Abstract
Background
The optimal duration of immune checkpoint blockade (ICB) therapy is not well established. Active residual disease is considered prohibitive for treatment discontinuation and its detection by diagnostic CT imaging is limited. Here, we set out to determine the potential added value of 2-[18F]fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) to identify patients at higher risk of relapse following discontinuation of ICB in advanced melanoma.
Methods
Metastatic melanoma patients who discontinued ICB were identified retrospectively. Eligible patients received FDG-PET and diagnostic CT within four months of ICB discontinuation. We defined morphologic response using RECIST v1.1. Complete metabolic response (CMR) was defined as uptake in tumor lesions below background, whereas any site of residual, FDG-avid disease was rated as non-CMR. The primary endpoint was time to progression (TTP) after therapy discontinuation stratified by morphologic and metabolic imaging response using Kaplan–Meier estimates and log-rank test.
Results
Thiry-eight patients were eligible for this analysis. Median follow-up was 37.3 months since ICB discontinuation. Median TTP in the overall cohort was not reached. A greater proportion of patients were rated as CMR in PET (n = 34, 89.5%) as compared to complete response (CR) in CT (n = 13, 34.2%). Median TTP was reached in patients with non-CMR (12.7 months, 95%CI 4.4-not reached) but not for patients with CMR (log-rank: p < 0.001). All patients with complete response by CT had CMR by PET. In a subset of patients excluding those with complete response by CT, TTP remained significantly different between CMR and non-CMR (log-rank: p < 0.001).
Conclusion
Additional FDG-PET at time of discontinuation of ICB therapy helps identify melanoma patients with a low risk of recurrence and favourable prognosis compared to CT imaging alone. Results may have clinical relevance especially for patients with residual tumor burden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Immune checkpoint blockade (ICB) with programmed cell death protein-1 (PD-1) and/or cytotoxic T lymphocyte antigen-4 (CTLA-4) inhibitors remarkably improved 5-year overall survival (OS) rates in patients with metastatic melanoma [1,2,3,4]. In contrast to conventional chemotherapy, ICB can induce high rates of durable responses, even when treatment is discontinued [5]. In the CheckMate 067 trial, 74% patients in the combined anti-PD-1 and anti-CTLA-4 treatment arm who were still alive after 5 years (n = 151) had discontinued immunotherapy and had not received subsequent systemic therapy [4]. In the phase 3 KEYNOTE-006 study, sustained efficacy was seen in patients who discontinued therapy according to protocol after 2 years of treatment [3]. OS of patients who stopped treatment with stable disease as best response, however, was inferior to patients with partial or complete response [6].
Optimal duration of ICB treatment in patients with metastatic melanoma has not been defined yet. Most clinical trials evaluating PD-1 and PD-L1 inhibitors for metastatic melanoma did not limit duration of treatment and drugs were to be given until disease progression, unacceptable toxicitiy or withdrawal of consent [7]. Few clinical trials have observed patients who discontinued treatment after responding to therapy, and prospective studies exploring the optimal timing of treatment discontinuation have only recently started recruitment [8].
A current review suggested that discontinuation of ICB can be considered in advanced melanoma patients who show a complete response (CR) for at least six months after discussion of risks and benefits. If partial response (PR) or stable disease (SD) is present and unchanged for at least six months, additional 2-[18F]fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) imaging and pathological assessment could identify patients without vital disease who could safely pause immunotherapy [7].
This study investigated the value of FDG-PET to determine the potential added value of FDG-PET to further identify patients with residual morphologic disease and at risk of relapse following discontinuation of immunotherapy in metastatic melanoma.
Methods
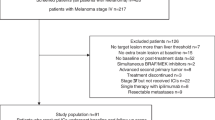
This is a monocentric, retrospective study of metastatic melanoma patients who discontinued immunotherapy. To identify eligible patients, institutional database records were searched for melanoma patients who discontinued immunotherapy for either unacceptable toxicity or durable response (i.e. at least 6 months of tumor control on conventional imaging and decision to discontinue based on multidisciplinary tumorboard) between 2010 and 2020.
Patients who received adjuvant ICB were excluded. Eligible metastatic patients had to have discontinued treatment with CTLA-4 and/or PD-1 inhibitors due to unacceptable toxicity and/or durable response and have received both, FDG-PET and diagnostic CT examinations within 4 months of discontinuation of ICB. Decision for therapy cessation in most cases was discussed due to durable CT-response and additional FDG-PET to detect residual metabolic disease at the time of discontinuation. Patients were not included in this analysis if they had switched or stopped ICB due to progression.
