Abstract
Background
Despite cognitive deficits frequently represent the first clinical manifestations of Progressive Multifocal Leukoencephalopathy (PML) in Natalizumab-treated MS patients, the importance of cognitive deficits in PML diagnosis is still under-investigated. The aim of the current study is to investigate the cognitive deficits at PML diagnosis in a group of Italian patients with PML.
Methods
Thirty-four PML patients were included in the study. The demographic and clinical data, the lesion load and localization, and the longitudinal clinical course was compared between patients with (n = 13) and without (n = 15) cognitive deficit upon PML suspicion (the remaining six patients were asymptomatic). Clinical presentation of cognitive symptoms was described in detail.
Result
After symptoms detection, the time to diagnosis resulted to be shorter for patients presenting with cognitive than for patients with non cognitive onset (p = 0.03). Within patients with cognitive onset, six patients were presenting with language and/or reading difficulties (46.15%); five patients with memory difficulties (38.4%); three patients with apraxia (23.1%); two patients with disorientation (15.3%); two patients with neglect (15.3%); one patients with object agnosia (7.7%), one patient with perseveration (7.7%) and one patient with dementia (7.7%). Frontal lesions were less frequent (p = 0.03), whereas temporal lesions were slightly more frequent (p = 0.06) in patients with cognitive deficits. The longitudinal PML course seemed to be more severe in cognitive than in non cognitive patients (F = 2.73, p = 0.03), but differences disappeared (F = 1.24, p = 0.29) when balancing for the incidence of immune reconstitution syndrome and for other treatments for PML (steroids, plasma exchange (PLEX) and other therapies (Mefloquine, Mirtazapine, Maraviroc).
Conclusion
Cognitive deficits at PML onset manifest with symptoms which are absolutely rare in MS. Their appearance in MS patients should strongly suggest PML. Clinicians should be sensitive to the importance of formal neuropsychological evaluation, with particular focus on executive function, which are not easily detected without a formal assessment.
Similar content being viewed by others
Background
Progressive multifocal leukoencephalopathy (PML) is an uncommon brain disease emerging in the setting of immune deficiency [1], caused by the reactivation of the John Cunningham virus (JCV) in the brain. Despite widely studied in HIV patients [1], in the last decade PML has also been observed in Multiple Sclerosis (MS) patients treated with Natalizumab (NTZ) [2]. Critically, the infection is present in the brain before the occurrence of the first clinical symptoms [3, 4], thus a delay in PML recognition and Natalizumab cessation can often occur. Furthermore, due to the relative lack of specificity in PML related neurological symptoms, the occurrence of new focal deficits can be misinterpreted as a MS relapse. As rapid immune reconstitution by removal of Natalizumab appears to determine prognosis, early diagnosis is mandatory [5].
Focal neurological syndromes as well as neuropsychological deficits are described as presenting symptoms in PML [3, 6, 7], but the prevalence of specific cognitive disorders as distinctive signs of PML in differential diagnosis with other MS related cognitive impairments has not been yet clarified. Dong-Si et al. [8] described 372 PML patients, who experienced during the course of PML cognitive/behavioral or speech symptoms in 75.5% of the cases. However, these data refer to a later stage of the PML course. In Clifford et al. [6] series, 57.1% of the patients showed cognitive, behavioral or speech symptoms at PML onset, but no specifications about the nature of cognitive deficits were provided by the authors. Finally, Hoepner et al. [7] showed that, although only half of the patients with PML complained of cognitive deficits, all of them demonstrated neuropsychological impairment at formal evaluation, suggesting a higher prevalence of cognitive impairment than what was subjectively reported. However, the authors did not consider aphasia as a cognitive deficit, and described only 8 PML patients, thus limiting the generalizability of the results. Hence, the importance of cognitive deficits in PML diagnosis is still underinvestigated.
