Abstract
Background
Ninety patients American Society of Anesthesiologists (ASA) I–II, aged (18–60 years), were enrolled in this randomized controlled trial. All enrolled patients had undergone elective primary unilateral open inguinal hernia repair under spinal anesthesia; at the end of the surgery, transversus abdominis plane (TAP) block was done by bupivacaine combined with 4 mg dexamethasone in (group I), 8 mg dexamethasone in (group II), or saline in (group III.). We aimed to compare the analgesic efficacy of two different doses of dexamethasone (4 mg and 8 mg) added to bupivacaine in a unilateral single-injection (TAP) block. The first outcome measure was the time of the first analgesic request, and the secondary outcome measure was the VAS scale in the first postoperative 24 h.
Results
There was no need for any analgesia in group I and group II in the first postoperative 24 h. The time of the first analgesic request in group III was 720 ± 90 min. VAS scores were significantly lower in group I and group II than in group III, with no significant difference between group I and group II.
Conclusions
There is no difference in the first postoperative 24 h analgesic effect of the two doses of dexamethasone when added to a long-acting local anesthetic mixture in TAP blocks in patients undergoing inguinal hernia repair.
Trial registration
ClinicalTrials.gov, NCT03863977
Similar content being viewed by others
Background
Inguinal hernia repair (IHR) is one of the most common one-day surgeries (Callesen et al. 2001), it is associated with 60% of the incidence of moderate to severe postoperative pain (Beldi et al. 2008). Several methods used to reduce this pain are pharmacological methods, topical anesthetics, epidural analgesia, ilioinguinal, and iliohypogastric nerve blocks, TAP block, and non-pharmacological methods (Joshi et al. 2012; Demirci et al. 2014; Toivonen et al. 2001).
Ultrasound-guided transverses abdominis plane block (TAP block) used for postoperative analgesia following abdominal surgeries by blocking sensation to the skin, muscles of the anterior abdominal wall, and parietal peritoneum (Bajwa and Kaur 2013).
Dexamethasone is commonly used as an adjuvant to local anesthetics in TAP block to prolong the duration of the block (Ammar and Mahmoud 2012; Akkaya et al. 2014; Yildiz and Bayir 2015). Dexamethasone doses were varied in the previous studies and ranging from 4 to 8 mg and no one of them identified the ideal effective dose (Ammar and Mahmoud 2012; Akkaya et al. 2014; Yildiz and Bayir 2015; Wegner et al. 2017; Deshpande et al. 2017; Kartalov et al. 2015), so we planned this study to identify is there any difference in the postoperative analgesic effect of the two commonly used doses of dexamethasone (4 mg and 8 mg) (Chen et al. 2018), added to bupivacaine in ultrasound-guided TAP block for inguinal hernia repair.
Methods
Enrollment and eligibility
After approval from the local Medical Ethics Committee (IRB 17100670), and clinical trials registration ClinicalTrials.gov (ID NCT03863977), this randomized, double-blind clinically controlled trial was started on the 15th of March 2019 and ended in December 2019, in the department of general surgery. Ninety male patients American Society of Anesthesiologists (ASA) I or II, aged from 18 to 60 and scheduled for elective unilateral open inguinal hernia repair under spinal anesthesia, were included in this study. We got written informed consent from all patients before participation in this study. Excluded from this study any patients with known allergy to amino amide local anesthetics, skin infection, diseases at the site of injection, coagulation disorders, patients with body mass index (BMI) > 35 kg/m2 or scrotal hernias.
Randomization and blinding
An independent researcher did the randomization of ninety patients to receive unilateral TAB block by using computer-generated randomized tables. At the end of surgery after closure of the surgical wound, unilateral TAB block (at the side of the surgery) was done. To perform the block, we used the injection of either 4 mg dexamethasone added to 1 mg/kg of 0.5% bupivacaine in (group I), 8 mg dexamethasone added to 1 mg/kg of 0.5% bupivacaine (group II), or 1 mg/kg of 0.5% bupivacaine in the control group (group III); the study drugs were prepared by an independent researcher in syringes with an equal volume (25 ml) of the study solutions (studied drugs diluted with normal saline 0.9%), and he put them in coded envelopes according to the randomization order and the anesthesiologist opened the envelopes just before the injection.