Diagnostic CT (i.e. full dose and contrast enhanced) as part of PET/CT imaging was permitted (n = 33). In case of low-dose PET/CT, a post-treatment full-dose CT scan within 6 weeks of discontinuation was required (observed range 6–38 days) (n = 5). Morphologic CT response was defined by RECIST v1.1. FDG-PET was performed as per EANM guidelines [9]. In brief, patients received a mean activity of 314 ± 75 MBq FDG and underwent PET following a mean of 67 ± 17 min after injection. CT images were used for attenuation correction. Complete metabolic response (CMR) at the time of discontinuation was defined as uptake in tumor lesions below background levels, using mediastinal blood pool as reference. Most patients had no baseline scan prior to ICB for comparison; any site of residual, FDG-avid disease was therefore rated as non-CMR. In patients with cerebral metastases (n = 3) (stage M1d according to American Joint Cancer Committee (AJCC) 8th edition), cranial magnetic resonance imaging (MRI) response was also considered. Following the evaluated FDG-PET and CT, patients received a standardized follow-up consisting of staging examinations comprising CT images of the thorax, abdomen, and MRI of the skull every three months as per clinical routine. Additional imaging examinations were added depending on individual indication. Staging examinations were continued at three-monthly intervals and therapy response was assessed for all patients during and after therapy discontinuation.
The primary endpoint was time to progression (TTP) stratified by morphologic response (i.e. grouped into CR, PR and SD as per RECIST v1.1) using diagnostic CT and cranial MRI in case of cerebral metastasis and metabolic response (i.e. grouped into CMR and non-CMR) using PET. TTP was defined as time from discontinuation until clinical or radiological evidence of tumor progression or recurrence. Survival of subgroups was compared using Kaplan–Meier methods and log-rank comparisons.
As secondary endpoint, we report overall survival (OS) measured from time of therapy start. Chi-squared test was used to compare the rate of recurrence within 12 months between complete responders from morphologic and metabolic imaging. The relative risk (RR) was calculated as the ratio of the probability of relapse within 12 months. Grade 3 or higher toxicities were recorded using Common Terminology Criteria of Adverse Events (CTCAE Version 5.0) definitions. All statistical analyses were performed using R statistics (version 3.4.1, www.r-project.org). The study was approved by the local ethics committee (Reference: 20–9433-BO).
Results
We identified 38 eligible patients who discontinued ICB. Patient characteristics are outlined in Table 1. Median age at the time of PET scan was 58 years (range 33–86); 22 patients (57.9%) were male. Most patients had received combined immunotherapy (n = 24, 63.2%). PD-1 monotherapy was either nivolumab (n = 5, 13.2%) or pembrolizumab (n = 9, 23.7%). Seven patients (18.4%) had received prior lines of ICB, e.g. as adjuvant therapy. A BRAF mutation was present in 15 patients (39.5%). Median treatment duration was 19.0 months (range 0.7–48.0). Twenty-three out of 38 patients (60.5%) experienced toxicities greater or equal to CTCAE grade 3. Most frequent toxicities were colitis (n = 7, 18.4%) and hepatitis (n = 6, 15.8%). Detailed information on adverse events in this cohort can be found in the supplement.
Treatment was discontinued due to unacceptable toxicity in 11 patients (28.9%) and due to durable response in 27 patients (71.1%). Median time to therapy discontinuation for patients ceasing therapy for durable response was 24.0 months (range 8.7–48.0) from ICB start and 1.3 months (range 0.7–22.0) in patients who discontinued due to unacceptable toxicity.
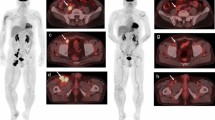
FDG-PET was performed within four months of treatment cessation (median 0.3, range -3.7–4.0). PET identified a greater proportion of patients with complete response compared to RECIST in CT. According to CT, four patients (10.5%), had stable disease (SD), 21 (55.3%) had a PR, and 13 (34.2%) had a CR at the time of treatment discontinuation CT. Based on FDG-PET, 34 (89.5%) patients had CMR and four (10.5%) patients had non-CMR. Of 34 patients with CMR in PET, 13/34 (38.2%), 18/34 (52.9%) and 3/34 (8.8%) had CR, PR and SD in CT, respectively. Of four patients with non-CMR, 3/4 (75.0%) and 1/4 (25.0%) were classified as PR and SD by CT. In total, 21 patients with residual, non-progressive disease (i.e. PR or SD) in CT were identified with CMR in PET. Table 2 shows a comparison of PET and CT responses.
