routy B, DenHollander N, Gupta V, Wang XH, et al. A phase I trial of NK-92 cells for refractory hematological malignancies relapsing after autologous hematopoietic cell transplantation shows safety and evidence of efficacy. Oncotarget. 2017;8:89256–68.
Shimasaki N, Jain A, Campana D. NK cells for cancer immunotherapy. Nat Rev Drug Discov. 2020;19:200–18.
Gong Y, Klein WR, Wang J, Bos G, Germeraad W. Chimeric antigen receptor natural killer (CAR-NK) cell design and engineering for cancer therapy. J Hematol Oncol. 2021;14:73.
Sadelain M. Chimeric antigen receptors driving immunology towards synthetic biology. Curr Opin Immunol. 2016;41:68–76.
Wang X, Yang X, Yuan X, Wang W, Wang Y. Chimeric antigen receptor-engineered NK cells: new weapons of cancer immunotherapy with great potential. Exp Hematol Oncol. 2022;11:85.
Zhang Y, Zhou W, Yang J, Yang J, Wang W. Chimeric antigen receptor engineered natural killer cells for cancer therapy. Exp Hematol Oncol. 2023;12:70.
Zhang Y, Wallace DL, de Lara CM, Ghattas H, Asquith B, et al. In vivo kinetics of human natural killer cells: the effects of ageing and acute and chronic viral infection. Immunology. 2007;121:258–65.
Pan K, Farrukh H, Chittepu V, Xu H, Pan CX, Zhu Z. CAR race to cancer immunotherapy: from CAR T, CAR NK to CAR macrophage therapy. J Exp Clin Cancer Res. 2022;41:119.
Oei V, Siernicka M, Graczyk-Jarzynka A, Hoel HJ, Yang W, Palacios D, et al. Intrinsic functional potential of NK-cell subsets constrains retargeting driven by chimeric antigen receptors. Cancer Immunol Res. 2018;6:467–80.
Tallerico R, Todaro M, Di Franco S, Maccalli C, Garofalo C, Sottile R, et al. Human NK cells selective targeting of colon cancer-initiating cells: a role for natural cytotoxicity receptors and MHC class I molecules. J Immunol. 2013;190:2381–90.
Leary J, Goodarzi M, Drayton D, Andrian U. T cell- and B cell-independent adaptive immunity mediated by natural killer cells. Nat Immunol. 2006;7:507–16.
Chu J, Deng Y, Benson DM, He S, Hughes T, Zhang J, et al. CS1-specific chimeric antigen receptor (CAR)-engineered natural killer cells enhance in vitro and in vivo antitumor activity against human multiple myeloma. Leukemia. 2014;28:917–27.
Oelsner S, Friede ME, Zhang C, Wagner J, Badura S, Bader P, et al. Continuously expanding CAR NK-92 cells display selective cytotoxicity against B-cell leukemia and lymphoma. Cytotherapy. 2017;19:235–49.
Ng YY, Du Z, Zhang X, Chng WJ, Wang S. CXCR4 and anti-BCMA CAR co-modified natural killer cells suppress multiple myeloma progression in a xenograft mouse model. Cancer Gene Ther. 2022;29:475–83.
Dong H, Ham JD, Hu G, Xie G, Vergara J, Liang Y, et al, Tarannum M, Donner H, Baginska J, et al. Memory-like NK cells armed with a neoepitope-specific CAR exhibit potent activity against NPM1 mutated acute myeloid leukemia.
Liu E, Marin D, Banerjee P, Macapinlac HA, Thompson P, Basar R, et al. Use of CAR-transduced natural killer cells in CD19-positive lymphoid tumors. N Engl J Med. 2020;382:545–53.
Marofi F, Saleh MM, Rahman HS, Suksatan W, Al-Gazally ME, Abdelbasset WK, et al. CAR-engineered NK cells; a promising therapeutic option for treatment of hematological malignancies. Stem Cell Res Ther. 2021;12:374.
