Abstract
Background
In Viet Nam, tuberculosis (TB) represents a devastating life-event with an exorbitant price tag, partly due to lost income from daily directly observed therapy in public sector care. Thus, persons with TB may seek care in the private sector for its flexibility, convenience, and privacy. Our study aimed to measure income changes, costs and catastrophic cost incurrence among TB-affected households in the public and private sector.
Methods
Between October 2020 and March 2022, we conducted 110 longitudinal patient cost interviews, among 50 patients privately treated for TB and 60 TB patients treated by the National TB Program (NTP) in Ha Noi, Hai Phong and Ho Chi Minh City, Viet Nam. Using a local adaptation of the WHO TB patient cost survey tool, participants were interviewed during the intensive phase, continuation phase and post-treatment. We compared income levels, direct and indirect treatment costs, catastrophic costs using Wilcoxon rank-sum and chi-squared tests and associated risk factors between the two cohorts using multivariate regression.
Results
The pre-treatment median monthly household income was significantly higher in the private sector versus NTP cohort (USD 868 vs USD 578; P = 0.010). However, private sector treatment was also significantly costlier (USD 2075 vs USD 1313; P = 0.005), driven by direct medical costs which were 4.6 times higher than costs reported by NTP participants (USD 754 vs USD 164; P < 0.001). This resulted in no significant difference in catastrophic costs between the two cohorts (Private: 55% vs NTP: 52%; P = 0.675). Factors associated with catastrophic cost included being a single-person household [adjusted odds ratio (aOR = 13.71; 95% confidence interval (CI): 1.36–138.14; P = 0.026], unemployment during treatment (aOR = 10.86; 95% CI: 2.64–44.60; P < 0.001) and experiencing TB-related stigma (aOR = 37.90; 95% CI: 1.72–831.73; P = 0.021).
Conclusions
Persons with TB in Viet Nam face similarly high risk of catastrophic costs whether treated in the public or private sector. Patient costs could be reduced through expanded insurance reimbursement to minimize direct medical costs in the private sector, use of remote monitoring and multi-week/month dosing strategies to avert economic costs in the public sector and greater access to social protection mechanism in general.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Tuberculosis (TB) is a pandemic that has ravaged public health for thousands of years [1], causing an estimated billion deaths in the past two centuries [2]. In 2022, TB was the world’s second deadliest infectious disease with 10.6 million individuals falling sick with and 1.3 million people dying of TB [3]. The disease’s devastating effects are exacerbated by its surreptitious bias towards impoverished families and individuals, granting the disease the moniker of parent, child and provider of poverty [4].
TB-affected families often face depletion of resources and savings due to the long, arduous treatment, resulting in a substantial impairment of the productivity of the patient and economic wellbeing of the TB-affected family [5,6,7]. Consequently, a ‘catastrophic costs’ indicator was conceived to measure the deleterious socioeconomic impact, defined as a loss of ≥ 20% of annual household income, due to an episode of TB [8]. To measure this indicator, a standardized survey instrument and guidance for data collection were developed [9]. This growing appreciation of the need to address catastrophic costs [10, 11] culminated in the inclusion of the goal of zero TB-affected households suffering from catastrophic costs by 2025 in the World Health Organization’s (WHO) End TB Strategy [12]. However, the recent estimate that 48% of individuals with TB experience catastrophic costs highlights a gaping dissonance between ambition and reality [13].
In Viet Nam, an estimated 172,000 individuals fell ill with TB, including 9200 people with drug-resistant TB in 2022, causing an estimated 13,600 deaths [14]. Quality-assured TB care is provided by the National TB Program (NTP) at District TB Units. While persons with TB receive diagnosis and treatment largely free of charge, pre-treatment services such as chest x-ray and liver function tests have to be paid out of pocket. A nationally representative patient cost survey of persons with TB receiving treatment from the NTP found that 63% of households affected by drug-susceptible TB (DS-TB) experienced catastrophic costs. The catastrophic cost incurrence was primarily driven by lost income associated with the inability to retain employment or paid leave, or having to switch to less laborious occupations with lower levels of remuneration. Root causes of these productivity losses were the TB-related disabilities and directly observed therapy (DOT) requirements tied to the quality-assured TB care provided by the NTP [15].
In response, 31% of persons with TB in Viet Nam seek care in the private sector. Despite concerns about the quality or safety of care, and potential supply-induced demand [16,17,18], the greater privacy to protect from stigma and related negative social consequences especially for women [19,20,21,22] along with the convenience of self-administered treatment, multi-day dosing, shorter wait times and after-hour consultations are perceived to outweigh high out-of-pocket treatment costs [23,24,25,26]. However, to date there have been no studies to verify this perceived trade-off by directly comparing catastrophic cost incurrence in TB-affected households between people receiving care from the private sector versus the NTP. Our study aimed to measure income changes, costs and catastrophic cost incurrence among TB-affected households in the public and private sector.
Methods
Study design
This was a prospective cohort study to measure the comparative patient costs and rates of catastrophic cost incurrence among affected families due to an episode of DS-TB in public and private sectors. Data were collected using a localized, longitudinal adaptation of the WHO patient cost survey tool.
