Abstract
Background
Pleural effusion is the most prevalent pleural disorder. One third of pleural effusions are caused by lung cancer. Thoracoscopy is regarded as the most reliable diagnostic method for the evaluation of suspected pleural malignancy.
Aim and objectives
To assess visible pleural characteristics of abnormalities and their locations for malignant and benign pathologies as well as to determine the incidence of malignancy in the apparent normal pleura.
Patients and methods
This was a descriptive, observational, and cross-sectional research that was performed on 36 cases with undiagnosed exudative pleural effusions prepared for medical thoracoscopy and on whom the cytological analysis was inconclusive, at the thoracoscopic Unit Department of Chest Diseases, Faculty of Medicine Zagazig University, from December 2023 to May 2024.
Results
The apparent normal pleura and adhesions were significantly greater in benign effusions than in malignant effusions (p = 0.019 and p = 0.04, respectively), while nodular effusion was significantly greater in malignant effusions than in benign effusions (p = 0.003). Bleeding was significantly greater in malignant effusions than in benign effusions (p = 0.019). As regards the thoracoscopic findings, 24 (66.7%) patients showed nodular patterns, 14 (38.9%) patients showed adhesions, and two (5.6%) patients had pus, while six (16.7%) patients had apparent normal pleura. The costal pleura was the most frequently affected site (88.9%) followed by the visceral pleura (55.6%) then the diaphragmatic pleura (38.9%).
Conclusion
Medical thoracoscopy (MT), a minimally invasive and a generally safe treatment, enables the interventional pulmonologist to access the pleural cavity directly and obtain pleural samples under direct view helping in predicting the pathology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Pleural effusions are frequently caused by malignant inclusion of the pleura, which is a prevalent medical disorder [1]. Pleural deposits might be caused by almost all tumors, which interrupt the physiological turnover of pleural fluid and spread cancer cells. Pleural effusions are primarily caused by lung cancer, which accounts for one third of the cases [2]. It is important to quickly diagnose a malignant pleural effusion (MPE) in order to adequately stage the patient as well as start appropriate therapy, despite the underlying neoplasm, as it is indicative of progressive illness and a poor prognosis.
A clinical assessment, complementary imaging studies, and minimally invasive techniques are necessary for determining the reason for an undiagnosed pleural effusion. The 1ry pleural fluid sample undergoes cytological assessment, which has a mean sensitivity of 62% for malignancy. The diagnostic result is increased to approximately 72% by the collection of a second specimen (total range 49–91%) [3].
The underlying reason for the effusion is determined by image-guided pleural biopsy or thoracoscopy if pleural fluid cytology is unable to establish an accurate diagnosis and malignant illness is suspected, as stated by international guidelines, because of its variable sensitivity [3, 4].
Thoracoscopy is regarded as the most reliable diagnostic method for the evaluation of suspected pleural malignancy [5].
The macroscopic findings of thoracoscopy demonstrate characteristics which are thought to be indicative of malignancy involving hard pale pachypleuritis nodules and large localized mass as well as lymphangitis on either the visceral and/or parietal surfaces [6]. Thoracoscopy might aid in the identification of a reason for benign effusion by enabling the direct observation of features like several micronodules in rheumatoid effusion [7].
Patients and methods
This was a descriptive, observational, and cross-sectional research that was performed on 36 cases with undiagnosed exudative pleural effusions prepared for medical thoracoscopy and on whom the cytological analysis was inconclusive, at the thoracoscopic Unit Department of Chest Diseases, Faculty of Medicine Zagazig University, from December 2023 to May 2024.
The inclusion criteria are as follows: undiagnosed exudative pleural effusions patients and patients above 18 years.
The exclusion criteria are as follows: the following patients listed were not involved in the research:
cases who were not healthy enough to have a thoracoscopy, such as in the following situations: patients who continued to have uncured severe hypoxemia, patients who were unable to maintain lateral decubitus for long enough for the thoracoscopy to be performed, patients whose hemodynamic or cardiovascular condition is unstable, and people who suffered from coagulation defects. The platelet count should be larger than 60,000/mm3, and the prothrombin level must be at least higher than 60%.
