Abstract
Background
The methylcobalamin deficiency G (cblG) disorder, a rare autosomal recessive disease, is attributed to mutations in the MTR gene, resulting in heightened homocysteine levels and reduced methionine and megaloblastic anemia levels. This disease is predominantly diagnosed using MTR gene variation analysis.
Case presentation
Herein, we report the case of a 2.1-month-old Chinese girl with the cblG disorder with poor feeding, failure to thrive, and pancytopenia, esotropia, ocular nystagmus, and hypotonia. However, in order to determine the possible genetic cause of the disease, whole-exome sequencing was adopted and detected compound-heterozygous mutations in MTR gene. One was splicing site mutation c.1812 + 3A > G and the other was missense mutation c.2405G > A (p.A802G), which were likely disease-causing mutations (DM). Variant c.1812 + 3A > G has not been reported before in the literature.
Conclusion
Our data elucidated the genetic etiology of the patient and enriched the known spectrum of mutations in the MTR gene worldwide, offering exhaustive and invaluable insights for early diagnosis and appropriate medication of the cblG disorder.
Similar content being viewed by others
Introduction
The methylcobalamin deficiency G (cblG) disorder (MIM#250940), also called methionine synthase deficiency (cblG complementation group) or homocystinuria–megaloblastic anemia (cblG complementation type), is a rare condition characterized by homocystinuria, hyperhomocysteinemia (HHcy), and hypomethioninemia. It was first described in 1988 as an autosomal recessive genetic condition caused by biallelic defects in the MTR gene [1]. Methionine synthase (MS, EC2.1.1.13), encoded by the MTR gene, catalyzes methyl transfer to convert 5-methyltetrahydrofolate (5-MTHF) to homocysteine (Hcy) [2]. This process involves transferring a methyl group from 5-MTHF to the enzyme-bound cobalamin, forming methylcobalamin. Subsequently, the methyl group is transferred from methylcobalamin to homocysteine (Met), forming Met [3]. The MS activity is crucial for maintaining adequate Met levels, preventing Hcy accumulation. Additionally, MS plays a critical role in the methylation cycle, regulating the cellular level of S-adenosylmethionine, a methyl group donor involved in various cellular processes, such as DNA and RNA methylation and neurotransmitter synthesis. MS activity deficiency affects Met and Hcy levels. It leads to the sequestration of cellular folate as 5-MTHF, which results in its inaccessibility for other folate-dependent processes, including purine and pyrimidine biosynthesis and other single-carbon-transfer-reactions [2]. When MS activity is impaired, the Hcy remethylation is hindered, resulting in Hcy accumulation in the bloodstream and subsequent HHcy. HHcy is primarily linked to neurocognitive and vascular pathology [4, 5]. Hcy and its metabolic derivative, homocysteic acid, have been implicated in the elicitation of seizures in rats [6, 7]. In addition to its impact on renal function, it has been shown to induce synergistic mitochondrial dysfunction [8, 9].
The cblG disorder impedes the remethylation of Hcy to Met, leading to HHcy. Affected patients typically exhibit non-specific clinical features in the first year of life or early childhood, including poor feeding, macrocytic anemia, pancytopenia, seizures, developmental delay, encephalopathy, ataxia, nystagmus, and hypotonia [10, 11]. To date, no more than 50 patients with the cblG disorder have been reported in the literature [11]. Therefore, the cblG disorder is a highly heterogeneous disorder with a wide spectrum of clinical manifestations, resulting in diagnosis of the cblG disorder is difficult especially in early stages of the disease. Comprehensive metabolic analyses and genetic tests have been used to diagnose cblG disorder. Early identification of this rare disease and timely administration of parenteral vitamin B12, oral betaine, and leucovorin therapy is critical for controlling disease progression and improving prognosis.
We report the case of a 2.1-month-old Chinese girl with the cblG disorder with poor feeding, failure to thrive, and pancytopenia, esotropia, ocular nystagmus, and hypotonia. WES detected a pair of compound-heterozygous MTR variants, and a novel pathogenic, de novo mutation in the MTR gene was identified, which is believed to enrich the mutation spectrum of the MTR gene and enhances clinical awareness of this disease among physicians. Additionally, the mutations are summarized and discussed.
