Abstract
Introduction
The aim of this study was to investigate patients’ preferences regarding the evolving treatment landscape in Crohn’s disease (CD) and ulcerative colitis (UC) based on a discrete choice experiment.
Methods
Eligible patients (aged 18 years or older) had a confirmed diagnosis of CD or UC and were willing and able to participate in telephone interviews. The survey design is based on a prior literature review, a pilot study, and clinical expert discussions. Preferences related to clinical and practical features of advanced therapies, like tumor necrosis factor alpha inhibitors, anti-integrins, anti-interleukins, and Janus kinase inhibitors, were assessed. Patients were asked to choose between two different hypothetical treatment alternatives visualized in up to 11 choice scenarios. Based on these choices, the relative importance of treatment characteristics was derived from regression coefficients estimated by a conditional logit model.
Results
Of the 291 patients included, 219 (75%) were eligible for this analysis. Among the evaluated attributes in CD, 1-year remission rate was ranked highest, with 42.3% relevance for the overall decision. The second most important attribute was the frequency of serious adverse events (AE) (25.1%), followed by sustained remission over 2 years (17.8%). Lower importance was assigned to the administration mode (14.6%) and none to the frequency of non-serious AE (0.1%). In UC, preferences were driven by efficacy (25.3% for mucosal healing; 23.4% for corticosteroid-free remission) and the frequency of serious AE (18.3%), followed by the administration mode (18.1%). Also, non-serious AE were classified as relevant factors for decision-making (10.7%), while maintaining remission for at least 2 years showed no significant impact (4.4%).
Conclusion
For both indications, efficacy outcomes were rated most important, followed by the frequency of serious AE. Variations were mainly found in the evaluation of non-serious AE and sustained remission. Considering patient preferences may improve the effectiveness of available therapies for moderate to severe CD and UC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Treatment characteristics determine its convenience and thus impact patients’ quality of life. Because patients are more likely to adhere to therapies that match their preferences, actively involving patients in therapeutic decisions can have a significant impact on treatment outcomes. |
The aim of this study was to assess patients’ preferences for advanced therapies used in inflammatory bowel diseases based on a discrete choice experiment using structured telephone interviews. |
What was learned from the study? |
Preferences are expressed both as the importance of attributes in comparison to each other with respect to treatment decisions of surveyed patients and as utility associated with each specific attribute level. |
Long-term efficacy and avoidance of serious adverse events are most important, while the route of administration is a secondary consideration. |
Treatment preferences were similar between German patients with ulcerative colitis and Crohn’s disease. |
Introduction
Inflammatory bowel diseases (IBD), comprising ulcerative colitis (UC) and Crohn’s disease (CD), are characterized by chronic inflammation of the gastrointestinal tract. Since the beginning of this century, the prevalence of actively treated patients with IBD in Germany has increased to more than 600,000 [1]. Age-specific incidence rate were highest in the second to fourth decade of life for both UC and CD [1]. As a result of physical strain and psychosocial impairments in everyday life, patients with IBD are affected by substantial disruption of their quality of life (QoL) [2].
The primary therapeutic objective in IBD is a long-lasting corticosteroid (CS)-free disease remission with an improved QoL. When a long-term medical treatment is required, clinical guidelines for IBD recommend the use of anti-inflammatory agents such as aminosalicylates, conventional immunosuppressants (azathioprine, mercaptopurine), biologic therapies, or small molecules [3, 4]. In patients who have failed conventional therapy, the choice of drug for advanced treatment is based on the course of disease and patient-based criteria like comorbid conditions and previous therapies [4, 5]. Recent drug approvals have increased the armamentarium of advanced therapies for IBD. In Europe, the anti-tumor necrosis factor alpha (anti-TNFα) antibodies infliximab and adalimumab, the interleukin antibody ustekinumab, and the anti-integrin agent vedolizumab are biologic treatments indicated for moderately to severely active CD and UC in patients, who did not respond to conventional treatment or have contraindications to such therapies. In addition, the anti-TNFα agent golimumab, the small-molecule Janus kinase (JAK) inhibitors tofacitinib and filgotinib and the sphingosine 1-phosphate receptor modulator ozanimod are approved for UC only.