The current paper describes the neuropsychological symptoms at onset and the longitudinal clinical course of a group of Italian MS patients treated with Natalizumab, who experienced PML, with the aim to better identify the possible peculiar aspects of PML related cognitive symptoms. The current study includes 34 Natalizumab treated MS patients who developed PML between 2009 and 2015 and were retrospectively collected from 25 Italian MS sites. Firstly, the whole sample has been analyzed. Secondly, we focused on patients presenting with cognitive deficits and compared their demographic and clinical features with those ones of patients presenting with other symptoms at PML diagnosis. Moreover, for patients with cognitive symptoms at onset, we considered the type of neuropsychological deficits reported the possible anatomo-clinical correlation between lesion location and the neuropsychological deficit.
Methods
Patients inclusion
An Italian, independent spontaneous collaborative repository initiative made a registry for the collection of patients with MS treated with NTZ who developed possible or definite PML according to the American Academy of Neurology criteria [8], as described in detail elsewhere [9]. In the current paper, the data from 25 Italian MS Centers, which took part to the initiative were included, resulting in 34 PML patients who received diagnosis of definite PML between 2009 and June 2015. To our knowledge, one NTZ-PML italian patient with was not included in the registry since he/she denied his consent for data sharing.
In each Center patients were regularly followed-up, and their data were retrospectively collected from members of the Italian PML group, were included in a centralized database and were stored by the MS centre of Montichiari (Brescia). The retrospective analysis of patients’ data was approved by the ethical committee of the Spedali Civili of Brescia and was conducted in accordance with specific national laws and the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Data collection
A detailed description of the data collected is present elsewhere [9]. Here, we only describe the data relevant for the current paper, extracted from patient charts.
Demographic data included: gender; age at NTZ start; age at PML diagnosis.
Clinical data included: disease duration (years); previous immune suppression; total number of NTZ infusions; annual relapse rate (ARR) in the year before NTZ start and during NTZ treatment; symptomatic or asymptomatic PML (i.e. detection of PML lesions at brain MRI scan in presence or absence of new signs or symptoms respectively); number of JCV-DNA copies detected with quantitative polymerase chain reaction performed on cerebrospinal fluid sample at PML suspect; clinical symptom (if any) manifested at PML suspect; diagnosis delay, defined as days elapsed between the day when the treating neurologist become aware of the symptomatology and the day in which cerebrospinal fluid was sampled for JCV search; whether or not a neuropsychological (NPS) formal assessment has been performed; longitudinal Expanded Disability Status scores (EDSS [10]) collected at NTZ start (hereafter referred as baseline), at PML diagnosis (M0), at 2 months (M2), 6 months (M6) and 12 months (M12) from PML diagnosis; whether or not patients were treated with steroids, plasma exchange (PLEX) and other therapies (Mefloquine, Mirtazapine, Maraviroc).
Magnetic resonance images (MRI) data included: lesion patterns classified as unilobar (confined to one lobe), multilobar (involving two or more contiguous lobes), widespread (involving two or more non-contiguous lobes and/or present in both hemispheres) [11] and infratentorial [9]; lesion localization; presence or absence of the radiological features of immune reconstitution inflammatory syndrome (IRIS) as defined in Prosperini et al. [9].
Statistical analysis
First, we present the data of the whole sample (n = 34). Secondly, we compared patients with and without cognitive onset.
Categorical variables are expressed as count (percentage) and continuous variables as mean (SD) or median (range), as appropriated. Between-group differences were tested using the Chi-squared or the U Mann-Whitney test/ two independent sample t-tests for categorical and continuous variables, respectively.
The EDSS scores distribution at all time intervals were not different from a normal distribution (Kolmogorov-Smirnov tests, all ps > .20). A repeated measures (RM) ANOVA with Group (two levels: Cognitive; no Cognitive) as between subjects variable and Time (5 levels: NTZ beginning; Baseline; M2; M6; M12) as within subjects variable was used in order to compare the longitudinal clinical course of patient with or without cognitive deficits. Plasma exchange, therapy with steroids and other therapies (i.e. Mirtazapine, Mefloquine, Maraviroc) were included in the model as covariates, in order to remove their effects from the results. Newmann-Keuls post hoc test was used when necessary.
