Abstract
Background
Addressing Patient Reported Outcomes (PROs) is essential for patient-centred care, shared decision making and improved health outcomes. Value-based health care systems in New South Wales (NSW) have a growing focus on collecting and using PROs that matter most to patients to improve their healthcare outcomes. Developing oral health patient reported outcomes measures (OH-PROM) is a first step towards value-based oral health care. This paper describes the development process of an adult and child OH-PROM tool that can be piloted for NSW public dental patients.
Methods
An expert panel was assembled to undertake a systematic process of developing OH-PROMs for NSW Health. Key methodological considerations included: (1) forming an expert panel to specify the target population and context of implementation, (2) rapid literature review and environmental scan to identify existing validated OH-PROM tools for adults and children. (3) consensus gathering with the expert panel (4) consumer feedback, and (5) finalisation of the tool for electronic oral health record (eOHR) integration to establish a set of questions, that were relevant, context-appropriate, and important to oral healthcare outcomes for patients using public dental services.
Results
The panel considered a total of 59 questions from two child (15), and four adult (44) Oral Health Related Quality of Life (OHRQoL) questionnaires used to collect OH-PROMs. These questions were mapped to the four key dimensions of OHRQoL for OH-PROMs: Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact. The consensus resulted in seven questions that aligned with these four dimensions to form two new NSW OH-PROM tools: one for adults and one for children. The tools were tested with consumers for understandability and usefulness before being incorporated into the electronic oral health record system, in readiness for future pilot testing.
Conclusion
The process for developing new OH-PROMs for NSW public dental services took a pragmatic approach that combined literature appraisal, expert consensus, and consumer consultation. Future work will assess the implementation of the OH-PROM tool and test its validity for broader use as an outcome measure for value-based oral healthcare.
Similar content being viewed by others
Introduction
Globally, healthcare systems see a necessity to adopt value-based healthcare systems to deliver the best healthcare outcomes to patients in a financially sustainable way [1]. With rising healthcare demands, an aging population and an increasing burden of complex non-communicable diseases, understanding what patients and communities value most is a foundational step to more effective and efficient care [1]. Patient-reported outcome measures are a crucial way to understand the patient’s perspective and measure this in a systematic way. By understanding the patient, we shift our health system paradigms from “What is the matter with people” to “What matters to people” [1]. A recent systematic review of value-based healthcare systems internationally has highlighted the variability and lack of well-implemented PROM measures [2]. This paper has called for flexible frameworks to guide the uptake of value-based care and developing PROMs allowing for localisation and flexibility of its application to health conditions and contexts [2]. In the Australian context, the National Health Reform Agreement 2020–2025 highlighted the use of PROMs in clinical care to empower patients to be more involved in their healthcare [3]. The Australian Commission on Safety and Quality in Healthcare has defined PROMs as “any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else” [4, 5].
In the dental setting, recent systematic reviews specific for Patient Reported Outcome Measures for dental patients have identified four dimensions that are essential components of a patient’s oral health experience namely: Oral Function, Orofacial Pain, Orofacial Appearance and Psychosocial Impacts [6, 7]. These essential components should be considered when developing dental specific PROMs. The International Consortium of Health Outcomes Measurement (ICHOM) in collaboration with large public dental organisations internationally have also developed an Adult Oral Health Standard Set (AOHSS) which includes some questions that are reported directly from the patient [8]. Jurisdictions who have contributed to the consortium have also highlighted the benefits of OH- PROMs to deliver consistent, best practices, and reduce unwarranted variation to enable the quantification of value generated for the patient and system [9, 10]. The use of routinely collected and tailored PROM tools can improve patient/provider communication, ensures quality and enables the health system to measure oral health patient-driven healthcare outcomes [11,12,13].
New South Wales (NSW) Health is the public health provider for Australia’s largest state. In the NSW Health context, there is a system-wide transition to emphasise value-based healthcare with concentrated efforts to implement a broad range of generic and condition-specific PROMs adjacent to service delivery [14]. In alignment with this, NSW public dental services are also strategically moving towards a value-based oral health system. A structured and localised process to collect and use OH-PROMs in routine oral healthcare is the foundational building block to drive value-based oral health service delivery within NSW Health. This study is the first part of a broader program of work aiming to implement OH-PROMs in NSW public dental services. The aim of the first stage of the program is to develop a standardised tool for adult and child patients to record OH-PROMs within NSW public dental services.