Li Y, Hermanson DL, Moriarity BS, Kaufman DS. Human iPSC-derived natural killer cells engineered with chimeric antigen receptors enhance anti-tumor activity. Cell Stem Cell. 2018;23:181–92.
Nanbakhsh A, Best B, Riese M, Rao S, Wang L, Medin J. Dextran enhances the lentiviral transduction efficiency of murine and human primary NK cells. J Vis Exp. 2018;131:55063.
van Ostaijen-ten DM, Prins HJ, Boerman GH, Vervat C, Pende D, Putter H, et al. Preparation of cytokine-activated NK cells for use in adoptive cell therapy in cancer patients: protocol optimization and therapeutic potential. J Immunother. 2016;39:90–100.
Greene S, Robbins Y, Mydlarz W, Huynh A, Schmitt N, Friedman J, et al. Inhibition of MDSC trafficking with SX-682, a CXCR1/2 inhibitor, enhances NK-cell immunotherapy in head and neck cancer models. Clin Cancer Res. 2020;26:1420–31.
Parihar R, Rivas C, Huynh M, Omer B, Lapteva N, Metelitsa L, et al. NK cells expressing a chimeric activating receptor eliminate mdscs and rescue impaired CAR-T cell activity against solid tumors. Cancer Immunol Res. 2019;7:363–75.
Archilla-Ortega A, Domuro C, Martin-Liberal J, Munoz P. Blockade of novel immune checkpoints and new therapeutic combinations to boost antitumor immunity. J Exp Clin Cancer Res. 2022;41:62.
Cao Y, Wang X, Jin T, Tian Y, Dai C, Widarma C, et al. Immune checkpoint molecules in natural killer cells as potential targets for cancer immunotherapy. Signal Transduct Target Ther. 2020;5:250.
Liu Z, Yu X, Xu L, Li Y, Zeng C. Current insight into the regulation of PD-L1 in cancer. Exp Hematol Oncol. 2022;11:44.
Green MR, Monti S, Rodig SJ, Juszczynski P, Currie T, O’Donnell E, et al. Integrative analysis reveals selective 9p24.1 amplification, increased PD-1 ligand expression, and further induction via JAK2 in nodular sclerosing Hodgkin lymphoma and primary mediastinal large B-cell lymphoma. Blood. 2010;116:3268–77.
Armand P, Shipp MA, Ribrag V, Michot JM, Zinzani PL, Kuruvilla J, et al. Programmed death-1 blockade with pembrolizumab in patients with classical hodgkin lymphoma after brentuximab vedotin failure. J Clin Oncol. 2016;34:3733–9.
Khodadoust MS, Rook AH, Porcu P, Foss F, Moskowitz AJ, Shustov A, et al. Pembrolizumab in relapsed and refractory mycosis fungoides and sezary syndrome: a multicenter phase II study. J Clin Oncol. 2020;38:20–8.
Ribrag V, Avigan DE, Green DJ, Wise-Draper T, Posada JG, Vij R, et al. Phase 1b trial of pembrolizumab monotherapy for relapsed/refractory multiple myeloma: KEYNOTE-013. Br J Haematol. 2019;186:e41–4.
Zinzani PL, Ribrag V, Moskowitz CH, Michot JM, Kuruvilla J, Balakumaran A, et al. Safety and tolerability of pembrolizumab in patients with relapsed/refractory primary mediastinal large B-cell lymphoma. Blood. 2017;130:267–70.
Ruggeri L, Capanni M, Casucci M, Volpi I, Tosti A, Perruccio K, et al. Role of natural killer cell alloreactivity in HLA-mismatched hematopoietic stem cell transplantation. Blood. 1999;94:333–9.
Kohrt HE, Thielens A, Marabelle A, Sagiv-Barfi I, Sola C, Chanuc F, et al. Anti-KIR antibody enhancement of anti-lymphoma activity of natural killer cells as monotherapy and in combination with anti-CD20 antibodies. Blood. 2014;123:678–86.
