Abstract
Background
Cardiac symptoms are a characteristic feature of chronic obstructive pulmonary disease (COPD), a disorder with lately achieved recognition as a systemic illness according to established standards. The research’s objective was aimed at investigating the transthoracic echocardiography role in assessing right ventricular (RV) dysfunction among individuals diagnosed with COPD, as well as to examine the potential correlation between blood pro B-type natriuretic peptide (BNP) concentrations + and this diagnostic procedure.
Methods
Arterial blood gasses, spirometry, echocardiography, and serum pro BNP were done for 80 COPD patients and 20 healthy smokers, and some echocardiographic parameters were correlated with degree of airflow limitation.
Results
77.5% of COPD cases exhibited pulmonary hypertension (PHTN), and on classifying our COPD patients, it was found that 65% of patients in group II had PHTN and 90% of patients in group III had PHTN. Systolic pulmonary artery pressure (SPAP), mean pulmonary arterial pressure (MPAP), right ventricular mid diameter (RVMD), right ventricular basal diameter (RVBD), right ventricular longitudinal diameter (RVLD), right ventricular outflow tract (RVOT) above pulmonary and aortic valve, and tricuspid annular plane systolic excursion (TAPSE) along with RVEF exhibited a significant variance among all groups. A negative correlation was observed among forced expiratory volume (FEV) 1% and (RVMD as well as RVBD) and between Pro BNP and (TAPSE and RVEF).
Conclusions
PHTN was found in 77.5% of COPD patients and is negatively correlated with FEV1%. Serum pro BNP level exhibits a negative correlation with FEV1% in stable COPD patients.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) represents a prevalent, avoidable, and controllable disorder, characterized by enduring respiratory symptoms along with limited airflow. The persistent restriction of airflow is attributed to a combination of conditions affecting the small airways, including obstructive bronchiolitis and parenchymal damage, sometimes known as emphysema [1]. COPD exhibits various systemic manifestations, with cardiac manifestations being the prevailing extrapulmonary features observed in individuals with COPD. COPD impacts the blood vessels within the lungs, inducing pulmonary hypertension (PHTN), cor-pulmonale, and dysfunction of right ventricle [2].
The PHTN along with aberrant right ventricular (RV) activity among COPD cases, regardless of its severity, are linked to greater hospitalization rates in addition to a worse prognosis [3].
PHTN remains linked to an average pulmonary arterial pressure (PAPm) rise, reaching at least 25 mmHg at rest, which was determined by right heart catheterization (RHC) [4].
As addressed by multiple studies, estimations of PAP obtained by echocardiography correspond closely with those obtained from cardiac catheterization [5].
Echocardiography represents a non-invasive method, employed for evaluating the heart’s condition, including several aspects such as ventricular RV function, RV filling pressure, tricuspid regurgitation, and LV function. Brain natriuretic peptides (NT-pro B-type natriuretic peptide (BNP) or BNP) have shown significant promise as blood biomarkers for assessing the risk of individuals with PHTN [6]. NT-pro BNP as well as BNP are formed from the precursor hormone pro-BNP, synthesized inside ventricular myocytes and then released in response to myocardial strain. The substance levels increase during acute COPD exacerbations then return to their original levels following successful treatment [7].
The research employing medications approved for PAH among PHTN cases linked to COPD or emphysema have addressed contradictory findings. Their limitations involved modest sample size, short periods, and inadequate PHTN hemodynamic characterization [8]. Within an RCT lasting for 16 weeks, which involved 28 participants developing COPD along with severe PHTN confirmed by RHC, sildenafil therapy exhibited significant enhancements as regards PVR as well as quality of life [9]. Registry data addressed that approximately 30% of cases developing COPD along with severe PHTN, predominantly managed with PDE5is, showed an improvement as regards WHO-FC, 6MWD, and PVR vs. baseline, while those with a treatment response showed an improvement as regards transplant-free survival [10].
Simvastatin was ineffective in exacerbation prevention among COPD cases who did not have any metabolic or cardiovascular indications requiring statin therapy [11]. A correlation between statin and outcome improvements (involving exacerbations as well as mortalities reduction) has been documented within observational studies, including COPD cases who received them for cardiovascular or metabolic indications [12].