In summary, a considerable number of new agents entered the market in the last 5 years, and, in addition to anti-TNFα inhibitors, several treatment options have become available for patients with moderate to severe CD or UC. The real-world efficacy of the available therapies can be considerably influenced by the patient preferences. Yet, little is known about those so far worldwide and even less so for patients in Germany. Therefore, the InPuT study (“Inflammatory Bowel Disease Patients’ Treatment Preferences Using a DCE Technique”) was initiated to investigate and compare patient preferences towards advanced treatment options for CD and UC in Germany, using a discrete choice experiment (DCE).
Methods
Study Design
This patient preference study was a cross-sectional, multicentric survey conducted among German patients with IBD from January to November 2020. To develop the DCE questionnaire, a preliminary qualitative investigation was conducted assessing the relevance of different treatment characteristics for patients with IBD, reflecting short-term and long-term efficacy, safety, time since market approval, and mode of administration (MoA) [6]. Semi-structured interviews were conducted with a total number of 30 patients (15 each with CD and UC). Participants were presented with a list of therapeutic attributes that they were asked to rank in order of importance on a 10-point Likert scale. Additionally, the distinctiveness of each attribute was rated on a four-point Likert scale by comparing the corresponding attribute levels. A list of all attributes assessed is included in the electronic supplementary material. In the pilot study, therapeutic safety was found to be the most important treatment attribute for patients, followed by long-term efficacy, while MoA, time since market approval, and short-term efficacy were rated as less important. To quantitatively test the importance of MoA, it was decided to include this attribute in the DCE design. The final list of attributes was discussed and approved within the steering board of this study, including clinical experts from gastroenterology practice.
Survey participants were recruited at 24 study sites of outpatient gastroenterologists from across Germany. Participating study sites were asked to consecutively enroll up to 35 patients who met the predefined inclusion criteria. Patients were eligible for the study if they had a minimum age of 18 years, were diagnosed with CD or UC, and received treatment with either systemic CS, conventional immunosuppressants, or advanced therapies within 12 months prior to study inclusion. Furthermore, written informed consent was obtained from each participant confirming their willingness and ability to participate in a telephone interview in the German language.
We collected data for up to 300 patients with IBD via an electronic case report form completed by the participating study sites and through telephone interviews with enrolled patients. Previously, each participant received the selection cards for visualization of the DCE in written form. At the beginning of each interview, the attributes were explained in detail to the participants by experienced interviewers who were thoroughly trained and supervised by the research organization (Ingress-Health HWM GmbH). The telephone interviews were guided by a questionnaire displayed on a computer screen, allowing the interviewer to focus entirely on the interview itself. Patient responses were entered directly into the survey database in a structured format, eliminating the need for additional data processing (e.g., transcription, data entry, and coding) and potential documentation errors.
Study variables
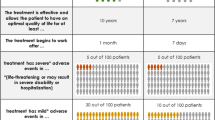
Two separate DCE questionnaires were designed, allowing for the distinction of patient preferences between CD and UC. The therapy characteristics included in this survey were derived from a preliminary qualitative study of 30 patients. In the final DCE design, five attributes were included for CD:
-
“Mode of administration”
-
“Intravenous infusion every 4–8 weeks (treatment duration 0.5–2.0 h)”
-
“Subcutaneous injection every 1–2 weeks (can be self-administered at home)”
-
“Subcutaneous injection every 4–12 weeks (can be self-administered at home)”
-
-
“Serious adverse event (SAE) rate in the first year of treatment”
-
“9 of 100 patients”
-
“25 of 100 patients”
-
-
“Adverse event (AE) rate in the first year of treatment”
-
“59 of 100 patients”
-
“87 of 100 patients”
-
-
“Remission rate after 52 weeks”
-
“7 of 100 patients”
-
“32 of 100 patients”
-
“51 of 100 patients”
-
-
“Patients in continuous remission after 2 years of treatment”
-
“69 of 100 patients”
-
“82 of 100 patients”
-
“92 of 100 patients”
-
In UC, six attributes were selected to reflect the most relevant therapy characteristics:
-
“Mode of administration”
-
“Intravenous infusion every 4–8 weeks (treatment duration 0.5–2.0 h)”
-
“Subcutaneous injection every 1–2 weeks (can be self-administered at home)”
-