Methods
Patient
Written informed consent was obtained from the parents of the patient for publication of this case report and any accompanying images. Ethical approval was granted by Wuhan Children’s Hospital Research Ethics Committee (No.2022R038).
Patient clinical characteristics and laboratory results were collected. The patient was a 2.1-month-old Chinese girl, the third child of non-consanguineous parents, delivered at full term. She gave birth vaginally after a spontaneous conception at 39 weeks. Her birth weight, body length, and head circumference were 3.0 kg (25–50th percentile), 50 cm (50th percentile), and 34 cm (50th percentile), respectively. There was no family history of metabolic disorders, unexplained pediatric neurological diseases, or deaths. She visited our hospital with complaints of poor feeding, failure to thrive, and poor growth (weight: 3.2 kg, < 3rd percentile; length: 51 cm, < 3rd percentile; head circumference: 37.5 cm, < 3rd percentile). She had obvious signs of anemia, such as pale lips and nail beds pallor. Thin subcutaneous fat, esotropia, ocular nystagmus, and hypotonia were also observed. Her facial features were normal. A complete blood count revealed that she had pancytopenia, with a white blood cell count (WBC) of 3.26 × 109/L (5.6–14.5), red blood cell count (RBC) of 2.22 × 1012/L (3.5–5.6), hemoglobin (Hb) of 71 g/L (99–196), and platelets count of 61 × 109/L (203–653). 24-h video-electroencephalographic showed multifocal sharp waves, mainly during sleep and two spasms during wakefulness. (Fig. 1A), and magnetic resonance imaging exhibited widened peripheral cerebrospinal fluid spaces, slightly deepened cerebral sulcus, decreased brain parenchyma, and corpus callosum hypoplasia (Fig. 1B). Bone marrow examination revealed megaloblastic changes. Parents refused ophthalmological examinations during hospitalization. The other test results were normal.
Comprehensive metabolic analyses
After the patient was admitted to the hospital, metabolic tests were performed, including blood amino acid and acylcarnitine profiling using liquid chromatography–tandem mass spectrometry (LC–MS/MS), urinary organic acid analysis using gas chromatography–mass spectrometry (GC–MS), and total plasma homocysteine (tHcy), B12, and folate levels.
Whole-exome sequencing and validation
Peripheral blood was collected from the patient and their parents. Whole-exome sequencing (WES) was performed at the Chigene Medical Laboratory in Beijing, China. Hybridization was used to enrich target DNA fragments and construct an exome library. Illumina NovaSeq 6000 sequencers were used for high-throughput sequencing. Quality control of raw data (FASTQ format) was performed to ensure the significance of downstream analysis. Genome Analysis Toolkit (GATK) was used to identify single-nucleotide and indel variants. The Burrows-Wheeler Aligner (BWA) was used to align both ends. The screening of SNPs and indels was conducted by taking into account the sequence depth and mutation quality. The alignment of high-quality paired-end reads was performed against the human reference genome sequence sourced from the UCSC database (GChR37hg19, http://genome.ucsc.edu/) using the Burrows-Wheeler Alignment tool. The variants were annotated using the OMIM, ESP6500 [12], ExAC [13], ClinVar [14], and Human Gene Mutation Database (HGMD). The verification of candidate genes in the patient and his parents was verified through Sanger sequencing. Additionally, American College of Medical Genetics and Genomics (ACMG) guidelines [15] were followed to classify possible variations in this patient. Mutation sites in protein sequences were analyzed using Molecular Evolutionary Genetics Analysis (MEGA) software.
Results
Comprehensive metabolic analyses
A patient’s serum B12 concentration was 230 pmol/L (139.4–651.5), and his folate concentration was 41.25 nmol/L (7.0–46.4). Further examinations revealed that she had a distinctly elevated plasma tHcy level (92.25 µmol/L [5–15]). The amino acid and acylcarnitine analysis documented low Met (4.67 µmol/L [10–50]). Urinary organic acid displayed normal methylmalonic acid.
