Abstract
Background
Pulmonary embolism (PE) is a lethal type of venous thromboembolic disease. Right ventricular (RV) failure is not an uncommon complication of PE leading to higher adverse outcomes. The tricuspid annular peak systolic excursion/pulmonary artery systolic pressure (TAPSE/PASP) ratio as a surrogate for RV–pulmonary artery coupling has proven to be among the predictor of clinical outcomes in multiple patient groups. We evaluated in this study the role of TAPSE/PASP ratio in predicting adverse clinical outcomes in patients with acute PE.
Results
Among patients with established diagnosis of acute PE admitted to the coronary care unit, echocardiography was done within 12 h of admission and TAPSE/PASP ratio was calculated. The patients were followed during hospitalization and after discharge for 3 months for development of adverse outcomes including rehospitalization due to heart failure, recurrent PE and mortality. A total of fifty-five consecutive patients were recruited with mean age 58.3 ± 6.9 years and nearly equal male-to-female ratio. The mean ratio of TAPSE/PASP was 0.479 ± 0.206. In-hospital and 3-month follow-up showed that 10.9% needed rehospitalization with heart failure, 14.5% developed recurrent pulmonary embolism, and mortality was 9.1%. TAPSE/PASP ratio was significantly lower among the patients who developed adverse outcomes. TAPSE/PASP ratio was among the independent predictors of rehospitalization with heart failure, recurrent pulmonary embolism but not mortality at 3-month follow-up. TAPSE/PASP ratio predicted rehospitalization with heart failure at a cutoff point ≤ 0.325, with 100% sensitivity and 79.6% specificity, and predicted recurrent pulmonary embolism at a cutoff point ≤ 0.325, with 75% sensitivity and 78.7% specificity.
Conclusion
TAPSE/PASP ratio is a noninvasive tool that can predict the development of early adverse outcomes in patients with acute PE including rehospitalization with heart failure and recurrent pulmonary embolism.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Pulmonary embolism (PE) is a lethal type of venous thromboembolic disease. It is considered the third among the cause of cardiovascular mortality with in-hospital mortality rates between 5 and 10% [1, 2].
Right ventricular (RV)–pulmonary artery (PA) coupling refers to relation between the RV afterload and the RV contractility. Chronic conditions associated with increased pulmonary artery (PA) pressure and RV afterload provide time for the RV contractility to increase to try to maintain the RV–PA coupling. This is not the case for acute conditions as acute PE, so this leads to failure of this balance causing acute RV failure that is associated with increased adverse clinical outcomes mainly rehospitalization and mortality [3].
RV failure complicates 30% of acute PE patients leading to 5% in-hospital mortality. This emphasizes the importance of early detection of RV dysfunction in these patients [4].
The main method for assessing the RV–PA coupling is the right heart catheterization (RHC). Multiple research has been conducted to find noninvasive modalities to evaluate RV–PA coupling including echocardiographic measurement of the ratio between tricuspid annular peak systolic excursion and pulmonary artery systolic pressure (TAPSE/PASP) [3].
The predictive value of TAPSE/PASP ratio has been evaluated in multiple patient groups including patients with pulmonary hypertension, heart failure, valvular heart disease and post-cardiac surgery [5,6,7,8,9].
Few studies addressed the predictive value of TAPSE/PASP ratio in patients with acute PE. We aimed in this study to evaluate the predictive role of TAPSE/PASP to detect adverse clinical outcomes in acute PE patients.
Methods
The study was cross-sectional analytical prospective including fifty-five patients with confirmed diagnosis of acute PE admitted to the intensive care unit of the cardiovascular department of Kasr Alainy Hospital, Cairo University, in the period between January 2023 and January 2024.
Eligible participants included patients ≥ 18 years admitted with normotensive acute PE according to the latest European Society of Cardiology guidelines [10]. Exclusion criteria included previous PE, history of RV dysfunction, history of tricuspid valve disease or tricuspid valve replacement, PE due to malignancy, PE with hemodynamic instability and technical difficulties in assessing RV–PA coupling by echocardiography.