Methods
Phases of development
The development of a standardised tool comprised multiple phases that occurred concurrently. The general phases of our work included: (1) forming an expert panel to specify the target population and context of implementation, (2) rapid literature review, (3) consensus gathering with the expert panel (4) consumer feedback, and (5) finalisation of the tool for eOHR integration.
Phase 1 Forming an expert panel to specify the target population and context
The expert panel was formed to ensure a pragmatic end-to-end design and implementation of an OH-PROM embedded into clinical practice within NSW public dental services. An expression of interest was circulated to all 15 Local Health Districts (LHDs) dental services across NSW. Six LHDs confirmed their participation. It was essential to include key stakeholders within each of the six LHDs who could lead and influence the implementation of OH-PROMs in NSW public dental services. Thus, the expert panel consisted of six dental directors/public oral health specialists, two policy officers from the Centre for Oral Health Strategy at the NSW Ministry of Health and two senior public oral health clinicians with academic affiliations. Members had varied dental clinical backgrounds including dentists, public dental health specialists, and oral health therapists.
The expert panel identified the target population and context of implementation being patients who were seeking generalist care within NSW Health public dental clinics. Public dental services in NSW are delivered across 15 Local Health Districts (LHDs) and two speciality networks. The services have over 600 dental and oral health clinicians who provide dental care across approximately 175 public dental facilities in NSW. NSW public dental services offer a range of services to children and adults who meet eligibility criteria [15]. They also have a prioritisation criterion for emergency situations, as well as for patient groups most in need and at the highest risk of dental diseases [16]. The type of dental treatment ranges from episodic emergency care to comprehensive general dental treatment and specialist care. As this PROM project was in its initial stage of the broader Value-based oral health program the expert panel determined that only patients receiving general dental treatment would be targeted.
Phase 2 Rapid evidence review
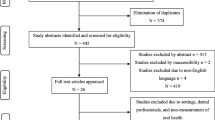
The development of the OH-PROMs process began with a rapid literature review and environmental scan of the evidence, including a search of peer-reviewed literature and grey literature (including policy documents and white papers from the policy registers like the Analysis & Policy Observatory in Australia, and National Institute for Health and Care Excellence in the UK, as well as further email communications with authors of these papers jurisdictions) to identify existing information related to OH-PROMs. The review focused on evidence specific to dental patient reported outcome measures that were published in the main electronic databases including PubMed and Medline over the last 30 years. Whilst there is a paucity of published evidence reviews on the utilisation of OH-PROMs, there were existing examples of health services in The Netherlands [17] and the US [18] that have used validated OHRQoL questionnaires to collect OH-PROMs [6, 7]. Thus, our rapid literature review also leveraged existing systematic reviews that identified OHRQoL measures that have been used for general OH-PROM collection [6]. Dimensions identified by this existing systematic review namely: Oral Function, Orofacial Pain, Orofacial Appearance and Psychosocial Impact would form part of our inclusion criteria [7]. Additionally, the Australian Commission on Safety and Quality in Health Care (ACSQHC) guided our search by identifying existing OHRQoL tools specific to oral health [4] as well as highlighting the need to consider the emerging work of the International Consortium for Health Outcome Measures’ (ICHOM) Adult Oral Health set of questions [8].
Inclusion and exclusion criteria for the literature search developed by the panel were pragmatically chosen specific to the NSW Health public dental service context of implementation (Table 1). The panel agreed that our OH-PROM should be mapped to the OHRQoL dimensions identified by previous literature [6]. The OH-PROM for public dental services also needed to be quick to administer (20 questions or less), clinically relevant and simple to understand [17]. The panel agreed that there were different nuances when developing OH-PROMS for the child (under 18 years) and adult (18 years and above), therefore the literature review was split and run in parallel for adults and children.
Phase 3 Consensus gathering with the expert panel
Once the expert panel decided on the context of implementation, they were provided an additional template to reach consensus around the (A) relevance to OHRQoL dimensions (B) consolidation of the questions and (C) comparable dimensions between the adult and child set. This template also had a list of questions from tools that fit the inclusion and exclusion criteria mapped to the OHRQoL dimensions. A parallel process to review the list of questions was conducted for the adult and child sets. All our expert panel members had worked in the fast-paced, high-demand services with public dental services that aimed to reach priority populations. This ensured relevance and practical implementation aspects were considered. We also reviewed the inclusion of these questions to fit the previously published and identified dimensions of OHRQoL [6]. The expert panel ensured that the consolidation of questions between the child and adult set also had comparable dimensions.