Median TTP of the total cohort was not reached. At a median follow-up time of 37.3 months since immunotherapy discontinuation, disease relapse had occurred in six patients (Additional file table 3), four had ceased immunotherapy for durable response and two for unacceptable toxicity. Three out of four (75.0%) patients with non-CMR at time of discontinuation had progression, and threeout of thirty-four (8.8%) patients with CMR. Of the patients with relapse, 2/6 (33.3%), 3/6 (50.0%) and 1/6 (16.7%) patients had CR, PR and SD according to CT-assessed RECIST at the time of discontinuation, respectively. According to PET, 3/6 (50.0%) patient with relapse after discontinuation had been rated CMR at the time of discontinuation and 3/6 (50.0%) patients had been rated non-CMR. Fig. 1 illustrates patients’ events since start of ICB.
All thirty eight patients had > 12 months of follow-up and were thus available for analysis of relative risk for progression within twelve months after discontinuation. Patients without complete response in metabolic imaging had higher relative risk (RR) of recurrence (RR 8.3, 95%CI 2.4–27.9); Chi-square: p = 0.008). Results were not significant for morphologic imaging (RR 1.1, 95%CI 0.2- 5.1; Chi-square: p = 0.9).
Median TTP was not reached in any RECIST subgroup (Fig. 2a). Patients with non-CMR had a significantly shorter TTP compared to CMR patients (12.7 months, 95%CI 4.4-NR, vs not reached, p < 0.0001, Fig. 2B).
In patients with residual, non-progressive disease (i.e. PR and SD) identified by CT (n = 25), further classification was achieved by metabolic imaging. From these, 21/25 (84.0%) patients had CMR identified by PET, which was associated with longer TTP compared to non-CMR (12.7 months, 95%CI 4.4-NR, vs not reached, p = 0.0007, Fig. 2C). Three of 34 (8.8%) patients with CMR at therapy discontinuation received subsequent systemic treatment with either pembrolizumab therapy, adjuvant nivolumab monotherapy after complete resection of recurrence, or combinational therapy of ipilimumab plus nivolumab. Recurrence occurred 2.5, 24.2 and 24.0 months after therapy discontinuation, respectively (Additional file Table 3), all other patients with CMR had no recurrence until data cut and did not receive subsequent therapy. Three patients with non-CMR received subsequent systemic therapies following disease progression, hereof two patients with PD-1 monotherapy and one patient underwent surgery. Response to subsequent systemic therapy was CR in one patient (16.7%), PR in one patient (16.7%) and SD in another (16.7%). Two patients with CR at time of discontinuation have received subsequent therapy. Detailed outcomes of patients with relapse are listed in Additional file table 3.
Median OS was not reached. One patient died with unknown cause of death. Median survival of subgroups was also not reached. Survival curves for overal survivall can be found in the supplement.
Discussion
Durable responses and ongoing remissions even after discontinuation of ICB [3, 4] evoke hope of cure in both patients and physicians. Currently, however, no accurate instrument is available that identifies patients who do not require further maintenance treatment. Although toxicities usually occur early after starting ICB, the possibility of late-emergent toxicity as well as time burden for both the patient and the healthcare system give a strong reason to discuss the required treatment duration with ICB [8]. Biomarkers that reliably differentiate between patients who require additional treatment and those who can safely stop treatment are urgently needed.
Three modalities are available to exclude residual disease to allow safe treatment discontinuation: blood-based biomarkers, histology, and imaging. Among blood-based biomarkers, circulating tumor DNA (ctDNA) has efficacy in predicting and monitoring response of melanoma to immunotherapy [10,11,12]. To date however, liquid biopsies are not routinely used for the detection of residual disease following.
No published study has systematically obtained histologic specimen in patients following palliative immunotherapy of melanoma, but some knowledge can be derived from neoadjuvant ICB in other solid tumors [13]. However, pathological assessment is not an option for patients with metastatic disease at multiple sites.
Metabolic imaging with FDG-PET complements morphologic assessments, especially with predominant hybrid PET/CT or PET/MRI scanners available. FDG-PET scans are highly effective in staging of advanced melanoma [14] and have been demonstrated to be able to detect early metabolic responses that are predictive of survival [15,16,17] In routine practice, however, regular (re-)staging is performed by means of CT and MRI examinations as PET scans are often not reimbursed. Notably, the socioeconomic burden of ICB beyond clinical benefit would greatly outweigh the cost of additional PET scans for this cohort, which supports the rationale to test prospectively PET-based treatment discontinuation [8].