This work was aimed at assessing the transthoracic echocardiography accuracy in evaluating pulmonary artery pressure as well as RV characteristics among cases developing varying degrees of COPD and examining its correlation with the blood biomarker pro-BNP.
Patients and methods.
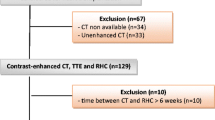
This research was conducted on a group of 80 male patients, all of whom were over the age of 18 and were diagnosed with COPD in accordance with the guidelines outlined in GOLD 2021. Additionally, a control group of 20 healthy people was included in the study. The research was conducted between November 2022 and November 2023, after the authorization of the Ethical Committee of Tanta University Hospitals in Tanta, Egypt (Approval code: 35666/8/22). The patients provided informed written consent.
The exclusion criteria were people who had an acute exacerbation of COPD during the month before the research, individuals with chronic lung disease (CLD) unrelated to COPD, individuals with chronic cardiovascular illness, and patients with a limited echocardiographic window, along with cases unable to do spirometry.
Participants underwent a categorization into three distinct groups: group I (n = 20) constituted the control group, group II (n = 40) represented the mild/moderate COPD group, and group III (n = 40) represented the severe COPD group.
According to GOLD and severity of airflow obstruction in COPD (based on post -bronchodilator FEV1) [13] (Fig. 1)
History taking, clinical examination (general and local cardiac examination was done for all participants, involving vital signs (heart rate, blood pressure, respiratory rate as well as temperature)), head and neck examination, upper and lower limb examination, abdominal examination, and local examination. Symptoms were assessed by mMRC and COPD assessment test (CAT); spirometry, laboratory, and radiographic investigations were conducted on all patients.
Spirometry
The spirometric test was performed using electronic spirometry (CHESTGRAPH HI-101).
Cardiac assessment
-
a
Electrocardiogram (ECG): 6 lead electrocardiograms were done.
-
b
Echocardiography: All patients had a two-dimensional transthoracic Doppler echocardiogram while laying on their left side, utilizing the eSaoteSpA Mylab50 X vision echocardiography equipment. The measurement of SPAP was conducted using a continuous wave Doppler assessment to evaluate tricuspid insufficiency. The MPAP is determined by measuring the peak PR Doppler signal. PHTN was considered when SPAP was more than 25 mmHg. Mild PHTN ranged from 25 to 40 mmHg, moderate PHTN ranged from 40 to 55 mmHg, and severe PHTN was more than 55 mmHg [14]. Apical four-chamber view was used to estimate the RV’s dimensions. Measuring the right ventricular outflow tract (RVOT) was conducted with two-dimensional echocardiograms at the aortic root level, namely in the para-sternal short axis view. The TAPSE phenomenon was seen using a four-apical chamber view acquired via the use of an M-mode probe.
Pro BNP
The values of Pro BNP for this analysis were acquired from blood samples taken at the beginning of the study using a Myriad-RBM assay (Austin, TX).
Statistical analysis
Our team analyzed the data statistically with SPSS v26, a statistical tool developed by IBM Inc. of Chicago, IL, USA. For quantitative variables, we utilized means and standard deviations (SDs). To conduct a comparison among groups, we employed an analysis of variance (ANOVA) and then a Tukey post hoc test. For assessing qualitative traits, the chi-square test was utilized. Researchers showed a relationship between several variables using the Pearson moment correlation equation. In a two-tailed test, a significance level of 0.05 was deemed statistically significant.
Results
The demographic data reveals that the severe COPD group had a notably greater age in comparison to both control and mild/moderate COPD groups. Significant changes were seen in the smoking index, systolic blood pressure (SBP), diastolic blood pressure (DBP), and HR across all groups. The three groups did not exhibit any significant differences in comorbidities, including diabetes mellitus, renal dysfunction, and hepatic impairment. Significant variations were seen in the symptoms of COPD, as well as the symptoms and signs of PHTN, between the group developing mild to moderate COPD and the group developing severe COPD, as illustrated in Table 1.
Regarding laboratory examinations, significant variances were documented as regards C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), carbon dioxide (CO2), bicarbonate (HCO3), partial pressure of oxygen (PaO2), and O2 saturation between the mild/moderate and severe groups. There was a substantial increase in Pro BNP levels observed within the severe COPD group as opposed to both the mild/moderate COPD and control groups. However, no significant variances were documented between the control and the mild/moderate COPD groups (Table 2).