“Subcutaneous injection every 4–12 weeks (can be self-administered at home)”
-
“Oral intake of one tablet, twice daily”
-
-
“SAE rate in the first year of treatment”
-
“5 of 100 patients”
-
“23 of 100 patients”
-
-
“AE rate in the first year of treatment”
-
“49 of 100 patients”
-
“85 of 100 patients”
-
-
“CS-free remission rate after 52 weeks”
-
“6 of 100 patients”
-
“14 of 100 patients”
-
“45 of 100 patients”
-
-
“Patients in continuous remission after 2 years of treatment”
-
“72 of 100 patients”
-
“85 of 100 patients”
-
“95 of 100 patients”
-
-
“Patients, who achieved mucosal healing within 52 weeks”
-
“13 of 100 patients”
-
“31 of 100 patients”
-
“55 of 100 patients”
-
Regarding the safety attributes, two levels per attribute were determined according to the minimum and maximum event rates of each side effect reported in the respective pivotal clinical trials on CD [7,8,9,10,11] and UC [12,13,14,15,16,17], which have been identified in a prior targeted literature search. With respect to attribute levels, three levels were defined for the efficacy attributes describing the minimum, median, and maximum values derived from the literature. For MoA, three different treatment options were considered in CD, representing the available treatment regimens in this indication. Because the JAK inhibitor tofacitinib was the only approved oral treatment for UC during the study period, an additional attribute level (oral use—twice daily) was added to the DCE design in UC. The description of the MoA corresponded to the details presented in the summary of product characteristics of the respective agents.
To reduce the number of choice alternatives during the telephone interviews for the DCE, a fractional factorial design was generated on the basis of an orthogonal main-effects design, using STATA/MP 14. Thus, the number of hypothetical choice sets was minimized to ensure that they could be handled by interviewed participants, while it remained possible to conclude utilities for all possible treatment alternatives. The fractional design resulted in eight different choice sets for patients with CD and 11 choice sets for patients with UC (each with two alternative treatment options). In addition, it was supplemented with a test card displaying identical choices of a previous choice set in reverse order to assess the consistency of a patient’s responses. Finally, the choice sets were graphically visualized. Figure 1 gives an example of a visualized choice card and displays two different hypothetical treatment alternatives for UC derived from a combination of the defined attributes and the respective level. Patients needed to decide between option A and B.
Additionally, information on patient characteristics (age, gender, disease activity) and medication history at the time of inclusion were gathered retrospectively by the participating study sites on the basis of their medical records. The information on disease burden (rated from 1 to 4, marginal–high) and previous treatment experience was assessed as patient-reported outcomes during the telephone interviews with the participants.
Statistical Analysis
As proposed by Johnson and Orme [18], the minimum sample size required for the DCE was calculated separately for each indication:
- c :
-
Largest number of attribute levels
- t :
-
Number of choice sets
- a :
-
Number of alternatives
As a result, the minimum sample size for the DCE was 94 subjects with CD (eight choice sets with two alternative scenarios and a maximum of three attribute levels) and 90 with UC (11 choice sets with two alternative scenarios and a maximum of four attribute levels). Another rule of thumb, proposed by Pearmain and Kroes [19], suggested that, for DCE designs, sample sizes over 100 can provide a basis for modeling preference data. Accordingly, the design of this study fulfills both conditions.
Patient characteristics were analyzed at study inclusion using descriptive summary statistics. For categorical variables, absolute and relative frequencies were reported. For continuous variables, mean, standard deviation, and median were calculated.
Inconsistency in the DCE was assessed on the basis of responses given to a test set. This test set displayed an identical choice with a reversed order of choice alternatives. Patients with conflicting responses to those test cards were excluded from the analyses. The DCE data set was analyzed using a conditional logit regression model that included the treatment attributes as independent variables. The conditional logit relates to the probability of choice among the alternatives (choice sets) to the characteristics of the attribute levels defining those alternatives.
The relative importance of each attribute for the overall decision was calculated on the basis of the absolute distance between the minimum and maximum coefficients of the level of each attribute. The relation of the coefficient distance of each attribute to the sum of the absolute coefficient distances of all attributes can be interpreted as relative importance.