To date, most publications on FDG-PET response assessment of ICB in malignant melanoma have focused on predicting responses early in the course of treatment to identify non-responding patients. Iravani et al. found that PET response after a median of 2.4 months of combination ICB was predictive of survival. Additionally, inflammatory findings in PET were also capable of detecting immune-related adverse events even before clinical onset [15]. Ito et al. evaluated FDG-PET for monitoring response to ipilimumab and found FDG-PET response to be a strong predictor of overall survival but identified pseudo-progression in non-target lesions as a potential pitfall [16].
Kong et al. investigated the added value of FDG-PET to detect residual metabolic disease in 27 melanoma patients receiving anti-PD-1 therapy [18]. In their study, five patients with CMR stopped treatment and did not develop a recurrence within a 6–10 months follow-up period [18]. We here present outcomes of 38 patients discontinuing ICB of which 34 had a CMR. After a median follow-up of 37.3 months, three (8.8%) of these patients had disease relapse after > 24 months of therapy discontinuation, with completely resectable in one, complete response to reinitiation of pembrolizumab in another, suggesting that for patients with CMR the risk of relapse is low and relapse might be treatable. This demonstrates that favourable metabolic response on FDG-PET can further select patients with durable tumor control to ICB and underlines its value to guide treatment discontinuation. In this regard, Schank et al. found that metabolic responsiveness predicted disease progression in patients without progression at therapy discontinuation [19].
We observed a low rate of relapse in patients with morphologic complete response and no patient with morphologic complete response had residual metabolic disease. Therefore, additional FDG-PET to assess risk for relapse might be of greatest value in patients with durable SD and PR seen in CT. More than half of all patients in this study achieved only PR or SD according to RECIST v1.1 but were complete metabolic responders by PET. Similar results had been observed for patients under continued immunotherapy. Following 12 months of immunotherapy, 68% of melanoma patients with PR in CT had CMR in FDG-PET, which was associated with longer progression-free survival when compared to patients with non-CMR [20].
The ongoing phase II PET-Stop trial (NCT04462406) investigates the feasibility of PET-guided discontinuation of anti PD-1 therapy. To be eligible for active surveillance, patients will either have to have a negative PET-scan or a negative biopsy of PET-positive regions to rule out residual tumor after 52 weeks of immunotherapy. However, results are not expected before 2026. In the meantime, discontinuation will remain an individual approach. Our study provides a rationale for FDG-PET in multiple settings arising during ICB. These include e.g. [1] prior to per-protocol discontinuation of ICB, [2] when toxicity limits therapy continuation, [3] if patients wish to cease systemic therapy, to guide decision making, especially in patients with residual disease visible in CT.
Although the present study benefits from long follow-up with regular imaging (typically every three months), it is limited by the retrospective assessment and a small sample size and does not serve as definitive evidence. Furthermore, we did not perform systematic biopsies in these patients and therefore, non-CMR was often not confirmed. Despite this, high rates of relapse following non-CMR scans support the hypothesis that these patients had residual disease.
Finally, there is need for biomarker-driven, randomized trials in advanced melanoma patients to determine safety, quality of life benefit, socioeconomic impact and (most-importantly) non-inferiority of discontinuation especially in presence of CMR.
Conclusion
Compared to morphologic imaging with CT, metabolic imaging with FDG-PET identified a greater proportion of patients with complete responses, who were associated with a low rate of relapse after treatment discontinuation. PET-CT may more accurately identify patients at risk who require closer surveillance or further treatment. Prospective studies investigating PET-based treatment discontinuation are warranted.
Availability of data and materials
Data are available on reasonable request.
References
Michielin O, van Akkooi ACJ, Ascierto PA, Dummer R, Keilholz U, clinicalguidelines@esmo.org EGCEa. Cutaneous melanoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-updagger. Ann Oncol. 2019;30(12):1884–901.
Hodi FS, Chiarion-Sileni V, Gonzalez R, Grob JJ, Rutkowski P, Cowey CL, et al. Nivolumab plus ipilimumab or nivolumab alone versus ipilimumab alone in advanced melanoma (CheckMate 067): 4-year outcomes of a multicentre, randomised, phase 3 trial. Lancet Oncol. 2018;19(11):1480–92.