There were substantial differences observed in the spirometric measures (forced expiratory volume (FEV)1/forced vital capacity (FVC), FEV1, FVC) through the three groups (Table 3).
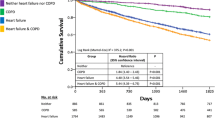
As regards echocardiographic assessment in the studied groups, on categorizing PHTN severity, mild and moderate PHTN were most common in our patients with percentages 33.75% and 35% respectively while severe PHTN without right-sided heart failure and severe PHTN with right-sided heart failure were less frequent with percentages 5% and 3.75% respectively. In mild/moderate COPD group, PHTN was found to be present in 65% of patients (35% of mild severity and 25% of moderate severity) while in severe COPD group PHTN was found to be present in 90% of patients and it was found to be mild in 32.5% of patients and moderate in 45% of patients (Table 4, Fig. 2).
SPAP, MPAP, quantitative function of RV (RVMD, RVBD, RVOT above pulmonary valve and aortic valve), and qualitative function of RV (TAPSE and RVEF) were significantly different among the three groups (Table 5).
As regards correlation between spirometric measurements, serum pro BNP, and echocardiographic findings, a negative association was documented between FEV1% and (SPAP and MPAP). A positive association was also observed between FEV1% and (TAPSE and RVEF) and between Pro BNP and (SPAP and MPAP) (P = 0.001). A negative association was documented between FEV1% and (RVMD and RVBD) and between Pro BNP and (TAPSE and RVEF) (Table 6).
Discussion
The etiology of PHTN in CLD complex is influenced by several factors. The heightened tone seen in tiny pulmonary arteries may be attributed to the pulmonary vasoconstriction as a result of hypoxia, the proliferation of capillary endothelium as well as smooth muscle cells, and the muscularization of arteries that were previously non-muscular [15]. A thorough understanding of the precise mechanism behind the association between persistent hypoxemia and PHTN is still lacking. However, practical studies have shown that prolonged lack of oxygen may cause damage to the endothelium, hence hindering the ability of prostacyclin and nitric oxide to regulate vascular remodeling [16].
COPD remains linked to altered structure and mechanics within the pulmonary vascular bed, leading to an elevation in RV afterload. Consequently, this condition is also linked to unfavorable outcomes, involving elevated hospital readmissions and death [17].
On assessment of cardiac condition in our COPD patients, SBP, DBP, and HR exhibited significant variances among all groups. Supporting our results, Arslan et al. [18] proposed that individuals with COPD exhibited notably greater systolic and diastolic blood pressure measurements as opposed to controls. The research conducted by Warnier et al. [19] showed that individuals with COPD had a higher mean heart rate (72 bpm (SD 14)) in comparison to the control group (65 bpm (SD 13), P < 0.001). There were notable differences in the symptoms and indications of PHTN between the mild/moderate COPD group and the severe COPD group. Rao and Eswaramma [20] demonstrated that pedal edema was the most often seen physical manifestation of cor-pulmonale, followed by the presence of a loud second heart sound in 20.96% of patients.
The severe COPD group had substantially elevated levels of CRP and ESR in comparison to the mild/moderate COPD group, as seen in laboratory examinations. Wang et al. [21] concurred with our findings, determining that ESR levels might partially indicate the severity of COPD in older patients and exhibit a negative correlation with FEV1%, which is a measure of lung function.
In relation to ABG, the severe COPD group had markedly elevated levels of CO2 and HCO3 as opposed to the mild/moderate COPD group. In contrast, the group with severe COPD had a significant reduction in PaO2 and O2 saturation in comparison to the group with mild to moderate COPD. Consistent with our findings, Çaltekin et al. [22] observed that severe COPD patients exhibited lower pH and PO2 values, whereas greater values were seen for PCO2 and HCO3 when compared to mild and moderate COPD patients.
