Abstract
Patients with malignant central airway obstruction often present with dyspnea and sometimes with frank respiratory failure. Airway stenting has become a routine modality in the management of these patients. A correctly placed airway stent will give good relief in dyspnea and respiratory failure and will even improve the patient's ECOG (Eastern Cooperative Oncology Group) performance score. The common complications associated with stents are migration, fracture, infection, and obstruction by tumors, granulation tissue, and secretions. These complications are more pronounced with metallic stents. Surveillance bronchoscopy should ideally be done in these patients at least 4–6 weeks post-stent insertion. Removal of granulation tissue has been attempted with modalities like lasers, Argon plasma coagulation, cryotherapy, and snare electrocautery. Here, we present a novel case of post-stent granulation tissue, which was removed and debulked with the help of electrocoagulation bronchoscopy biopsy forceps (hot biopsy forceps).
Conclusion Hot biopsy forceps can be safely and easily used for the removal of granulation tissue in patients post-tracheobronchial stent insertion.
Similar content being viewed by others
Background
Patients with malignant central airway obstruction often present with dyspnea and sometimes with frank respiratory failure. Airway stenting has become a routine modality in the management of these patients [1]. A correctly placed airway stent will give good relief in dyspnea and respiratory failure and will even improve the patient's ECOG (Eastern Cooperative Oncology Group) performance score [2].
Airway stents, whether metallic or silicon are not devoid of complications. The common complications associated with stents are migration, fracture, infection, obstruction by tumors, granulation tissue, and secretions. These complications are more pronounced with metallic stents. Granulation tissue formation inside the lumen of the stent is a serious complication and it often requires frequent bronchoscopic interventions for the same. Surveillance bronchoscopy should ideally be done in these patients at least 4–6 weeks post-stent insertion [1].
Removal of granulation tissue has been attempted with modalities like lasers, Argon plasma coagulation, cryotherapy, and snare electrocautery. Here, we present a novel case of post-stent granulation tissue, which was removed and debulked with the help of electrocoagulation bronchoscopy biopsy forceps (hot biopsy forceps).
Case
A 48-year-old male, known case of locally advanced carcinoma esophagus was referred in view of breathing difficulty and cough while eating, on evaluation was found to have a large tracheoesophageal fistula. There was no history of any known comorbidities. For the treatment of carcinoma esophagus patient underwent chemotherapy (6 cycles) and radiotherapy (28 fractions, 50.4 grey) with a substantial response to treatment. For the tracheoesophageal fistula patient underwent Ryle’s tube insertion and was managed conservatively.
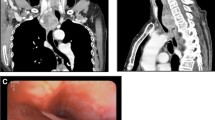
Despite optimal chemoradiation therapy, tracheoesophageal fistula remained patent and was managed with the help of an esophageal stent to seal the large fistula. Post-stent placement patient developed breathing difficulty and airway assessment revealed significant extrinsic compression on the posterior wall of the trachea (Fig. 1). In view of significant luminal narrowing and respiratory distress patient underwent tracheobronchial Y-SEMS (Self-expanding metallic stent) placement and had significant response with almost complete resolution of symptoms. Surveillance bronchoscopy done after 2 weeks, showed both the lumen of the stent being patent with pooling of secretions which were suctioned out.
One month after stent placement, the patient presented with worsening breathlessness and noisy breathing in emergency. On presentation, the patient had respiratory distress with stridor during normal breathing with room air oxygen saturation of 87%. Emergency radiology was done which showed tracheal stent in situ and other relevant causes of respiratory failure were ruled out. An emergency flexible bronchoscopy was performed, which showed both distal limbs of the tracheobronchial stent were covered with granulation tissue leading to significant airway narrowing. Figure 2 shows the presence of granulation tissue causing airway narrowing of the right limb of the stent giving the unique appearance of a pseudo-vocal cord. To achieve patency of the airway, patient was shifted to the bronchoscopy room. With the help of a flexible bronchoscope, airway patency was achieved after carefully removing the granulation tissue using hot biopsy forceps (Fig. 3) followed by dilatation with a CRE (controlled radial expansion) balloon. Post-procedure assessment revealed an open airway, as shown in Fig. 4. The patient’s symptoms of breathlessness and noisy breathing improved significantly following the intervention. The patient could be discharged the very next day. The patient is under follow-up and routine surveillance bronchoscopies are being done.