Study protocol
In the preoperative visit, we described to the patients the seclude of spinal anesthesia, TAB block, and the visual analog scale (VAS) for pain description. l2.5 mg. In the operating room, insertion of peripheral IV cannula (18 or 20 gauge) to all patients to revive 20 ml/kg crystalloid fluid followed by spinal anesthesia was done, and spinal anesthesia was administered to patients at sitting position using intrathecal 12.5 mg of 0.5% bupivacaine at the level of L3-4 by 25-G spinal needle; we checked the block level and surgery started when the level established at T7, and intraoperative patients were monitored with standard monitor (ECG, pulse oximeter, and non-invasive blood pressure). At the end of the surgery, sensory and motor spinal levels were recorded; then, we did ultrasound-guided TAB block using the ultrasound probe (Sonosite Inc., Bothell, WA, USA). A high frequency (5–10 MHz) after sterilization of the skin, the probe was sheathed and placed in the midaxillary line between the lower costal margin and the iliac crest; then, we introduced a needle of 21-G, 100 mm 22 (SonoPlex Stim cannula, Pajunk®GmbH, Geisingen, Germany) medially in the plane of the ultrasound beam and directed towards the transversus abdominis plane; after the tip of the needle was at the correct position between the internal oblique muscle and transversus abdominis muscles, we injected the study drugs according to group assignment, during injection the distribution of the studied drugs observed by hypoechoic enlargement in the screen of the ultrasound. Then, all patients were transferred to PACU; in arrival at the PACU, the successes of the TAP block were examined by pinprick sensory test of the abdominal wall and the Bromage scale was used to examine the motor block (to ensure that the effect of spinal anesthesia was abolished and exclude failed block from the study).
Postoperative patients assessment
Postoperatively, we evaluated motor and sensory regression of spinal anesthesia. Visual analog scale (VAS) and demonstrated by using a ruler numbered from 0 to 10 (0 = no pain, 1–3 = mild pain, 4–6 = moderate pain, and 7–10 = severe pain) (Gao et al. 2017), and it was recorded at rest and during coughing. These were assessed on admission to PACU (baseline), and 2, 4, 6, 12, and 24 h postoperatively. If the VAS scale was more than 3, 1 g IV paracetamol was administered to the patient, and repeated after 8 h if needed. Time and total dose of analgesic consumption was recorded. We recorded also heart rate and mean arterial blood pressure before the block, and 2, 4, 6, 12, and 24 h postoperatively. Incidence of nausea and vomiting and any postoperative adverse effects were recorded.
Statistical analysis
Data entry and data analysis were done using SPSS version 22 (Statistical Package for Social Science). Data normality was tested with the Kolmogorov–Smirnov test. Data were presented as mean (standard deviation), median (range), and number. The Student t test was used for normally distributed continuous data and the Wilcoxon signed-rank test in case of nonparametric data. The chi-squared test or the Fisher exact test was used to analyze frequency variables, and ordinal variables were analyzed using the Mann-Whitney U test. A P value of < 0.05 was considered statistically significant.
Results
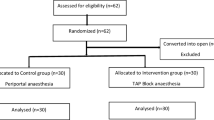
Ninety-six patients were screened for eligibility and 90 patients were involved in the study 30 patients in each group (Fig. 1).
There were no significant changes between the studied groups according to demographic data, anesthesia time, and surgical time (Table 1).
The postoperative VAS score was classified to VAS at rest and VAS at exertion (by asking the patient to cough) (Figs. 2 and 3). Postoperative VAS scores at rest were significantly lower in group I and group II than group III from 1 h postoperatively to 24 h (P value between group I and group III at rest was 0.013 at 1 h, 0.001 at 2 h, and 0 at 4h, 8 h, 16 h, and 24 h, while P value between group II and group III was 0 from 1 h to 24 h). Also, postoperative VAS scores at exertion were significantly lower in group I and group II than group III from early postoperative to 24 h (P value between group I and group III at exertion was 0.005 immediately after injection, 0.001 at 15 min, 0.032 at 30 min, 0.026 at 1 h, 0.011 at 2 h and 4 h, 0.003 at 8 h, and 0 at 16 h and 24 h, while P value between group II and group III at exertion was 0 immediately after injection and 15 min, 30 min, 1 h, 2 h, 4h, 16 h, and 24 h while was 0.001 at 8 h).VAS scores were not significantly reduced in group II than group I at rest or at exertion at any time postoperatively.
