Abstract
Background
Addressing knowledge and concerns related to corticosteroid is essential to enhance patient care, promote optimal utilization, and minimize their potential side effects.
Methods
A cross-sectional study was conducted to assess knowledge and attitudes regarding corticosteroid use among healthcare providers (HCPs) in the United Arab Emirates using a validated questionnaire. Knowledge, attitudes, and fear items were described as frequency and percentages. Then, a total score was calculated; multilinear regression was used to see the effect of demographics on these scores.
Results
Among 129 HCPs, 100 had previously prescribed corticosteroids (77.5%), with intranasal spray being the most dispensed dosage form (89.0%). Respiratory diseases were the most reported indication for corticosteroid dispensing (93.0%). HCPs preferred corticosteroids for their ability to quickly relief of patients' symptoms (67.0%). About 60.0% identified increased appetite as a patient-reported side effect. The assessment of the HCPs' knowledge showed a median score of 10 out of 11 (IQR = 9–11). The median fear score was six out of 10 (IQR = 4–10), but they were significantly and conversely related to each other.
Conclusion
This study revealed that while HCPs in the UAE possess substantial knowledge regarding corticosteroid use, their concerns, particularly around side effects, indicate a need for further education. Addressing these concerns through targeted educational programs could enhance the safe and effective utilization of corticosteroids, ultimately improving patient care outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Corticosteroids (CSs), known as “magic bullets”, are one of the most commonly used drugs worldwide [28]. Corticosteroids exert an effective immune suppression property and are indicated as a cornerstone in treating a wide range of acute and chronic diseases, ranging from allergic rhinitis, to eczema, asthma, colitis, and lupus [13]. In spite of their integral role in managing inflammatory and immunologic disorders, their use might be associated with detrimental consequences, especially with long-term use of high doses. The potentially corticosteroids associated risks range from minor adverse drug reactions to serious hazards such as cardiovascular, musculoskeletal, digestive, endocrine, ophthalmic, and neurological disorders [20].
Optimal clinical and safety outcomes are positively correlated with patients' knowledge and awareness about the inherent risks associated with the use of corticosteroids. Studies have shown that patients have less than adequate level of awareness of corticosteroid indications, side effects, dosage administration, and cautions [14, 21], which may be partially attributed to factors associated with healthcare professionals (HCPs), such as nonoptimal HCP education and failure of HCP-patient communication. According to a previous study, increased workload, inadequate time, and attention provided by healthcare professionals to patients have greatly influenced patients’ knowledge and awareness about corticosteroids [18]. Thus, it is essential to actively engage both patients and healthcare providers to ensure a comprehensive understanding of the recommended use of corticosteroids and any associated risks. The primary mission of both physicians and pharmacists should be to secure optimal therapeutic outcomes by ensuring accurate prescription and appropriate dispensing [17]. Pharmacists' duties are not restricted to medication dispensing, but also to properly provide medication education and counseling to guarantee safe and effective use of prescribed corticosteroids. Conversely, physicians are responsible of prescribing, monitoring, and managing the potential side effects of corticosteroids. As a result, healthcare providers' familiarity with and understanding of corticosteroids are essential for achieving the intended therapy goals, as misinformation would lead to undesirable outcomes [32]. Pharmacists and physicians should emphasize the most pertinent side effects, enhance patient education, and provide comprehensive training based on their experience to ensure the optimal therapeutic outcome for patients [22].
To date, various population-based studies have assessed knowledge and attitudes concerning corticosteroids both on local and international levels. However, their findings were limited to the general population rather than incorporating insights from healthcare professionals [2]. In the UAE, corticosteroids are frequently prescribed, particularly for respiratory and dermatological conditions; yet, the knowledge and confidence of healthcare providers in prescribing these medications remain under-explored. But so far, no study has investigated the healthcare professional knowledge and perception of corticosteroids in the United Arab Emirates (UAE). Understanding the level of knowledge and fear about corticosteroid-containing drugs is important since it will improve patient care, ensure optimal utilization, and minimize unwanted side effects. This is a national study that aims to assess the knowledge, awareness, and attitudes about corticosteroid use among different healthcare professionals in the United Arab Emirates.
Methods
Study design, setting, and population
A cross-sectional study was conducted between February and October 2023. Healthcare providers were recruited using a convenience-based, snowball sampling method. Any healthcare provider (Physicians and pharmacists) in the United Arab Emirates (UAE) expressing willingness to answer the survey was considered eligible to participate in the study. The study's survey was distributed mainly through WhatsApp, Facebook, and LinkedIn. Participation was entirely voluntary and anonymous.