Study setting
The study was conducted in Ha Noi, Hai Phong and Ho Chi Minh City (HCMC). These high TB burden, urban provinces had a combined population of 19.1 million persons per the latest census and according to NTP surveillance notified 23,502 persons with DS-TB in 2019. Since 2017, the Viet Nam NTP has implemented a private sector engagement model with an implementation partner, Friends for International TB Relief, serving the role of an intermediary agency to collect, verify and notify private TB treatment data [16]. This collaboration enabled the patient cost comparisons between private and public cohorts.
Study population and eligibility
The study population consisted of persons with DS-TB taking and completing treatment with the NTP or a private healthcare provider. Recruitment occurred between October 2020 and March 2022 and employed a continuous sampling strategy for the private cohort. Participants for the public cohort were recruited to match with private participants in terms of residing district and treatment initiation date. All treatment-naïve persons aged 18 years or older with pulmonary DS-TB, residence in the study provinces and providing informed consent to participate were included. Persons already participating in or with a household member participating in another patient cost survey were excluded to avoid double counting this household in the overall dataset, and avoid bias from overstating the risk of catastrophic costs.
Data sources and collection
Our study employed the WHO patient cost survey tool, adapted for longitudinal data collection and for local conditions as detailed elsewhere [27]. Briefly, the tool assessed participant characteristics, financial and economic costs, and socioeconomic impact due to the episode of TB. The latter included changes in employment status, food insecurity, productivity loss, social exclusion and use of coping strategies [9]. In terms of localization, the tool was translated and the survey’s asset list was expanded with items relevant for the urban Vietnamese context. For the longitudinal adaptation, questions concerning pre-treatment costs, social health insurance (SHI) status and asset ownership were omitted during the second and third interviews. To reduce recall bias, participants were surveyed at three separate time points. In accordance with national TB treatment guidelines, uncomplicated DS-TB treatment consists of a two-month intensive phase, followed by a four-month continuation phase. The first survey took place within the intensive phase of treatment, but after two weeks from initiation. The second survey was conducted within two months after the participant entered the continuation phase of treatment. The last survey took place within two months of treatment completion.
Recruitment in the public sector was done by study staff situated at the public TB care facilities upon treatment initiation. Private sector recruitment occurred based on introduction and referral by the private provider with their client’s consent. Interviews were typically conducted face-to-face at the Lung Hospital, District TB Unit, commune health station, patient’s house or other places convenient for the participant. From 2021, interviews were conducted primarily via phone to sustain recruitment and ensure follow-up during periods of social distancing in response to the COVID-19 pandemic [28]. Paper-based consent forms were collected from all participants regardless of the interview modality. Participants were asked to produce receipts from all healthcare interactions at their second and third interview to reduce recall and social desirability bias. Data were collected on paper and audio recorded. Paper surveys were digitized using the Organizational Network Analysis data survey tool (Ona, Nairobi, Kenya). On a monthly basis, five percent of digital surveys were randomly selected and verified by another interviewer using the audio recordings.
Statistical analyses
Demographic, socioeconomic, clinical and behavioral characteristics as well as health seeking behaviors were described by public and private cohort. Categorical variables were tabulated by frequencies and proportions; continuous variables by mean and standard deviation, or median and interquartile range based on their distribution. To analyze differences, Chi-squared, Fisher's exact, Student’s t or Wilcoxon rank-sum tests were performed as applicable.
Household incomes pre-treatment, during the intensive phase, the continuation phase and at the end of treatment for both cohorts were tabulated by mean and standard deviation, as well as median and interquartile range, and compared by Wilcoxon rank-sum test due to their right skewed distribution.
Patient cost calculations followed WHO guidelines [9]. Direct medical costs encompassed consultations, diagnostic tests, hospitalizations and medications. Direct non-medical expenses encompassed expenditure related to food, travel and accommodation arising from medical visits, supplements and loan interest. Indirect costs were defined as reported income loss during treatment only and were calculated using the output approach with caregiver time loss excluded to match the national patient cost survey [15]. We calculated mean and median direct medical, direct non-medical and indirect costs for the entire episode of TB, as well as disaggregated into pre-treatment and treatment phases. Given large standard deviations, we used the Wilcoxon rank-sum test to analyze differences in costs between the two cohorts. We disaggregated total treatment costs by main cost components (medical, non-medical and indirect) and direct medical costs by unplanned health care visits and hospitalizations, drug pick-ups, and follow-up appointments. These cost breakdowns were compared across cohort using t-tests for proportions.
Catastrophic cost was defined as total costs exceeding 20% of the annual household income prior to diagnosis [9]. The catastrophic cost estimates for the two cohorts were compared using χ2 tests. We fitted univariate and multivariate logistic regression models to assess the association between catastrophic cost incurrence as the primary outcome and survey cohort as the primary exposure. Secondary covariates were included to adjust for confounding included demographic, socioeconomic, behavioral and health-seeking factors based on prior research [29,30,31]. A post-hoc analysis to investigate the association of household income and patient costs in the private sector did not yield relevant associations (Additional file 1).
All costs were collected in Viet Nam Dong (VND) and converted to US dollars (USD) using the average 2020–2022 exchange rates reported by XE.com for the study period (VND 1 = USD 0.000043). Hypotheses were two-tailed and P-values below 0.05 were considered statistically significant. Data were analyzed using Stata v17 (Stata Corp, College Station, TX, USA).