Absolute contraindications are the following situations: cases in whom the pleural space was determined to be difficult to access; cases in whom the pleural space was completely destroyed by fibrous tissue, otherwise cases in whom multiloculated effusions were detected; cases with extremely thickened pleura, as shown through CT scan, as this prevented the underlying lung from expanding fully after the surgery; and patients with highly vascularized pulmonary lesions, pulmonary arteriovenous aneurysms, probable hydatid cysts, and honeycomb lung.
Medical thoracoscopy surgery
Prior to thoracoscopy, blood pressure has been assessed, and coagulation function tests, viral markers, blood routine tests, blood ion tests, and oxygen saturation as well as electrocardiogram have been carried out. An ultrasound examination has been conducted the day prior to the medical thoracoscopy.
The cases were positioned in a supine position with the impacted side directed upward. The entry point is located at the level of the 5th–6th intercostal gap in the mid-axillary line or the posterior axillary line. The parietal pleura was anesthetized with local penetration of 0.2% lidocaine in 5–10 mL before a 1–2-cm surgical incision has been performed.
The thoracic cavity and subcutaneous tissue have been abruptly split apart. The core is extracted after a trocar cannula has been introduced into the pleural cavity. A flexible electronic thoracoscope then was inserted. Multiple biopsies were carried out if pleural nodules were discovered. Biopsy samples were sent for pathological analysis, and before the wound was stitched up, a drainage tube was placed in the pleural cavity.
Statistical analysis
IBM SPSS software package version 25.0 (IBM Corp. Released 2017) was utilized to analyze the data that was inputted into the computer (Version 25.0 of IBM SPSS Statistics for Windows; Armonk, NY: IBM Corp.). Numbers and percentages have been utilized for presenting qualitative data. The normality of the distribution has been confirmed utilizing the Shapiro–Wilk test. Range (min and max), mean, standard deviation, median, and interquartile range (IQR) have been utilized for presenting quantitative data. The outcomes were assessed at the 5% level of significance. The utilized tests were as follows: chi-square test for categorical variables, to show association among 2 or more categorical (nominal) variables; Monte Carlo correction for chi-square when up to 20% of the cells have predicted count below 5.
Results
The age of the examined cases varied among 35 years and 80 years, with a mean age of 54.72 ± 12.25 years, with most cases (72.2%) having age less than 60 years. There were twenty-five (69.4%) males and eleven (30.6%) females, with the male-to-female ratio being 2.27:1. Twenty (55.6%) patients were smokers (Table 1).
As regards the thoracoscopic findings, 24 (66.7%) patients showed nodular patterns, 14 (38.9%) patients showed adhesions, and two (5.6%) patients had pus, while six (16.7%) patients had apparent normal pleura. The costal pleura was the most frequently affected site (88.9%) followed by the visceral pleura (55.6%) then the diaphragmatic pleura (38.9%) (Table 2).
The cause of pleural effusions is within the studied cases. The diagnostic result of medical thoracoscopy for undiagnosed pleural effusion was 100%. Diagnosis was malignant pleural effusion in 18 (50%) cases, and 18 (50%) patients had benign pleural effusion. Considerably, metastatic adenocarcinoma was the most frequent cause of exudative pleural effusions throughout the research duration responsible for 33.3% of every reason followed by chronic non-specific inflammation (27.8%) then mesothelioma (16.7%). Complications from the procedure was reported in 16 (44.4%) cases. Pain was reported in 14 (38.9%) cases, surgical emphysema in six (16.7%) cases, and bleeding in six (16.7%) cases. Most studied cases (83.3%) had a length of hospitalization of more than 5 days (Table 3).
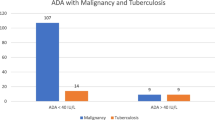
The apparent normal pleura and adhesions were significantly greater in benign effusions than in malignant effusions (p = 0.019 and p = 0.04 respectively), while nodular effusion was significantly greater in malignant effusions than in benign effusions (p = 0.003). Bleeding was significantly greater in malignant effusions than in benign effusions (p = 0.019) (Figs. 1, 2, and 3) (Table 4).
Discussion
Pleural effusion is a frequently encountered entity in pulmonary practice and may be due to varying diseases with different pathogenic mechanisms. Pleural effusion is primarily caused by high pulmonary capillary pressure, raised permeability, lymphatic blockage, decreased negative intrapleural pressure, and reduced oncotic pressure (e.g., in hypoalbuminemia) [8].
The two most prevalent reasons for undiagnosed exudative pleural effusion are pleural malignancy (either primary or metastatic) and pleural tuberculosis (TB) [9, 10].