A written consent statement was presented at the beginning of the study's survey, stating, "Your participation in completing the current survey is highly appreciated". Potential participants indicated their consent by choosing to complete the survey, and researchers regarded this as informed consent to partake in the study. Ethical approval was granted by the Research Ethics Committee of the affiliated University (approval number: ERSC_2022_1886).
Study tool
The study questionnaire was developed following the fundamental principles of effective survey design [5] and was informed by previously validated surveys in the literature [1, 2, 5, 7, 10]. To ensure its relevance and accuracy, a comprehensive pool of questions was compiled to align with the study's objectives. The content validity of the questionnaire, which was prepared in English, was evaluated by five academic experts. A pilot test was conducted with five participants to assess the clarity and comprehension of the items. Based on the feedback, necessary linguistic adjustments were made to enhance the questionnaire's clarity. The pilot responses were excluded from the final analysis to maintain data integrity. The final version of the questionnaire was distributed electronically, and the internal consistency of the scale was confirmed with a Cronbach's alpha of 0.85, indicating high reliability and validation of the study tool.
The survey was structured into five sections, each containing close-ended questions. The first section focused on sociodemographic items. The second section addressed HCPs' perceptions toward CS dispensing corticosteroids. The third section assessed participants' knowledge regarding corticosteroids, while the fourth section assessed corticosteroids dispensing phobias/fears. Lastly, the fifth section assessed participants' preference for alternative products over corticosteroids.
The study's survey was written in English and evaluated by three independent academics. They assessed the survey content for both clarity and face validity, ensuring that all items were easily understood and clear. Subsequently, a pilot study was conducted before distributing the survey (n = 15). The responses from the pilot study were not taken into consideration in the final study's analysis.
Sample size calculation
The sample size for this study was calculated using the OpenEpi software, based on an estimated population of 13,000 healthcare providers in the United Arab Emirates [16]. A confidence level of 90% and a margin of error of 7% were chosen to achieve a balance between statistical power and practical feasibility, resulting in a target sample size of 169 participants. This sample size was considered sufficient to provide reliable estimates while accounting for the exploratory nature of the study. The margin of error was slightly adjusted to accommodate recruitment constraints while ensuring that the sample remained representative of the broader population. The final sample of 169 healthcare providers is reflective of the diverse demographics within the UAE healthcare system, ensuring robust and generalizable findings.
Statistical analyses
Data obtained from Google Forms were extracted into an Excel sheet and subsequently transferred to Statistical Package for the Social Sciences version 25.0 (IBM SPSS Statistics for Windows, version 25, IBM Corp., Armonk, N.Y., USA). Continuous variables were presented as medians and interquartile range (IQR), while categorical variables were presented as frequency and percentages.
Multiple linear regression was performed to screen for the independent factors affecting the participants' knowledge about corticosteroids. Simple linear regression was conducted first, and any variable that exhibited significance (p < 0.25) was then included in the multiple linear regression analyses. The selection of variables involved checking their independence, with tolerance values > 0.1 and variance inflation factor (VIF) values < 10 confirming the absence of multicollinearity between independent variables. No variables displayed multicollinearity, leading to the retention of all variables. Statistical significance was considered at p ≤ 0.05.
Results
Demographics
Among 169 HCPs, 129 agreed to participate in this study (response rate = 76%). The median age for the study's participants was 46 years (IQR = 36.5–55). More the half of the HCPs were females (58.9%), and the majority resided in urban areas (84.5%). Regarding the workplace, 63.6% of the HCPs were employed in hospitals, with approximately half of them working in the private sector. Among the HCPs, 42.6% were in Abu Dhabi (n = 55), followed by 27.9% in Dubai (n = 36). Most of the HCPs (82.2%) were pharmacists (Table 1).
One hundred HCPs (77.5%, n = 100) have previously prescribed corticosteroids (Table 2). Furthermore, as shown in Fig. 1, the most frequently reported corticosteroid dosage form dispensed by them was intranasal spray (89%), followed closely by inhaler/nebulizer (87%), then ointment/cream (84%).
More than half of the HCPs identified respiratory conditions (e.g., COPD and asthma), dermatological diseases (e.g., eczema), and joint or rheumatological diseases as the primary indications for dispensing corticosteroids (93%, 82%, and 59%, respectively; Table 2).