Results
Participant characteristics and health-seeking
We identified 294 persons TB treated in the private sector and 90 by the NTP. Of these, we recruited 64 participants in each of the private (64/294 = 22%) and NTP (64/90 = 71%) survey cohorts. There were 14 (14/64 = 22%) and 4 (4/64 = 6%) participants in the respective cohorts who did not complete all of the survey milestones. Therefore, the final study sample consisted of 50 private sector and 60 NTP participants (Table 1).
Most participants were male (79/110 = 72%), with a mean age of 44.4 years. About 51% reported completion of secondary schooling, 44% indicated that they were the main earners in their household and 85% reported SHI coverage. While 13% were unemployed before treatment initiation, this proportion increased to 41% during treatment. Only 6% reported a history of TB, but the majority (77%) reported a comorbidity. About 5% of participants reported daily alcohol consumption, while 17% were daily smokers. In terms of health-seeking, the median diagnostic delay was eight weeks between the onset of symptoms and treatment initiation.
While most of the sample was homogenous across the two cohorts, significantly more participants from the private sector cohort completed secondary education compared to the NTP cohort (62% vs 42%; P = 0.034). There were also significantly more participants with bacteriologic confirmation in the private sector cohort (80% vs 62%; P = 0.037). Similarly, participants from the private sector cohort visited more healthcare providers prior to treatment (5 vs 6, P = 0.046).
Household income
The pre-treatment median monthly household income was USD 678 [Inter-quartile range (IQR): USD 430–1032] across all participants (Table 2). Household incomes fell by over 30% to USD 471 (IQR: USD 322–903) and USD 473 (IQR: USD 292–882) during the intensive and continuation phases, respectively, and rose to USD 602 (IQR: USD 280–860) by the end of treatment, representing 89% of the pre-TB earnings. The median household income was significantly higher in the private sector cohort prior to treatment (USD 868 vs USD 578; P = 0.010) and during the intensive phase of treatment (USD 763 vs USD 419; P = 0.003), but income differences in the continuation phase were not significant. By the end of treatment significant differences in income between the private sector and NTP cohorts were restored (USD 710 vs USD 464; P = 0.006).
Costs of TB care
The median total costs of an episode of DS-TB across the sample were USD 1726 (IQR: USD 879–2820) (Table 3). Of these, median pre-treatment costs were USD 151 (IQR: USD 72–236) and consisted mainly of direct medical costs of USD 138 (IQR: USD 55–212). Median treatment costs were USD 1541 (IQR: USD 737–2477), driven primarily by indirect costs with a median of USD 585 (IQR: USD 0–1548) (Fig. 1).
When comparing private sector and NTP cohorts, median total costs in the private sector cohort were significantly higher (USD 2075 vs USD 1313; P = 0.005). This was primarily driven by the significant differences in direct medical costs (USD 754 vs USD 164; P < 0.0001) in both the pre-treatment (USD 153 vs USD 99; P = 0.028) and treatment phases (USD 609 vs USD 16; P < 0.001). Specifically, the main cost driver was the cost of drugs, which comprised 90% direct medical costs within the private sector cohort (Fig. 2). Between the private sector and NTP cohorts, there were no significant differences in median direct non-medical costs (USD 398 vs USD 345; P = 0.737) and indirect costs from lost salaries and wages (USD 710 vs USD 578; P = 0.954). However, indirect costs comprised a significantly higher portion of total costs for the NTP cohort (64% vs 42%; P = 0.021) due to the larger share of direct medical costs in the private sector cohort (Fig. 3).
Catastrophic costs and associated risks
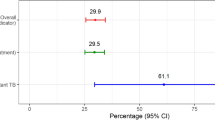
Catastrophic cost incurrence in the private sector and NTP cohorts were 52% and 55%, respectively (Table 4). There was no evidence of a statistical difference in the risk of catastrophic cost incurrence in either cohort [adjusted Odds Ratio (aOR) = 1.26; 95% CI: 0.42–3.77; P = 0.675]. Instead, risk factors associated with catastrophic cost incurrence include being a single-person household (aOR = 13.71; 95% CI: 1.36–138.14; P = 0.026), unemployment during treatment (aOR = 10.86; 95% CI: 2.64–44.60; P < 0.001) and experiencing TB-related stigma (aOR = 37.90; 95% CI: 1.72–831.73; P = 0.021).
Discussion
Our study found no difference in catastrophic cost incurrence in public and private sector TB treatment. Surprisingly, we also did not detect a difference in indirect costs, which disproves our hypothesis that the lack of DOT in private sector care can alleviate costs from lost salaries and wages. Conversely, as expected we measured high direct medical costs before and during treatment in the private sector, largely arising from drug pick-ups, as well as higher pre-treatment household incomes among private sector participants to help absorb the higher treatment costs. Overall, our study highlighted that an episode of TB in Viet Nam represents a costly life-event, irrespective of whether treatment is sought in public or private sectors, with catastrophic costs mainly driven by economic and social factors.