Results
Whole group analysis (n = 34)
Socio-demographic and clinical data
The 34 patients consisted in ten males and 24 females, with a mean age of 41.7 ± 9.3 years. The mean EDSS at PML diagnosis is 4.9 ± 2.0. The mean number of infusions of NTZ before PML onset was 36.94 ± 17.0 (range 11–78). Annualized Relapse Rate resulted significantly lower in the NTZ treatment interval than in the pre NTZ period (0.13 vs. 1.76, respectively, t = 9.76, df = 66, p < 0.001), confirming NTZ efficacy in reducing the progression of the MS disease in terms of relapses. The mean time elapsed between the symptoms onset and the PML diagnosis was 50.2 ± 31.4 days. The mean number of viral copies in the whole sample was 1750 ± 4682 copies/mL, ranging from 10 to 5174 copies/mL with an outlier patient with 26300 viral copies/mL. IRIS emerged in 24 out of 34 patients (70.5%). The survival rate was 91%: at one-year follow up 31 out of 34 patients were still alive. One patient died within the first 6 months from PML onset due to the complication of acute acalculous cholecystitis, while two patients died within 1 year from PML onset due to IRIS complications. All of them were symptomatic at PML onset. Twenty-three out of 34 (67.6%) of PML patients developed IRIS.
Lesion load and localization at PML onset
the MRI scan was available for 31 out of 34 patients. For the three remaining patients, the MRI scan was acquired but images were not available and information were obtained from the neuroradiologist’ s report. Thirteen (38.2%) patients had a unilobar lesion at PML onset; 9 (26.4%) had multilobar lesions; 6 (17.6%) had widespread lesions and 6 (17.6%) had infratentorial lesion (cerebellum or brainstem). Within the encephalic lesions (i.e. excluding the brainstem lesions, n = 28), occipital lesions were present in six patients (21.4%), temporal lesions in 12 patients (42.8%), parietal lesions in 11 patients (39.2%), frontal lesions in 17 patients (60.7%) and diencephalic lesions in three patients (10.7%). Thus, frontal lesions were preminent within this cohort of patients.
Clinical presentation of PML
Six patients (17.6%) were asymptomatic, while 28 (82.3%) manifested ≥1 symptom. Within this group, ten patients (35.7%) presented with pure cognitive symptoms; three patients (10.7%) with cognitive and motor symptoms; six patients (21.42%) with pure motor symptoms; three patients (10.7%) with symptoms indicative of brainstem involvement; two patients (7.14%) with both motor and brainstem symptoms; two patients (7.14%) with epilepsy; one patient (3.5%) with visual loss and one patient (3.5%) with hallucination.
Longitudinal clinical course
The RM ANOVA on longitudinal EDSS scores revealed a main effect of the variable Time (F[4132] = 25.25, p < 0.001). Post hoc tests highlight an EDSS worsening between NTZ beginning (mean:3.89) and PML onset (4.98, p < 0.001), which is likely to reflect PML insurgence. EDSS at NTZ beginning is also better than EDSS at the following observations (all ps < 0.001). EDSS at PML diagnosis (4.98) better than EDSS at M2 (5.94, p < 0.001), M6 (6.39, p < 0.001) and M12 (6.04, p < 0.001), while no difference between M2, M6 and M12 emerged (all ps > 0.21).
Patients with cognitive symptoms at PML onset (n = 13)
Socio-demographic and clinical data
Table 1 presents the comparison between the demographic and clinical features of PML patients who had a cognitive symptom at onset (n = 13) and the remaining patients with a symptomatic onset without cognitive symptoms (n = 15). The two groups do not differ in any of clinical and demographic features considered but gender. IRIS, though not significantly, appears to be more frequent in patients with cognitive onset (p = 0.077). Plasma Exchange (PLEX) results to be slightly more frequently administered in patients with cognitive onset (p = 0.077). Two patients within the cognitive onset and one patients within the non cognitive onset group died.