The current study showed that a total number of 36 cases with undiagnosed exudative pleural effusions prepared for medical thoracoscopy have been included. The age of examined cases varied among 35 years and 80 years, with an average age was 54.72 ± 12.25 years, with most cases (72.2%) having age less than 60 years. There were twenty-five (69.4%) males and eleven (30.6%) females, with the male-to-female ratio being 2.27:1. Twenty (55.6%) patients were smokers.
These age groups’ results matched with the results reported by Sharath et al. [11] who analyzed the value of medical thoracoscopy within cases with exudative pleural effusion of unidentified cause. The average age of the cases was 52.9 years (standard deviation ± 13.5), with seventeen (60.7%) being male and eleven (39.3) being female. The patient’s age varied among 25 and 75 years. More cases were in the 40–60 age group.
For the current study, as regards the thoracoscopic findings, 24 (66.7%) patients showed nodular patterns, 14 (38.9%) patients showed adhesions, and two (5.6%) patients had pus, while six (16.7%) patients had apparent normal pleura. The costal pleura was the most frequently affected site (88.9%) followed by the visceral pleura (55.6%) then the diaphragmatic pleura (38.9%).
Our results supported the results reported by Sharath et al. [11] who found that only one case had bilateral effusion, while 96.4% of cases (27/28) had unilateral pleural effusion, 60.7% had right-sided effusion, and 35.7% had left-sided effusion. Pleural thickening was observed in 10.7% (3/28) of cases, adhesions in 21.4% (6/28) of cases, and nodules in 67.9% (19/28) of cases on thoracoscopy. In nineteen cases, nodules were the most common result in the gross thoracoscopic investigation. In a total of 19 cases with nodules, 84.21% (16/19) had been diagnosed as malignant, while 15.79% (3/19) were classified as nonmalignant. The 2nd prevalent discovery in the gross thoracoscopic investigation was the presence of adhesions in 6 cases, all of whom were nonmalignant.
In addition, Wang et al. [12], who studied 833 patients of undiagnosed pleural effusion, reported that 342 cases (41.1%) had malignant pleural effusion, 429 cases (51.5%) had benign pleural effusion, and 62 cases (7.4%) were unable to obtain definitive diagnoses. In total, the diagnostic effectiveness of MT was 92.6% (771/833).
According to Singh et al. [13], thoracoscopy is a technique that is well-tolerated and safe, with minimal risk, enabling the precise diagnosis of undiagnosed pleural effusion.
In addition, Singh et al. [13] demonstrated that 63.07% of cases had multiple variable-sized nodules, primarily in patients of adenocarcinoma. Pleural adhesions were present in 29.74% of cases, while pleural plaques were present in 16.41% of cases (primarily parapneumonic effusions). Hyperemic pleura was present in 55.89% of cases (primarily mesothelioma subsequent to chronic nonspecific pleuritis), sago grain nodules were present in 25.12% of cases (tubercular pleuritis), and smooth, almost healthy pleura was present in 4.6% of cases.
Also, Gong et al. [14] who studied 82 patients by medical thoracoscopy demonstrated that pleural adhesions were absent in 66.7% of acute and chronic inflammation (ACI) cases, moderate in 34.4% of TB cases, and severe in 34.4% of TB cases. Pleural surface nodules were present in 100% of M and TB cases, and pleural surface nodules were present in 77.8% of ACI cases. Encapsulated pleural effusion was observed in 49.2% of TB cases and 33.3% of M cases.
The current study demonstrated the etiology of undiagnosed pleural effusions with 50% diagnosed as a malignant (18 case). Diagnosis was malignant pleural effusion in 18 (50%) cases, and 18 (50%) patients had benign pleural effusion. Considerably, metastatic adenocarcinoma was the most prevalent reason for exudative pleural effusions throughout the research duration, responsible for 33.3% of every reason followed by chronic non-specific inflammation (27.8%) then mesothelioma (16.7%). Complications from the procedure were reported in 16 (44.4%) cases.
Pain was reported in 14 (38.9%) cases, surgical emphysema in six (16.7%) cases, and bleeding in six (16.7%) cases. Most studied cases (83.3%) had a length of hospital stay of more than 5 days.