We found statistically significant variances among all groups when it came to spirometric measures. El Gazzar et al. [23] provided strong evidence that spirometric measurements (FEV1/FVC%, FVC%, FEV1%, MVV% of predicted, as well as PaO2) exhibited significant reductions with increasing COPD severity, lending credence to our claims. Our research found that 77.5% of COPD patients had PHTN, in the following proportions: 33.75% for mild, 35% for moderate, 5% for severe without right-sided heart failure, and 3.75% for severe with right-sided heart failure. Over two-thirds of the individuals in the mild to moderate COPD group had PHTN. In 35% of cases, it was determined to be mild, 25% to be moderate, and 5% to be severe. In the group of individuals with severe COPD, 90% had PHTN, without right-sided cardiac problems, it was determined to be mild in 32.5% of patients, moderate in 45%, and severe in 5% of patients, and only 7.5% of patients had severe PHTN with right-sided heart failure. Similarly, the study conducted by Gupta and Mann [24] had shown a strong association between the PHTN occurrence and COPD severity. The research by Gupta et al. [2] addressed that 42.5% of COPD cases developing varied severity degrees had indications of PHTN. Furthermore, it has been shown that severe PHTN is only seen in cases with severe or very severe COPD. Scharf et al. [25] proposed that there has been a documented prevalence of up to 60% of patients with severe COPD experiencing PHTN.
In our study, we observed significant increases in RVMD, RVBD, RVLD, RVOT above pulmonary valve, and RVOT above aortic valve within the mild/moderate COPD group as opposed to controls. Similarly, these values are greater within the severe COPD group as opposed to both the control and mild/moderate COPD groups. In accordance with the findings of Jeji et al. [26], a noteworthy correlation was seen between the dimensions of the RV and the extent of COPD. This was shown by the presence of dilated RV in 23 out of 50 participants, with an average value of 34.84 ± 7.99 mm.
Regarding qualitative assessment of right ventricle, 7.5% of patients had severe PHTN with echocardiographic signs suggestive of right-sided heart failure (TAPSE < 17 mm and RVEF < 45%). Similarly, El Gazzar et al. [23] showed a total of 14% of the COPD cases involved within the research exhibited normal echocardiograms, whereas 85% displayed abnormal echocardiograms. This distribution was seen among 52% of the mild group and 92% of the moderate group, along with all cases developing severe and very severe COPD grades. Approximately 84% of the patients had tricuspid regurgitation, which ranged in severity from moderate to severe. Ninety-seven percent of patients had normal TAPSE results.
When comparing the groups developing mild to moderate COPD, the control, and severe COPD, the current study found that Pro BNP showed much greater levels within severe COPD group. The control as well as mild/moderate COPD groups, however, did not vary significantly from one another. In addition, Pro BNP was shown to have a direct correlation with SPAP and MPAP. The variables TAPSE and RVEF were shown to have a negative correlation with Pro BNP. Consistent with our findings, Su et al. [27] reached the conclusion that there are notable variations in NT-pro BNP levels throughout several phases of COPD and during the illness. These variations serve as indicators for pulmonary hypoxia extent, inflammation, and cardiovascular stress experienced by individuals with COPD.
Right heart catheterization represents the most reliable method for PHTN diagnosis and classification [28].
Combining right cardiac catheterization with echocardiography allows for a more precise diagnosis along with reducing their adverse events [29].
Soofi et al. [30] found that the RHC’s diagnostic sensitivity and specificity in diagnosing PHTN indicated 0.93 and 1 respectively.
Gonzalez-Hermosillo et al. [31] found that echo measurements of PAPm utilizing formulas incorporating PAPs exhibited good sensitivity, indicating a high positive predictive value (sensitivity 89–94% while PPV 76–88%).
The findings of our investigation revealed a significant inverse relationship between FEV1% and both SPAP and MPAP. A direct relationship was seen between FEV1% and both TAPSE and RVEF. Corroborating our findings, Jeji et al. [26] documented a noteworthy association between PAP and FEV1. The incidence of PAH patients exhibited a positive correlation with the severity of the illness as determined by GOLD staging.
An inherent constraint of this study was the very tiny sample size. The study did not include data on the previous treatment received by the participants with COPD, which might have influenced the results. The available data on the following actions is inadequate.
Conclusions
Echocardiography can be used as a screening method for early detection of PHTN and RV dysfunction in all COPD patients. Incidence of PHTN in studied COPD patients was 77.5%; it was mainly of mild and moderate degree. In mild/moderate COPD group, PHTN was found to be present in 65% of patients while in severe COPD group PHTN was found to be present in 90% of patients. PHTN is negatively correlated with FEV1%. Serum pro BNP level is negatively correlated with FEV1% in stable COPD patients. So, it could be a beneficial biomarker in assessing the severity of COPD while identifying cases possessing greater chances for complications.