Of note, the time elapsed between the symptoms onset and the PML diagnosis significantly differs between patients with cognitive onset and patients with non cognitive onset, being significantly shorter for patients with cognitive onset (27.5 ± 27.2 days) than for patients with non cognitive onset (56.6 ± 39.7, two independent t test = 2.24, df = 26, p = 0.03).
Lesion load and localization at PML onset
MRI scan was available for 12 out of 13 patients. For the remaining patient, MRI was acquired but images were not available and information were obtained from the neuroradiologist’ s report. Four (30.6%) patients had a unilobar lesion at PML onset; 5 (38.4%) had multilobar lesions; 3 (23.0%) had widespread lesions and 1 (7.6%) had infratentorial lesion (cerebellum). Within the supratentorial lesions, occipital lesions were present in four patients (33.3%), temporal lesions in nine patients (75%), parietal lesions in six patients (50%), frontal lesions in three patients (25.0%) and diencephalic lesions in one patient (8.3%). Interestingly, frontal lesions were hypo-represented in patients with cognitive onset compared with the whole cohort (25.0% vs 60.7%, chi square = 4.28, p = 0.03), whereas temporal lesions were hyper-represented within patients with cognitive onset (42.8% vs 75%, chi square = 3.48, p = 0.06). Lesions are shown in Fig. 1.
For each patient with cognitive onset is represented the lesion localization and the presenting symptom. The MRI images are available for 12 out of 13 patients. The data of the last patient, reported in Table 2, was derived from the neuroradiologist’s report
Clinical presentation of cognitive PML
Table 2 shows the PML lesion site at MRI, the type of neuropsychological deficits manifested and/or complained by the patients, the possible anatomo clinical correlation between the lesion site and the cognitive deficit. Six patients (46.15%) presented language and/or reading difficulties (from mild anomia to severe aphasia); five patients (38.4%) memory difficulties; three (23.1%) patients apraxia; two patients (15.3%) disorientation; two patients (15.3%) neglect; one patients (7.7%) object agnosia, one patient (7.7%) perseveration and one patient (7.7%) dementia. An at least partial anatomo-clinical correlation was present in 12/13 patients. Moreover, in the table was also specified how the symptoms were detected. Formal neuropsychological (NPS) assessment has been conducted in 10 out of 13 patients (76.9%). In five out of ten of these cases we were provided with the NPS tests performed (reported in Table 2), whereas in the remaining five cases, only a clinical description of the cognitive deficits manifested by patients was available. In particular, NPS assessment was performed in seven cases (53.84%) because of patient’s complaint, in one case (7.7%) upon observation of neuropsychological symptoms during the neurological examination, whereas in two patients (15.3%) the deficits were found during their routing monitoring.. In the remaining three cases, NPS deficit was diagnosed basing on patient complaint only (one case), evidence of the deficit during neurological examination only (one case) and both patient’s complain and evidence during neurological examination (one case).
Longitudinal clinical course
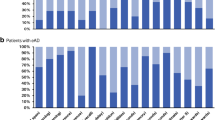
The longitudinal clinical course in terms of disability of patients with and without cognitive symptoms at onset is shown in Fig. 2. The RM ANOVA on longitudinal EDSS scores revealed a significant Group x Time interaction (F[4104] = 2.73, p = 0.03). Post hoc tests highlight different clinical course in the two groups. Indeed, in patients without cognitive impairment at PML onset, the EDSS at NTZ beginning (mean 4.36) is slightly better than the EDSS at PML diagnosis (5.4, p = 0.06), and is better than the EDSS at M2 (5.83, p = 0.009), M6 (6.36, p < 0.001) and M12 (5.93, p = 0.008). However, EDSS at PML diagnosis do not differ from EDSS at all the following observations (all ps > 0.15) and no differences in EDSS between M2, M6 and M12 emerged (ps > 0.34). On the contrary, in patients with cognitive impairment at PML diagnosis, EDSS at NTZ beginning (mean 3.92) is better than EDSS at PML diagnosis (5.3, p = 0.009), M2 (6.9, p < 0.001), M6 (7.3, p < 0.001) and M12 (7.11, p < 0.001). Statistical worsening also emerged between EDSS at PML diagnosis at EDSS at M2 (p = 0.008), M6 (p < 0.001) and M12 (p = 0.002). No differences in EDSS between M2, M6 and M12 emerged (ps > 0.55).