The rates of catastrophic cost incurrence measured on our study (52–55%) were concordant with rates measured among DS-TB patients receiving NTP care on prior studies conducted in Viet Nam at national and sub-national levels (30–63%). This concordance also applies to previously reported median total costs of an episode of DS-TB (USD 894–1779), median indirect costs (USD 460–925) and the percentage of indirect costs as a proportion of total (48–68%), strengthening the generalizability of our results in the Vietnamese context [27, 32, 33].
Our regression analysis showed that catastrophic cost incurrence was driven mainly by socioeconomic risk factors, such as being a single income household and becoming unemployed during TB treatment. This association between income insecurity and susceptibility to catastrophic costs is well documented in Viet Nam and other high burden settings [31, 34, 35]. As such, expansion of access, coverage and level of support of social protection mechanisms in TB-endemic countries remains urgently needed [36]. One such example is the charity fund for TB patients, called Patient Support to Fight TB (PASTB), established by the Viet Nam NTP in response to the national patient cost survey results. PASTB has financed the purchase of SHI coverage and unreimbursed expenses related to TB care such as chest x-rays or liver function tests [37]. Beyond these short-term mitigation efforts, the NTP has sought collaborations with the Ministry of Health and Ministry of Labor, Invalids and Social Affairs to explore adaptation measures, such as making existing social protection schemes accessible to persons with TB, linking TB survivors with vocational training and exploring avenues for better job protection and worker’s rights [38]. In the short-term, alternative indirect measures could include scaling up active case finding and community-based interventions to alleviate the economic and social burden on TB-affected families and individuals [39, 40].
Another risk factor of catastrophic cost incurrence was patient-experienced stigma. Studies have reported that public sector care and the associated DOT requirement may intensify stigma [41, 42]. Consequently, there is a growing momentum towards people-centered care that addresses social determinants, including stigmatization [43]. As part of this movement, demands have included the phase out of traditional DOT, which has constituted a pillar of public sector patient management over the last three decades [44,45,46]. Removing the DOT requirement could both reduce stigma and alleviate much of the indirect cost burden in the public sector, which represented 52% of total treatment costs within the NTP cohort and was equal to the average monthly household income before the episode of TB.
While the lack of DOT has long represented a core value proposition of the private sector to clients [19, 47], it also constitutes one of its core criticisms from a public health perspective, due to suspicions of fueling drug resistance [17, 48]. Thus, it may be helpful to offer an alternative to ensure that the quality of care is maintained. Many process alternatives to facility-based DOT have been deemed effective for patient care [46, 49]. Specifically, these alternatives include community-based DOT [50,51,52], home delivery and multi-period dispensing for self-administered therapy [53, 54]. More recently, digital adherence technologies (DAT) have emerged [55,56,57]. These include video-DOT [58, 59], SMS-based remote monitoring tools, such as 99DOTS [60], and Medication Event Reminder Monitors [61]. These tools remain underutilized given the limited, discordant evidence on the impact of DATs on clinical outcomes, incremental treatment costs and patient-centeredness of care [62,63,64,65].
With respect to optimizing private sector TB care, direct medical costs could be shifted to public health financing schemes. Viet Nam has set ambitious targets of achieving Universal Health Coverage through its national SHI scheme [66]. In doing so, Viet Nam has embarked on transitioning major public health programs for HIV and TB to SHI financing [67, 68]. However, the TB transition is in its infancy and thus continues to face challenges [69] and the current national SHI scheme offers suboptimal protection [70]. Nevertheless, the principle could conceivably be applied to the private sector as well to reduce the financial burden of treatment for patients [71, 72]. This is particularly needed for informally employed individuals who comprised one-third of our sample. Their options for treatment tend to be restricted by their limited job security, which may force them to seek out costly private sector care as a form of social protection, despite the premium it commands. It is noteworthy that regional precedence exists. In the healthcare systems of some Asian countries, privatization of TB care and pay-for-performance schemes have task shifted a portion of the TB caseload to the private sector [73, 74].
A key limitation of our study was the small sample size of persons with TB receiving private sector care who agreed to participate. This resulted in a potential underpowering of statistical comparisons leading to missed distinctions between the two cohorts. Furthermore, a core value proposition of private TB treatment is the privacy offered to patients unwilling to be exposed to the stigma attached to the disease, particularly among women, so that our results contain an inherent selection bias [75, 76]. Lastly, this study was set in three municipal provinces with a high degree of urbanization, thus limiting generalizability to rural settings, where travel times and transport costs would likely be very different. The timing of the data collection, much of which occurred at the height of the COVID-19 pandemic, may have further introduced bias, as external factors other than TB may have affected drivers of catastrophic costs.
This was the first direct comparison of catastrophic cost incurrence in private versus public sector patients. More evidence is undoubtedly needed to elucidate the underlying differences between private versus NTP care, including job security and social protection, the consequent complex choices persons with TB have to make in light of the prevailing information asymmetry and threat of misinformation, and the socioeconomic consequences they have to bear. However, there is little doubt that the question of how to achieve zero TB-affected families suffering catastrophic costs must be addressed to ensure greater health equity, effective abatement of the deleterious socioeconomic consequences and to end TB both as a public health emergency and a catastrophic life-event for affected families.