Availability of data and materials
Data is available upon reasonable request from corresponding author.
Abbreviations
- ANOVA:
-
Analysis of variance
- BNP:
-
B-type natriuretic peptide
- CLD:
-
Chronic lung disease
- COPD:
-
Chronic obstructive pulmonary disease
- DBP:
-
Diastolic blood pressure
- ECG:
-
Electrocardiogram
- FEV:
-
Forced expiratory volume
- HR:
-
Heart rate
- MPAP:
-
Mean pulmonary arterial pressure
- PAP:
-
Pulmonary arterial pressure
- PHTN:
-
Pulmonary hypertension
- RHC:
-
Right heart catheterization
- RV:
-
Right ventricular
- RVBD:
-
Right ventricular basal diameter
- RVEF:
-
Right ventricular ejection fraction
- RVLD:
-
Right ventricular longitudinal diameter
- RVMD:
-
Right ventricular mid diameter
- RVOT:
-
Right ventricular outflow tract
- SBP:
-
Systolic blood pressure
- SDs:
-
Standard deviations
- SPAP:
-
Systolic pulmonary artery pressure
- TAPSE:
-
Tricuspid annular plane systolic excursion
References
Association AL (2013) Trends in COPD (chronic bronchitis and emphysema): morbidity and mortality. MMWR Morb Mortal Wkly Rep 140:51–102
Gupta N, Agrawal RK, Srivastav A, Ved M (2011) Echocardiographic evaluation of heart in chronic obstructive pulmonary disease patient and its co-relation with the severity of disease. Lung India 28:105–121
Doi M, Nakano K, Hiramoto T, Kohno N (2003) Significance of pulmonary artery pressure in emphysema patients with mild-to-moderate hypoxemia. Respir Med 97:915–20
Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL (2005) Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest 128:2099–2107
Daniels LB, Krummen DE, Blanchard DG (2004) Echocardiography in pulmonary vascular disease. Cardiol Clinic. 22:383–99
Goetze JP, Bruneau BG, Ramos HR, Ogawa T, de Bold MK, de Bold AJ (2020) Cardiac natriuretic peptides. Nat Rev Cardiol 17:698–717
Nishimura K, Nishimura T, Onishi K, Oga T, Hasegawa Y, Jones PW (2014) Changes in plasma levels of B-type natriuretic peptide with acute exacerbations of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 9:155–162
Goudie AR, Lipworth BJ, Hopkinson PJ, Wei L, Struthers AD (2014) Tadalafil in patients with chronic obstructive pulmonary disease: a randomised, double-blind, parallel-group, placebo-controlled trial. Lancet Respir Med 2:293–300
Vitulo P, Stanziola A, Confalonieri M, Libertucci D, Oggionni T, Rottoli P et al (2017) Sildenafil in severe pulmonary hypertension associated with chronic obstructive pulmonary disease: a randomized controlled multicenter clinical trial. J Heart Lung Transplant 36:166–174
Vizza CD, Hoeper MM, Huscher D, Pittrow D, Benjamin N, Olsson KM et al (2021) Pulmonary hypertension in patients with COPD: results from the comparative, prospective registry of newly initiated therapies for pulmonary hypertension (compera). Chest 160:678–689
Verberkt CA, van den Beuken-van Everdingen MHJ, Schols J, Hameleers N, Wouters EFM, Janssen DJA (2020) Effect of sustained-release morphine for refractory breathlessness in chronic obstructive pulmonary disease on health status: a randomized clinical trial. JAMA Intern Med 180:1306–1314
Lewthwaite H, Jensen D, Ekström M (2021) How to assess breathlessness in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 16:1581–1598
Agustí A, Celli BR, Criner GJ, Halpin D, Anzueto A, Barnes P et al (2023) Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Eur Respir J 61:18–20
Wood C, Balciunas M, Lordan J, Mellor A (2021) Perioperative management of pulmonary hypertension. A review. J Crit Care Med (Targu Mures) 7:83–96
Weitzenblum E, Chaouat A, Canuet M, Kessler R (2009) Pulmonary hypertension in chronic obstructive pulmonary disease and interstitial lung diseases. Semin Respir Crit Care Med 30:458–470
Poor HD, Girgis R, Studer SM (2012) World health organization group III pulmonary hypertension. Prog Cardiovasc Dis 55:119–127