Discussion
Malignant airway compression is seen in up to 30% of patients with bronchogenic carcinoma. Whether the cause of airway compression is benign or malignant, an airway stent has a potential role in both and gives immediate relief of symptoms, improves quality of life, and helps in recovering from respiratory failure [3, 4]. Stent being a foreign body, will have its own set of associated complications, The most common complications are migration of the stent, granulation tissue formation around the stent, problems with mucociliary clearance, poor patient tolerance, hemoptysis, tumor overgrowth, stent fracture, mucus plugging, problems with placement and removal and long term complication like infection. Of these complications, granulation tissue formation is one of the serious complications as it requires immediate intervention for management [5, 6]. In our case, the stent led to significant granulation tissue formation and subsequent narrowing of the airway lumen, which led to the patient developing stridor and subsequently respiratory failure.
Overall 40–60% of patients will develop some form of stent-related complication and the majority in the first 2–3 months [7, 8]. Avoidance of stent placement is the best management strategy. In cases where stent placement cannot be avoided then active surveillance bronchoscopy should be offered to all of these patients especially during the first 2–3 months in detecting these complications [9]. If a complication arises then management should be tailored accordingly. Patients may require bronchoscopy in managing these complications including rigid bronchoscopes also, especially when dealing with migration of stent and in case of planned removal and reinsertion.
Removal of airway granulation tissue has been performed with instruments such as cryotherapy, lasers, argon plasma coagulation(APC), and flexible forceps [10, 11]. Each modality has its own advantages and disadvantages. Lasers, both Nd:YAG (neodymium-doped yttrium aluminum garnet) and Carbon dioxide lasers have been used in the past for the management of granulation tissue post-stenting [12]. Advantage of this modality is its precision and can penetrate to greater depths. But the important drawback is that it can cause wall perforation, and stent damage, needs a lot of expertise and cost is an issue, especially in developing countries. APC on the other hand being a non-contact modality, requires argon gas as conductive media. The advantage of APC is its suitability for treating bronchial segments which take off at an acute angle from the major airways, such as apical and posterior segments of the upper lobes or the apical lower lobe segments where as In case of Laser, bundles leaves probe in a straightforward way. The disadvantage of APC is superficial coagulation with this modality. The problem with both APC and lasers is that they cannot be used in a high oxygen environment and for removal of tissue separate biopsy forceps is required.
Cryotherapy is also a promising modality for the management of central airway obstruction and for the management of stent-related granulation tissue. Advantage of using this technique is relatively lower cost as compared to lasers, easy learning curve, safe handling for the operator, and most importantly no need for reduction of Fraction of Inspired Oxygen (FiO2). On the other hand, cryotherapy has the disadvantage that it takes a longer time to act, requires a rigid bronchoscope and every time to remove tissue flexible bronchoscope along with cryoprobe needs to be pulled out [13].
To the best of our knowledge hot biopsy, forceps have not been reported to remove granulation tissue, in the available literature. Previous use of this modality has been for biopsy of endobronchial lesions and management of carcinomatous central airway obstruction [14]. In our case use of hot biopsy forceps gave us the advantage of shorter procedure time, ease of use, no significant bleeding reduced overall cost of the procedure, and no adjacent tissue injury. Even the whole procedure could be completed on 40% FiO2 with the help of flexible bronchoscopy alone under deep sedation and the patient could go home the very same day.