A latent class analysis was applied to account for potential heterogeneity in treatment preferences by identifying distinct patient segments. Additionally, separate conditional logit regression models were estimated for predefined subgroups. In total, nine subsamples were analyzed for both indications: “Age median” (38 years vs. ≥ 38 years), “Gender” (male vs. female), “Disease burden” (marginal/low vs. moderate/severe), “Disease activity” (according to the global physician’s assessment [PGA]) (normal/mild vs. moderate/high), “IV experience” (Yes vs. No), “SC experience” (Yes vs. No), “Travelling time to treating physician” (< 26 min vs. ≥ 26 min), “Interview timing before COVID-19 outbreak” (before 1 March 2020 vs. after 1 March 2020), and “Disease duration” (≤ 3 years vs. > 3 to ≤ 7 years vs. > 7 years).
All statistical analyses were performed using STATA/MP 14 and Microsoft Excel.
Regulatory Aspects and General Considerations
This cross-sectional survey was a non-interventional study, which was approved by an independent ethics committee (Medical Faculty at the University of Rostock; registered under A 2019-0058). The study was conducted in accordance with the Declaration of Helsinki. Participants provided written informed consent prior to their enrollment in the study. All procedures of the conducted survey were carried out in accordance with the guidelines laid out by the ISPOR Good Research Practices for Conjoint Analysis Task Force [20].
Within this study, there was no assignment of a patient to a particular therapeutic strategy. The treatment decision fell within the current medical practice and was explicitly independent of the decision to include the patient in the study. No additional diagnostic or monitoring processes were required for the inclusion or during the study.
Results
Patient Characterization
In total, 291 patients with IBD (149 with CD and 142 with UC) were included in this DCE. As a result of inconsistent answers given in the DCE, 72 patients had to be excluded. The final study cohorts consisted of 118 patients with CD (female share 56.8%) and 101 patients with UC (female share 47.5%). Both samples were on average about the same age at the time of study inclusion (mean age 39.6/39.8 years). No significant differences were detected between the DCE analysis sets and excluded patients in terms of gender and age (Table 1).
Mean time since CD diagnosis was 13.7 years, while patients with UC had a mean diagnosis of 11.1 years at study inclusion. Gastroenterologists reported mild or no disease activity for most of the patients analyzed with CD (77.1%) and UC (56.5%). Most patients with CD (87.3%) and patients with UC (80.2%) were exposed to advanced therapies within the last 12 months prior to study inclusion. Among the analyzed sample of patients with CD, 103 patients (87.3%) had previous experiences with biological therapies, whereas 81 (80.2%) patients diagnosed with UC had received advanced therapies including JAK inhibitors. Other recently used therapies associated with CD/UC management were locally acting corticosteroids (CS; 7.6%/12.9%), systemic CS (22.9%/33.7%), aminosalicylates (11.0%/51.5%), and other conventional immunosuppressives (18.6%/24.8%).
Within the DCE analysis sample, 190 out of 219 patients reported previous experience with intravenous (IV) medication application. Out of the 190 patients, 150 (78.9%) experienced the IV application as “not stressful” or “marginally stressful”. Furthermore, significantly more patients with UC received a subcutaneous (SC) medication application prior to the time of the interview than patients with CD (61.9% vs. 35.6%; p < 0.001). Of those patients who had experience with an SC application (n = 109), more than one in four reported experiencing moderate to high levels of distress from the treatment (31.2%). To reach their treating gastroenterologist, patients traveled a mean distance of 17.0/22.3 km (CD/UC), for which they needed a mean travel time of 25.7/30.2 min (CD/UC).
Patients’ Preferences
Generally, patients with CD preferred treatment alternatives that are characterized by a higher remission rate after 52 weeks, a lower probability for severe side effects, and an increased likelihood to maintain remission over 2 years of treatment. In addition, patients were in favor of therapies with longer treatment intervals regardless of the proposed MoA (SC or IV). The utilities associated with each attribute level as well as the relative influence of the given attributes on the overall decision regarding the CD therapy are shown in Fig. 2. Based on the results from conditional logit regression models, patients ranked the importance of the different attributes towards their treatment decision as follows: “Remission rate after 52 weeks” (42.3% influence on overall treatment decision), “SAE rate in the first year of treatment” (25.1% influence), “Patients in continuous remission after 2 years of treatment” (17.8% influence), “Mode of administration” (14.6% influence), and “AE rate in the first year of treatment” (0.1% influence).