After obtaining informed consent [11], history and physical examination data were collected. Laboratory workup and 12-lead electrocardiogram were done. Within 12 h of admission, transthoracic echocardiography was done using a vivid machine equipped with a transthoracic 2.5 MHz transducer. Echocardiographic parameters assessed included left ventricular (LV) size, LV contractility, right atrial (RA) size, RV size and PASP. RV systolic function was evaluated by RV S wave velocity, RV fractional area changes (RV-FAC) and TAPSE. TAPSE/PASP ratio was used as a measure for RV–PA coupling.
All patients were followed during their hospital admission for their clinical status and after discharge for 3 months to detect the development of short-term outcomes including rehospitalization with heart failure, recurrent pulmonary embolism and mortality.
Statistical analysis was conducted using Statistical Package for the Social Science (SPSS) 28th edition. Mann–Whitney's and Chi-square tests were used to evaluate nonparametric and parametric variables, respectively. Univariate and multivariate regression analyses were used to detect the predictors of development of adverse outcomes. A receiver operator characterized curve (ROC) was constructed to assess the sensitivity, specificity and area under the curve (AUC) of TAPSE/PASP ratio to predict adverse outcomes and to set optimal cutoff point for development of these adverse outcomes. P value < 0.05 was used to prove statistical significance.
Results
Basic demographic data of patients are illustrated in Table 1; nearly half of patients were males with mean age 58.3 ± 6.9 years. All laboratory workup was within normal except for elevated levels of HbA1C, as illustrated in Table 2.
Echocardiographic data revealed normal mean LV dimensions and contractility, normal mean RA dimensions, normal mean RV dimensions and normal RV systolic function. The mean ratio of TAPSE/PASP was 0.479 ± 0.206 (Table 3).
At 3-month follow-up, mortality accrued in 9% of the patients (Table 4).
Binary logistic regression was executed for factors predicting occurrence of adverse events (Tables 5, 6, 7), where TAPSE/PASP ratio predicted rehospitalization with heart failure, with an odds ratio of 0.964. Also, TAPSE/PASP ratio predicted occurrence of recurrent pulmonary embolism, with an odds ratio of 0.99, while it couldn’t predict mortality.
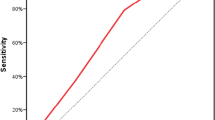
ROC curve analysis showed that TAPSE/PASP ratio predicted rehospitalization with heart failure at a cutoff point ≤ 0.325, with 100% sensitivity and 79.6% specificity. It also predicted recurrent pulmonary embolism at a cutoff point ≤ 0.325, with 75% sensitivity and 78.7% specificity (Table 8, Figs. 1, 2).
Discussion
The main findings of this study include:
-
1.
Among the recruited patients, 10.9% needed rehospitalization with heart failure, 14.5% developed recurrent pulmonary embolism, and mortality was 9.1% through a period of three months follow up.
-
2.
TAPSE/PASP ratio was significantly lower among patients who developed adverse outcomes.
-
3.
TAPSE/PASP ratio was among the independent predictors of rehospitalization with heart failure, recurrent pulmonary embolism but not mortality at 3-month follow-up.
-
4.
TAPSE/PASP ratio predicted rehospitalization with heart failure at a cutoff point ≤ 0.325, with 100% sensitivity and 79.6% specificity, and predicted recurrent pulmonary embolism at a cutoff point ≤ 0.325, with 75% sensitivity and 78.7% specificity.
Multiple studies validated TAPSE/PASP ratio as a simple, noninvasive echocardiographic method for evaluating RV–PA coupling [3]. TAPSE/PASP ratio has been studied as a predictor of clinical adverse outcomes in multiple patient groups. Among patients with heart failure, TAPSE/PASP ratio was among the important prognostic variables for adverse outcomes [5]. Also, TAPSE/PASP ratio predicted the occurrence of adverse outcomes among pulmonary hypertension patients [6]. In the Global-Tri-Valve registry, among patients with tricuspid regurgitation scheduled for percutaneous intervention either repair or replacement, TAPSE/PASP ratio predicted the occurrence of 12-month all-cause mortality [7]. Also, in the EuroSMR registry that included severe mitral incompetence patients indicated for percutaneous valve replacement [8], TAPSE/PASP ratio was an independent predictor of 24-month mortality. Partner 3 trial showed that TAPSE/PASP ratio independently predicted 2-year composite adverse outcomes among low-risk patients with symptomatic severe aortic stenosis indicated for percutaneous or surgical valve replacement [9].