The RM ANOVA was repeated using gender, IRIS insurgence and PLEX as covariates, in order to remove their effects on the results. Including these covariates into the ANOVA, the ANOVA is no more significant (F[4,92] = 1.24, p = 0.29), i.e. no differences in EDSS between patients with and patients without cognitive onset was found.
Discussion
Despite the high prevalence of cognitive deficit at PML diagnosis, their importance on the clinical point of view and their diagnostic relevance has often been neglected. In the present observational study, we aimed at describing the main features of patients presenting with cognitive symptoms, in order to underline the possible identification of specific symptoms as red flag for PML, and to compare their clinical course with that oneof patients presenting with different symptoms at PML diagnosis. The current paper provides several interesting findings, namely, the prevalence and type of cognitive deficit in our population, the time-to-diagnosis of PML; the PML lesion localization and the anatomo-clinical correlation.
13 out of 34 (38.2%) MS patients with Natalizumab associated PML were presenting with cognitive deficit as a suggestive symptom of PML onset. This percentage is lower than the one reported by Clifford et al. [6], who showed a percentage of 57.1% of cognitive onset, although without any specification of the nature of cognitive deficits. On the other hand, in our sample, though limited, the symptoms were carefully described at individual level and reported mainly as disorders in memory, attention, neglect, reading, calculation, naming or orientation. Unfortunately, neuropsychological tests were available for a minority of patients and the performed test widely differed across patients, thus preventing a better analysis and interpretation of neuropsychological tests scores.
Another interesting finding is that the aforementioned cognitive deficits are not peculiar of MS patients’ cognitive impairment. Indeed, typical cognitive impairment in MS is described as a general cognitive slowdown and mainly involves information processing speed, attention, working memory and executive functions [12, 13], which are likely to worsen with the disease evolution [14], typically sparing language and orientation. Furthermore, neglect, acalculia, apraxia agraphia are notably not peculiar of MS patients. Since these symptoms are absolutely rare in MS, their appearance in MS patients treated with NTZ should be considered as a red flag and should give rise to a suspicion of PML, thus prompting a rapid MR scan. Indeed, evidences are now available regarding the positive effects of NTZ on cognitive deterioration of MS patients over long follow ups, as well as on cognitive improvement of MS patients treated with NTZ over time [15–21]. Furthermore, a rebound of cognitive impairment has also been described following natalizumab discontinuation [22]. For these reasons, any new cognitive symptom emerging during treatment with Natalizumab should alert the treating neurologist to consider a potential sign of PML.
Another interesting finding is that amongst the 28 symptomatic PML cases, we observed a shorter time to diagnosis in patients presenting with cognitive symptoms than in those ones presenting with other symptoms. We may speculate that cognitive and behavioral changes, differently from new or worsening motor symptoms, alerted clinicians toward a possible PML diagnosis. Similarly to newly appearing MRI lesions in NTZ treated patients, any new cognitive symptom or symptoms occurring beyond the first year of treatment should be considered with suspicion [23]. However, fluctuations of motor function, which are frequent in patients with MS and sometimes misinterpreted as MS relapses, could have delayed PML diagnosis [24]. Literature data report that another diagnosis is considered before PML in nearly two-thirds of PML patients, and that more than three-quarters of PML patients suffered from diagnostic delay, irrespective of their underlying immunosuppressive condition [25].