Conclusions
High costs for patients and affected families remain a major barrier to global ambitions to end TB. In their personal calculus, each person with TB needs to make the choice of treatment provider, public or private, that offers the greatest perceived benefit. Currently, TB-affected persons in Viet Nam either face high time loss and foregone income with the NTP or high out-of-pocket treatment costs with private providers. It is therefore imperative to explore ways to invert the current paradigm and enable persons with TB to have access to several affordable treatment options. This particularly applies to TB-affected households that typically are poorer than the general population. Changes in policies and practice, such as expansion of SHI reimbursement for private TB care services or introduction of remote adherence monitoring by the NTP, may alleviate the socioeconomic burden for TB-affected individuals and families, accelerate reductions in catastrophic costs towards achieving End TB Strategy goals, and produce greater equity in health.
Availability of data and materials
The data that support the findings of this study are available from the Viet Nam National Lung Hospital/NTP, Ha Noi Lung Hospital, Hai Phong Lung Hospital and Pham Ngoc Thach Hospital. However, restrictions apply to the availability of these data, which include programmatic clinical patient information, and so are not publicly available. Data can be made available from the authors upon reasonable request and with permission of the relevant government authorities listed above.
Abbreviations
- DAT:
-
Digital adherence technology
- DOT:
-
Directly observed therapy
- HCMC:
-
Ho Chi Minh City
- IQR:
-
Inter-quartile range
- NTP:
-
National TB program
- (a)OR :
-
(Adjusted) odds ratio
- SD :
-
Standard deviation
- SHI:
-
Social health insurance
- (DS-)TB:
-
(Drug-susceptible) tuberculosis
- VNĐ:
-
Viet Nam Dong
- WHO:
-
World Health Organization
References
Daniel TM. The history of tuberculosis. Respir Med. 2006;100:1862–70.
Epidemiology PT. A mortal foe. Nature. 2013;502:S2-3.
World Health Organization. Global Tuberculosis Report 2023. Geneva, Switzerland; 2023.
Watson HH. African learning experience. Nurs Stand. 2014;28:66–66.
Tanimura T, Jaramillo E, Weil D, Raviglione M, Lönnroth K. Financial burden for tuberculosis patients in low- and middle-income countries: a systematic review. Eur Respir J. 2014;43:1763–75.
Kyu HH, Maddison ER, Henry NJ, Ledesma JR, Wiens KE, Reiner R, et al. Global, regional, and national burden of tuberculosis, 1990–2016: results from the Global Burden of Diseases, Injuries, and Risk Factors 2016 Study. Lancet Infect Dis. 2018;18:1329–49.
Silva S, Arinaminpathy N, Atun R, Goosby E, Reid M. Economic impact of tuberculosis mortality in 120 countries and the cost of not achieving the Sustainable Development Goals tuberculosis targets: a full-income analysis. Lancet Glob Heal. 2021;9:e1372–9.
Wingfield T, Tovar MA, Huff D, Boccia D, Montoya R, Ramos E, et al. The economic effects of supporting tuberculosis-affected households in Peru. Eur Respir J. 2016;48:1396–410.
World Health Organization. Tuberculosis patient cost surveys: a handbook. 2017.
Wingfield T, Tovar MA, Huff D, Boccia D, Saunders MJ, Datta S, et al. Beyond pills and tests: addressing the social determinants of tuberculosis. Clin Med. 2016;16:s79-91.
Boccia D, Bond V. The catastrophic cost of tuberculosis: advancing research and solutions. Int J Tuberc Lung Dis. 2019;23:1129–30.
World Health Organization. The End TB Strategy. Geneva, Switzerland; 2015.
World Health Organization. Global Tuberculosis Report 2022. Geneva, Switzerland; 2022.
World Health Organization. Global Tuberculosis Report 2023—Country Profile: Viet Nam. Geneva, Switzerland; 2023.
Nhung NV, Hoa NB, Anh NT, Ngoc Anh LT, Siroka A, Lönnroth K, et al. Measuring catastrophic costs due to tuberculosis in Viet Nam. Int J Tuberc Lung Dis. 2018;22:983–90.
Vo LNQ, Codlin AJ, Huynh HB, Mai TDT, Forse RJ, Van TV, et al. Enhanced private sector engagement for tuberculosis diagnosis and reporting through an intermediary agency in Ho Chi Minh City, Viet Nam. Trop Med Infect Dis. 2020;5:143.
Lönnroth K, Tran TU, Thuong LM, Quy HT, Diwan V. Can I afford free treatment? Perceived consequences of health care provider choices among people with tuberculosis in Ho Chi Minh City, Vietnam. Soc Sci Med. 2001;52:935–48.
Lönnroth K, Thuong LM, Lambregts K, Quy HT, Diwan VK. Private tuberculosis care provision associated with poor treatment outcome: comparative study of a semi-private lung clinic and the NTP in two urban districts in Ho Chi Minh City, Vietnam. Int J Tuberc Lung Dis. 2003;7:165–71.
Courtwright A, Turner AN. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. 2010;125(SUPPL. 4):34–42.
Nhassengo P, Yoshino C, Zandamela A, De Carmo V, Burström B, Lönnroth K, et al. ‘They didn’t look at me with good eyes’–experiences of the socioeconomic impact of tuberculosis and support needs among adults in a semi-rural area in Mozambique: a qualitative study. Glob Public Health. 2024;19:2311682.
