Abstract
Background
COVID-19-related lockdowns had resulted in overburdening on health services. The lockdowns along with anxiety of the disease have resulted in delay in routine vaccination of many under-5 children. The current study was undertaken to understand the extent of the delay in under-5 vaccination during COVID-19-related lockdown in March-December 2020.
Methods
It was a cross-sectional study conducted during January-December 2021. Study population was under five children due for vaccination during the first COVID-19 lockdown at March-December 2020. Vaccination cards were used to confirm the status of vaccination, and questionnaire was used to study the attitude of parents towards vaccination and reasons for delay in vaccination, if any. The calculated sample size was 1434. But cluster random sampling method was applied; hence, 2274 subjects were included in the study. Statistical analysis was done using IBM SPSS-22™, using descriptive statistics and chi-squared test.
Results
Percentages of children with delayed vaccination ranged from lowest for “at birth dose” (12.47%) to highest for “9th month dose, i.e. MR vaccine” (54.29%). Majority of parents stated lockdown and risk of COVID-19 infection as to be reason of the delay in vaccination. There was no uniform association between vaccination delay and attitude of parents towards vaccination.
Conclusion
COVID-19 pandemic and subsequent lockdown are the reasons stated by majority of parents with delayed vaccination in their children. This could be important lesson to plan for such contingencies for developing health services in future.
Similar content being viewed by others
Background
Childhood immunization is one of the key public health interventions adopted globally in the twentieth century. After the successful eradication of smallpox, WHO launched expanded immunization programme in 1974. At the launch of programme, the vaccine coverage in developing countries was meagre. In spite of many hurdles and shortcomings, the programme has helped in improving the vaccination coverage and also expanded the cover multiple diseases impacting from childhood to adulthood [1].
Following the outbreak of COVID-19 in Wuhan province of China in 2019, it spreads globally. It caused global lockdown resulting in disruption of economic and other day-to-day human activities [2]. Most of the countries experienced acute increase in cases of COVID-19, which lead to overburdening on healthcare staff and disruption of various routine health services [3].
Routine immunization programme is one of key areas of health services, which was affected due to the COVID-19 pandemic. In May 2020, WHO and UNICEF estimated that due to missed or delayed vaccination, 80 million infants from 68 countries may face increased risk to vaccine-preventable diseases like diphtheria, measles and polio. Fear of venturing out during lockdowns in the minds of parents, lack of transportation facilities, fear of COVID-19 infections and lack of health workers were some of the important reasons for the disruption of these services [4]. The impact was prominent in the developing countries from Africa and Asia like Ghana, Zimbabwe, Libera, Vietnam and Pakistan [5].
India launched its vaccination programme in 1978 and which gradually developed into one of the world’s biggest programme serving 300 million women and 260 million infants. It includes free vaccination for the children against many vaccine-preventable diseases like hepatitis B, polio, measles, diphtheria, pertussis, tetanus and rubella [6]. Following the elimination of polio, India is attempting to eliminate measles, with the help of intensified vaccination efforts [7]. Such efforts were hampered during COVID-19 pandemic, lowering the vaccination coverage [8].
The current research was conducted with objectives of finding the extent of under-5 vaccination coverage and delay during COVID-19 lockdown, assessing the attitude of parents towards vaccination and studying the reasons for the delay, in an urban area from Sangli district of Maharashtra state, India.
Methods
Study settings
It was a cross-sectional study, conducted in an urban area from the field practice area of a medical college from Sangli district of Maharashtra, India. The study was conducted from June 2021 to March 2022.
Permissions and consents
Institutional ethical committee approval, permissions from the relevant authorities and the written informed consent from each participant were acquired. The study population were children under the age of 5 years during March to December 2020, i.e. during first COVID-19 wave and lockdown. All the government advisory precautions on COVID-19 and lockdown were meticulously followed for the data collection.