The time to first analgesic request for IV paracetamol was 720 ± 90 min in group III versus 24 h in group I and group II. No patients request for rescue analgesia in group I and group II in the first postoperative 24 h versus all patients request analgesia in group III; three patients received IV 1 g paracetamol once and 27 patients received IV paracetamol twice during the first postoperative 24 h (Table 2).
The mean blood pressure was decreased significantly in group I and group II than group III at 8 h, 16 h, and at 24 h postoperatively (P value between group I and group III was 0.024 at 8 h and 0 at 16 h and 24 h, and P value between group II and group III was 0.042 at 8 h and 0 at 16 h and 24 h), with no significant difference between groups I and II (Fig. 4).
This study reported also that the heart rate was decreased significantly in patients of group I and group II than group III at 16 h and 24 h postoperatively (P value between group I and group III was 0.005 and 0.004 at 16 h and 24 h, respectively, and P value between group II and group III was 0 at 16 h and 24 h) (Fig. 5).
Hemodynamics effects were significantly lower in dexamethasone groups than the control group and corresponded to the visual analog score but without clinical significant as there were no incidence of bradycardia (heart rate bradycardia < 60 beat/min) or hypotension (mean BP < 20% of the base line).There were no postoperative adverse effects recorded in all patients (not presented).
Discussion
In this study, we studied the postoperative analgesic effect of two doses of dexamethasone (4 mg and 8 mg added to bupivacaine in unilateral TAP block for inguinal hernia repair), and we noted that VAS scores, time to rescue analgesia, and total postoperative analgesic consumption were lower in dexamethasone groups than the control group with no difference between the two doses of dexamethasone.
Ultrasound use makes TAP block more easily in performance, very safe, with a high rate of success, and low incidence of complication (Ripollés et al. 2015; Belavy et al. 2009). Multiple previous studies noticed that TAP block reduced postoperative analgesic consumption (Gao et al. 2017; Seervi et al. 2019; Sujatha et al. 2017), but this effect has a limited duration (Moyo et al. 2016). Several adjuvants were used to prolong the duration of local anesthetics and suggested that dexamethasone is the best adjuvant to local anesthetics agents in peripheral nerve block and could be superior to clonidine, fentanyl, neostigmine, and tramadol (Yaghoobi et al. 2013; Shah et al. 2015; Yadav et al. 2008; Trabelsi et al. 2013) and has similar analgesic effect as dexmedetomidine without any adverse hemodynamic effect associated with dexmedetomidine (Lee et al. 2016; Verma and Ranjan 2016).
Efficacy of addition of dexamethasone in the TAP block studied previously (Ammar and Mahmoud 2012; Akkaya et al. 2014; Yildiz and Bayir 2015). Dexamethasone is a long-acting steroid used to prolong the duration of the effect of local anesthetics in a dose-dependent manner, and it does not have any effect if used alone without local anesthetics (Kartalov et al. 2015). This effect may be due to their anti-inflammatory or immune-suppressive actions (McCormack 1994), perineural vasoconstriction may decrease the absorption rate of local anesthetics (Wang et al. 2011; Shishido et al. 2002), direct inhibition of ectopic neural discharge (Devor et al. 1985), or through modulation of potassium channels (Pennington et al. 1994).
Similar to our results, Chen et al. (2018) and Zhang et al.’s (2019) in their meta-analysis demonstrated that dexamethasone in the TAP block improve the analgesic effect of local anesthetics in a dose ranging from 4 to 8 mg and recommended the need for further studies to identify the optimal dexamethasone dose.
The duration of analgesia depends on the dose of local anesthetics used in the block (Demirci et al. 2014) and the dose of dexamethasone. Several studies investigate the effect of dexamethasone and demonstrated different results; some results were similar to our results and recorded the duration of analgesia ranges from 20 to 24 h and others recorded duration of analgesia ranges from 12 to16 h (Ammar and Mahmoud 2012; Kartalov et al. 2015).