Nasir SA, Singh S, Fotedar M, Chaudhari SK, Sethi KK (2020) Echocardiographic evaluation of right ventricular function and its role in the prognosis of chronic obstructive pulmonary disease. J Cardiovasc Echogr 30:125–130
Arslan S, Yildiz G, Özdemir L, Kaysoydu E, Özdemir B (2019) Association between blood pressure, inflammation and spirometry parameters in chronic obstructive pulmonary disease. Korean J Intern Med 34:108–115
Warnier MJ, Rutten FH, Numans ME, Kors JA, Tan HL, de Boer A et al (2013) Electrocardiographic characteristics of patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 10:62–71
Rao VV, Eswaramma S (2016) Study of cardiovascular changes in COPD by ECG & 2D echo and correlation with duration and severity of COPD. Sch J App Med Sci 4:4430–4438
Wang L, Yang H, Gu W (2021) Value of erythrocyte sedimentation rate and serum EPO levels in evaluating the condition and prognosis of COPD in the elderly. Pak J Pharm Sci 34:435–439
Çaltekin İ, Gökçen E, Albayrak L, Atik D, Savrun A, Kuşdoğan M et al (2020) Inflammatory markers and blood gas analysis in determining the severity of chronic obstructive pulmonary disease. Eurasian J Crit Care 2:187–192
El Gazzar AG, Essawy TS, Ebaid HH, Mohammad AED, AboYoussof SM (2022) Integrated use of transthoracic ultrasound and echocardiography in evaluating patients with chronic obstructive pulmonary disease. Egypt J Crit Care Med 88:3668–3675
Gupta R, Mann S (2016) Correlation between COPD and echocardiographic features with severity of disease. NJIRM 7:147–247
Scharf SM, Iqbal M, Keller C, Criner G, Lee S, Fessler HE (2002) Hemodynamic characterization of patients with severe emphysema. Am J Respir Crit Care Med 166:314–322
Jeji PS, Kapila S, Gupta S, Mittal S (2020) Echocardiographic evaluation of right heart in patients of chronic obstructive pulmonary disease. COPD 10:1
Su X, Lei T, Yu H, Zhang L, Feng Z, Shuai T et al (2023) NT-proBNP in different patient groups of COPD: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 18:811–825
Mehra MR, Canter CE, Hannan MM, Semigran MJ, Uber PA, Baran DA et al (2016) The 2016 International Society for Heart Lung Transplantation listing criteria for heart transplantation: a 10-year update. J Heart Lung Transplant 35:1–23
Elmonim SMA, Elsharawy DE, Elsheikh RG, Elkholy MGA (2023) Role of right heart catheterization in diagnosis of pulmonary arterial hypertension. Egypt J Chest Dis Tuberc 72:570–8
Soofi MA, Shah MA, AlQadhi AM, AlAnazi AM, Alshehri WM, Umair A (2021) Sensitivity and specificity of pulmonary artery pressure measurement in echocardiography and correlation with right heart catheterization. J Saudi Heart Assoc 33:228–236
Gonzalez-Hermosillo L-M, Cueto-Robledo G, Roldan-Valadez E, Graniel-Palafox L-E, Garcia-Cesar M, Torres-Rojas M-B et al (2022) Right heart catheterization (RHC): a comprehensive review of provocation tests and hepatic hemodynamics in patients with pulmonary hypertension (PH). Curr Probl Cardiol 47:101351
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [Mohamed Ahmed Fouad Abdelalim], [Mohamed A. Khalil] and [Ragia Samir Sharshr]. The first draft of the manuscript was written by [Ayman Hassan Abdelzaher] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was conducted between November 2022 and November 2023, after the authorization of the Ethical Committee of Tanta University Hospitals in Tanta, Egypt (Approval code: 35666/8/22). The patients provided informed written consent.
Consent for publication
Not applicable.
Competing interests
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelalim, M.A.F., Khalil, M.A., Sharshr, R.S. et al. The role of transthoracic echocardiography in evaluating right ventricular parameters in chronic obstructive pulmonary disease. Egypt J Bronchol 18, 71 (2024). https://doi.org/10.1186/s43168-024-00325-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-024-00325-7