Study procedure
Sampling technique applied was cluster random sampling, The municipal corporation is divided in territorial constituencies known as wards. A ward was selected randomly; mapped and visits were conducted to all the houses in the ward. In the households with children belonging to targeted age groups, parents were requested to participate in the study. The information regarding the study subjects and consent for participation was acquired from the parents/reliable informant. The exclusion criteria were non consent by parent(s), closed house and unavailability of the vaccination card at the time of data collection. If the household had more than one eligible child, then separate proforma was filled for each of them. After the completion of data collection, required vaccination counselling was given to the parents. Children who had missed vaccination at the time of data collection were noted, their parents were counselled, and with their consent, the information was shared with medical social worker (MSW) for follow-up. It was ensured with the help of MSW that those children received the missed dose and date of vaccination noted in the original data collection sheet. It was decided that the parents of children with missed vaccination, not consenting for the follow-up by the MSW and subsequent vaccination, should be considered as consent withdrawal from the study. However, we did not encounter any such case, and all the “missed” children were vaccinated. Choudhary et al. reviewed the data of NFHS-IV (2015–2016); he observed timeliness of OPV3 was lowest at 35%, i.e. delay of more than week in 65% children. Hence, 65% was considered as expected proportion for our study [9]. The calculated minimum sample size (confidence level at 99%, absolute precision at 5%) was 1434, but due to sampling method, the data was collected for 2274 study subjects.
Vaccination cards were used to confirm the dates of vaccination and date of birth of the child. For the purpose of the study, only the vaccines under Universal Immunization Programme (UIP) in the study area, until 5 years of age, were considered, and the optional vaccination or additional vaccines recommended by professional bodies like Indian Academy of Paediatricians (IAP) were not considered.
There is no universally accepted definition for “delayed vaccination”. It varies based on vaccine in question, study area and many other factors. In the literature, the definition of “delayed vaccination” varies from the strict definition of postponement of even a single day to loose definition of 30- to 90-day postponement [9,10,11]. In our study area, health facilities follow a practice of reserving a fixed day of a week for vaccination, to avoid wastage of vaccine vials and other resources (e.g. vaccination may be available every Thursday). This practice may inevitably result in a waiting period of up to 7 days from the expected date of vaccination. Hence, operational definition for the “delayed vaccination” in our study was vaccination postponement by more than 7 days from the expected date. We also took in account the minimum required interval while calculating expected date of vaccination. Hence, e.g. if dose 1 (6 week) was delayed, that does not automatically mean that dose 2 (10 weeks) was automatically delayed as the new expected date 4 weeks apart was applied.
Dose | Vaccines given under UIP (considered for this study) |
|---|---|
Dose 0 (at birth) | BCG, OPV, hepatitis B birth dose |
Dose 1 (6 weeks) | OPV-1, pentavalent-1, Rotavirus vaccine-1 (RVV), fractional dose of inactivated poliovirus vaccine (fIPV-1) |
Dose 2 (10 weeks) | OPV-2, pentavalent-2, RVV-2 |
Dose 3 (14 weeks) | OPV-3, pentavalent-3, RVV-3, fIPV-2 |
Dose 4 (9 months) | Measles and rubella (MR)-1 |
Dose 5 (18 months) | MR-2, diphtheria-pertussis-tetanus (DPT) booster-1, OPV |
Dose 6 (60 months) | Diphtheria-pertussis-tetanus (DPT) booster-2 |
Study tool
A pretested study questionnaires was used to collect the data from the parents. The initial section of proforma had basic information like birth date of child and mother’s education; the second section was for noting dates of vaccination from vaccine cards, and final section had questions regarding attitude of parents towards vaccination and reasons for delay in vaccination, if any. Only the information regarding vaccines and reasons for their delay, if any, which were due during the March to December 2020 were noted and included in the study. The proforma was finalized after pilot study.
Statistical analysis
Analysis was done using IBM SPSS-22™ and Microsoft Excel™ 2007. For the simplicity of presentation, the data is presented in the form of doses, which represent all the vaccines given at that age; individual vaccines are not considered.
Median, interquartile range, percentage and chi-square were the statistical tests applied. Data from the pilot study and incomplete proforma were not included in the final analysis.
Results
Data was collected for 2274 children; however, as some children were due for multiple vaccines during the March to December 2020, the table total is higher. The children who were expected to receive vaccination from dose 0 to dose 6 are 489, 539, 530, 520, 501, 510, and 68 respectively (master chart attached in supplementary material).
Missed or delayed vaccination
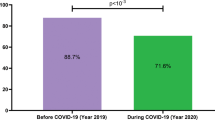
Two-hundred and twenty-one children (9.7%) had missed a vaccine at the time of data collection. Lowest percentage of missed dose was for “dose 0” 5 (1%), and highest was for “dose 6” 18 (26.5%). Their parents were counselled and followed up for the completion of vaccination (Fig. 1).
Median age of vaccination for all the doses is displayed in Table 1. If we considered the difference between expected age of vaccination and the median age at the time of actual vaccination, the difference was lowest for dose 0 and showed increasing difference with latter doses. However, this trend is not linear.