Deshpande et al. (2017) reported that time to first analgesic request was 13.2 ± 7.6 h when using ropivacaine 0.5% added to 4 mg dexamethasone in TAP block, Sharma et al. (2018) found time to first analgesic request was 10 h using 8 mg dexamethasone added to ropivacaine 0.5% in TAP block; similar to these studies, our result suggested the equipotent analgesic effect of 4 mg and 8 mg dexamethasone, and time to first analgesic request was prolonged up to 24 h in our study; this prolongation may be due to the use of bupivacaine. Cummings III and coworkers noticed prolonged duration of interscalene blocks when using 0.5% bupivacaine dexamethasone than 0.5% ropivacaine dexamethasone (Singh et al. 2013), as ropivacaine has lower pH than bupivacaine (Wegner et al. 2017).
In our study, there was no incidence of postoperative nausea and vomiting in all groups in contrast to our results. Chen et al.’s (2018) meta-analysis found that dexamethasone in TAP block associated with a 72% decrease in the incidence of (POVN) compared with local anesthetics alone, due to reduction in opioid consumption (Singh et al. 2013; McMorrow et al. 2011); we did not use opioid in the rescue analgesia, and this may explain the absence of postoperative nausea and vomiting in our results.
Although the use of perineural dexamethasone is still an off-label route (Choi et al. 2014), there were no observed complications in our study; similar to our results, Ma et al. (2010) suggested that dexamethasone may have a protective effect on bupivacaine-induced neuron injury in vitro by activating the Akt (threonine-serine protein kinase B) signaling pathway.
Limitation
Our observation period was limited to 24 h because patients were discharged from the hospital as a part of our surgical department protocol, so we could not assess the definite duration of analgesia of the two doses of dexamethasone, and the effect on the mobilization time, so a large study is needed with prolonged observation period. Another limitation was we did not measure the serum level to prove the local effect of dexamethasone.
Conclusion
There is no difference in the first postoperative 24 h analgesic effect of the two doses of dexamethasone when added to a long-acting local anesthetic mixture in TAP blocks in patients undergoing inguinal hernia repair.
Availability of data and materials
Confidential patient data can be asked by special request from the corresponding author.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- TAP block:
-
Transverses abdominis plane block
- IHR:
-
Inguinal hernia repair
- BMI:
-
Body mass index
- VAS:
-
Visual analog scale
- IV:
-
Intravenous
- PACU:
-
Postanesthesia care unit
- POVN:
-
Postoperative nausea and vomiting
- Akt:
-
Threonine-serine protein kinase B
References
Akkaya A, Yildiz I, Tekelioglu UY, Demirhan A, Bayir H, Ozlu T et al (2014) Dexamethasone added to levobupivacaine in ultrasound-guided tranversus abdominis plain block increased the duration of postoperative analgesia after caesarean section: a randomized, double blind, controlled trial. Eur Rev Med Pharmacol Sci 18(5):717–722
Ammar AS, Mahmoud KM (2012) Effect of adding dexamethasone to bupivacaine on transversus abdominis plane block for abdominal hysterectomy: a prospective randomized controlled trial. Saudi J Anaesth 6(3):229–233
Bajwa SJ, Kaur J (2013) Clinical profile of levobupivacaine in regional anesthesia: a systematic review. J Anaesthesiol Clin Pharmacol 29(4):530–539
Belavy D, Cowlishaw PJ, Howes M, Phillips F (2009) Ultrasound-guided transversus abdominis plane block for analgesia after Caesarean delivery. Br J Anaesth 103(5):726–730
Beldi G, Haupt N, Ipaktchi R, Wagner M, Candinas D (2008) Postoperative hypoesthesia and pain: qualitative assessment after open and laparoscopic inguinal hernia repair. Surg Endosc 22(1):129–133
Callesen T, Bech K, Kehlet H (2001) One-thousand consecutive inguinal hernia repairs under unmonitored local anesthesia. Anesth Analg 93(6):1373–1376 table of contents
Chen Q, An R, Zhou J, Yang B (2018) Clinical analgesic efficacy of dexamethasone as a local anesthetic adjuvant for transversus abdominis plane (TAP) block: a meta-analysis. PLoS One 13(6):e0198923