Our results matched with the results reported by Augustine et al. [15], who demonstrated that regarding the etiology of pleural effusions, a final diagnosis was obtained in all the patients who underwent MT, thus providing a diagnostic yield of 100%. Pleural tuberculosis contributed to 60% (15 out of 25) of undiagnosed exudative effusions. The rest (40%) of the effusions (10 out of 25) were due to malignant disease involving the pleura. The average length of hospitalization was 8.53 (SD 3.662) and 9.60 (SD 2.86) days in the granuloma group and malignancy groups, respectively. A mean difference of 1.067 days was noted between these groups, but it was not statistically significant.
Also, our results supported the results reported by Sharath et al. [11], who observed that the diagnosis of malignancy has been determined in seventeen cases (60.7%), tuberculosis in eight cases (28.6%), and nonspecific pleuritis/fibrosis in three cases (10.7%). Metastatic adenocarcinoma was the most prevalent type of malignancy, detected in 70.58% (12/17) of cases. Malignant mesothelioma has been identified in 17.64% (3/17) of cases, and undifferentiated carcinoma had been identified in 11.76% (2/17) of cases. The procedure did not result in any significant complications or mortality. Three patients had a few minor complications, like a mild fever in 1 case (3.57%) and minor bleeding in 2 cases (7.14%).
Furthermore, Prasanth et al. [16] demonstrated that malignancy was the cause of 56.6% of their cases.
Also, Wang et al. [12] demonstrated that following medical thoracoscopy, 342 (41.1%) cases had been determined to have malignant pleural effusion, 429 (51.5%) cases had benign pleural effusions, and 62 (7.4%) cases were unable to obtain a definitive diagnosis. He observed that lung cancer was the most common cause of malignant pleural effusion (67.8%), subsequent to mesothelioma (10.2%), lymphoma (2.9%), and so forth. In twenty-five cases (7.3%) with malignant pleural effusion, the original malignancies were not identifiable. Empyema was the only severe complication, affecting three cases (0.4%). Transient chest pain (44.1%) from the indwelling chest tube was the most prevalent mild complication.
In addition, Singh et al. [13] demonstrated that the etiological diagnosis in 99 cases (50.76%) was malignant pleural effusion. Of the 99 malignant effusions, metastatic adenocarcinoma was the most prevalent cause in 45.45% of the cases (45 patients). Malignant mesothelioma was present in approximately 36.36% of the patients (36 patients). Metastatic squamous cell carcinoma was the cause of effusion in 11.1% (11 patients), while small cell carcinoma was the cause in 6.06% (6 patients). One patient had effusion as a result of malignant lymphoma, which accounted for 1% of the cases. Granulomatous inflammation caused by tuberculosis was the most prevalent among the non-malignant effusions (31.79%).
Moreover, Nour et al. [17] found that mild complications have been found within ten and 16.5% of cases.
Our findings showed that apparent normal pleura and adhesions were significantly greater in benign effusions than in malignant effusions (p = 0.019 and p = 0.04 respectively), while nodular effusion was significantly greater in malignant effusions than in benign effusions (p = 0.003). Bleeding was significantly greater in malignant effusions than in benign effusion (p = 0.019). Insignificance among the examined groups was observed according to age, sex, smoking, and hospitalization after thoracoscopy.
Our outcomes agreed with Gong et al. [14] who documented insignificance among the examined groups according to age, sex, and smoking. They demonstrated a significance among the examined groups according to nodules.
Conclusion
MT, a minimally invasive and generally safe treatment, enables the interventional pulmonologist to access the pleural cavity directly and obtain pleural samples under direct view helping in predicting the pathology.
Availability of data and materials
No datasets were generated or analyzed during the current study.
References
Jovanovic D (2021) Etiopathogenesis of malignant pleural effusion. AME Med J 25:6
Maloney-Newton S, Hickey M, Brant JM, editors. Mosby’s Oncology Nursing Advisor-E-Book: A Comprehensive Guide to Clinical Practice. Elsevier Health Sciences; 2023. https://karger.com/res/article-abstract/101/1/46/829121/Objective-Thoracoscopic-Criteria-in, https://books.google.com.eg/books?hl=en&lr=lang_en&id=fEXnEAAAQBAJ&oi=fnd&pg=PP1&dq=2.%09Maloney-Newton+S,+Hickey+M,+Msn+MS,+Brant+J+(Eds.)+(2023)+Mosby%27s+Oncology+Nursing+Advisor-E-Book:+A+Comprehensive+Guide+to+Clinical+Practice.+Elsevier+Health+Sciences.&ots=aVNCTJd5qt&sig=1Rs4RCbi_X8hFIs8j8GZ0w1BogI&redir_esc=y#v=onepage&q&f=false.