Robert C, Ribas A, Schachter J, Arance A, Grob JJ, Mortier L, et al. Pembrolizumab versus ipilimumab in advanced melanoma (KEYNOTE-006): post-hoc 5-year results from an open-label, multicentre, randomised, controlled, phase 3 study. Lancet Oncol. 2019;20(9):1239–51.
Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Rutkowski P, Lao CD, et al. Five-year survival with combined nivolumab and iilimumab in advanced Melanoma. N Engl J Med. 2019;381(16):1535–46.
Ascierto PA, Long GV, Robert C, Brady B, Dutriaux C, Di Giacomo AM, et al. Survival outcomes in patients with previously untreated BRAF wild-type advanced melanoma treated with nivolumab therapy: three-year follow-up of a randomized phase 3 trial. JAMA Oncol. 2019;5(2):187–94.
Long GV, Schachter J, Arance A, Grob J-J, Mortier L, Daud A, et al. Long-term survival from pembrolizumab (pembro) completion and pembro retreatment: Phase III KEYNOTE-006 in advanced melanoma. J Clin Oncol. 2020;38(15_suppl):10013.
Robert C, Marabelle A, Herrscher H, Caramella C, Rouby P, Fizazi K, et al. Immunotherapy discontinuation - how, and when? data from melanoma as a paradigm. Nat Rev Clin Oncol. 2020;17(11):707–15.
Marron TU, Ryan AE, Reddy SM, Kaczanowska S, Younis RH, Thakkar D, et al. Considerations for treatment duration in responders to immune checkpoint inhibitors. J Immunother Cancer. 2021;9(3):e001901.
Boellaard R, Delgado-Bolton R, Oyen WJ, Giammarile F, Tatsch K, Eschner W, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42(2):328–54.
Forschner A, Battke F, Hadaschik D, Schulze M, Weissgraeber S, Han CT, et al. Tumor mutation burden and circulating tumor DNA in combined CTLA-4 and PD-1 antibody therapy in metastatic melanoma - results of a prospective biomarker study. J Immunother Cancer. 2019;7(1):180.
Lipson EJ, Velculescu VE, Pritchard TS, Sausen M, Pardoll DM, Topalian SL, et al. Circulating tumor DNA analysis as a real-time method for monitoring tumor burden in melanoma patients undergoing treatment with immune checkpoint blockade. J Immunother Cancer. 2014;2(1):42.
Boyer M, Cayrefourcq L, Dereure O, Meunier L, Becquart O, Alix-Panabieres C. Clinical relevance of liquid biopsy in melanoma and merkel cell carcinoma. Cancers (Basel). 2020;12(4):960.
Provencio M, Nadal E, Insa A, Garcia-Campelo MR, Casal-Rubio J, Domine M, et al. Neoadjuvant chemotherapy and nivolumab in resectable non-small-cell lung cancer (NADIM): an open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol. 2020;21(11):1413–22.
Xing Y, Bronstein Y, Ross MI, Askew RL, Lee JE, Gershenwald JE, et al. Contemporary diagnostic imaging modalities for the staging and surveillance of melanoma patients: a meta-analysis. J Natl Cancer Inst. 2011;103(2):129–42.
Iravani A, Osman MM, Weppler AM, Wallace R, Galligan A, Lasocki A, et al. FDG PET/CT for tumoral and systemic immune response monitoring of advanced melanoma during first-line combination ipilimumab and nivolumab treatment. Eur J Nucl Med Mol Imaging. 2020;47(12):2776–86.
Ito K, Teng R, Schoder H, Humm JL, Ni A, Michaud L, et al. (18)F-FDG PET/CT for monitoring of ipilimumab therapy in patients with metastatic melanoma. J Nucl Med. 2019;60(3):335–41.
Cho SY, Lipson EJ, Im HJ, Rowe SP, Gonzalez EM, Blackford A, et al. Prediction of response to immune checkpoint inhibitor therapy using early-time-point (18)F-FDG PET/CT imaging in patients with advanced melanoma. J Nucl Med. 2017;58(9):1421–8.
Kong BY, Menzies AM, Saunders CA, Liniker E, Ramanujam S, Guminski A, et al. Residual FDG-PET metabolic activity in metastatic melanoma patients with prolonged response to anti-PD-1 therapy. Pigment Cell Melanoma Res. 2016;29(5):572–7.
Schank TE, Forschner A, Sachse MM, Dimitrakopoulou-Strauss A, Sachpekidis C, Stenzinger A, et al. Complete metabolic response in FDG-PET-CT scan before discontinuation of immune checkpoint inhibitors correlates with long progression-free survival. Cancers (Basel). 2021;13(11):2616.