Bagot M, Porcu P, Marie-Cardine A, Battistella M, William BM, Vermeer M, et al. IPH4102, a first-in-class anti-KIR3DL2 monoclonal antibody, in patients with relapsed or refractory cutaneous T-cell lymphoma: an international, first-in-human, open-label, phase 1 trial. Lancet Oncol. 2019;20:1160–70.
Romagne F, Andre P, Spee P, Zahn S, Anfossi N, Gauthier L, et al. Preclinical characterization of 1–7F9, a novel human anti-KIR receptor therapeutic antibody that augments natural killer-mediated killing of tumor cells. Blood. 2009;114:2667–77.
Yalniz FF, Daver N, Rezvani K, Kornblau S, Ohanian M, Borthakur G, et al. A pilot trial of lirilumab with or without azacitidine for patients with myelodysplastic syndrome. Clin Lymphoma Myeloma Leuk. 2018;18:658–63.
Armand P, Lesokhin A, Borrello I, Timmerman J, Gutierrez M, Zhu L, et al. A phase 1b study of dual PD-1 and CTLA-4 or KIR blockade in patients with relapsed/refractory lymphoid malignancies. Leukemia. 2021;35:777–86.
Morad G, Helmink BA, Sharma P, Wargo JA. Hallmarks of response, resistance, and toxicity to immune checkpoint blockade. Cell. 2021;184:5309–37.
Judge SJ, Dunai C, Aguilar EG, Vick SC, Sturgill IR, Khuat LT, et al. Minimal PD-1 expression in mouse and human NK cells under diverse conditions. J Clin Invest. 2020;130:3051–68.
Sharma P, Goswami S, Raychaudhuri D, Siddiqui BA, Singh P, Nagarajan A, et al. Immune checkpoint therapy-current perspectives and future directions. Cell. 2023;186:1652–69.
Postow MA, Sidlow R, Hellmann MD. Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med. 2018;378:158–68.
Davids MS, Kim HT, Costello C, Herrera AF, Locke FL, Maegawa RO, et al. A multicenter phase 1 study of nivolumab for relapsed hematologic malignancies after allogeneic transplantation. Blood. 2020;135:2182–91.
J Randall Patrinely Jr, Rebecca Johnson, Aleigha R Lawless, Prachi Bhave, Amelia Sawyers, Maya Dimitrova, et al. Chronic Immune-Related Adverse Events Following Adjuvant Anti-PD-1 Therapy for High-risk Resected Melanoma. Jama Oncol 2021,7(5):744–748.
Johnson DB, Nebhan CA, Moslehi JJ, Balko JM. Immune-checkpoint inhibitors: long-term implications of toxicity. Nat Rev Clin Oncol. 2022;19:254–67.
Esfahani K, Elkrief A, Calabrese C, Lapointe R, Hudson M, Routy B, et al. Moving towards personalized treatments of immune-related adverse events. Nat Rev Clin Oncol. 2020;17:504–15.
Commins SP, Borish L, Steinke JW. Immunologic messenger molecules: cytokines, interferons, and chemokines. J Allergy Clin Immunol. 2010;125:S53–72.
Mazumder A, Rosenberg SA. Successful immunotherapy of natural killer-resistant established pulmonary melanoma metastases by the intravenous adoptive transfer of syngeneic lymphocytes activated in vitro by interleukin 2. J Exp Med. 1984;159:495–507.
Lafreniere R, Rosenberg SA. Successful immunotherapy of murine experimental hepatic metastases with lymphokine-activated killer cells and recombinant interleukin 2. Cancer Res. 1985;45:3735–41.
Rosenberg SA, Mule JJ, Spiess PJ, Reichert CM, Schwarz SL. Regression of established pulmonary metastases and subcutaneous tumor mediated by the systemic administration of high-dose recombinant interleukin 2. J Exp Med. 1985;161:1169–88.