The value of TAPSE/PASP ratio in predicting adverse outcomes in patients with acute PE is not well studied. In this study, TAPSE/PASP ratio independently predicted the occurrence of adverse clinical outcomes in acute PE patients including rehospitalization with heart failure and recurrent pulmonary embolism at 3-month follow-up. This can be explained by the acute desynchrony between the RV afterload and RV contractility that occurs in acute PE patients due to acute increase in RV afterload unmatched by similar compensatory increase in the RV contractility. This desynchrony is reflected on the TAPSE/PASP ratio. This is concordant with the results of a recent study involving patients with acute PE evaluated multiple echocardiographic parameters that can assess RV–PA coupling. This study showed that TAPSE/PASP ratio was independently associated with adverse events during hospitalization [12]. Also, another recent retrospective study involving acute PE patients showed that TAPSE/PASP ratio predicted the development of 7-day adverse outcomes including mortality and hemodynamic compromise. In this study, a cutoff value of 0.4 for the TAPSE/PASP ratio was identified as the optimal cutoff value for predicting adverse clinical outcome in patients with acute PE [13].
Limitations of the study
The limitations of the study include that it is a single-center study. Also, TAPSE provides data about the longitudinal rather than the global RV function. RHC is the gold standard for assessment of the PASP; however, in this study we used the echocardiographic assessment.
Conclusions
TAPSE/PASP ratio is a noninvasive tool that can predict development of early adverse clinical outcomes among patients with acute PE including rehospitalization with heart failure and recurrent pulmonary embolism. Further multicenter studies are needed to validate the use of this bedside parameter to predict adverse outcomes in this critical patient group.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PE:
-
Pulmonary embolism
- RV:
-
Right ventricle
- PA:
-
Pulmonary artery
- TAPSE:
-
Tricuspid annular peak systolic excursion
- PASP:
-
Pulmonary artery systolic pressure
- LV:
-
Left ventricle
- EF:
-
Ejection fraction
- RA:
-
Right atrium
- FAC:
-
Fractional area change
- ROC:
-
Receiver operator characterized
References
Turetz M, Sideris AT, Friedman OA, Triphathi N, Horowitz JM (2018) Epidemiology, pathophysiology, and natural history of pulmonary embolism. Semin Intervent Radiol 35(2):92–98
Arrigo M, Huber LC, Winnik S, Mikulicic F, Guidetti F, Frank M, Ruschitzka F (2019) Right ventricular failure: pathophysiology, diagnosis and treatment. Card Fail Rev 5(3):140
He Q, Lin Y, Zhu Y, Gao L, Ji M, Zhang L, Xie M, Li Y (2023) Clinical usefulness of right ventricle-pulmonary artery coupling in cardiovascular disease. J Clin Med 12(7):2526
Grifoni S, Olivotto I, Cecchini P, Pieralli F, Camaiti A, Santoro G, Conti A, Agnelli G, Berni G (2000) Short-term clinical outcome of patients with acute pulmonary embolism, normal blood pressure, and echocardiographic right ventricular dysfunction. Circulation 101:2817–2822
Bosch L, Lam CSP, Gong L, Chan SP, Sim D, Yeo D, Jaufeerally F, Leong KTG, Ong HY, Ng TP, Richards AM, Arslan F, Ling LH (2017) Right ventricular dysfunction in left-sided heart failure with preserved versus reduced ejection fraction. Eur J Heart Fail 19(12):1664–1671
Li Y, Guo D, Gong J, Wang J, Huang Q, Yang S, Zhang X, Hu H, Jiang Z, Yang Y, Lu X (2021) Right ventricular function and its coupling with pulmonary circulation in precapillary pulmonary hypertension: a three-dimensional echocardiographic study. Front Cardiovasc Med 8:690606
