Abstract
Background
Leiomyosarcoma (LMS) of vascular origin is a rare entity of soft tissue sarcomas. Although they arise mostly from retroperitoneal major vascular structures, some encountered cases may arise from the smaller vascular structures of the thigh as the femoral vein. Due to their origin from the vascular structures, they represent a diagnostic challenge as they may be misdiagnosed as deep vein thrombosis (DVT).
Case presentation
We present a case of a 45-year-old woman with left femoral and iliac vein LMS that was previously described in the vascular ultrasound (US) report as extensive DVT involving the femoral and external iliac veins. The patient did not improve after receiving the prescribed anticoagulants. Seven months later, the patient underwent computerized tomography (CT) with contrast, revealing a soft tissue mass in the anatomical site of the left common femoral and external iliac veins. The patient underwent both US-guided tru-cut biopsy and incisional biopsy from the iliac lymph nodes which revealed leiomyosarcoma.
Materials and methods
The patient underwent both vascular ultrasound and magnetic resonance imaging of the pelvis and the left thigh at the time of the first presentation. Seven months later, she underwent contrast-enhanced CT of the abdomen and pelvis.
Outcome
The patient was referred to the oncology department to receive the appropriate chemotherapy protocol as the tumor was inoperable.
Conclusions
Although leiomyosarcoma of vascular origin is a rare entity of neoplasms, it is usually underestimated. A high index of suspicion would help the clinician to suspect such a neoplasm and save time for early diagnosis and management. Special caution should be taken for patients with venous thrombosis not improving on anticoagulants. When there is suspicion, other modalities such as computerized tomography and magnetic resonance imaging help confirm the diagnosis.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Vascular leiomyosarcomas are a rare subtype of leiomyosarcoma affecting the vascular structures [1,2,3]. It mainly affects the venous rather than the arterial system [1, 4]. They mostly arise from the retroperitoneal vascular structures particularly the inferior vena cava [IVC] [4, 5]. As with other types of soft tissue sarcomas, the presentation may be delayed due to the deep origin of the neoplasm. The presenting symptom is usually lower limb edema due to venous stasis and recurrent DVT [3]. It may be also presented by deep-seated pain or distal embolism [4]. The tumor tends to progress slowly, invade the surrounding soft tissue, and metastasize within the circulation. It has a relative female predilection [male:female = 1:4] [5].
While a mass in the femoral triangle is relatively common most of which are benign conditions, LMS of the common femoral vein is exceedingly rare [6]. Differential diagnosis includes lymphadenopathy, hernias, femoral artery aneurysms, and saphena varix [6]. LMS of the femoral vein can result in lower limb edema and pain, so it is difficult to differentiate from DVT. Although the ultrasonographic features of LMS of the vein have been reported in some cases, no studies have described specific features of vascular LMS [7].
The diagnosis of LMS is usually delayed because the majority of the patients remain asymptomatic for a long time. LMS has an extremely poor prognosis, with 5-year malignancy-free survival rates between 30 and 50% after a wide surgical excision [2]. Early diagnosis of this tumor is important to save the patient the time necessary for surgical excision. The pitfall of misdiagnosing this tumor as DVT is a useful reminder [7].
The ultrasonographic features of LMS by B-mode are fairly indistinguishable from those of DVT. It usually manifests as a hypoechoic mass within the lumen of the vein. The involved vein usually appears dilated with a thickened wall. By color Doppler (CD), LMS may show color spots and linear vascularity within the hypoechoic mass filling the vein lumen. By pulsed-wave Doppler (PWD), the mass usually shows arterial vascularity inside [7, 8].
Contrast-enhanced CT (CECT) is very useful in the diagnosis of deeply seated lesions. LMS usually appears as a heterogeneous mass within the lumen of the vein that enhances in the arterial phase. In the case of extra-venous extension, the vein may not be visualized (being completely infiltrated by the mass). LMS may also exert pressure and invade the surrounding organs [7, 8].
Leiomyosarcomas in MRI usually display low to intermediate signals in their solid parts in T1-weighted images and high signals in T2-weighted images. Black blood images may also be useful in the assessment of the extent of intravascular extension. In case of hemorrhagic changes within the mass, areas of hemorrhage may display high signals in both T1- and T2-weighted images [9].