Hof S, Najilis C, Bloss E, Straetemans M. A systematic review on the role of gender in tuberculosis control. Adv Med Sci. 2010;63:1–2.
Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11:353–63.
Hanson C, Osberg M, Brown J, Durham G, Chin DP. Finding the missing patients with tuberculosis: lessons learned from patient-pathway analyses in 5 countries. J Infect Dis. 2017;216:S686–95.
Lönnroth K, Thuong LM, Linh PD, Diwan V. Risks and benefits of private health care: exploring physicians’ views on private health care in Ho Chi Minh City, Vietnam. Health Policy. 1998;45:81–97.
Viet Nam National TB Control Programme. Measuring the level of under-reporting and estimating incidence for tuberculosis in Viet Nam: preliminary results TB Inventory Study 2016–2017. In: Workshop Report January. Ha Noi; 2018.
Nguyen MP, Tariq A, Hinchcliff R, Luu HN, Dunne MP. Contribution of private health services to universal health coverage in low and middle-income countries: factors affecting the use of private over public health services in Vietnam. Int J Health Plann Manage. 2023;38:1613–28.
Vo LNQ, Forse RJ, Codlin AJ, Dang HM, Van Truong V, Nguyen LH, et al. Socio-protective effects of active case finding on catastrophic costs from tuberculosis in Ho Chi Minh City, Viet Nam: a longitudinal patient cost survey. BMC Health Serv Res. 2021;21:1051.
World Health Organization. Viet Nam COVID-19 Situation Report # 108. Ha Noi, Viet Nam; 2023.
Kirubi B, Ongango J, Nguhiu P, Lönnroth K, Rono A, Sidney-Annerstedt K. Determinants of household catastrophic costs for drug sensitive tuberculosis patients in Kenya. Infect Dis Poverty. 2021;10:95.
Kilale AM, Pantoja A, Jani B, Range N, Ngowi BJ, Makasi C, et al. Economic burden of tuberculosis in Tanzania: a national survey of costs faced by tuberculosis-affected households. BMC Public Health. 2022;22:600.
Stracker N, Hanrahan C, Mmolawa L, Nonyane B, Tampi R, Tucker A, et al. Risk factors for catastrophic costs associated with tuberculosis in rural South Africa. Int J Tuberc Lung Dis. 2019;23:756–63.
Nhung NV, Hoa NB, Anh NT, Anh LTN, Siroka A, Lönnroth K, et al. Measuring catastrophic costs due to tuberculosis in Viet Nam. Int J Tuberc Lung Dis. 2018;22:983–90.
Dinh LV, Wiemers AMC, Forse RJ, Phan YTH, Codlin AJ, Annerstedt KS, et al. Comparing catastrophic costs: active vs. passive tuberculosis case finding in urban Vietnam. Trop Med Infect Dis. 2023;8:423.
Fuady A, Houweling TAJ, Mansyur M, Richardus JH. Catastrophic total costs in tuberculosis-affected households and their determinants since Indonesia’s implementation of universal health coverage. Infect Dis Poverty. 2018;7:3.
Muniyandi M, Thomas BE, Karikalan N, Kannan T, Rajendran K, Saravanan B, et al. Association of tuberculosis with household catastrophic expenditure in South India. JAMA Netw open. 2020;3: e1920973.
Wingfield T, Tovar MA, Huff D, Boccia D, Montoya R, Ramos E, et al. A randomized controlled study of socioeconomic support to enhance tuberculosis prevention and treatment, Peru. Bull World Heal Organ. 2017;95:270–80.
Ministry of Interior Affairs. Approval of the bylaws and to establish the Patient Support Foundation to end TB (PASTB). Viet Nam; 2018.
Nguyen HB, Nguyen NV. National tuberculosis patients cost survey: research findings lead to change in policy and practice, Viet Nam. Public Heal Action. 2019;9:50–2.
Vo LNQ, Forse RJ, Codlin AJ, Vu TN, Le GT, Do GC, et al. A comparative impact evaluation of two human resource models for community-based active tuberculosis case finding in Ho Chi Minh City, Viet Nam. BMC Public Health. 2020;20:934.
Verguet S, Riumallo-Herl C, Gomez GB, Menzies NA, Houben RMGJ, Sumner T, et al. Catastrophic costs potentially averted by tuberculosis control in India and South Africa: a modelling study. Lancet Glob Heal. 2017;5:e1123–32.
McLaren ZM, Milliken AA, Meyer AJ, Sharp AR. Does directly observed therapy improve tuberculosis treatment? More evidence is needed to guide tuberculosis policy. BMC Infect Dis. 2016;16:537.
Cremers AL, Gerrets R, Kapata N, Kabika A, Birnie E, Klipstein-Grobusch K, et al. Tuberculosis patients’ pre-hospital delay and non-compliance with a longstanding DOT programme: a mixed methods study in urban Zambia. BMC Public Health. 2016;16:1130.
Stop TB Partnership. The Global Plan to End TB 2023-2030. Geneva, Switzerland; 2022.
Tuberculosis Coalition for Technical Assistance. International Standards for Tuberculosis Care (ISTC): Diagnosis, treatment, public health. 2006.