Phase 4 Consumer feedback
Consumer feedback was paramount for the development of OH-PROMs and is embedded in NSW Health processes for developing new patient-centred models of care [19]. Consistent with this, consumer feedback was sought from active oral health consumers from the participating LHDs. Firstly, questions were placed on the Sydney Health Literacy Lab’s Health Literacy editor, generating a grade 6 reading level, which is lower than the recommended grade 8 reading level for health literacy documents [20]. Consumers were then given a printed version of the draft OH-PROM questions and were asked about whether the questions were (1) easy to understand and (2) if they were comfortable answering the questions as well as the opportunity to provide further feedback on these measures.
Phase 5 Finalisation of the tool for eOHR integration
After consumer feedback was sought the expert panel reviewed the feedback before finalising the questions. These were then formatted into a templated questionnaire that would be embedded into the current electronic Oral Health Record (eOHR) system currently used by NSW public dental services.
Results
The results of our paper will be presented in the five phases of our work outlined in the methods section of our paper.
Phase 1 Specifying the target population context of implementation
The expert panel first discussed the context for implementation [11]. Agreement on the context and the target population guided the discussion about the specific questions and system requirements for the OH-PROMs. The agreed upon setting and process for OH-PROM collection is outlined in Table 2.
Phase 2 Results of the rapid evidence review
The rapid literature review was conducted specific to the target population and the context of implementation. The review identified two child (with a total of 15 questions), and four adult tools (with a total of 44 questions) that fit the inclusion/exclusion criteria. This included a set of questions from another Australian health jurisdiction that had applied OH-PROMs based on the ICHOM measures [8]. The working group mapped each of these questions to the four Oral Health Related Quality of Life dimensions found in Table 3.
Phase 3 Consensus gathering with the expert panel
Relevance of the questions
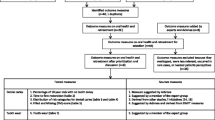
Of the initial 44 adult questions considered by the expert panel (Fig. 1) 39 questions were mapped and considered relevant to an OHRQoL dimension. Five questions were removed from the ICHOM Adult Oral Health Standard Set (AOHSS) [8], as they were findings that were reported by clinicians. This did not fit the Australian Commission on Safety and Quality in Healthcare’s definition of a PROM, which is stated as “a report of the patient’s conditions that comes directly from the patient” [4, 5]. Of the 15 child questions that were presented to the group, all questions were considered relevant to the OHRQoL dimensions and fit the criteria for a OH-PROM (Fig. 2).
Consolidation of the questions
At this stage, the group focused on consolidating all the questions that addressed similar OHRQoL dimensions. Many of the 39 questions in the adult set addressed similar dimensions and were consolidated into 11 questions. For the child set, 15 questions were consolidated to six questions.
Comparable dimensions for adults and child OH-PROM tools
Ensuring comparable dimensions between child and adult OH-PROMs is crucial for establishing system-wide measures that could drive future quality improvement projects [11]. Therefore, only questions addressing similar OHRQoL dimensions were selected with a final set of six questions for each tool. The expert panel also agreed that a global oral health rating question should be included, resulting in consensus for a final set of seven questions (inclusive of the global rating question) for the adult and child tool.
Phase 4 Results of the consumer feedback
We obtained 47 anonymous responses (25 for the adult and 22 for the child set) from active oral health consumers from the participating LHDs. The feedback on whether each of the questions was easy to understand, showed that respondents rated 86–96% of the questions positively. When considering whether they were comfortable answering the questions, positive responses for the questions ranged from 88 to 98%. The only feedback from consumers regarding the wording of the questions related to the ambiguity of the term “usual activities”. In response to this, the expert panel revised the term “usual activities” to “daily activities” resulting in the following question “Because of the condition of your mouth, teeth and gums how often do you have difficulty doing daily activities?”. Some consumers also sought clarity about whether questions like “Because of the condition of your mouth, teeth and gums do you feel embarrassed?” related specifically to the patient’s oral health or were also inclusive of their general health conditions. This feedback informed implementation strategies including training materials focused on how staff could ask these questions specific to the oral health condition of the patient. After considering consumer feedback, the expert panel finalised the two sets of questions (Tables 4 and 5).