Concerning the reasons for corticosteroid preference (Table 2), "Quick relief for patients’ symptoms" was the most reported reason (67%), followed by "According to guidelines and literature, it is the most effective treatment for the most common cases I have" at (60%), and "According to my experience, it is the most effective treatment for the most common cases I have" at (49%).
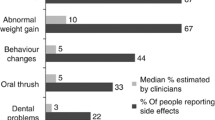
As listed in Table 2, among the HCPs, 59% reported increased appetite as a patient-reported side effect. This was followed by an increased infection risk (56%), as well as mood changes/swings and depression (55%).
Healthcare providers knowledge
The assessment of the HCPs' knowledge revealed a median knowledge score of 10 out of 11, with an IQR ranging from 9 to 11 (Table 3). The most correctly answered item among the knowledge items was "Corticosteroids are used to treat various health conditions (e.g., asthma, eczema, COVID-19, etc.)", with 97.7% (n = 126) providing correct answers. This was followed by "The used dose needs to be reduced slowly over a few weeks or months before stopping Corticosteroids if you have been taking them for a long time" at (96.9%, n = 125), and "Corticosteroids are anti-inflammatory medicine" at 95.3% (n = 123). Moreover, weight gain and increased risk of infections were identified correctly by more than 90.0% (n = 126 and 119; respectively) of the HCPs as potential side effects of long-term treatment (Table 3).
Fear score
The assessment of the fear score revealed a median of six out of 10, with an IQR ranging from 4 to 10. The risk of hyperglycemia among their patients was the most reported reason for fear of prescribing corticosteroids (81.4%). The second most reported reason was increased blood pressure among their patients, as it was reported by 74.4% of the HCPs (Table 4).
Regarding HCPs' preference toward using alternatives to corticosteroids, more than half of them expressed a preference for traditional therapy (n = 73), while 38.8% of the HCPs reported using any other medicine rather than corticosteroids, and 30.2% reported using herbal therapy (Fig. 2).
Multilinear regression analysis revealed that the fear score was negatively and significantly associated with the knowledge score (p value = 0.002, OR = 0.27, 95% CI 0.05–0.20), after accounting for major, specialty and workplace (Table 5).
Discussion
Statement of principal findings
The majority of HCPs who participated in this study had previously prescribed/dispensed CSs (77.5%). Respiratory diseases were the most reported indication, followed by dermatologic conditions, with intranasal spray, inhalers/nebulizers, and ointments/creams being the most dispensed dosage forms; respectively. HCPs preferred corticosteroids for their ability to quickly relief of patients' symptoms (67.0%) and guideline recommendations (60%). The mostly commonly patient-reported side effects were appetite increase, rise in infections risk, and mood changes. The assessment of the HCPs' knowledge showed a median score of 10 out of 11 (IQR = 9–11). The median fear score was six out of 10 (IQR = 4–10), but they were significantly and conversely related to each other.
Strengths and limitations
The study is the first in the Gulf region to address knowledge about CSs, in addition to fears and concerns regarding their utilization by HCPs, using a validated tool. Nevertheless, the study is marked by several limitations, including the relatively small sample size of participants. The electronic administration of questionnaires introduces potential concerns regarding the authenticity of responses and is influenced by factors such as computer literacy and information bias. Additionally, the utilization of a snowball sampling technique raises concerns about election bias, as the absence of random selection may affect the broader generalizability of the study's findings.
Interpretation within the context of the wider literature
CSs have been extensively associated with a diverse range of local and systemic side effects, such as clarified in the existing literature [11, 29, 32]. Serious consequences, including suppression of the hypothalamic-pituitary axis and susceptibility to severe, life-threatening infections, are prominently associated with prolonged administration of supraphysiologic doses of corticosteroids [19, 32]. However, fractures, gastrointestinal bleeds, and cataracts have been documented following extended use of low-to-moderate doses of glucocorticoid [9, 15, 32]. Furthermore, certain side effects induced by corticosteroids exhibit a linear dose–response pattern, where the incidence escalates with increasing dosage, exemplified by cushingoid symptoms and leg edema. Conversely, other side effects exhibit a threshold dose–response pattern, showing an elevated frequency of events beyond a specific threshold dose, as seen in weight gain and glaucoma [32].
Curtis et al. [8] conducted a study aiming to investigate the incidence of side effects in patients on long-term low-dose glucocorticoid therapy in the US population. Among 2446 participants, the majority reported ever discussing a corticosteroid-induced side effect with their primary care provider, with weight gain being the most reported side effect. This aligns with the findings of the current study, where weight gain was also the most reported side effect in patients taking corticosteroids. Moreover, the scientific literature reports a considerable occurrence of more severe side effects, including osteoporosis and fractures, with frequencies reaching as high as 40.0% in patients undergoing long-term steroid therapy [12, 31]. The outcomes from the current study indicate a comparable incidence of patient-reported osteoporosis, with 37.0% of the HCPs noting that their patients developed this condition.