Choi S, Rodseth R, McCartney CJ (2014) Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: a systematic review and meta-analysis of randomized trials. Br J Anaesth 112(3):427–439
Demirci A, Efe EM, Turker G, Gurbet A, Kaya FN, Anil A et al (2014) Iliohypogastric/ilioinguinal nerve block in inguinal hernia repair for postoperative pain management: comparison of the anatomical landmark and ultrasound guided techniques. Rev Bras Anestesiol 64(5):350–356
Deshpande JP, Ghodki PS, Sardesai SP (2017) The analgesic efficacy of dexamethasone added to ropivacaine in transversus abdominis plane block for transabdominal hysterectomy under subarachnoid block. Anesth Essays Res 11(2):499–502
Devor M, Govrin-Lippmann R, Raber P (1985) Corticosteroids suppress ectopic neural discharge originating in experimental neuromas. Pain 22(2):127–137
Gao T, Zhang JJ, Xi FC, Shi JL, Lu Y, Tan SJ et al (2017) Evaluation of transversus abdominis plane (TAP) block in hernia surgery: a meta-analysis. Clin J Pain 33(4):369–375
Joshi GP, Rawal N, Kehlet H, collaboration P, Bonnet F, Camu F et al (2012) Evidence-based management of postoperative pain in adults undergoing open inguinal hernia surgery. Br J Surg 99(2):168–185
Kartalov A, Jankulovski N, Kuzmanovska B, Zdravkovska M, Shosholcheva M, Spirovska T et al (2015) Effect of adding dexamethasone as a ropivacaine adjuvant in ultrasound-guided transversus abdominis plane block for inguinal hernia repair. Pril (Makedon Akad Nauk Umet Odd Med Nauki) 36(3):35–41
Lee MJ, Koo DJ, Choi YS, Lee KC, Kim HY (2016) Dexamethasone or dexmedetomidine as local anesthetic adjuvants for ultrasound-guided axillary brachial plexus blocks with nerve stimulation. Korean J Pain 29(1):29–33
Ma R, Wang X, Lu C, Li C, Cheng Y, Ding G et al (2010) Dexamethasone attenuated bupivacaine-induced neuron injury in vitro through a threonine-serine protein kinase B-dependent mechanism. Neuroscience 167(2):329–342
McCormack K (1994) The spinal actions of nonsteroidal anti-inflammatory drugs and the dissociation between their anti-inflammatory and analgesic effects. Drugs 47(Suppl 5):28–45 discussion 6-7
McMorrow RC, Ni Mhuircheartaigh RJ, Ahmed KA, Aslani A, Ng SC, Conrick-Martin I et al (2011) Comparison of transversus abdominis plane block vs spinal morphine for pain relief after Caesarean section. Br J Anaesth 106(5):706–712
Moyo N, Madzimbamuto FD, Shumbairerwa S (2016) Adding a transversus abdominis plane block to parenteral opioid for postoperative analgesia following trans-abdominal hysterectomy in a low resource setting: a prospective, randomised, double blind, controlled study. BMC Res Notes 9:50
Pennington AJ, Kelly JS, Antoni FA (1994) Selective enhancement of an A type potassium current by dexamethasone in a corticotroph cell line. J Neuroendocrinol 6(3):305–315
Ripollés J, Mezquita SM, Abad A, Calvo J (2015) Analgesic efficacy of the ultrasound-guided blockade of the transversus abdominis plane - a systematic review. Braz J Anesthesiol (Elsevier) 65(4):255–280
Seervi SN, Singariya G, Kamal M, Kumari K, Siddeshwara A, Ujwal S (2019) Effect of addition of buprenorphine or dexamethasone to levobupivacaine on postoperative analgesia in ultrasound guided transversus abdominis plane block in patients undergoing unilateral inguinal hernia repair: a prospective randomized double blind controlled trial. Korean J Anesthesiol 72(3):245–252
Shah DM, Arora M, Trikha A, Prasad G, Sunder R, Kotwal P et al (2015) Comparison of dexamethasone and clonidine as an adjuvant to 1.5% lignocaine with adrenaline in infraclavicular brachial plexus block for upper limb surgeries. J Anaesthesiol Clin Pharmacol 31(3):354–359
Sharma UD, Prateek, Tak H (2018) Effect of addition of dexamethasone to ropivacaine on postoperative analgesia in ultrasonography-guided transversus abdominis plane block for inguinal hernia repair: a prospective, double-blind, randomised controlled trial. Indian J Anaesth 62(5):371–375
Shishido H, Kikuchi S, Heckman H, Myers RR (2002) Dexamethasone decreases blood flow in normal nerves and dorsal root ganglia. Spine (Phila Pa 1976) 27(6):581–586