Phase 5 Finalisation and eOHR integration
In the next stage, the two finalised OH-PROM tools were built into the eOHR as electronic forms (eForms). The eForms incorporated fields to also record variability in the way the OH-PROMs were completed, e.g., whether the OH-PROM was completed by the patient in the waiting room or by direct interview with the dental clinician. For the child PROMs, our eForm also recorded who was answering the questions for the child OH-PROMs, i.e., the child, their parents/carers, or others. This was considered important for future analysis of the implementation process.
Discussion
Internationally, the recent shifts towards value-based oral health care have highlighted the importance of systematically using PROMs to ensure that the patient voice remains core to oral health service delivery. This has prompted many health systems internationally and in Australia to consider integrating dental PROMs into oral health clinical service delivery. An essential component of developing PROMs is to seek consumer input at the onset of development in a meaningful way [25]. However, there is paucity in the literature about how this can be pragmatically applied to larger public oral health contexts. Our paper aims to share the methods and pragmatic lens that large multi-site public health service units have undertaken to develop OH-PROMs. By engaging key clinical experts and ensuring shared decision making our process bridges the implementation gaps; thus expediting the translation of evidence into practice. Our expert panel was able to balance the learnings from the academic literature, and a variety of settings internationally to localise the OH-PROMs tools for use in public dental services in Australia. Our paper builds on systematic reviews [6, 26, 27] and existing localised projects from the Netherlands [17], the US [6] and other jurisdictions within Australia including Victoria [28]. Our core set of seven questions for an adult and child OH-PROMs tool aligns with the four (OHRQoL) dimensions including Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact that have previously been synthesised from international sources[6, 26]. Our paper demonstrates how local input, including consumer consultation during the development of OH-PROMs ensures that the questions are understandable and appropriate to support broad implementation of OH-PROMs. The involvement of key working party members with a strong understanding of the eOHR (Titanium®) system also enabled the OH-PROMs to be embedded as an eForm, reducing barriers to implementing and scaling the project in the future [29]. Although developed for the Australian context, our methods are transferrable and bridge an implementation science gap by providing a framework for other public health organisations that run safety-net clinical services nationally and internationally seeking to integrate OH-PROMs into their service delivery.
This phase of the project demonstrates the necessary first step to enable the widespread collection and use of OH-PROM data to support clinician-patient communication and system-level data to improve patient-centred care [11, 30]. To facilitate the timely collection of OH-PROMs, our project also strategically set out structural components including the development of eForms within the centralised eOHR system used across NSW public dental services. Previous literature has indicated that a major barrier to the clinician’s engagement with the collection of PROMs often related to the lack of interoperability of the PROM collection tool with their regular electronic record database [29, 31]. Cognisant of this, the expert panel chose to integrate the OH-PROMs with the eOHR before the pilot project, to support clinician uptake by enabling the efficient collection of OH-PROMs [30].
There are some limitations with our tool as it is currently only in English. The questions may be challenging to understand for non-English speaking patients. However, these patients will have access to interpreter services within NSW public dental services who will assist them in completing the OH-PROMs. Future iterations of this tool may involve the translation to popular languages reflective of our diverse patient populations.
Our focus on pragmatic data collection directly from the patient’s perspective has also meant that we may not have the granularity compared to other tools like ICHOM’s 18 questions in the AOHSS and 14 questions in the OHIP-14. Furthermore, compared to the ICHOMs questions, the NSW OH-PROMs are all collected directly from the patient and our tool does not have any clinical questions that can only be determined by clinicians. However, as our tool is mapped to all four dimensions of OHRQoL: Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact [6], it continues to enable comparison to other OH-PROMs used in the literature [27]. This alignment to the four quality of life dimensions could support future implementation and comparison of non-dental specific PROMs broadly used across the NSW Health system [11]. This may include a comparison of dimensions to the Patient Reported Outcome Measurement Information System (PROMIS) [32]. PROMIS is a set of person-centred measures that evaluates and monitors physical, mental, and social health in adults and children [32]. Alignment to other PROMs like PROMIS used in the NSW Health system could be important for future service planning especially when these tools have been extended to include economic analysis [33].