As we reported shorter time to diagnosis in patients with cognitive presentation compared to those without cognitive presentation, consequently smallest lesion size, less viral copies and presumably better prognosis would be expected in the cognitive onset sample of patients, which was not the case. The possible interpretation of this mismatch is that, in our opinion, cognitive deficits’ identification really occurred late in its course, maybe due to the lack of a careful neuropsychological investigation and assessment in the majority of the patients. This may have caused a delay in the “red flag” recognition by the neurologists and, as a consequence, larger lesions, more viral copies and worse prognosis in patients with cognitive presentation. What is worth noting is the need of sensitizing both physicians and patients toward the appearance/worsening of cognitive deficit, that might be also subtle and difficult for the patients to understand and describe, and for the neurologist to detect, in particular if related to the frontal lobe.
Furthermore, lesion analysis in PML patients with cognitive onset revealed that the anatomo-clinical correlation was present in the large majority of cases, even when the lesion size was small; thus giving strength to the clinical diagnosis of such cognitive deficit. Similarly to Richert et al. [11], we also found in the whole PML group of patients a prevalence of frontal lesions at PML onset; on the other hand, considering PML patients with cognitive symptom at onset only, a prevalence in temporal lesions was found. It is possible that some cognitive signs of prefrontal involvement could have been under-diagnosed by clinicians: noteworthy frontal signs may be less clinically evident, particularly in the right hemisphere. It might also be possible that, for this reason, in our patients with PML without cognitive symptoms at onset, and even in the asymptomatic one, some peculiar neuropsychological deficits would have been present and not clinically detected.
Finally, a careful neuropsychological examination in MS patients assuming NTZ should be regularly performed, including not only tests measuring attention, information processing speed and memory, but also executive functions, language, visual exploration and scales assessing a possible behavioral abnormalities. This could reveal early cognitive deficits suggestive of PML and allow the neurologist to quickly obtain MR scans, CSF sampling for JCV searching and withdrawing natalizumab if a strong suspicion of PML is present. It is worth noting that formal neuropsychological evaluation with appropriate tests would not only allow an accurate measure of cognitive deficits, but also its repetition over follow up would be able to monitor the evolution of these deficits over time.
Conclusions
Cognitive deficits at PML onset present with symptoms that are absolutely rare in MS, such as apraxia, aphasia, neglect, disorientation. Their appearance should strongly suggest PML. Clinicians should be sensitized about the importance of formal neuropsychological evaluation, with particular focus on executive function, which are not easily detected without a formal assessment. Patients should be sensitized as well to tell the doctor every, even small, change in their clinical status.
Abbreviations
- ARR:
-
Annualized relapse rate
- EDSS:
-
Expanded disability status score
- IRIS:
-
Immune reconstitution inflammatory syndrome
- JCV:
-
John Cunningham virus
- M12:
-
Observation at twelve months from PML diagnosis
- M2:
-
Observation at two months from PML diagnosis
- M6:
-
Observation at six months from PML diagnosis
- MRI:
-
Magnetic resonance images
- MS:
-
Multiple sclerosis
- NPS:
-
Neuropsychological
- NTZ:
-
Natalizumab
- PLEX:
-
Plasma exchange
- PML:
-
Progressive multifocal leukoencephalopathy
- RM ANOVA:
-
Repeated measures analysis of variance
References
Pavlovic D, Patera AC, Nyberg F, Gerber M, Liu M, Consortium PML. Progressive multifocal leukoencephalopathy: current treatment options and future perspectives. Ther Adv Neurol Disord. 2015;8(6):255–73.
Dong-Si T, Gheuens S, Gangadharan A, Wenten M, Philip J, McIninch J, et al. Predictors of survival and functional outcomes in natalizumab-associated progressive multifocal leukoencephalopathy. J Neurovirol. 2015;21(6):637–44.
Dong-Si T, Richman S, Wattjes MP, Wenten M, Gheuens S, Philip J, et al. Outcome and survival of asymptomatic PML in natalizumab-treated MS patients. Ann Clin Transl Neurol. 2014;1(10):755–64.
Clifford DB. Neurological immune reconstitution inflammatory response: riding the tide of immune recovery. Curr Opin Neurol. 2015;28(3):295–301.