Case presentation
Case history
A 45-year-old woman presented to our vascular surgery department with left lower limb edema. The patient underwent vascular ultrasound of the left lower limb which revealed dilated left common femoral and external iliac veins with hypoechoic content inside. The patient did not have any risk for increased coagulability, so MRI of the pelvis was ordered to exclude any pelvic mass compressing the venous system. The MRI revealed markedly dilated left common femoral and external iliac veins with heterogeneous signals inside (Fig. 1). No definite pelvic masses were detected, so the patient was diagnosed with extensive DVT and was prescribed anticoagulants. The patient was arranged for future visits for the follow-up of her DVT. During that period, the patient’s prothrombin time (PT) was 13.9 s and the international normalized ratio (INR) was kept between 1.4 and 1.6. The patient’s platelet count was 262 k/uL.
[MRI of the pelvis]: a Axial T1 WIs showing dilated left external iliac vein with intermediate SI (green arrowhead), b axial T2 WIs showing dilated left external iliac vein with alternating high and intermediate signal inside its lumen (blue arrowhead), c, d sequential coronal STIR images showing the dilated left external iliac and common femoral veins with internal mixed high and low signal within their lumen (yellow arrowheads)
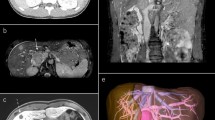
The patient’s symptoms did not improve during the next seven months. Another vascular ultrasound was ordered to follow up the extension of the DVT. The ultrasound revealed progressive dilatation of the venous system with a mass-like structure extending outside the lumen with areas of cystic degeneration. CD revealed color spots within the solid portions of the lesion with arterial wave by PWD. The patient underwent CECT which revealed heterogeneously enhancing mass in the arterial phase totally encasing the external iliac vessels with non-visualization of the common femoral and external iliac veins (Fig. 2). The CT also revealed multiple suspicious-looking regional lymph nodes (Fig. 3a) and distant metastatic spread in the form of multiple non-enhancing hepatic focal lesions (Fig. 3b), pulmonary nodules (Fig. 3c), and necrotic left hilar lymph node (Fig. 3d).
[Multislice post-contrast CT of the pelvis (arterial phase)]: a Axial image showing a heterogeneously enhancing mass in the anatomical site of the left external iliac vein totally encasing the normally enhancing left external iliac artery (red arrowhead), b axial image showing the previously mentioned mass partially encasing the left common femoral artery (light blue arrowhead), c, d sequential coronal images showing the longitudinal extent of the mass, as well as the relation between the mass and the normally enhancing left external iliac and common femoral arteries (orange arrowhead)
[Post-contrast Multislice CT]: a Axial image showing necrotic suspicious looking inguinal lymph node adjacent to the mass (red arrowhead), b axial image of the abdomen showing non-enhancing hepatic focal lesion in segment VII (white arrowhead) and an incidentally noted tiny hepatic cyst in segment VIII (yellow arrowhead), c axial image of the lower chest (lung window) showing a solid pulmonary nodule of the left lung base (blue arrowhead), d axial image of the chest (mediastinal window) showing necrotic left hilar lymph node (green arrowhead)
Biopsy and pathology
The patient underwent a tru-cut biopsy from the mass. Microscopic examination of the slides prepared from the sample revealed malignant spindle/pleomorphic cell proliferation with high-grade nuclear atypia, pleomorphism, and hyperchromasia. The pathologist recommended another larger biopsy for the completion of immunohistochemistry (IHC). Another incisional biopsy was obtained from the left external iliac lymph nodes and sent for microscopic examination which revealed malignant spindle cell proliferation arranged into fascicles of atypical spindle-shaped cells with hyperchromatic nuclei and a high degree of atypia. IHC for smooth muscle actin (SMA) and H-Caldesmon revealed diffuse positive reaction in the tumor cells (Fig. 4). The final diagnosis was leiomyosarcoma of the femoral vein.
(Microscopic pictures): a The tumor showed malignant spindle cell proliferation with areas of necrosis (H&E, × 40), b the component cells showed a high degree of cytologic atypia and pleomorphism with frequent mitotic figures (H&E, × 200), c, d the component cells showed positive cytoplasmic reaction for both SMA and H-Caldesmon, respectively (SMA & H-Caldesmon, × 200 & 100 , respectively)
Multi-disciplinary team (MDT) decision
The patient was referred to the oncology department to receive the appropriate protocol of chemotherapy on account of inoperability based on the radiological findings which revealed distant metastases.