Genetic analysis
We conducted the trio-WES to identify the causative gene. We performed bioinformatics analysis to identify candidate variants using a filtering strategy based on population frequency, variant classification, and variant functional damaging prediction. Compound-heterozygous variants c.1812 + 3A > G and c.2405G > A (p.A802G) were discovered in the MTR gene (NM_000254.3) in this patient (Fig. 2A). Variant c.2405G > A (p.A802G) was inherited from his Mather, whereas variant c.1812 + 3A > G was inherited from his father. Sanger sequencing confirmed these two mutations in the patient and discovered that the parents were heterozygous for one of each mutated allele, and the two elder sisters had no abnormalities (Fig. 2B). The variant c.2405G > A (p.A802G) has been identified in dbSNP (rs760932771, gnomAD 0.003%) as a causative variant [11]. Bioinformatic analysis indicated that the missense mutation, c.2405G > A (p.A802G), was conserved among different species (Fig. 2C). The amino acid substitutions were probably damaging, with a high PolyPhen-2 score of 0.998, a SIFT tolerance index of 0.0018, a REVEL score of 0.829 (deleterious), and an M-CAP score of 0.397 (damaging) [15]. Variant c.1812 + 3A > G has been discovered in dbSNP (rs1201235550, TOPMed Bravo < 0.01%) and other variation databases (UCSC, gnomAD); however, the variant has not been previously reported in the literature. Following the ACMG guidelines, these two variants were categorized as ‘likely pathogenic’ (PS3 + PM2 + PP3) [15]. The three-dimensional structure suggests that the protein stability was decreased after mutation due to the reduction in hydrogen bonds (Fig. 3A).
A Sanger sequencing of MTR gene variants in this patient of this study. B Genealogical tree of this family, no abnormalities were found in her sisters. C Conservation analysis of MTR protein among different species. D Scheme of the distribution of MTR mutations, and the mutations in red arrow were reported in our patient
A Three-dimensional structure pattern MTR protein. The mutated amino acids at the mutation site are represented by gray sticks, while the amino acids with polar interactions with the mutated amino acids are represented by yellow sticks. In the wild-type, polar interactions exist between Arg802 and Ile775, Gly773. In the p.Arg802Gln mutant type, a new polar interaction occurs between Gln802 and Thr774, potentially leading to structural changes in the protein and affecting its normal physiological function. B The splicing site mutation (c.1812 + 3A > G) and missense mutation lead to exons skipping on RNA processing
Effect of variants on RNA Processing
RNA was extracted from the patient and normal control using TRIzol reagent, and the results revealed that the splicing site mutation (c.1812 + 3A > G) led to the deletion of exon 17 during mRNA processing. c.2405G > A (p.A802G) was a missense mutation located at the last position of exon 22. We suspect that this mutation also affects RNA processing and maturation, and the experimental results present that this missense mutation can lead to the deletion of exon 22 during mRNA processing (Fig. 3B).
Treatment and prognosis
Initially, the patient received a blood transfusion, gamma globulin infusion, and anti-infective treatment. However, the clinical situation exhibited no significant improvement. Hydroxocobalamin (1 mg, every other day) i.m., betaine (1 g/day) p.o., and calcium folinate (5 mg/day) p.o. were administered to reduce tHcy and normalize Met when metabolic workup strongly supports inherited disorders of cobalamin intracellular. Her general condition gradually improved, and her blood routine parameters returned to the normal range within seven days. The patient was advised to follow up in the outpatient clinic two weeks after discharge. Regrettably, the patient did not return for any follow-up visits and did not take medicine regularly for 17 months due to COVID-19. At the first follow-up visit (one year and seven months old), the patient’s complete blood count was normal, the growth and development (length: 77.5 cm, 3rd–10th percentile and weight: 9.0 kg, 3rd–10th percentile) lagged substantially behind their peers, and the plasma tHcy levels were markedly elevated. Her plasma tHcy levels significantly decreased, while Met levels slowly returned to near-normal after regular medication for two months. Afterward, the patient was transferred to maintenance therapy, consisting of intramuscular hydroxycobalamin 5 mg twice weekly. At the final follow-up visit (one year and 11 months old), her plasma tHcy declined to the normal range, while the Met level increased to the normal range, and all hematological parameters normalized (Table 1). However, the physical growth (length: 81.5 cm, 10–25th percentile; weight was 10.5 kg, 10–25th percentile), gross and fine motor skills, verbal abilities, social competence, and personal activities revealed slight deficiency than peers.