Delay for “dose 0” was observed in least percentage of children (12.47%), while delay for “dose 4, i.e. MR vaccination” was observed in highest percentage of children (54.29%). The median delay (in days) was lowest for “dose 0” and highest for “dose 3” and “dose 5” (Table 2).
Reasons for delay in vaccination
The presence of lockdown and risk of COVID infections were the most commonly accepted reasons by the parents for delay in vaccination. These two reasons attributed to over 80% delay for “dose 0”, 88–90% for “dose 1” to “dose 5” and 100% for “dose 6” (Table 3).
Attitude of parents
Majority of parents had good attitude towards vaccination. The attitude was better among the parents, whose children were due for latter dose of vaccination (i.e. older children) as compared to those due for earlier dose (Table 4).
Statistically significant association was not observed between mother’s education and delay in vaccination, except for dose 1 (chi-squared value = 5.624, df = 1, p-value = 0.018). However, for every vaccination dose, it was observed that within college educated/higher educated mother’s group, the percentage of delayed vaccination was lower as compared to non-delayed ones.
There is no statistically significant difference in attitude of parents with the delay in vaccination, except for dose 5 (chi-squared value = 15.781, df = 1, p-value = 0.00). The relationship of poor attitude and delayed vaccination was not uniform. For dose 0, dose 1, dose 2 and dose 3, higher percentage of parents with poor attitude had the delayed vaccination in their children. But for remaining doses, the percentages show the opposite trend.
Discussion
We observed that 9.7% of children had missed vaccination, who were later vaccinated with the help of MSW. Based on this finding, we can state that 90.3% of children did get their expected dose of vaccine, either in time or delayed during the period of March-December 2020. The dose 0 (BCG, OPV, hepatitis B birth dose) was received by 99% of children, with reducing trend in subsequent vaccines. The National Family Health Survey (NFHS)-5 collected during 2019–2021 observed the coverage for BCG at 95%; DPT 1 to 3 at 94%, 91% and 87%, respectively, and measles coverage at 88% [12]. Coverage in our study is slightly better than NFHS-5 data, but the difference is minor and can be attributed to the fact that NFHS-5 is a multicentric survey. Baghdadi et al. conducted a similar survey in Saudi Arabia [13]. The observation regarding missed vaccination was similar to our observation, i.e. birth dose was least missed vaccine, and proportion of missed vaccination increased with age.
In our study for most of the vaccines, the median age of children at the time of vaccination was within a week of desirable age of vaccination. However, the median delay among the children receiving “delayed vaccination” was considerably high. This suggests that parents who had passed over the expected date of vaccination had delayed the vaccination for weeks and in some cases for months. Smith et al. (2010) in the USA and Stein-Zamir and Israeli (2017) had observed that early vaccination delay results in less likely completion of all the vaccination within recommended age [14, 15]. Thus, the delay goes on compounding.
The percentage of children with delayed vaccination varied from lowest 12.47% for dose 0 (BCG, OPV, hepatitis B birth dose) to highest 51.92% for measles-rubella vaccine (9th month) dose. The study area is an urban area with good health infrastructure including two medical colleges, multiple government health centres and hundreds of private practitioners. Despite all these facilities, about 10% of missed vaccination and very high percentage of delayed vaccination are worrisome. The delay for measles dose may hamper the measles — rubella elimination efforts [7]. Vaccination timeliness is a neglected aspect as compared to vaccination coverage. But timeliness is also important, as the delay increases susceptibility to infection and its potential complications. Gurrero F. (USA) has observed delay in vaccination due to complacency of success achieved in immunization and low incidence of disease. The author has concluded this as a threat to the development optimal immunity and can pose a risk in future [16]. On reviewing the data of NFHS-4 (2015–2016), Chowdhury et al. had observed that BCG, DPT-1st dose and measles were delayed in 23.1%, 29.3% and 34.8% children, respectively [17]. This study data precedes our data by 4–5 years; hence, better coverage and timeliness in our study are expected. We had more strict definition for vaccination delay as compared to Chowdhury et al.; hence, we cannot directly compare the results. The timeliness for the BCG was quite good in our study. This could be attributed to the substantial increase in institutional deliveries in 2019–2021 as compared to 2015–2016 [12].