Materials and methods
-
The Doppler ultrasonography examination was performed by (TOSHIBA Aplio 500) using both a linear array transducer (7.5 MHZ) for examination of the common femoral vein and a curvilinear (3.5 MHZ) transducer for examination of the external iliac vein.
-
The CECT examination was performed by the multidetector CT scan (GE-healthcare).
-
The MRI examination of the pelvis was performed by a 1.5-Tesla scanner (Siemens Magnetom Aera). The patient was positioned supine in the magnetic bore.
Discussion
Leiomyosarcomas of vascular origin are a rare form of soft tissue sarcomas [10]. They usually arise from venous structures rather than arterial vascular structures [1, 4, 10]. They represent a diagnostic challenge since they mimic to a great extent the symptoms of DVT [7, 8].
Leiomyosarcoma of vascular origin is more prevalent in females than in males [5]. In our case, the patient is female agreeing with the case reports presented by (Attila Maria Pizzini and Cesare Tripolino) and those presented by both (Zhang M., et al.) and (Yingjiang Xu) in which the patient was also a female.
The median age of presentation of leiomyosarcomas is 56 years with age ranges between 33 and 61 [5]. The patient in our case was 45 years at the time of presentation agreeing with the age range of the patients presented in the case report of (Attila Maria Pizzini and Cesare Tripolino) in which the patient’s age was 49 years and the one presented by (Zhang M., et al.) in which the age of the patient was 55 years.
In our case, the origin of the LMS was the common femoral vein. Although LMS of the femoral vessels are relatively less common than those arising from the IVC, this comes in agreement with other case reports presented by both (Zhang M., et al.) and (Yingjiang Xu) in which the origin of the LMS was the femoral vein as well.
There are three known patterns of tumor growth for vascular LMS: extraluminal (outside the vessel) which represents the most common form, intraluminal (inside the vessel), and mixed pattern [6, 11]. In our case, the mass showed a mixed (intra- and extraluminal) growth pattern. This agrees with the case presented by (Gonzalez-Cantu Y.M., et al.) in which the mass showed a mixed growth pattern. On the other hand, the case presented by (Yingjiang Xu) showed an intraluminal pattern of growth.
In the case report we present, the patient’s complaint was lower limb edema which is usually the presenting symptom in case of LMS of vascular origin [7, 8] as mentioned by (Gonzalez-Cantu Y.M., et al.) and those mentioned by (Attila Maria Pizzini and Cesare Tripolino), (Zhang M., et al.) and (Yingjiang Xu).
The patient in our case underwent an ultrasound examination as the primary investigation which was the primary investigation done in the cases presented by both (Zhang M., et al.) and (Yingjiang Xu). However, in our study, the patient underwent additional MRI in search of pelvic masses. Although MRI is highly sensitive for the diagnosis of pelvic masses, neoplastic lesions of vascular origin could be mistaken for extensive DVT with vein dilatation. Hence, a high index of suspicion is crucial to pick up such lesions.
Color spots by CD and arterial wave by PWD are important findings as they represent newly formed arteries which are key findings to differentiate between benign thrombus and LMS. In concordance with the findings of the case report presented by (Zhang M., et al.), Doppler ultrasound revealed arterial vascularity within the thrombosed portion of the vein in our case. Therefore, ultrasound examination based merely on B-mode in case of suspected DVT is not sufficient and CD is crucial for early diagnosis of vascular sarcomas.
In agreement with (Zhang M., et al.), the CECT performed in our case revealed a heterogeneous mass along the course of the femoral and external iliac vein with preferential enhancement in the arterial phase. In line with previous studies [7, 12], triphasic CT with adequate bolus timing is necessary to confirm the enhancement of the thrombus in the arterial phase reflecting the neoangiogenesis and the vascular nature of the tumor.
Conclusions
-
Although leiomyosarcomas are relatively uncommon, they are always underestimated as benign deep vein thrombosis.
-
The use of color Doppler and pulsed-wave Doppler is very important for the early detection of tumors of vascular origin.
-
The presence of color spots particularly arterial wave within a thrombus is an alarming sign for further investigation to exclude tumors of vascular origin.
-
An early vascular leiomyosarcoma may be overlooked in the MRI examination and misdiagnosed as a benign deep vein thrombus.
-
Triphasic CT with adequate bolus timing is essential to demonstrate arterial enhancement within the malignant thrombus in the arterial phase.
Limitations
-
The ultrasound images of the lesion could not be provided as they were not uploaded to our picture archiving and communication system (PACS).