Patients with UC clearly preferred treatment options providing better efficacy in terms of mucosal healing and CS-free remission. Also, similar to Crohn’s disease, patients preferred therapies that have a lower likelihood of causing SAEs. There was no clear preference regarding the route of administration. However, an SC injection every 1–2 weeks was the lowest-rated option compared to all other alternatives (IV infusion every 4–8 weeks, SC injection every 4–12 weeks, or one tablet twice a day). The achievement of mucosal healing and a CS-free remission after 52 weeks were the highest-ranked attributes, with 25.3% and 23.4% relevance for the overall choice, respectively (Fig. 3). This was followed by the likelihood of avoiding SAEs in the first year of treatment (18.3%) and MoA (18.1%). Significantly less relevance was assigned to non-severe AEs (10.7%) and remission maintenance after 2 years of treatment (4.4%).
For both indications, no preference segments were identified by the conducted latent class analysis. Furthermore, the results of separately performed multivariate regression analyses for subgroups stratified by predefined patient characteristics confirmed the homogeneity of treatment preferences in the two study cohorts (Figs. S1 and S2 in the supplementary material).
Discussion
Patient Treatment Preferences in IBD
In this study, we investigated the treatment preferences of patients with CD and UC towards different attributes of advanced therapies for IBD by applying two indication-specific DCE approaches. To the best of our knowledge, this is the first study of its kind in Germany. Our results from conditional logit regression models showed that for both IBD conditions the efficacy of therapy or specifically the achievement of remission after 1 year was rated as the most important aspect of the treatment decision-making process (CD: 42.3%; UC: 48.7% based on 25.3% for mucosal healing and 23.4% for the remission rate). This was closely followed by the appearance of severe adverse events in the first year of treatment (CD: 25.1%; UC: 18.3%). Interestingly, the preferences diverged mainly regarding the continuous remission after 2 years of therapy: While it did not play any role in the decision-making process of patients with UC, it was the third most important attribute for patients with CD (CD: 17.8%; UC: 4.4%). Non-serious adverse events, on the other hand, were not considered crucial by patients with CD, in contrast to patients with UC (CD: 0.1%; UC: 10.7%). Additional analyses revealed that these results remained stable even when different patient subgroups were examined.
As patient preference data become an important component of treatment decision-making, preference differences should be considered when recommending therapies at different stages in the treatment journey. Understanding patient preferences regarding treatment decisions is essential for gaining insights into the impact of conditions and treatments on their lives, the outcomes that matter to them, and their needs and fears. It is crucial to tailor therapies to patients’ needs because treatments that are effective in clinical trials but have low patient acceptance are likely to lose their efficacy in everyday clinical practice, e.g., as a result of inadequate adherence [21, 22]. In fact, patients do prefer to be included in the decision-making process [21, 23]. Considering patient preferences may also positively influence the patient–physician relationship, which in turn could improve medication adherence and thus increase the real-world effectiveness of therapies [24].
In contrast to that, the patient perspective is currently not systematically taken into account in health technologies assessments (HTA) by European payers. The patient perspective is not considered in cost-effectiveness analysis because it does not determine how patients value this condition, and the value (i.e., benefits) of the patient’s health condition is often determined using societal valuations. Direct patient involvement is still considered subjective, potentially biased, and unrepresentative. However, because consideration of patient preferences in therapeutic decision-making could possibly lead to more cost-effective outcomes, HTA bodies are more and more willing to incorporate patient preferences as supportive evidence examining characteristics related to drug benefits, risks, and administration. Patient preferences can be quantified and statistically analyzed on the basis of preference elicitation methods, like DCEs, enabling evidence-based decision-making [25,26,27]. Lastly, since advanced therapies are constantly evolving, regularly updating research on patient preferences regarding the relevant attributes is crucial.