Tan AC, Emmett L, Lo S, Liu V, Kapoor R, Carlino MS, et al. FDG-PET response and outcome from anti-PD-1 therapy in metastatic melanoma. Ann Oncol. 2018;29(10):2115–20.
Acknowledgements
None
Funding
Open Access funding enabled and organized by Projekt DEAL. JF has received a Junior Clinician Scientist Stipend granted by the University Duisburg-Essen. Part of this work was funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) – SCHA 422/17–1 (KFO 337). Part of this work was funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation, RTG 2535, Knowledge- and data-driven personalization of medicine at the point of care).
Author information
Authors and Affiliations
Contributions
JF and AZ were responsible for data acquisition. JF, AZ, LZ, EL and WPF were responsible for study design, wrote the first version of the manuscript and performed data analysis. JF, LUM, and WPF interpreted imaging data. All authors contributed to the writing and approval of the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This analysis was approved by the local ethics committee (Reference: 20–9433-BO).
Consent for publication
Not required
Competing interests
JF has received fees from Eisai, outside of the submitted work. AZ received travel support from Novartis, Sanofi Genzyme, and Bristol-Myers Squibb, outside the submitted work. LZ received honoraria from Roche, BMS, MSD, Novartis, Pierre Fabre; Consultant or Advisory Role: BMS, Novartis, Pierre Fabre, Sunpharma, Sanofi, MSD; Research funding to institution: Novartis; Travel support: BMS, Pierre Fabre, Sanofi, Amgen, Novartis, Sunpharma. LU reports Speaker for Bayer Healthcare; Speaker and Research Grant Siemens Healtcare outside of the submitted work. VG reports grants, personal fees and non-financial support from Astra Zeneca, Bristol-Myers Squibb, MSD Sharp & Dohme, Ipsen, Pfizer. Personal fees from Merck Serono, EUSAPharm, Novartis, Eisai, Bayer, Roche, Janssen-Cilag, Lilly and PharmaMar. SU declares research support from Bristol Myers Squibb and Merck Serono; speakers and advisory board honoraria from Bristol Myers Squibb, Merck Sharp & Dohme, Merck Serono, Novartis and Roche, and travel support from Bristol Myers Squibb, and Merck Sharp & Dohme. EC received travel support from Bristol-Myers Squibb, Merck Sharp & Dohme, and Novartis, outside the submitted work. DS reports personal fees and non-financial support from Roche/Genentech, grants, personal fees, non-financial support and other from BMS, personal fees from Merck Sharp & Dohme, personal fees and non-financial support from Merck Serono, grant, personal fees and non-financial support from Amgen, personal fees from Immunocore, personal fees from Incyte, personal fees from 4SC, personal fees from Pierre Fabre, personal fees and non-financial support from Sanofi/Regeneron, personal fees from Array BioPharma, personal fees from Pfizer, personal fees from Philogen, personal fees from Regeneron, personal fees from Nektar, personal fees from Sandoz, grants, personal fees and non-financial support from Novartis, personal fees and non-financial support from SunPharma, Replimune, Helsinn, OncoSec and InFlaRx outside the submitted work. WPF is a consultant for BTG, and he received fees from RadioMedix, Bayer, and Parexel outside of the submitted work. EL served as consultant and/or has received honoraria from Amgen, Bristol-Myers Squibb, Merck Sharp & Dohme, Novartis, Medac, Sanofi, Sunpharma and travel support from Amgen, Merck Sharp & Dohme, Bristol-Myers Squibb, Pierre Fabre, Sunpharma and Novartis, outside the submitted work. All others have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1.
Type and frequency of G3/G4 toxicity.
Additional file 2: Table 2.
Relative risk of Progression within 12 months after discontinuation.
Additional file 3: Table 3.
Outcomes of patients with relapse.
Additional file 4: Table 4.
Response by reason of discontinuation.
Additional file 5: Figure 1.
Overall survival from therapy start.
Additional file 6: Figure 2.
Comparison of CT- and PET-imaging responses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ferdinandus, J., Zaremba, A., Zimmer, L. et al. Metabolic imaging with FDG-PET and time to progression in patients discontinuing immune-checkpoint inhibition for metastatic melanoma. Cancer Imaging 22, 11 (2022). https://doi.org/10.1186/s40644-022-00449-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40644-022-00449-3