Miller JS, Tessmer-Tuck J, Pierson BA, Weisdorf D, McGlave P, Blazar BR, et al. Low dose subcutaneous interleukin-2 after autologous transplantation generates sustained in vivo natural killer cell activity. Biol Blood Marrow Transplant. 1997;3:34–44.
Dutcher JP, Gaynor ER, Boldt DH, Doroshow JH, Bar MH, Sznol M, et al. A phase II study of high-dose continuous infusion interleukin-2 with lymphokine-activated killer cells in patients with metastatic melanoma. J Clin Oncol. 1991;9:641–8.
Kruit WH, Punt KJ, Goey SH, de Mulder PH, van Hoogenhuyze DC, Henzen-Logmans SC, et al. Cardiotoxicity as a dose-limiting factor in a schedule of high dose bolus therapy with interleukin-2 and alpha-interferon. An unexpectedly frequent complication. Cancer-Am Cancer Soc. 1994;74:2850–6.
Zhang H, Chua KS, Guimond M, Kapoor V, Brown MV, Fleisher TA, et al. Lymphopenia and interleukin-2 therapy alter homeostasis of CD4+CD25+ regulatory T cells. Nat Med. 2005;11:1238–43.
Ghiringhelli F, Menard C, Terme M, Flament C, Taieb J, Chaput N, et al. CD4+CD25+ regulatory T cells inhibit natural killer cell functions in a transforming growth factor-beta-dependent manner. J Exp Med. 2005;202:1075–85.
Romee R, Cooley S, Berrien-Elliott MM, Westervelt P, Verneris MR, Wagner JE, et al. First-in-human phase 1 clinical study of the IL-15 superagonist complex ALT-803 to treat relapse after transplantation. Blood. 2018;131:2515–27.
Parrish-Novak J, Dillon SR, Nelson A, Hammond A, Sprecher C, Gross JA, et al. Interleukin 21 and its receptor are involved in NK cell expansion and regulation of lymphocyte function. Nature. 2000;408:57–63.
Timmerman JM, Byrd JC, Andorsky DJ, Yamada RE, Kramer J, Muthusamy N, et al. A phase I dose-finding trial of recombinant interleukin-21 and rituximab in relapsed and refractory low grade B-cell lymphoproliferative disorders. Clin Cancer Res. 2012;18:5752–60.
Talpaz M, Kantarjian H, McCredie K, Trujillo J, Keating M, Gutterman JU. Therapy of chronic myelogenous leukemia. Cancer-Am Cancer Soc. 1987;59:664–7.
Nguyen KB, Salazar-Mather TP, Dalod MY, Van Deusen JB, Wei XQ, Liew FY, et al. Coordinated and distinct roles for IFN-alpha beta, IL-12, and IL-15 regulation of NK cell responses to viral infection. J Immunol. 2002;169:4279–87.
Bhattacharya S, Zheng H, Tzimas C, Carroll M, Baker DP, Fuchs SY. Bcr-abl signals to desensitize chronic myeloid leukemia cells to IFNalpha via accelerating the degradation of its receptor. Blood. 2011;118:4179–87.
Hjorth-Hansen H, Stentoft J, Richter J, Koskenvesa P, Hoglund M, Dreimane A, et al. Safety and efficacy of the combination of pegylated interferon-alpha2b and dasatinib in newly diagnosed chronic-phase chronic myeloid leukemia patients. Leukemia. 2016;30:1853–60.
Hughes TP, Hochhaus A, Branford S, Muller MC, Kaeda JS, Foroni L, et al. Long-term prognostic significance of early molecular response to imatinib in newly diagnosed chronic myeloid leukemia: an analysis from the International Randomized Study of Interferon and STI571 (IRIS). Blood. 2010;116:3758–65.
Dreno B, Urosevic-Maiwald M, Kim Y, Guitart J, Duvic M, Dereure O, et al. TG1042 (Adenovirus-interferon-gamma) in primary cutaneous B-cell lymphomas: a phase II clinical trial. PLoS ONE. 2014;9: e83670.