Singh S, Dhir S, Marmai K, Rehou S, Silva M, Bradbury C (2013) Efficacy of ultrasound-guided transversus abdominis plane blocks for postcesarean delivery analgesia: a double-blind, dose-comparison, placebo-controlled randomized trial. Int J Obstet Anesth 22(3):188–193
Sujatha C, Zachariah M, Ranjan RV, George SK, Ramachandran TR, Pillai AR (2017) Transversus abdominis plane block versus ilioinguinal/iliohypogastric nerve block with wound infiltration for postoperative analgesia in inguinal hernia surgery: a randomized clinical trial. Anesth Essays Res 11(4):976–980
Toivonen J, Permi J, Rosenberg PH (2001) Effect of preincisional ilioinguinal and iliohypogastric nerve block on postoperative analgesic requirement in day-surgery patients undergoing herniorrhaphy under spinal anaesthesia. Acta Anaesthesiol Scand 45(5):603–607
Trabelsi W, Lebbi A, Romdhani C, Naas I, Sammoud W, Elaskri H et al (2013) Dexamethasone provides longer analgesia than tramadol when added to lidocaine after ultrasound guided supraclavicular brachial plexus block. A randomized, controlled, double blinded study. Analg Resusc 2:2
Verma NK, Ranjan A (2016) A clinical comparison of dexmedetomidine and dexamethasone as adjuvant to ropivacaine in supraclavicular brachial plexus blocks for upper arm surgeries. Int J Adv Res Biol Sci 3(7):56–61
Wang PH, Tsai CL, Lee JS, Wu KC, Cheng KI, Jou IM (2011) Effects of topical corticosteroids on the sciatic nerve: an experimental study to adduce the safety in treating carpal tunnel syndrome. J Hand Surg Eur Vol 36(3):236–243
Wegner R, Akwar D, Guzman-Reyes S, Pednekar G, Chaudhry R, Grewal N et al (2017) Evaluating the adjuvant effect of dexamethasone to ropivacaine in transversus abdominis plane block for inguinal hernia repair and spermatocelectomy: a randomized controlled trial. Pain Physician 20(5):413–418
Yadav RK, Sah BP, Kumar P, Singh SN (2008) Effectiveness of addition of neostigmine or dexamethasone to local anaesthetic in providing perioperative analgesia for brachial plexus block: a prospective, randomized, double blinded, controlled study. Kathmandu Univ Med J 6(23):302–309
Yaghoobi S, Seddighi M, Yazdi Z, Ghafouri R, Khezri MB (2013) Comparison of postoperative analgesic effect of dexamethasone and fentanyl added to lidocaine through axillary block in forearm fracture. Pain Res Treat 2013:761583
Yildiz I, Bayir H (2015) Effect of dexamethasone added to levobupivacaine used for TAP block. Hippokratia 19(3):285
Zhang D, Zhou C, Wei D, Ge L, Li Q (2019) Dexamethasone added to local anesthetics in ultrasound-guided transversus abdominis plain (TAP) block for analgesia after abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. PLoS One 14(1):e0209646
Acknowledgements
The authors are grateful to the colleagues and staff of the operating theater, the PACU, and the ward for their cooperation in data collection.
Funding
We received no funding.
Author information
Authors and Affiliations
Contributions
A.H.: This author helped in study design, data analysis, and manuscript writing and editing. E.A.: This author helped in conduct of study and manuscript writing. A.Y.: This author helped in conduct of study, data collection, and Excel sheet formation. All authors read and approved the final version of the manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
1. Local Medical Ethics Committee, Faculty of Medicine, Assiut University, Assiut, Egypt (IRB 17100670)
2. ClinicalTrials.gov registration number is NCT03863977
3. Written informed consent was taken from all the study participants.
Consent for publication
Participants accepted publication in a written consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdel-wahab, A.H., Osman, E.A. & Ahmed, A.Y. Comparison of postoperative analgesic effects of two doses of dexamethasone in ultrasound-guided transversus abdominis plane block for inguinal hernia repair: a randomized controlled trial. Ain-Shams J Anesthesiol 13, 20 (2021). https://doi.org/10.1186/s42077-021-00139-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-021-00139-5