-
Contrast-enhanced ultrasonography (CEUS) was not used. The addition of such investigation would have been of great value in the differentiation between benign and malignant thrombosis.
Recommendations
Great caution should be taken while performing an ultrasound examination of the venous system. The operator should have a high index of suspicion, particularly in the absence of risk factors for DVT.
Availability of data and materials
The data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- LMS:
-
Leiomyosarcoma
- DVT:
-
Deep vein thrombosis
- US:
-
Ultrasound
- CT:
-
Computerized tomography
- MRI:
-
Magnetic resonance imaging
- CD:
-
Color Doppler
- PWD:
-
Pulsed wave Doppler
- IVC:
-
Inferior vena cava
- WIs:
-
Weighted images
- PT:
-
Prothrombin time
- INR:
-
International normalized ratio
- IHC:
-
Immunohistochemistry
- SMA:
-
Smooth muscle actin
- MHZ:
-
Megahertz
- PACS:
-
Picture archiving and communication system
References
Roland CL, Boland GM, Demicco EG, Lusby K, Ingram D et al (2016) Clinical observations and molecular variables of primary vascular leiomyosarcoma. JAMA Surg 151(4):347–354
Al-Saif OH, Sengupta B, Amr S, Meshikhes AW (2011) Leiomyosarcoma of the infra-renal inferior vena cava. Am J Surg 201(2):e18–e20
González Valverde FM, Gómez Ramos MJ, Torregrosa N, Molto M, Vázquez Rojas JL (2009) Leiomyosarcoma of the iliac vein. Ann Vasc Surg 23(4):536.e5-536.e8
Tilkorn DJ, Hauser J, Ring A, Goertz O, Stricker I et al (2010) Leiomyosarcoma of intravascular origin—a rare tumor entity: clinical pathological study of twelve cases. World J Surg Oncol 8(1):103
Zhang H-X, Wang K, Hong P, Lu M, Liu Z et al (2021) Clinical experience with the treatment of retroperitoneal vascular leiomyosarcoma originating from large veins. BMC Surg 21(1):326
Xu Y, Xie W, Shang DJV (2021) Primary leiomyosarcoma is a rare cause of femoral triangle mass: a case report. Vascular 29(3):468–471
Zhang M, Yan F, Huang B, Wu Z, Wen X (2017) Multimodal ultrasonographic assessment of leiomyosarcoma of the femoral vein in a patient misdiagnosed as having deep vein thrombosis: a case report. Medicine 96(46):e8581
Pizzini AM, Tripolino C (2021) Femoral vein leiomyosarcoma mimicking thrombosis. Ann Vasc Surg 74:520.e19-520.e22
Marko J, Wolfman DJ (2018) Retroperitoneal leiomyosarcoma from the radiologic pathology archives. Radiographics 38(5):1403–1420
Gonzalez-Cantu YM, Tena-Suck ML, Serna-Reyna S, Sánchez-Maldonado H, Quintanilla-Garza S et al (2015) Leiomyosarcoma of vascular origin: case report. Case Rep Clin Pathol 2(4):60
Díaz PA, Montoya MIP, Cuartas CP, Vélez MIC (2021) Leiomyosarcoma of the inferior vena cava. What to look for in the images? Presentation of a case. Rev Colomb Radiol 32(3):5616–5621
Perisano C, Maffulli N, Colelli P, Marzetti E, Panni AS et al (2013) Misdiagnosis of soft tissue sarcomas of the lower limb associated with deep venous thrombosis: report of two cases and review of the literature. BMC Musculoskelet Disord 14(1):1–6
Acknowledgements
Not applicable.
Funding
The authors declare that they have no funding sources.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript for publishing. MS analyzed the patient’s data, prepared the figures, and wrote the main body of the case report. MF revised the case report during different stages of writing. AH prepared the microscopic pictures for the lesion and wrote the pathology report. MG revised the case report, provided literature sources, and contributed to the evaluation of radiological findings.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
An informed consent was obtained from the patient.
Consent for publication
An informed consent was obtained from the patient to use the necessary data for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ayyad, M.S., Elbellasy, M.F., Hassan, A. et al. Leiomyosarcoma of vascular origin: lessons learned from misdiagnosis. Egypt J Radiol Nucl Med 55, 166 (2024). https://doi.org/10.1186/s43055-024-01336-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01336-6