Discussion
The cblG disorder is a hereditary condition affecting cobalamin metabolism that results in a functional deficiency of MS and causes HHcy, hypomethioninemia, and megaloblastic anemia but not methylmalonic aciduria [16, 17]. Its pathogenesis has been primarily attributed to MS and HHcy dysfunction [4, 5]. The MS dysfunction leads to the block of Met remethylation and HHcy. HHcy is mainly associated with neurocognitive and vascular diseases. It has also been shown to induce synergistic mitochondrial dysfunction.
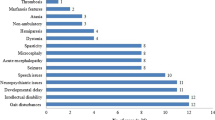
MTR gene encoding MS, located on chromosome 1p43, contains 33 exons and 32 introns, with a minimum length of 60 kb, the sizes of two introns being undefined [2]. To date, 57 mutations of the MTR gene are documented in HGMD (Fig. 2D), including 47 (82.5%) disease-causing mutations (DM), seven likely disease-causing mutations (DM), and three disease-associated polymorphisms (DP). Among them, c.3518C > T p.P1173L is a highly prevalent mutation detected in the MTR gene, affecting approximately 40% of European cblG patients [2]. However, genotype and phenotype did not significantly correlate with cblG until now. Regarding the type of variants, HGMD collected 25 missense, 12 frameshifts, three inframe, nine splices (four canonical and one exonic), four nonsense, two regulatory, one noncoding, and one synonymous. Missense mutations account for nearly half (25/57, 43.9%) of all DMs and are the most common mechanism of cblG disorder. Cobalamin metabolism disorders are also associated with mutations of LMBRD1 genes. Methylmalonic acidemia/aciduria and HHcy/homocystinuria are associated with altered LMBRD1 genes [18]. The alteration MBRD1 c.1056delG (p.L352Lfs*18) is commonly reported and was found in 75% (18/24 chromosomes) of a cohort consisting of 12 patients with cblF deficiency [19]. There is a wide variation in the clinical features observed in patients with LMBRD1 [20]. The phenotypic variability of patients with the c.1056delG mutation varies considerably depending on whether they are compound-heterozygous or homozygous [20]. In this study, we also identified a missense mutation (c.2405G > A p.A802G), which has been linked to the malfunction of the proteins encoded by the MTR gene [11]. Moreover, we discovered a novel splice acceptor site mutation (c.1812 + 3A > G), which was infrequent in genetic MTR variants. The novel splicing acceptor site was A base change from A to G at position 1812, which resulted in skipping of exons and may cause mRNA instability (easy degradation) Or produce frameshift truncated proteins.
The clinical presentation of cblG patients is variable, depending on the age of onset and the degree of enzyme activity deficiency [21]. Patients may present with acute neurological distress in the neonatal period and acute neurologic changes or psychiatric disturbances in adolescence or adulthood [22]. The most frequently reported symptoms include macrocytic anemia, feeding difficulties, muscular hypotonia, nystagmus, failure to thrive, and seizures. Microangiopathy and hemolytic uremic syndrome, frequently described in cblC defect, have only been reported as two cases in the cblG disorder [11, 23]. A minority of patients may exhibit indications of subacute combined degeneration of the spinal cord [5]. Other less frequently reported clinical manifestations are pulmonary hypertension, recurrent infections, and hydrocephalus [17, 23,24,25,26]. The clinical presentations of pancytopenia, failure to thrive, nystagmus, and hypotonia observed in our patient are similar to previous reports.
The published experience of patients suffering from cblG disorder reveals that patients may experience potentially fatal acute or rapidly progressive neurological deterioration without appropriate therapy [11, 24, 27]. Therefore, early diagnosis and proper treatment are essential to ensure optimal outcomes. Many prior findings confirm that treatment for cblG disorder should be initiated as soon as possible [5, 24, 28, 29]. However, diagnosis is frequently delayed due to the variable and non-specific symptoms observed in cblG disorder patients, resulting in severe and irreversible neuromotor impairments. When an infant has megaloblastic anemia and neurological manifestations during the initial months of life, physicians should maintain a high index of suspicion for cblG disorder and order certain tests, such as plasma tHcy, Met, and methylmalonic acid levels. Once the biochemical values support a cobalamin defect, treatment should be started early.