Conclusion
Patients with central airway obstruction undergoing stent insertion should be offered regular surveillance bronchoscopies irrespective of symptoms. In the case of granulation tissue formation, hot biopsy forceps is a promising tool for its removal, especially in resource-limited settings, and where lasers are unavailable.
Availability of data and materials
Not applicable.
Abbreviations
- ECOG:
-
Eastern Cooperative Oncology Group
- SEMS:
-
Self-expanding metallic stent
- APC:
-
Argon plasma coagulation
- FiO2:
-
Fraction of Inspired Oxygen
- CRE:
-
Controlled radial expansion
- Nd:YAG:
-
Neodymium-doped yttrium aluminium garnet
References
Inchingolo R, Sabharwal T, Spiliopoulos S, Krokidis M, Dourado R, Ahmed I et al (2013) Tracheobronchial stenting for malignant airway disease: long-term outcomes from a single-center study. Am J Hosp Palliat Care 30(7):683–689
Razi SS, Lebovics RS, Schwartz G, Sancheti M, Belsley S, Connery CP et al (2010) Timely airway stenting improves survival in patients with malignant central airway obstruction. Ann Thorac Surg 90(4):1088–1093
Dutau H, Toutblanc B, Lamb C, Seijo L (2004) Use of the Dumon Y-stent in the management of malignant disease involving the carina. Chest 126(3):951–958
Furukawa K, Ishida J, Yamaguchi G, Usuda J, Tsutsui H, Saito M et al (2010) The role of airway stent placement in the management of tracheobronchial stenosis caused by inoperable advanced lung cancer. Surg Today 40(4):315–320
Lee HJ, Labaki W, Yu DH, Salwen B, Gilbert C, Schneider ALC et al (2017) Airway stent complications: the role of follow-up bronchoscopy as a surveillance method. J Thorac Dis 9(11):4651–4659
Ost DE, Shah AM, Lei X, Godoy MCB, Jimenez CA, Eapen GA et al (2012) Respiratory infections increase the risk of granulation tissue formation following airway stenting in patients with malignant airway obstruction. Chest 141(6):1473–1481
Zakaluzny SA, Lane JD, Mair EA (2003) Complications of tracheobronchial airway stents. Head Neck Surg 128(4):478
Wu C, Liu Y, Hsieh M, Wu Y, Lu M, Ko P et al (2007) Airway stents in management of tracheal stenosis: have we improved? ANZ J Surg 77(1–2):27–32
Hoag JB (2010) Practice patterns for maintaining airway stents deployed for malignant central airway obstruction. J Bronchol Interv Pulmonol 17(2):131
Li S, Wu L, Zhou J, Wang Y, Jin F, Chen X et al (2021) Interventional therapy via flexible bronchoscopy in the management of foreign body-related occlusive endobronchial granulation tissue formation in children. Pediatr Pulmonol 56(1):282–290
Madden B (1997) Successful resection of obstructing airway granulation tissue following lung transplantation using endobronchial laser (Nd:YAG) therapy. Eur J Cardiothorac Surg 12(3):480–485
Sjogren PP, Sidman JD (2013) Use of the carbon dioxide laser for tracheobronchial lesions in children. JAMA Otolaryngol Head Neck Surg 139(3):231
Hetzel J, Kumpf M, Hetzel M, Hofbeck M, Baden W (2011) Cryorecanalization of an obstructed bronchial stent in a 12-year-old boy. Respiration 82(3):290–293
Ugajin M, Kani H (2017) Successful treatment of carcinomatous central airway obstruction with bronchoscopic electrocautery using hot biopsy forceps during mechanical ventilation. Case Rep Oncol Med 2017:1–4
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors SP/PB/AK/SA contributed equally to data collection, drafting, and uploading of the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Given by all authors.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pahuja, S., Bajad, P., Khanna, A. et al. Novel use of hot biopsy forceps for removal of tracheobronchial stent-related granulation tissue. Egypt J Bronchol 18, 56 (2024). https://doi.org/10.1186/s43168-024-00305-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-024-00305-x