Brener MI, Lurz P, Hausleiter J, Rodés-Cabau J, Fam N, Kodali SK, Rommel KP, Muntané-Carol G, Gavazzoni M, Nazif TM, Pozzoli A, Alessandrini H, Latib A, Biasco L, Braun D, Brochet E, Denti P, Lubos E, Ludwig S, Kalbacher D, Estevez-Loureiro R, Connelly KA, Frerker C, Ho EC, Juliard JM, Harr C, Monivas V, Nickenig G, Pedrazzini G, Philippon F, Praz F, Puri R, Schofer J, Sievert H, Tang GHL, Andreas M, Thiele H, Unterhuber M, Himbert D, Alcázar MU, Von Bardeleben RS, Windecker S, Wild MG, Maisano F, Leon MB, Taramasso M, Hahn RT (2022) Right ventricular- pulmonary arterial coupling and afterload reserve in patients undergoing transcatheter tricuspid valve repair. J Am Coll Cardiol 79(5):448–461
Karam N, Stolz L, Orban M, Deseive S, Praz F, Kalbacher D, Westermann D, Braun D, Näbauer M, Neuss M, Butter C, Kassar M, Petrescu A, Pfister R, Iliadis C, Unterhuber M, Park SD, Thiele H, Baldus S, Stephan von Bardeleben R, Blankenberg S, Massberg S, Windecker S, Lurz P, Hausleiter J (2021) Impact of right ventricular dysfunction on outcomes after transcatheter edge-to-edge repair for secondary mitral regurgitation. JACC Cardiovasc Imaging 14(4):768–778
Cahill TJ, Pibarot P, Yu X, Babaliaros V, Blanke P, Clavel MA, Douglas PS, Khalique OK, Leipsic J, Makkar R, Alu MC, Kodali S, Mack MJ, Leon MB, Hahn RT (2022) Impact of right ventricle-pulmonary artery coupling on clinical outcomes in the PARTNER 3 trial. JACC Cardiovasc Interv 15(18):1823–1833
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing G-J, Harjola V-P, Huisman MV, Humbert M, Jennings CS, Jiménez D, Kucher N, Lang IM, Lankeit M, Lorusso R, Mazzolai L, Meneveau N, Ní Áinle F, Prandoni P, Pruszczyk P, Righini M, Torbicki A, Van Belle E, Zamorano JL, ESC Scientific Document Group (2020) 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Heart J 41(4):543–603
Goodyear MD, Eckenwiler LA, Ells C (2008) Fresh thinking about the Declaration of Helsinki. BMJ 337:a2128
Kiamanesh O, Prosperi-Porta G, Harper L, Solverson K, Boiteau P, Helmersen D, Ferland A, Fine N, Weatherald J (2022) Ventricular-arterial decoupling is associated with in-hospital adverse events in normotensive pulmonary embolism. Int J Cardiovasc Imaging 38(12):2655–2665. https://doi.org/10.1007/s10554-022-02677-x. (Epub 2022 Jul 15)
Lyhne MD, Kabrhel C, Giordano N, Andersen A, Nielsen-Kudsk JE, Zheng H, Dudzinski DM (2021) The echocardiographic ratio tricuspid annular plane systolic excursion/pulmonary arterial systolic pressure predicts short-term adverse outcomes in acute pulmonary embolism. Eur Heart J Cardiovasc Imaging 22(3):285–294
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
AM, MM, HH and WA shared in the study idea, collection and analysis of data and finalizing the results. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was obtained by the ethical committee of Cairo University, Faculty of Medicine in 28/2/2023, and the reference number is (MS-232-2023).
Consent to participate
Informed written consent to participate in the study was obtained from all recruited patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mostafa, A., Medhat, M., Alhosary, H. et al. Role of right ventricular–pulmonary arterial coupling assessed by echocardiography to predict adverse outcomes in patients with acute pulmonary embolism. Egypt Heart J 76, 122 (2024). https://doi.org/10.1186/s43044-024-00554-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-024-00554-7