Lockdown and risk of COVID-19 infection were the reasons given by majority (80% and above) of parents for delay in vaccination. Similar observations were made by Baktır and Kara in Türkiye, who found that fear of contracting COVID-19 was the most common reason for not being vaccinated during the pandemic [18]. We observed that most of the parents had good attitude regarding vaccination. A higher percentage of parents with older children had a better attitude than younger children. This may be due to experience and potentially repeated counselling at the time of each visit for vaccination. However, there was no uniformity when considering good attitude and timeliness of vaccination. This reflects that the anxiety related to COVID, and impact of lockdown, outweighed the attitude and probably knowledge regarding vaccination, in the health-seeking behaviour. The impact of COVID-19 on vaccination may be even worse in rural and difficult remote areas [19]. In survey conducted by Canadian researchers, it was concluded that vaccination delay increased during 1st wave of pandemic [20].
Though not statistically significant, higher percentage of children with college educated mothers received timely vaccination. Chandir, Siddiqi, Mehmood, Setayesh, Siddique, and Mirza had conducted a similar study in Sindh, Pakistan. They concluded that higher maternal education played a positive role in uptake of childhood immunization, even during a challenging lockdown [21].
Conclusion
Substantial proportion of children had delayed vaccination during the first COVID-19 lockdown. The proportion increased with age and impacted MR vaccine the highest. Such delays can hamper the progress achieved in controlling childhood illness and also derail progress in the campaigns like measles and rubella elimination.
Recommendations
It is easy to discard the current findings, as such globally disrupting events are rare. But this pandemic has exposed the current socio-political situation, state of international trade and deficiencies in health practices and services, as well as lack of preparedness. We have to plan our health services like vaccination programme, with consideration for contingencies that could arise.
Similarly, we believe there should be some information-technology-based reminder and follow-up mechanism for parents to vaccinate their children in time.
Limitations of the study
The study was conducted in a single urban area of Sangli district in Maharashtra, India. The rural, tribal and other remote areas might have fared differently with this respect. More detailed studies are required to understand the actual extent of the issue. Similar if we consider and hope that COVID-19 was one-off event in its impact and magnitude, then it will be difficult to generalize and use these findings for policy decisions.
Availability of data and materials
Submitting master chart in Excel format as supporting document.
Abbreviations
- COVID-19:
-
Coronavirus disease of 2019
- MR vaccine:
-
Measles and rubella vaccine
- OPV:
-
Oral polio vaccine
- BCG:
-
Bacille Calmette-Guerin (tuberculosis) vaccine
- MSW:
-
Medical social worker
- NFHS:
-
National Family Health Survey (India)
References
Keja K, Chan C, Hayden G, Henderson RH (1988) Expanded programme on immunization. World Heal Stat Q. 41(2):59–63
WHO. Advice for the public: coronavirus disease (COVID-19). World Health Organization. 2020. Cited 2022 Sep 16. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
Behera D, Praveen D, Behera MR (2020) Protecting Indian health workforce during the COVID-19 pandemic. J Fam Med Prim Care. 9(9):4541 (Cited 2022 Sep 16. Available from: /pmc/articles/PMC7652162/)
World Health Organization. At least 80 million children under one at risk of diseases such as diphtheria, measles and polio as COVID-19 disrupts routine vaccination efforts, warn Gavi, WHO and UNICEF. 2020. Cited 2022 Sep 16. Available from: https://www.who.int/news/item/22-05-2020-at-least-80-million-children-under-one-at-risk-of-diseases-such-as-diphtheria-measles-and-polio-as-covid-19-disrupts-routine-vaccination-efforts-warn-gavi-who-and-unicef
Nelson R (2020) COVID-19 disrupts vaccine delivery. Lancet Infect Dis 20(5):546. https://doi.org/10.1016/S1473-3099(20)30304-2
Lahariya C (2014) A brief history of vaccines & vaccination in India. Indian J Med Res 139(APR):491–511
Bavdekar S, Karande S (2017) Elimination of measles from India: challenges ahead and the way forward. J Postgr Med. 63(2):75–8 (Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5414430/ )
Khan A, Chakravarty A, Mahapatra J (2021) Impact of COVID-19 pandemic on childhood immunization in a tertiary health-care center. Indian J Community Med. 46(3):520 (Cited 2022 Sep 16. Available from: /pmc/articles/PMC8575194/)
Chaudhuri A, Debnath S. Timeliness and coverage of child vaccinations across India. IDEAS FOR INDIA. 2021; Available from: https://www.ideasforindia.in/topics/human-development/timeliness-and-coverage-of-child-vaccinations-across-india.html
Yadav K, Srivastava R, Kumar R, Chinnakal P, Rai SK, Krishnan A (2012) Significant vaccination delay can occur even in a community with very high vaccination coverage: evidence from Ballabgarh. India. J Trop Pediatr. 58(2):133–8 (Cited 2022 Sep 16. Available from: https://academic.oup.com/tropej/article/58/2/133/1636826 )
Varrasso D, Redlener I (1992) Defining delayed immunizations. Pediatr Infect Dis J. 11(10):897 (Available from: https://journals.lww.com/pidj/Citation/1992/10000/DEFINING_DELAYED_IMMUNIZATIONS.22.aspx )
Ministry of Health and Family Welfare Government of India. National Family Health Survey (NHFS-5), 2019-21: India Report. Vol. 361, Ministry of Health and Family Welfare National. Mumbai; 2020.