Lin Z, Liu L, Li Z, Xu B. Bispecific antibodies as monotherapy or in combinations for non-hodgkin B-cell lymphoma: latest updates from the American society of hematology 2022 annual meeting. Exp Hematol Oncol. 2023;12:41.
Felices M, Lenvik TR, Davis ZB, Miller JS, Vallera DA. Generation of BiKEs and TriKEs to Improve NK Cell-Mediated Targeting of Tumor Cells. Methods Mol Biol. 2016;1441:333–46.
Chames P, Van Regenmortel M, Weiss E, Baty D. Therapeutic antibodies: successes, limitations and hopes for the future. Br J Pharmacol. 2009;157:220–33.
Holliger P, Hudson PJ. Engineered antibody fragments and the rise of single domains. Nat Biotechnol. 2005;23:1126–36.
Gleason MK, Verneris MR, Todhunter DA, Zhang B, McCullar V, Zhou SX, et al. Bispecific and trispecific killer cell engagers directly activate human NK cells through CD16 signaling and induce cytotoxicity and cytokine production. Mol Cancer Ther. 2012;11:2674–84.
Singer H, Kellner C, Lanig H, Aigner M, Stockmeyer B, Oduncu F, et al. Effective elimination of acute myeloid leukemic cells by recombinant bispecific antibody derivatives directed against CD33 and CD16. J Immunother. 2010;33:599–608.
Kugler M, Stein C, Kellner C, Mentz K, Saul D, Schwenkert M, et al. A recombinant trispecific single-chain Fv derivative directed against CD123 and CD33 mediates effective elimination of acute myeloid leukaemia cells by dual targeting. Br J Haematol. 2010;150:574–86.
Gleason MK, Ross JA, Warlick ED, Lund TC, Verneris MR, Wiernik A, et al. CD16xCD33 bispecific killer cell engager (BiKE) activates NK cells against primary MDS and MDSC CD33+ targets. Blood. 2014;123:3016–26.
Hartmann F, Renner C, Jung W, Deisting C, Juwana M, Eichentopf B, et al. Treatment of refractory Hodgkin’s disease with an anti-CD16/CD30 bispecific antibody. Blood. 1997;89:2042–7.
Renner C, Hartmann F, Pfreundschuh M. Treatment of refractory Hodgkin’s disease with an anti-CD16/CD30 bispecific antibody. Cancer Immunol Immunother. 1997;45:184–6.
Kellner C, Bruenke J, Horner H, Schubert J, Schwenkert M, Mentz K, et al. Heterodimeric bispecific antibody-derivatives against CD19 and CD16 induce effective antibody-dependent cellular cytotoxicity against B-lymphoid tumor cells. Cancer Lett. 2011;303:128–39.
Glorius P, Baerenwaldt A, Kellner C, Staudinger M, Dechant M, Stauch M, et al. The novel tribody [(CD20)(2)xCD16] efficiently triggers effector cell-mediated lysis of malignant B cells. Leukemia. 2013;27:190–201.
Rothe A, Sasse S, Topp MS, Eichenauer DA, Hummel H, Reiners KS, et al. A phase 1 study of the bispecific anti-CD30/CD16A antibody construct AFM13 in patients with relapsed or refractory Hodgkin lymphoma. Blood. 2015;125:4024–31.
Bartlett NL, Herrera AF, Domingo-Domenech E, Mehta A, Forero-Torres A, Garcia-Sanz R, et al. A phase 1b study of AFM13 in combination with pembrolizumab in patients with relapsed or refractory Hodgkin lymphoma. Blood. 2020;136:2401–9.
An NK-cell Therapy for CD30+ Lymphomas. Cancer Discov 2022, 12:1401–1402.