Rivera MP, Mehta AC, Wahidi MM (2013) Establishing the diagnosis of lung cancer: diagnosis and management of lung cancer: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 143(5):e142S – e165
Mohamed EE, Talaat IM, Abd Alla AE, ElAbd AM (2013) Diagnosis of exudative pleural effusion using ultrasound guided versus medical thoracoscopic pleural biopsy. Egypt J Chest Dis Tuberc 62(4):607–615
Shaikh F, Lentz RJ, Feller-Kopman D, Maldonado F (2020) Medical thoracoscopy in the diagnosis of pleural disease: a guide for the clinician. Expert Rev Respir Med 14(10):987–1000
Ellayeh M, Bedawi E, Banka R, Sundaralingam A, George V, Kanellakis N et al (2022) Objective thoracoscopic criteria in differentiation between benign and malignant pleural effusions. Respiration 101(1):46–56
Ferreiro L, Toubes ME, San José ME, Suárez-Antelo J, Golpe A, Valdés L (2020) Advances in pleural effusion diagnostics. Expert Rev Respir Med 14(1):51–66
Jany B, Welte T (2019) Pleural effusion in adults—etiology, diagnosis, and treatment. Dtsch Arztebl Int 116(21):377
Mootha VK, Agarwal R, Singh N, Aggarwal AN, Gupta D, Jindal SK (2011) Medical thoracoscopy for undiagnosed pleural effusions: experience from a tertiary care hospital in north India. Indian J Chest Dis Allied Sci 53(1):21
Haridas N, Suraj KP, Rajagopal TP, James PT, Chetambath R (2014) Medical thoracoscopy vs closed pleural biopsy in pleural effusions: a randomized controlled study. J Clin Diagn Res: JCDR 8(5):MC01
Sharath Chandra KS, Thimmaiah CM, Hosmane GB (2023) The outcome of medical thoracoscopy in patients with unexplained exudative pleural effusion. Indian J Respir Care 12(2):110
Wang XJ, Yang Y, Wang Z, Xu LL, Wu YB, Zhang J et al (2015) Efficacy and safety of diagnostic thoracoscopy in undiagnosed pleural effusions. Respiration 90(3):251–255
Singh R, Shah NN, Dar KA, Farooq SS, Dar MY (2022) Medical thoracoscopy: diagnostic role in the management of undiagnosed pleural effusions and its complications. Indian J Chest Dis Allied Sci 64:258–262
Gong L, Huang G, Huang Y, Liu D, Tang X (2020D) Medical thoracoscopy for the management of exudative pleural effusion: a retrospective study. Risk Manag Healthc Policy 4:2845–2855
Augustine J, Vijay A, Ramachandran D, Cleetus M, Nirmal AS, John S et al (2021) Improving the yield of diagnostic medical thoracoscopy for undiagnosed exudative pleural effusions using a rigid diagnostic algorithm. Int J Mycobacteriol 10(4):405–410
Prasanth G, Anbumaran PM, Swetha S, Krishnarajasekhar OR, Gangadharan V (2023) Medical thoracoscopy–diagnostics of pleural effusion with indefinite etiology. Biomedicine 43(01):507–513
Nour Moursi Ahmed S, Saka H, Mohammadien HA, Alkady O, Oki M, Tanikawa Y et al (2016) Safety and complications of medical thoracoscopy. Adv Med 2016(1):3794791
Acknowledgements
Thanks To my professors for their kind support.
Author information
Authors and Affiliations
Contributions
M.E and H.S shared in the writing, editing, data collection, and statistical analysis of the research in almost the same way. M.E and H.S were responsible for the results of the study, while M.E was responsible for reviewing the end result collection. D.A was the supervisor and revised all our steps and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elfeqy, M.E.A.H., Hamed, H.S. & Ibrahim, D.A. Correlation between thoracoscopic presentations and pathological patterns in undiagnosed pleural effusion. Egypt J Bronchol 18, 72 (2024). https://doi.org/10.1186/s43168-024-00324-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-024-00324-8