World Health Organization. What is DOTS? A Guide to Understanding the WHO-recommended TB Control Strategy Known as DOTS. Geneva, Switzerland; 1999.
Zimmer AJ, Heitkamp P, Malar J, Dantas C, O’Brien K, Pandita A, et al. Facility-based directly observed therapy (DOT) for tuberculosis during COVID-19: a community perspective. J Clin Tuberc Other Mycobact Dis. 2021;24: 100248.
Philip S, Isaakidis P, Sagili KD, Meharunnisa A, Mrithyunjayan S, Kumar AMV. “They know, they agree, but they don’t do”—the paradox of tuberculosis case notification by private practitioners in Alappuzha district, Kerala, India. PLoS ONE. 2015;10:1–13.
Mahendradhata Y. The case for stronger regulation of private practitioners to control tuberculosis in low- and middle-income countries Infectious Diseases. BMC Res Notes. 2015;8:600.
Steffen R, Menzies D, Oxlade O, Pinto M, de Castro AZ, Monteiro P, et al. Patients’ costs and cost-effectiveness of tuberculosis treatment in dots and non-dots facilities in Rio de Janeiro, Brazil. PLoS ONE. 2010;5: e14014.
Zhang H, Ehiri J, Yang H, Tang S, Li Y. Impact of community-based DOT on tuberculosis treatment outcomes: a systematic review and meta-analysis. PLoS ONE. 2016;11: e0147744.
Wright CM, Westerkamp L, Korver S, Dobler CC. Community-based directly observed therapy (DOT) versus clinic DOT for tuberculosis: a systematic review and meta-analysis of comparative effectiveness. BMC Infect Dis. 2015;15:210.
Vo LNQ, Codlin AJ, Forse RJ, Nguyen HT, Vu TN, Van Truong V, et al. Tuberculosis among economic migrants: a cross-sectional study of the risk of poor treatment outcomes and impact of a treatment adherence intervention among temporary residents in an urban district in Ho Chi Minh City, Viet Nam. BMC Infect Dis. 2020;20:134.
Zimmer AJ, Klinton JS, Oga-Omenka C, Heitkamp P, Nawina Nyirenda C, Furin J, et al. Tuberculosis in times of COVID-19. J Epidemiol Community Health. 2022;76:310–6.
International Union Against Tuberculosis and Lung Disease. Abstract Book. In: 51st World Conference on Lung Health of the International Union Against Tuberculosis and Lung Disease (The Union). 2020. p. S1–480.
Berger C, Patel D, Kityamuwesi A, Ggita J, Tinka LK, Turimumahoro P, et al. Opportunities to improve digital adherence technologies and TB care using human-centered design. Int J Tuberc Lung Dis. 2020;24:1112–5.
Guzman K, Crowder R, Leddy A, Maraba N, Jennings L, Ahmed S, et al. Acceptability and feasibility of digital adherence technologies for drug-susceptible tuberculosis treatment supervision: a meta-analysis of implementation feedback. PLOS Digit Heal. 2023;2: e0000322.
World Health Organization. Report of the WHO consultation on digital technologies for tuberculosis. Geneva, Switzerland; 2023.
Garfein RS, Collins K, Muñoz F, Moser K, Cerecer-Callu P, Raab F, et al. Feasibility of tuberculosis treatment monitoring by video directly observed therapy: a binational pilot study. Int J Tuberc Lung Dis. 2015;19:1057–64.
Nguyen TA, Pham MT, Nguyen TL, Nguyen VN, Pham DC, Nguyen BH, et al. Video Directly Observed Therapy to support adherence with treatment for tuberculosis in Vietnam: a prospective cohort study. Int J Infect Dis. 2017;65:85–9.
Thakkar D, Piparva K, Lakkad S. A pilot project: 99DOTS information communication technology-based approach for tuberculosis treatment in Rajkot district. Lung India. 2019;36:108.
Drabarek D, Anh NT, Nhung NV, Hoa NB, Fox GJ, Bernays S. Implementation of Medication Event Reminder Monitors among patients diagnosed with drug susceptible tuberculosis in rural Viet Nam: a qualitative study. PLoS ONE. 2019;14: e0219891.
Teo AKJ, Morishita F, Islam T, Viney K, Ong CWM, Kato S, et al. Tuberculosis in older adults: challenges and best practices in the Western Pacific Region. Lancet Reg Health West Pac. 2023;36: 100770.
Holzman SB, Zenilman A, Shah M. Advancing patient-centered care in tuberculosis management: a mixed-methods appraisal of video directly observed therapy. Open Forum Infect Dis. 2018;5(4):ofy046.
Beeler Asay GR, Lam CK, Stewart B, Mangan JM, Romo L, Marks SM, et al. Cost of tuberculosis therapy directly observed on video for health departments and patients in New York city; San Francisco, California; and Rhode Island (2017–2018). Am J Public Health. 2020;110:1696–703.
Oxlade O, Benedetti A, Adjobimey M, Alsdurf H, Anagonou S, Cook VJ, et al. Effectiveness and cost-effectiveness of a health systems intervention for latent tuberculosis infection management (ACT4): a cluster-randomised trial. Lancet Public Health. 2021;6:e272–82.