Vermersch P, Kappos L, Gold R, Foley JF, Olsson T, Cadavid D, et al. Clinical outcomes of natalizumab-associated progressive multifocal leukoencephalopathy. Neurology. 2011;76(20):1697–704.
Clifford DB, De Luca A, DeLuca A, Simpson DM, Arendt G, Giovannoni G, et al. Natalizumab-associated progressive multifocal leukoencephalopathy in patients with multiple sclerosis: lessons from 28 cases. Lancet Neurol. 2010;9(4):438–46.
Hoepner R, Klotz P, Faissner S, Schneider R, Kinner M, Prehn C, et al. Neuropsychological impairment in natalizumab-associated progressive multifocal leukoencephalopathy: implications for early diagnosis. J Neurol Neurosurg Psychiatry. 2016;87(2):224–6
Berger JR, Aksamit AJ, Clifford DB, Davis L, Koralnik IJ, Sejvar JJ, et al. PML diagnostic criteria: consensus statement from the AAN neuroinfectious disease section. Neurology. 2013;80(15):1430–8.
Prosperini L, De Rossi N, Scarpazza C, Moiola L, Cosottini M, Gerevini S et al. Natalizumab-related progressive multifocal leukoencephalopathy in multiple sclerosis: findings from an Italian independent registry. Plos One. 2016; 11(12):e0168376.
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33(11):1444–52.
Richert N, Bloomgren G, Cadavid D, et al. Imaging findings for PML in natalizumab-treated MS patients. Mult Scler. 2012;18((Suppl 4):27. Oral 99.
Chiaravalloti ND, DeLuca J. Cognitive impairment in multiple sclerosis. Lancet Neurol. 2008;7(12):1139–51.
Borghi M, Cavallo M, Carletto S, Ostacoli L, Zuffranieri M, Picci RL, et al. Presence and significant determinants of cognitive impairment in a large sample of patients with multiple sclerosis. PLoS One. 2013;8(7):e69820.
Borghi M, Carletto S, Ostacoli L, Scavelli F, Pia L, Pagani M, et al. Decline of neuropsychological abilities in a large sample of patients with multiple sclerosis: a two-year longitudinal study. Front Hum Neurosci. 2016;10:282.
Mattioli F, Stampatori C, Bellomi F, Capra R. Natalizumab efficacy on cognitive impairment in MS. Neurol Sci. 2011;31 Suppl 3:321–3.
Mattioli F, Stampatori C, Capra R. The effect of natalizumab on cognitive function in patients with relapsing-remitting multiple sclerosis: preliminary results of a 1-year follow-up study. Neurol Sci. 2011;32(1):83–8.
Iaffaldano P, Viterbo RG, Paolicelli D, Lucchese G, Portaccio E, Goretti B, et al. Impact of natalizumab on cognitive performances and fatigue in relapsing multiple sclerosis: a prospective, open-label, two years observational study. PLoS One. 2012;7(4):e35843.
Wilken J, Kane RL, Sullivan CL, Gudesblatt M, Lucas S, Fallis R, et al. Changes in fatigue and cognition in patients with relapsing forms of multiple sclerosis treated with natalizumab: the ENER-G study. Int J MS Care. 2013;15(3):120–8.
Portaccio E, Stromillo ML, Goretti B, Hakiki B, Giorgio A, Rossi F, et al. Natalizumab may reduce cognitive changes and brain atrophy rate in relapsing-remitting multiple sclerosis--a prospective, non-randomized pilot study. Eur J Neurol. 2013;20(6):986–90.
Kunkel A, Fischer M, Faiss J, Dähne D, Köhler W, Faiss JH. Impact of natalizumab treatment on fatigue, mood, and aspects of cognition in relapsing-remitting multiple sclerosis. Front Neurol. 2015;6:97.
Mattioli F, Stampatori C, Bellomi F, Scarpazza C, Capra R. Natalizumab significantly improves cognitive impairment over three years in MS: pattern of disability progression and preliminary MRI findings. PLoS One. 2015;10(7):e0131803.