Due to the inherent complexity in predicting the occurrence of corticosteroid-induced side effects, HCPs tend to exercise increased vigilance, often leading to a reluctance in prescribing corticosteroids, a phenomenon commonly referred to as “Corticosteroid Phobia”. In a recent Egyptian study, it was observed that at least one-third of the study population had no prior experience in prescribing or dispensing corticosteroids in any dosage form [3], this difference with our results can be related to the workplace difference, as most HCPs were working in a community pharmacy, unlike our sample with majority of pharmacists is hospital-based. Therefore, the present study revealed a higher tendency of prescribing/dispensing, with 77.5% throughout their professional careers. Remarkably, the predominant use of corticosteroids in this study involved topical formulations, with high percentages of all HCPs prescribing or dispensing corticosteroids for the management of respiratory and dermatologic conditions. This preference for topical corticosteroids can be related to the perceived lower risk of side effects as compared to systemic therapy, oral high prevalence of immunologic dermatology diseases in the UAE [22].
Despite the well-established therapeutic role of corticosteroids in treating diverse immunological disorders such as inflammatory bowel diseases (IBD) and rheumatoid arthritis (RA) [6, 23], the present study revealed a notable disparity; as around half of all HCPs participated in the prescribing or dispensing of CSs for cases of GIT immunological disorders and joint/rheumatologic diseases. Existing literature indicates that pharmacists may lack comprehensive knowledge regarding the role of corticosteroids in managing these specific immunological conditions and is often reluctant to manage them [6, 23]. Given that a substantial proportion of participants comprised practicing pharmacists (82.2%), this finding likely reflects the observed patterns within the current study.
Glucocorticoids are acknowledged for causing unpredictable spikes in plasma glucose levels, leading to the development of hyperglycemia [4, 25]. Effectively managing the hyperglycemic response poses a significant challenge [4]. Consequently, 81.4% of the HCPs exhibits reluctance toward corticosteroid use, primarily driven by the perceived risk of hyperglycemia. This hesitation is evident in the elevated median fear score of 6 observed among HCPs. Significantly, around 39.0% of the participants express a preference for alternative products, even if they involve higher costs, highlighting the widespread reluctance in prescribing or dispensing corticosteroids within our study cohort.
Corticosteroids are extensively documented in the scientific literature for their prompt anti-inflammatory efficacy and quick relief of patients’ symptoms [12]. This was the primary rationale behind preference of HCPs in the prescription/dispensation of corticosteroids over alternative options. Despite that the study's findings revealed a high median knowledge of corticosteroids score at 10 [2, 12, 23], caution is advised against their excessive use, due to the potential for multiple side effects [27, 30]. This caution is particularly pertinent in chronic inflammatory disorders such as IBD and RA, where corticosteroids serve as a temporary bridge, and more effective long-term maintenance options exist [6, 23]. Thus, careful evaluating of each patient's situation is crucial for the careful optimization of management plans.
In the investigation conducted by Barakat and colleagues (2023), the average knowledge score of HCPs in Egypt was 8.7 out of 14 [3]. The current study in the United Arab Emirates (UAE), HCPs demonstrated rather superior knowledge regarding the of corticosteroids and their associated side effects, illustrated by a substantial median knowledge score of 10 [2, 12, 23]. The acquisition of knowledge enhances an individual's self-awareness and self-care. As anticipated, there is a significant negative correlation between corticosteroid phobia and knowledge, evident in both single and multilinear regression analyses. Additionally, a recent study has established a correlation between the possession of a university degree and steroid phobia [24].
Interestingly, corticosteroid phobia is closely tied to various factors in the literature, particularly the fear of experiencing side effects [12, 26, 29]. The current study highlights that, specifically for the Emirati population, the most significant concerns leading to corticosteroid phobia revolve around the potential risks of corticosteroid associated hyperglycemia and hypertension. Unlike prior studies, this research highlights a significant negative correlation between corticophobia and knowledge levels among UAE healthcare providers, a novel finding that underscores the need for targeted educational interventions. In other words, the lack of knowledge among HCPs is not the primary factor in the development of corticophobia. Hence, establishing a robust, formal, reassuring relationship between patients and caregivers is crucial to effectively convey this knowledge, educate patients, and prevent the emergence of corticophobia.