Le QN, Blizzard L, Si L, Giang LT, Neil AL. The evolution of social health insurance in Vietnam and its role towards achieving universal health coverage. Health Policy Open. 2020;1: 100011.
Local Health System Sustainability Project. LHSS Supports Vietnam to Cover TB Drugs in National Health Insurance, Paving the Way for Sustainable TB Treatment. 2022.
Vu LTH, Johns B, Bui QTT, Duong Thuy A, Nguyen Thi D, Nguyen Thi H, et al. Moving to social health insurance financing and payment for HIV/AIDS treatment in Vietnam. Health Serv Insights. 2021;14:1178632920988843.
Viet Nam National TB Control Programme. NTP Year-end report 2022. Ha Noi, Viet Nam; 2022. (In Vietnamese)
Thu Thuong NT, Van Den Berg Y, Huy TQ, Tai DA, Anh BNH. Determinants of catastrophic health expenditure in Vietnam. Int J Health Plann Manage. 2021;36:316–33.
Adepoju VA, Oladimeji O, Horsburgh CR. Rethinking Public Private Mix (PPM) performance in the tuberculosis program: how is care seeking impacting this model in high TB burden countries? Healthcare (Basel). 2022;10(7):1285.
Wells WA, Uplekar M, Pai M. Achieving systemic and scalable private sector engagement in tuberculosis care and prevention in Asia. PLoS Med. 2015;12: e1001842.
Yu S, Sohn H, Kim HY, Kim H, Oh KH, Kim HJ, et al. Evaluating the impact of the nationwide public-private mix (PPM) program for tuberculosis under National Health Insurance in South Korea: a difference in differences analysis. PLoS Med. 2021;18: e1003717.
Lee CY, Chi MJ, Yang SL, Lo HY, Cheng SH. Using financial incentives to improve the care of tuberculosis patients. Am J Manag Care. 2015;21:e35-42.
Lönnroth K, Thuong LM, Linh PD, Diwan V. Utilization of private and public health-care providers for tuberculosis symptoms in Ho Chi Minh City, Vietnam. Health Policy Plan. 2001;16:47–54.
Long NH, Johansson E, Diwan VK, Winkvist A. Fear and social isolation as consequences of tuberculosis in Vietnam: a gender analysis. Health Policy (New York). 2001;58:69–81.
Acknowledgements
The authors would like to thank the Viet Nam NTP hosted by the National Lung Hospital, as well as the People’s Committees, Health Departments, and Lung Hospitals of Ha Noi, Hai Phong and Ho Chi Minh City. We also express our gratitude to public health staff and private sector partners at primary and secondary care levels, and the communities and patients involved in the study.
Funding
Open access funding provided by Karolinska Institute. This work was funded by the Stop TB Partnership’s TB REACH initiative through Grant agreement STBP/TRREACH/GSA/W7-7001 and associated amendments.
Author information
Authors and Affiliations
Contributions
Funding was acquired by LNQV, AJC and RJF. The methodology was developed by RJF, YTHP, AJC, KSA, JS, KL and LNQV. Formal analyses were conducted by AMCW and YTHP. AMCW, LNQV and YTHP were responsible for visualization of the data. Resources were contributed by LVD, HBN, TDN, TMHD, LHN, JC and LNQV. The investigation was conducted by HBH, TTTD and YTHP, all three of whom were also responsible for data curation. Data were validated by AJC, RJF, AMCW and LNQV. Project administration was the responsibility of YTHP, RJF, TTTD and HBH. The original draft was prepared by LNQV. Overall supervision of the study was provided by LVD, HBN, TDN, KSA, KL, JS, TMHD, LHN, and LNQV. All authors reviewed and edited the draft manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Helsinki Declaration (7th Revision) and in strict compliance with guidelines and regulations of the Government of Viet Nam. Ethical approval for study-specific data collection was granted by the Ethical Review Board for Biomedical Research at Ha Noi University of Public Health (300/2020/YTCC-HD3, 17 July 2020; Amendments: 160/2021/YTCC-HD3, 12 April 2021, 345/2021/YTCC-HD3, 19 August 2021) and the Board of Ethics for Biomedical Research at Pham Ngoc Thach Hospital (1225/PNTH-HDDD, 16 September 2020; Amendment: 359/PNT-HDDD, 02 April 2021). Routine interventions were approved by the Ministry of Health (128/QD-BYT, 17 January 2020; 413/QD-BYT, 21 January 2021) and the HCMC People’s Committee (2681/QD-UBND, 29 July 2020; 3083/QD-UBND, 23 August 2021). All participants included in the analysis had provided informed written consent. Data were pseudonymized prior to analysis.
Consent for publication
Not applicable.
Competing interests
LNQV, AJC, RJF, YTHP, TTTD and HBH received funding from UNOPS/Stop TB Partnership. All other author(s) declared no competing interests.
Supplementary Information
Additional file 1.
Supplementary material and table.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nguyen, H.B., Vo, L.N.Q., Forse, R.J. et al. Is convenience really king? Comparative evaluation of catastrophic costs due to tuberculosis in the public and private healthcare sectors of Viet Nam: a longitudinal patient cost study. Infect Dis Poverty 13, 27 (2024). https://doi.org/10.1186/s40249-024-01196-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-024-01196-2