Currently, there are no formal guidelines for managing and treating cblG disorder dosages. However, most physicians now use folic or folinic acid, betaine, and hydroxocobalamin to combat this disease [5]. Met supplementation was also reported, but the efficacy is uncertain [5, 10]. The biochemical parameters tHcy and Met primarily respond positively to treatment, consistent with our finding. However, the clinical efficacy of neurological development treatment has not been established. Fortunately, a literature review suggests earlier therapy initiation may result in better developmental recovery and prevention of further neurological degeneration. There is no unanimous consensus on the recommended dose and frequency of the above drugs. In our patient, treatment included hydroxocobalamin (5 mg i.m., twice a week), betaine (1 g p.o., once per day), and calcium folinate (5 mg p.o., once per day) was provided. During follow-up, the patient’s hematological system returned to normal, and neurological development improved significantly.
In conclusion, WES detected a pair of compound-heterozygous MTR variants in a 2.1-month-old Chinese girl with cblG disorder who presented with pancytopenia and developmental delay. This study may provide empirical evidence for early diagnosis and suitable therapy of cblG disorder patients in the future. The study also reviewed and summarized MTR mutations reported in HGMD. Particularly, we detected a novel variant, c.1812 + 3A > G, enlarges the spectrum of diseases associated with the MTR gene and supports the early diagnosis and suitable treatment of CblG patients in the future.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Watkins D, Rosenblatt DS (1988) Genetic heterogeneity among patients with methylcobalamin deficiency. Definition of two complementation groups, cblE and cblG. J Clin Invest 81(6):1690–1694
Watkins D, Ru M, Hwang HY, Kim CD, Murray A, Philip NS et al (2002) Hyperhomocysteinemia due to methionine synthase deficiency, cblG: structure of the MTR gene, genotype diversity, and recognition of a common mutation, P1173L. Am J Hum Genet 71(1):143–153
Matthews RG (2001) Cobalamin-dependent methyltransferases. Acc Chem Res 34(8):681–689
Surtees R (1998) Demyelination and inborn errors of the single carbon transfer pathway. Eur J Pediatr 157(Suppl 2):S118–S121
Schiff M, Benoist JF, Tilea B, Royer N, Giraudier S, Ogier de Baulny H (2011) Isolated remethylation disorders: do our treatments benefit patients. J Inherit Metab Dis 34(1):137–145
Kubová H, Folbergrová J, Mares P (1995) Seizures induced by homocysteine in rats during ontogenesis. Epilepsia 36(8):750–756
Mares P, Folbergrová J, Langmeier M, Haugvicová R, Kubová H (1997) Convulsant action of D, L-homocysteic acid and its stereoisomers in immature rats. Epilepsia 38(7):767–776
Morath MA, Okun JG, Müller IB, Sauer SW, Hörster F, Hoffmann GF et al (2008) Neurodegeneration and chronic renal failure in methylmalonic aciduria–a pathophysiological approach. J Inherit Metab Dis 31(1):35–43
Zsengellér ZK, Aljinovic N, Teot LA, Korson M, Rodig N, Sloan JL et al (2014) Methylmalonic acidemia: a megamitochondrial disorder affecting the kidney. Pediatr Nephrol 29(11):2139–2146
Huemer M, Diodato D, Schwahn B, Schiff M, Bandeira A, Benoist JF et al (2017) Guidelines for diagnosis and management of the cobalamin-related remethylation disorders cblC, cblD, cblE, cblF, cblG, cblJ and MTHFR deficiency. J Inherit Metab Dis 40(1):21–48
Huemer M, Bürer C, Ješina P, Kožich V, Landolt MA, Suormala T et al (2015) Clinical onset and course, response to treatment and outcome in 24 patients with the cblE or cblG remethylation defect complemented by genetic and in vitro enzyme study data. J Inherit Metab Dis 38(5):957–967
Fu W, O’Connor TD, Jun G, Kang HM, Abecasis G, Leal SM et al (2013) Analysis of 6,515 exomes reveals the recent origin of most human protein-coding variants. Nature 493(7431):216–220
Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T et al (2016) Analysis of protein-coding genetic variation in 60,706 humans. Nature 536(7616):285–291