This quality improvement project laid the foundational work to develop and describe the process for designing a set of OH-PROMs. Value-based oral health emphasises the importance of capturing the patient’s perspective on their own health outcomes, to measure improvements in receiving care. Further work is needed to develop and evaluate the implementation of the OH-PROMs tools across NSW public dental services. This will ensure the broad reliability and validity of this tool across different settings including different iterations such as the translation of the tool into different languages. Future pilot projects with robust evaluations will inform the scale-up and broad uptake of OH-PROMs in NSW public dental settings.
Conclusion
This paper details the approach to develop patient reported outcome measures for use in NSW public dental services. The development process ensured a balance between scientific rigour, expert input, and the consumers’ perspective. A comprehensive framework is being designed to evaluate and validate these OH-PROM tools to ensure system scalability, and the potential of these tools to measure quality improvement projects in alignment with value-based oral health care. Future widespread use and systematic collection of OH-PROMs provide consumers, dental practitioners and policymakers with a consistent measure of value-based oral health care.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
References
WHO (2021) From value for money to value-based health services: a twenty-first century shift. WHO policy brief. Geneva
Zanotto BS, Etges APBdS, Marcolino MAZ, Polanczyk CA (2021) Value-based healthcare initiatives in practice: a systematic review. J Healthc Manag 66(5):340–365
Commonwealth Department of Health (2020) National Health Reform Agreement (NHRA) Canberra 2020–25. Canberra
ACSQHS (2023) What are PROMs? Cited 2024. Available from https://www.safetyandquality.gov.au/our-work/indicators-measurement-and-reporting/patient-reported-outcome-measures/about-proms#:%7E:text=PROMs%20are%20questionnaires%20that%20help,to%20be%20made%20over%20time
US Food and Drug Administration (2009) Guidance for industry patient reported outcome measures: use in medical product development to support labelling. FDA, Rockville. Available from https://www.fda.gov/media/77832/download
Mittal H, John MT, Sekulić S, Theis-Mahon N, Rener-Sitar K (2019) Patient-reported outcome measures for adult dental patients: a systematic review. J Evid-Based Dent Pract 19(1):53–70
Chanthavisouk P, Pattanaik S, John MT, Paulson D (2022) Commonalities among dental patient-reported outcomes. PloS ONE 17(6):e0268750
Riordain RN, Glick M, Mashhadani SSAA, Aravamudhan K, Barrow J, Cole D et al (2021) Developing a standard set of patient-centred outcomes for adult oral health– an international, cross-disciplinary consensus. Int Dent J 71(1):40–52
Porter ME (2006) Redefining health care: creating value-based competition on results. Harvard Business Review Press, Boston, Massachusetts
Lin CE, Nguyen TM, McGrath R, Patterson A, Hall M (2023) Dental health services Victoria value-based health care principles for oral health models of care. J Public Health Dent 83(3):325–328
NSW Health Agency for Clinical Innovation (2021) Analytic principles for patient-reported outcome measures. NSW Agency for Clinical Innovation, Sydney
Greenhalgh J, Gooding K, Gibbons E, Dalkin S, Wright J, Valderas J et al (2018) How do patient reported outcome measures (PROMs) support clinician-patient communication and patient care? A realist synthesis. J Patient-Rep Outcomes 2(1):42
Douglas-de-oliveira DW, Chen KJ (2023) Patient-reported measures outcomes: modern evaluation of oral health. BMC Oral Health 23(1):498
Koff E, Lyons N (2020) Implementing value-based health care at scale: the NSW experience. Med J Australia 212(3):104–6.e1
NSW Health (2017) Eligibility of persons for public oral health care in NSW. Available from https://www1.health.nsw.gov.au/pds/Pages/doc.aspx?dn=PD2017_027
NSwW Health (2017) Priority oral health program (POHP) and waiting list management St.Leonards NSW Health. Available from https://www1.health.nsw.gov.au/pds/Pages/doc.aspx?dn=PD2017_023
Amini M, Oemrawsingh A, Verweij LM, Lingsma HF, Hazelzet JA, Eijkenaar F et al (2021) Facilitators and barriers for implementing patient-reported outcome measures in clinical care: an academic centre’s initial experience. Health Policy (Amsterdam) 125(9):1247–1255
Paulson DR, Pattanaik S, Chanthavisouk P, John MT (2021) Including the patient’s oral health perspective in evidence-based decision-making. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 64(8):959–966