Iaffaldano P, Viterbo RG, Trojano M. Natalizumab discontinuation is associated with a rebound of cognitive impairment in multiple sclerosis patients. J Neurol. 2016;263(8):1620–5.
Hunt D, Giovannoni G. Natalizumab-associated progressive multifocal leucoencephalopathy: a practical approach to risk profiling and monitoring. Pract Neurol. 2012;12(1):25–35.
Ytterberg C, Johansson S, Andersson M, Widén Holmqvist L, von Koch L. Variations in functioning and disability in multiple sclerosis. A two-year prospective study. J Neurol. 2008;255(7):967–73.
Miskin DP, Ngo LH, Koralnik IJ. Diagnostic delay in progressive multifocal leukoencephalopathy. Ann Clin Transl Neurol. 2016;3(5):386–91.
Acknowledgements
We would like to acknowledge all the members of the Italian PML group, who shared the data of patients. In alphabetic order: Maria Pia Amato; Carlo Alberto Artusi; Fabio Bandini; Valeria Barcella; Antonio Bertolotto; Vincenzo Bresciamorra; Marco Capobianco; Guido Cavaletti; Paola Cavalla; Diego Centonze; Marinella Clerico; Cinzia Cordioli; Giangaetano D’Aleo; Marilena de Riz; Luciano Deotto; Luca Durelli; Mario Falcini; Ernesta Ferrari; Maria Luisa Fusco; Claudio Gasperini; Angelo Ghezzi; Luigi Grimaldi; Mario Guidotti; Alice Laroni; Alessandra Lugaresi; Paola Naldi; Chiara Pane; Patrizia Perrone; Matteo Pizzorno; Carlo Pozzilli; Luca Prosperini; Monica Rezzonico; Marco Rovaris; Giuseppe Salemi; Marco Salvetti; Giuseppe Santuccio; Elio Scarpini; Edoardo Sessa; Claudio Solaro; Giulia Tabiadon; Carla Tortorella; Maria Trojano; Paola Valentino.
Funding
This studies was not funded.
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Authors’ contributions
CS: conception and design of the study, analysis and interpretation of the data; drafting a significant portion of the manuscript/figures; NDR: acquisition of the data, analysis and interpretation of the clinical data; SG: analysis and interpretation of the MRI data; LM: acquisition of the data, analysis and interpretation of the clinical data; MC: analysis and interpretation of the MRI data; RC: conception and design of the study, drafting a significant portion of the manuscript/figures. FM: conception and design of the study, drafting a significant portion of the manuscript/figures. All the authors has been involved in revising the manuscript critically for important intellectual content. All the authors read and approved the final manuscript.
Competing interests
Dr. Scarpazza declares that she have no competing interests. Dr. De Rossi received speaker honoraria from Biogen and Teva and travel grants from Biogen, Teva and Merk Serono. Dr. Moiola received honoraria for speaking or for advisory board from Sanofi-Genzyme, Biogen, Novartis and Teva. Dr. Gerevini received speaker honoraria from Biogen. Dr. Cosottini received speaker honoraria from Biogen. Dr. Capra received consulting fees from Novartis, Biogen and lecture fees and/or travel grants from Novartis, Biogen, Genzyme and Sanofi-Aventis. Dr: Mattioli received travel grants from Merck Serono and advisory board honoraria from Novartis.
Consent for publication
Not applicable since this retrospective study on data available in a national registry reported data analyzed at group level and not at individual level.
Ethics approval and consent to participate
The retrospective analysis of patients’ data was approved by the ethical committee of the Spedali Civili of Brescia and was conducted in accordance with specific national laws and the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Consent is not applicable since this is a retrospective study on data available in a national registry. In no way this study interfere with the care received by patients.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Scarpazza, C., De Rossi, N., Moiola, L. et al. The still under-investigated role of cognitive deficits in PML diagnosis. Mult Scler Demyelinating Disord 2, 1 (2017). https://doi.org/10.1186/s40893-016-0018-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40893-016-0018-7