Comparable studies have been performed in other countries in recent years [28,29,30,31,32,33,34,35,36,37], addressing attributes of biologic therapies by performing adaptive choice-based conjoint surveys in patients with CD and UC, respectively. The patient populations were comparable to our study (in terms of disease severity, age, etc.); also, similar attributes (efficacy, side effect profile, MoA) were assessed [29, 33,34,35]. In an online DCE, Almario et al. examined patients with CD and UC in the USA [29]. The authors found that patients with UC were more likely to value therapeutic efficacy than patients with CD (odds ratio 1.41, 95% CI 1.01–2.00), whereas in CD, patients were more likely to report the side effect profile as most important (odds ratio 1.63, 95% CI 1.16–2.30) [29]. We have not observed those differences in the German population of patients with IBD. However, also in our study, the efficacy measures and the frequency of serious adverse events were the most important attributes. Another recent DCE study from the USA looked at patients with moderate to severe UC only, weighting among others the time to symptom improvement, the chance of long-term symptom control after a 1-year therapy, the risks of serious infection and malignancy, and the mode/frequency of administration [33]. These patients considered symptom control 2.5 times as important as the time to symptom improvement; the 5-year risk of malignancy was valued almost as important as the symptom control [33]. Interestingly, among the patients with UC in our study, the continuous remission after 2 years of therapy was not rated as highly. However, the efficacy measures (1-year CS-free remission and mucosal healing) were of the highest value for the German patients as well. Of note, the efficacy attribute used in the study by Boeri et al. [33] (symptoms under control after 1 year) does not directly discriminate between achieving remission and maintaining it; hence, a direct comparison of the results is unfeasible. Moreover, the patients with UC in Boeri et al.’s study [33] clearly preferred oral administration (relative importance of oral 0.47 vs. subcutaneous 0.11 vs. intravenous 0.18), yet we did not detect any stark difference between the modes of administration tested among German patients. A recent study from Denmark investigated the treatment preferences of patients with UC who had patient characteristics comparable to our study, evaluating among others the efficacy (medicine provides a significant improvement after 8 weeks), the time to effect, and the MoA [34]. Analogous to our results, the most important attribute was the efficacy measure [34]. Moreover, the patients preferred oral formulations (vs. subcutaneous or intravenous) as well as avoiding taking steroids [34]. Lastly, a recent study from Canada examined treatment preferences of patients with CD by looking among others at the following attributes: remission for at least 1 year, adverse events that require discontinuation of the medication, MoA/dosing, risk of serious infection, and possible increased risk of certain cancers [35]. Across the range of levels considered, maintaining remission was 2.5 times more important than withdrawal due to an adverse event (median utility 10 vs. 4.07); the other attributes were less important [35]. These findings agree with the treatment preferences of patients with CD in Germany identified in the study at hand.
Taken together, despite slight experimental differences and possible minor variations in patient characteristics, one can conclude that the efficacy measures and the appearance of serious adverse events are paramount in the decision-making process of patients with moderate to severe IBD across different countries.
Limitations
Some limitations to this study need to be acknowledged. The design of the DCE used in this project consisted of complex attributes. Thus, comprehension difficulties on the patients’ side cannot be excluded completely. To maximize user-friendliness, understandability, and convenience of the DCE charts and the interview, the following measures have been taken: (i) all DCE charts were visualized and sent to the patient via mail prior to the interview, (ii) telephone interviews were carried out in a computer-assisted form, (iii) all attributes were explained in detail by experienced and in-depth trained interviewers, and (iv) all patient queries were addressed throughout the entire interviewing process. Moreover, interviewers were monitored during their first interview as well as in regular spontaneous audits to control for interview quality. Finally, the inclusion of a consistency test card allowed for the detection of inconsistent/conflicting patient response behavior.
Despite the random selection of study centers with consecutive patient inclusion, a selection bias cannot be excluded because the willingness to participate is based on the motivation of the physician/patient. Those patients may carry common disease characteristics; for example, there may have been a selection bias in favor of healthier patients.
Moreover, the number and range of attribute levels can bias the outcome. It should be noted that a significant imbalance in the number of attribute levels presented in the DCE can make patients subconsciously assign a higher importance to the attribute that is presented with a higher number of levels than other attributes. This may have been the case in the present study with the MoA in UC which were presented with four levels.