Davis ZB, Vallera DA, Miller JS, Felices M. Natural killer cells unleashed: Checkpoint receptor blockade and BiKE/TriKE utilization in NK-mediated anti-tumor immunotherapy. Semin Immunol. 2017;31:64–75.
Chan WK, Kang S, Youssef Y, Glankler EN, Barrett ER, Carter AM, et al. A CS1-NKG2D Bispecific Antibody Collectively Activates Cytolytic Immune Cells against Multiple Myeloma. Cancer Immunol Res. 2018;6:776–87.
Vallera DA, Felices M, McElmurry R, McCullar V, Zhou X, Schmohl JU, et al. IL15 Trispecific Killer Engagers (TriKE) Make Natural Killer Cells Specific to CD33+ targets while also inducing persistence, in vivo expansion, and enhanced function. Clin Cancer Res. 2016;22:3440–50.
Arvindam US, van Hauten P, Schirm D, Schaap N, Hobo W, Blazar BR, et al. A trispecific killer engager molecule against CLEC12A effectively induces NK-cell mediated killing of AML cells. Leukemia. 2021;35:1586–96.
Gauthier L, Morel A, Anceriz N, Rossi B, Blanchard-Alvarez A, Grondin G, et al. Multifunctional natural killer cell engagers targeting NKp46 trigger protective tumor immunity. Cell. 2019;177:1701–13.
Gauthier L, Virone-Oddos A, Beninga J, Rossi B, Nicolazzi C, Amara C, et al. Control of acute myeloid leukemia by a trifunctional NKp46-CD16a-NK cell engager targeting CD123. Nat Biotechnol. 2023;1:1.
Demaria O, Gauthier L, Debroas G, Vivier E. Natural killer cell engagers in cancer immunotherapy: Next generation of immuno-oncology treatments. Eur J Immunol. 2021;51:1934–42.
Sun JC, Beilke JN, Lanier LL. Adaptive immune features of natural killer cells. Nature. 2009;457:557–61.
O’Sullivan TE, Sun JC, Lanier LL. Natural killer cell memory. Immunity. 2015;43:634–45.
Cooper MA, Elliott JM, Keyel PA, Yang L, Carrero JA, Yokoyama WM. Cytokine-induced memory-like natural killer cells. Proc Natl Acad Sci U S A. 2009;106:1915–9.
Ni J, Miller M, Stojanovic A, Garbi N, Cerwenka A. Sustained effector function of IL-12/15/18-preactivated NK cells against established tumors. J Exp Med. 2012;209:2351–65.
Romee R, Rosario M, Berrien-Elliott MM, Wagner JA, Jewell BA, Schappe T, et al. Cytokine-induced memory-like natural killer cells exhibit enhanced responses against myeloid leukemia. Sci Transl Med. 2016;8:123r–357r.
Gang M, Marin ND, Wong P, Neal CC, Marsala L, Foster M, et al. CAR-modified memory-like NK cells exhibit potent responses to NK-resistant lymphomas. Blood. 2020;136:2308–18.
Cichocki F, Zhang B, Wu CY, Chiu E, Day A, O’Connor RS, et al. Nicotinamide enhances natural killer cell function and yields remissions in patients with non-Hodgkin lymphoma. Sci Transl Med. 2023;15: e3341.
Rubio-Azpeitia E, Perez-Corral AM, Dorado-Herrero N, Monsalvo S, Perez-Balsera G, Fernandez-Santos ME, et al. Clinical grade production of IL-15 stimulated NK cells for early infusion in adult AML patients undergoing haploidentical stem cell transplantation with post-transplant cyclophosphamide. Transfusion. 2022;62:374–85.
Berrien-Elliott MM, Becker-Hapak M, Cashen AF, Jacobs M, Wong P, Foster M, et al. Systemic IL-15 promotes allogeneic cell rejection in patients treated with natural killer cell adoptive therapy. Blood. 2022;139:1177–83.