Landrum MJ, Chitipiralla S, Brown GR, Chen C, Gu B, Hart J et al (2020) ClinVar: improvements to accessing data. Nucleic Acids Res 48(D1):D835–D844
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17(5):405–424
Watkins D, Rosenblatt DS (1989) Functional methionine synthase deficiency (cblE and cblG): clinical and biochemical heterogeneity. Am J Med Genet 34(3):427–434
Harding CO, Arnold G, Barness LA, Wolff JA, Rosenblatt DS (1997) Functional methionine synthase deficiency due to cblG disorder: a report of two patients and a review. Am J Med Genet 71(4):384–390
Watkins D, Rosenblatt DS (2011) Inborn errors of cobalamin absorption and metabolism. Am J Med Genet C Semin Med Genet 157C(1):33–44
Rutsch F, Gailus S, Miousse IR, Suormala T, Sagné C, Toliat MR et al (2009) Identification of a putative lysosomal cobalamin exporter altered in the cblF defect of vitamin B12 metabolism. Nat Genet 41(2):234–239
Froese DS, Gravel RA (2010) Genetic disorders of vitamin B12 metabolism: eight complementation groups–eight genes. Expert Rev Mol Med 12:e37
Ogier de Baulny H, Gérard M, Saudubray JM, Zittoun J (1998) Remethylation defects: guidelines for clinical diagnosis and treatment. Eur J Pediatr 157(Suppl 2):S77-83
Carmel R, Watkins D, Goodman SI, Rosenblatt DS (1988) Hereditary defect of cobalamin metabolism (cblG mutation) presenting as a neurologic disorder in adulthood. N Engl J Med 318(26):1738–1741
Labrune P, Zittoun J, Duvaltier I, Trioche P, Marquet J, Niaudet P et al (1999) Haemolytic uraemic syndrome and pulmonary hypertension in a patient with methionine synthase deficiency. Eur J Pediatr 158(9):734–739
Kripps KA, Sremba L, Larson AA, Van Hove J, Nguyen H, Wright EL et al (2022) Methionine synthase deficiency: variable clinical presentation and benefit of early diagnosis and treatment. J Inherit Metab Dis 45(2):157–168
Farwell Gonzalez KD, Li X, Lu HM, Lu H, Pellegrino JE, Miller RT et al (2015) Diagnostic exome sequencing and tailored bioinformatics of the parents of a deceased child with cobalamin deficiency suggests digenic inheritance of the MTR and LMBRD1 genes. JIMD Rep 15:29–37
Outteryck O, de Sèze J, Stojkovic T, Cuisset JM, Dobbelaere D, Delalande S et al (2012) Methionine synthase deficiency: a rare cause of adult-onset leukoencephalopathy. Neurology 79(4):386–388
Vaisbich MH, Braga A, Gabrielle M, Bueno C, Piazzon F, Kok F (2017) Thrombotic microangiopathy caused by methionine synthase deficiency: diagnosis and treatment pitfalls. Pediatr Nephrol 32(6):1089–1092
Kasapkara ÇS, Yılmaz-Keskin E, Özbay-Hoşnut F, Akçaboy M, Polat E, Olgaç A et al (2019) An infant with an extremely rare cobalamin disorder: methionine synthase deficiency and importance of early diagnosis and treatment. Turk J Pediatr 61(2):282–285
Wong D, Tortorelli S, Bishop L, Sellars EA, Schimmenti LA, Gallant N et al (2016) Outcomes of four patients with homocysteine remethylation disorders detected by newborn screening. Genet Med 18(2):162–167
Acknowledgements
We would like to thank the patient and her family members for participating in this study. We also thank the GrandOmics Biosciences Co., Ltd (Beijing, China) for their technical assist.
Funding
Nothing to declare.
Author information
Authors and Affiliations
Contributions
XHC and HY provided the overall design of the manuscript. LJ, HG and PZ wrote the paper, revised the paper, and drew the tables and figures. LY and LF contributed to the acquisition of the data and clinical assessment. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was granted by Wuhan Children’s Hospital Research Ethics Committee (No.2022R038).
Consent for publication
Written informed consent was obtained from the parents of the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare that there is no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luo, J., Chen, X., Guo, H. et al. Novel MTR compound-heterozygous mutations in a Chinese girl with HHcy due to methionine synthase deficiency, cblG: a case report. Egypt J Med Hum Genet 25, 1 (2024). https://doi.org/10.1186/s43042-023-00469-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-023-00469-z