Implications for policy, practice, and research
Findings form this study underscores the need for comprehensive education initiatives aimed at bridging this gap and fostering informed decision making among healthcare professionals and patients alike. By fostering a deeper understanding of CS use and addressing concerns proactively, healthcare providers can play a pivotal role in promoting safe and effective utilization of CSs for various indications, ultimately improving patient outcomes and quality of life. The study's limitations include a relatively small sample size, which may limit generalizability, and a higher representation of pharmacists compared to physicians, potentially skewing the results. Larger future studies should be performed to confirm these findings, and the effect of CS awareness campaigns on reducing HCPs’ fears and concerns regarding CS use can be longitudinally evaluated.
Conclusions
This study showed that HCPs have a good knowledge about CSs in general; yet, they had some concerns and fears regarding CS prescribing/dispensing. Regarding CS’ side effect, however, there was a moderate knowledge gap among HCPs, despite their superior knowledge compared to counterparts in other regions.
Data availability
Not applicable.
Abbreviations
- HCPs:
-
Healthcare providers
- CS:
-
Corticosteroid
- IBD :
-
Inflammatory bowel diseases
- RA :
-
Rheumatoid arthritis
- UAE :
-
United Arab Emirates
References
Ahmad DS, Wazaify MM, Albsoul-Younes A (2014) the role of the clinical pharmacist in the identification and management of corticophobia–an interventional study. Trop J Pharm Res 13(3):445–453
Barakat M, Elnaem MH, Al-Rawashdeh A, Othman B, Ibrahim S, Abdelaziz DH et al (2023) Assessment of knowledge, perception, experience and phobia toward corticosteroids use among the general public in the era of COVID-19: a multinational study. Healthcare 11(2):255
Barakat M, Mansour NO, Elnaem MH, Thiab S, Farha RA, Sallam M et al (2023) Evaluation of knowledge, experiences, and fear toward prescribing and dispensing corticosteroids among Egyptian healthcare professionals: a cross-sectional study. Saudi Pharm J 31(10):101777
Barker HL, Morrison D, Llano A, Sainsbury CA, Jones GCJDT (2023) Practical guide to glucocorticoid induced hyperglycaemia and diabetes. Diabetes Therapy 14(5):937–945
Boynton PM (2004) Administering, analysing, and reporting your questionnaire. BMJ 328(7452):1372–1375
Chang L, Sultan S, Lembo A, Verne GN, Smalley W, Heidelbaugh JJ (2022) AGA clinical practice guideline on the pharmacological management of irritable bowel syndrome with constipation. Gastroenterology 163(1):118–136
Choi E, Chandran NS, Tan C (2020) Corticosteroid phobia: a questionnaire study using TOPICOP score. Singap Med J 61(3):149
Curtis JR, Westfall AO, Allison J, Bijlsma JW, Freeman A, George V, Saag KG (2006) Population-based assessment of adverse events associated with long-term glucocorticoid use. Arthritis Care Res 55(3):420–426
Da Silva JA, Jacobs JW, Kirwan JR, Boers M, Saag KG, Inês LB, Capell H (2006) Safety of low dose glucocorticoid treatment in rheumatoid arthritis: published evidence and prospective trial data. Ann Rheum Dis 65(3):285–293
El Hachem M, Gesualdo F, Ricci G, Diociaiuti A, Giraldi L, Ametrano O, Neri I (2017) Topical corticosteroid phobia in parents of pediatric patients with atopic dermatitis: a multicentre survey. Ital J Pediatr 43(1):22. https://doi.org/10.1186/s13052-017-0330-7
Heffler E, Madeira LNG, Ferrando M, Puggioni F, Racca F, Malvezzi L, Canonica GW (2018) Inhaled corticosteroids safety and adverse effects in patients with asthma. J Allergy Clin Immunol Pract 6(3):776–781
Hodgens A, Sharman T (2022) Corticosteroids. In: StatPearls. StatPearls Publishing
Liu D, Ahmet A, Ward L, Krishnamoorthy P, Mandelcorn ED, Leigh R et al (2013) A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy Asthma Clin Immunol 9:1–25
Oenning D, de Oliveira BV, Blatt CR (2011) Patient awareness about drugs prescribed after medical appointment and prescription. Ciência Saúde Coletiva 16(7):3277
Saag KG, Koehnke R, Caldwell JR, Brasington R, Burmeister LF, Zimmerman B et al (1994) Low dose long-term corticosteroid therapy in rheumatoid arthritis: an analysis of serious adverse events. Am J Med 96(2):115–123
Saleh S (2022) Total number of healthcare workers in the United Arab Emirates (UAE) from 2013 to 2017. https://www.statista.com/statistics/1120454/uae-number-of-healthcare-workers/#:~:text=In%202017%2C%20the%20total%20number,UAE)%20was%20approximately%20113%20thousand.