NSW Ministry of Health (2021) Elevating the human experience our guide to action for patient, family, carer, volunteer and caregiver experiences (ed: Brand SP). St. Leonards
Ayre J, Bonner C, Muscat DM, Dunn AG, Harrison E, Dalmazzo J et al (2023) Multiple Automated Health Literacy Assessments of Written Health Information: development of the SHeLL (Sydney Health Literacy Lab) Health Literacy Editor v1. JMIR Form Res 7:e40645–e
Slade GD (1997) Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol 25(4):284–290
Naik A, John MT, Kohli N, Self K, Flynn P (2016) Validation of the English-language version of 5-item oral health impact profile. J Prosthodont Res 60(2):85–91
Tsakos G, Blair YI, Yusuf H, Wright W, Watt RG, Macpherson LMD (2012) Developing a new self-reported scale of oral health outcomes for 5-year-old children (SOHO-5). Health Qual Life Outcomes 10(1):62
Gherunpong S, Tsakos G, Sheiham A (2004) Developing and evaluating an oral health-related quality of life index for children; the CHILD-OIDP. Community Dent Health 21(2):161–169
Greenhalgh T, Hinton L, Finlay T, Macfarlane A, Fahy N, Clyde B et al (2019) Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot. Health Expect 22(4):785–801
Omara M, Stamm T, Bekes K (2021) Four-dimensional oral health-related quality of life impact in children: a systematic review. J Oral Rehabil 48(3):293–304
Rener-Sitar K, John MT, Truong V, Tambe S, Theis-Mahon N (2021) Nonmalignant oral disease–specific dental patient-reported outcome measures for adult patients: a systematic review. J Evid-Based Dent Pract 21(1):101529
Nguyen TM, Bridge G, Hall M, Theodore K, Lin C, Scully B et al (2023) Is value-based healthcare a strategy to achieve universal health coverage that includes oral health? An Australian case study. J Public Health Policy 44(2):310–324
Gensheimer SG, Wu AW, Snyder CF (2018) Oh, the places we’ll go: patient-reported outcomes and electronic health records. Patient 11(6):591–598
Øvretveit J, Zubkoff L, Nelson EC, Frampton S, Knudsen JL, Zimlichman E (2017) Using patient-reported outcome measurement to improve patient care. Int J Qual Health Care 29(6):874–879
Nanayakkara S, Zhou X, Spallek H (2019) Impact of big data on oral health outcomes. Oral Dis 25(5):1245–1252
Gruber-Baldini AL, Velozo C, Romero S, Shulman LM (2017) Validation of the PROMIS® measures of self-efficacy for managing chronic conditions. Qual Life Res 26(7):1915–1924
Aghdaee M, Gu Y, Sinha K, Parkinson B, Sharma R, Cutler H (2023) Mapping the patient-reported outcomes measurement information system (PROMIS-29) to EQ-5D-5L. PharmacoEconomics 41(2):187–198
Acknowledgements
We would like to acknowledge the support of executive staff at the Centre for Oral Health Strategy, NSW Ministry of Health.
Funding
None to declare.
Author information
Authors and Affiliations
Contributions
R.C. and A.Y. provided the conception to the design of the work, acquisition, analysis, and interpretation of the work drafting and reviewing the work critically for important intellectual content. S.A., provided the conception to the design of the work, acquisition and interpretation of the work drafting and reviewing the work critically for important intellectual content. B.C. provided the conception to the design of the work, and interpretation of the work drafting and reviewing the work critically for important intellectual content. C.P., R.S., J.K., contributed to the acquisition, interpretation and reviewing the work critically for important intellectual content. M.O'C., K.C., and W.S. contributed to the interpretation and reviewing the work critically for important intellectual content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This paper describes the process undertaken by public dental services in the state of New South Wales (NSW), Australia, to develop patient reported outcome measures; as an approach to improving the quality of care for patients accessing public dental services in NSW. While a methodologically rigorous development process was undertaken, this was not a research activity and as such ethics approval was not sought.
Consent for publication
No applicable, our report does not contain data from individual persons.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Albert Yaacoub: Senior lead author.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, R., Ajwani, S., Christian, B. et al. The development of a new oral health patient reported outcome measure: the New South Wales public dental services approach. J Patient Rep Outcomes 8, 98 (2024). https://doi.org/10.1186/s41687-024-00777-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41687-024-00777-x