Silla L, Valim V, Pezzi A, Da SM, Wilke I, Nobrega J, et al. Adoptive immunotherapy with double-bright (CD56(bright) /CD16(bright) ) expanded natural killer cells in patients with relapsed or refractory acute myeloid leukaemia. A proof-of-concept study. Br J Haematol. 2021;195:710–21.
Gomez GL, Escudero A, Mestre C, Fuster SJ, Martinez AP, Vagace VJ, et al. Phase 2 Clinical Trial of Infusing Haploidentical K562-mb15-41BBL-activated and expanded natural killer cells as consolidation therapy for pediatric acute myeloblastic leukemia. Clin Lymphoma Myeloma Leuk. 2021;21:328–37.
Cooley S, He F, Bachanova V, Vercellotti GM, DeFor TE, Curtsinger JM, et al. First-in-human trial of rhIL-15 and haploidentical natural killer cell therapy for advanced acute myeloid leukemia. Blood Adv. 2019;3:1970–80.
Fehniger TA, Miller JS, Stuart RK, Cooley S, Salhotra A, Curtsinger J, et al. A phase 1 trial of CNDO-109-activated natural killer cells in patients with high-risk acute myeloid leukemia. Biol Blood Marrow Transplant. 2018;24:1581–9.
Bjorklund AT, Carlsten M, Sohlberg E, Liu LL, Clancy T, Karimi M, et al. Complete remission with reduction of high-risk clones following haploidentical NK-cell therapy against MDS and AML. Clin Cancer Res. 2018;24:1834–44.
Ciurea SO, Schafer JR, Bassett R, Denman CJ, Cao K, Willis D, et al. Phase 1 clinical trial using mbIL21 ex vivo-expanded donor-derived NK cells after haploidentical transplantation. Blood. 2017;130:1857–68.
Lee KH, Yoon SR, Gong JR, Choi EJ, Kim HS, Park CJ, et al. The infusion of ex vivo, interleukin-15 and -21-activated donor NK cells after haploidentical HCT in high-risk AML and MDS patients-a randomized trial. Leukemia. 2023;37:807–19.
Bednarski JJ, Zimmerman C, Berrien-Elliott MM, Foltz JA, Becker-Hapak M, Neal CC, et al. Donor memory-like NK cells persist and induce remissions in pediatric patients with relapsed AML after transplant. Blood. 2022;139:1670–83.
Shapiro RM, Birch GC, Hu G, Vergara CJ, Nikiforow S, Baginska J, et al. Expansion, persistence, and efficacy of donor memory-like NK cells infused for posttransplant relapse. J Clin Invest. 2022;132:1.
Berrien-Elliott MM, Foltz JA, Russler-Germain DA, Neal CC, Tran J, Gang M, et al. Hematopoietic cell transplantation donor-derived memory-like NK cells functionally persist after transfer into patients with leukemia. Sci Transl Med. 2022;14: m1375.
Acknowledgements
Not applicable.
Funding
This study was funded by National Natural Science Foundation (No.82270200, No.82070203 and No.81770210); Key Research and Development Program of Shandong Province (No.2018CXGC1213); Taishan Scholars Program of Shandong Province (No. tspd20230610, No. tspd20231251); Translational Research Grant of NCRCH (No.2021WWB02, No.2020ZKMB01); Shandong Provincial Engineering Research Center of Lymphoma; Academic Promotion Programme of Shandong First Medical University (No. 2019QL018); China Postdoctoral Science Foundation (No. 2023M741506); Shandong Provincial Natural Science Foundation (No. ZR2023QH193).
Author information
Authors and Affiliations
Contributions
JS wrote this manuscript, created figures and tables. SH and XW reviewed and revised the manuscript. XW provided direction and guidance throughout the preparation of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shang, J., Hu, S. & Wang, X. Targeting natural killer cells: from basic biology to clinical application in hematologic malignancies. Exp Hematol Oncol 13, 21 (2024). https://doi.org/10.1186/s40164-024-00481-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40164-024-00481-y