Sami SA, Marma KKS, Chakraborty A, Singha T, Rakib A, Uddin MG et al (2021) A comprehensive review on global contributions and recognition of pharmacy professionals amidst COVID-19 pandemic: moving from present to future. Future J Pharm Sci 7(1):119
Saqib A, Atif M, Ikram R, Riaz F, Abubakar M, Scahill S (2018) Factors affecting patients’ knowledge about dispensed medicines: a qualitative study of healthcare professionals and patients in Pakistan. PLoS ONE 13(6):e0197482
Schäcke H, Döcke W-D, Asadullah KJP (2002) Mechanisms involved in the side effects of glucocorticoids. Pharm Therapeutics 96(1):23–43
Shetty YC, Vinchurkar P, More S, Siddiqui A, Tilak S, Ginodia S et al (2022) Knowledge and awareness regarding corticosteroids and effectiveness of a novel steroid educational module among people visiting general OPD of a tertiary care hospital. Indian J Pharm Pract 15(1):10
Singh J, Singh N, Kumar R, Bhandari V, Kaur N, Dureja S (2013) Awareness about prescribed drugs among patients attending Out-patient departments. Int J Appl Basic Med Res 3(1):48
Smith SD, Harris V, Lee A, Blaszczynski A, Fischer G (2017) General practitioners’ knowledge about use of topical corticosteroids in paediatric atopic dermatitis in Australia. Aust Fam Phys 46(5):335–340
Smolen JS, Landewé RB, Bergstra SA, Kerschbaumer A, Sepriano A, Aletaha D et al (2023) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2022 update. Ann Rheumatic Dis 82(1):3–18
Song SY, Jung S-Y, Kim EJJ (2019) Steroid phobia among general users of topical steroids: a cross-sectional nationwide survey. J Dermatol Treat 30(3):245–250
Struja T, Nitritz N, Alexander I, Kupferschmid K, Hafner JF, Spagnuolo CC et al (2024) Treatment of glucocorticoid-induced hyperglycemia in hospitalized patients-a systematic review and meta-analysis. Clin Diabetes Endocrinol 10(1):1–14
Van Grunsven PJJ (2001) The magnitude of fear of adverse effects as a reason for nonparticipation in drug treatment: a short review. J Asthma 38(2):113–119
Vegiopoulos A, Herzig SJM (2007) Glucocorticoids, metabolism and metabolic diseases. Mol Cell Endocrinol 275(1–2):43–61
Verma S (2014) Sales, status, prescriptions and regulatory problems with topical steroids in India. Indian J Dermatol Venereol Leprol 80:201
Waljee AK, Rogers MA, Lin P, Singal AG, Stein JD, Marks RM et al (2017) Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. Br Med J. https://doi.org/10.1136/bmj.j1415
Wei L, MacDonald TM, Walker BR (2004) Taking glucocorticoids by prescription is associated with subsequent cardiovascular disease. Ann Intern Med 141(10):764–770
Weinstein RSJE (2012) Glucocorticoid-induced osteonecrosis. Endocrine 41:183–190
Yasir M, Goyal A, Bansal P, Sonthalia S (2021) Corticosteroid adverse effects. StatPearls Publishing, Florida
Acknowledgements
We are grateful for Mr. Mohammad Nakhal who helped with data collection.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MB was contributed conceptualization and tool development. DM and MO were involved in data collection and entry and manuscript writing. SA was performed project supervision, tool development, and ethical approval. OK and SZ were attributed data curation and manuscript writing. BS and RN were done statistical analysis and proofreading. AA was responsible for project supervision, tool development, data collection, and analysis. All authors had proof-read the manuscript and agreed on its contents.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was granted by the Research Ethics Committee of the United Arab Emirates University (Approval Number: ERSC_2022_1886).
Competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barakat, M., Malaeb, D., El Ouweini, A. et al. Healthcare providers' perspectives on corticosteroid-containing drugs: a cross-sectional study in the United Arab Emirates. Futur J Pharm Sci 10, 114 (2024). https://doi.org/10.1186/s43094-024-00690-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43094-024-00690-6