Baghdadi LR, Younis A, Al Suwaidan HI, Hassounah MM, Al Khalifah R. Impact of the COVID-19 pandemic lockdown on routine childhood immunization: a Saudi nationwide cross-sectional study. Front Pediatr. 2021;9. Cited 2022 Sep 16. Available from: https://pubmed.ncbi.nlm.nih.gov/34222155/
Smith PJ, Humiston SG, Parnell T, Vannice KS, Salmon DA (2010) Theassociation between intentional delay of vaccine administration and timely childhood vaccination coverage. Public Health Rep. 125(4):534–41. https://doi.org/10.1177/003335491012500408. (Cited 2022 Sept 25)
Stein-Zamir C, Israeli A (2017) Age-appropriate versus up-to-date coverage of routine childhood vaccinations among young children in Israel. Hum Vaccin Immunother. 13(9):2102–10. https://doi.org/10.1080/21645515.2017.1341028. (Cited 2022 Sept 25)
Guerra FA (2007) Delays in immunization have potentially serious health consequences. Paediatr Drugs 9(3):143–8. https://doi.org/10.2165/00148581-200709030-00002. Cited 2022 Sept 5
Choudhary TS, Reddy NS, Apte A, Sinha B, Roy S, Nair NP et al (2019) Delayed vaccination and its predictors among children under 2 years in India: insights from the national family health survey–4. Vaccine. 37(17):2331 (Cited 2022 Sep 16. Available from: /pmc/articles/PMC6996155/)
Baktır Altuntaş S, Kara Elitok G (2022) Routine pediatric vaccination during pandemic: attitudes of parents. Turk Arch Pediatr. 57(3):342–8 (Cited 2023 July 17. Available from: https://www.turkarchpediatr.org/en/routine-pediatric-vaccination-during-pandemic-attitudes-of-parents-131371 )
Vyas S, Sharma N, Archisman Roy P, Kumar R (2021) Repercussions of lockdown on primary health care in India during COVID 19. J Fam Med Prim Care. 10(7):2436 (Cited 2022 Sep 16. Available from: /pmc/articles/PMC8415688/)
Lee DID, Vanderhout S, Aglipay M, Birken CS, Morris SK, Piché-Renaud PP et al (2022) Delay in childhood vaccinations during the COVID-19 pandemic. Can J Public Heal. 113(1):126–34 (Cited 2022 Sep 16. Available from: https://springerlink.fh-diploma.de/article/10.17269/s41997-021-00601-9 )
Chandir S, Siddiqi DA, Mehmood M, Setayesh H, Siddique M, Mirza A et al (2020) Impact of COVID-19 pandemic response on uptake of routine immunizations in Sindh, Pakistan: an analysis of provincial electronic immunization registry data. Vaccine. 38(45):7146–55 (Cited 2022 Sep 16. Available from: https://pubmed.ncbi.nlm.nih.gov/32943265/ )
Acknowledgements
We would like to thank all the study participants for their cooperation.
Funding
It is self-funded by authors with no external funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to conception, design and drafting the manuscript. SSD, RVK and VBW contributed to development of research tool and procedure. RVK acquired the data. VBW analysed the data. SSD and VBW contributed to interpretation of data and writing the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional ethical committee of approval, permissions from the relevant authorities and the written informed consent from each participant were acquired. Institutional ethical committee of Bharati Vidyapeeth (Deemed to be) University Medical College & Hospital, Sangli, approved the project by IEC approval letter ref: BV(DU)MC&H/Sangli/IEC/440/21. Dated: 17 August 2021.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Master chart in Excel.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dhanawade, S.S., Kawade, R.V. & Waghachavare, V.B. Childhood immunization delay during the first wave of COVID-19 in an urban area of Sangli district from Maharashtra, India: a cross-sectional study. Egypt Pediatric Association Gaz 71, 51 (2023). https://doi.org/10.1186/s43054-023-00197-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-023-00197-4