Furthermore, the range of levels for each attribute differed strongly in some cases. For remission achievement and frequency of SAEs, the defined minimum levels reflected the placebo effect as measured in pivotal clinical trials on CD [7,8,9,10,11] and UC [12,13,14,15,16,17]. However, for remission maintenance, no data were available to determine the placebo effect based on the long-term extension studies. Those attributes have been presented with a significantly smaller range which may result in lower ratings of importance by the patients.
The patient’s perception of treatment characteristics may also depend on the information provided by the treating physician. This bias was minimized by the multicenter character of this study.
Also, it was not possible to include all attributes describing the different IBD treatment options since the number of resulting choice cards would have overloaded the participating patients during the interview. Therefore, the number of choice cards was determined by means of a fractional factorial design. For the same reason, it was not possible to include an additional attribute quantifying patient preferences for paying out-of-pocket costs to assess hypothetical trade-off costs between the different treatment options. In Germany, the costs of medical treatments are usually covered in full by health insurance, and co-payments are very limited. Patients with IBD are therefore not familiar with the out-of-pocket costs. Therefore, this question would be purely hypothetical from the patient’s point of view. In addition, given the high number of therapeutic attributes, the inclusion of a “willingness to pay” item would have resulted in an increase in the number of choices, making it practically infeasible for patients to respond, as this would have significantly increased the complexity and duration of the telephone interviews. Therefore, this study was unable to determine the willingness to pay for the preferred treatment option.
We acknowledge that the willingness to accept additional SAE risk to increase the probability of efficacy would be an interesting outcome. However, because of the broad treatment spectrum, multiple levels had to be considered for efficacy and safety characteristics. Therefore, it was not possible to determine the trade-off between safety and long-term efficacy. Lastly, we studied patients with moderate to severe IBD requiring advanced treatments, which limits the generalizability of the results. In other words, the identified patient preferences may not be identical in newly diagnosed IBD.
Conclusion
This multicenter patient survey presents the first study on treatment preferences of German patients with moderate to severe IBD. In summary, our study showed that in Germany most patients consider long-term efficacy and avoidance of potential SAEs as most important when choosing a therapy, whereas the MoA is often a secondary consideration. Moreover, treatment preferences among patients with IBD in Germany appear largely homogeneous—they do not differ significantly depending on specific patient characteristics. It is essential to understand the patient perspective and to involve patients in the decision-making process on their treatment options to increase the probability of treatment adherence and persistence and thus the overall real-world efficacy of therapies.
References
Hein R, Köster I, Bollschweiler E, Schubert I. Prevalence of inflammatory bowel disease: estimates for 2010 and trends in Germany from a large insurance-based regional cohort. Scand J Gastroenterol. 2014;49(11):1325–35.
Loftus CG, Loftus EV Jr, Harmsen SW, et al. Update on the incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota, 1940–2000. Inflamm Bowel Dis. 2007;13(3):254–61.
Burisch J, Weimers P, Pedersen N, et al. Health-related quality of life improves during one year of medical and surgical treatment in a European population-based inception cohort of patients with inflammatory bowel disease: an ECCO-EpiCom study. J Crohns Colitis. 2014;8(9):1030–42.
Preiß J, Bokemeyer B, Buhr H, et al. German Society of Gastroenterology. Z Gastroenterol. 2014;52:1431.
Gomollon F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 1: diagnosis and medical management. J Crohns Colitis. 2017;11(1):3–25.
Schubert S, Knop J, Picker N, Wilke T. PGI39 inflammatory bowel disease patient’s treatment preferences-using qualitative patient survey data to develop a discrete choice experiment. Value Health. 2020;23:S150.
Hanauer SB, Feagan BG, Lichtenstein GR, et al. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. Lancet. 2002;359(9317):1541–9.
Colombel JF, Sandborn WJ, Rutgeerts P, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn’s disease: the CHARM trial. Gastroenterology. 2007;132(1):52–65.
Feagan BG, Sandborn WJ, Gasink C, et al. Ustekinumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2016;375(20):1946–60.
Sandborn WJ, Feagan BG, Rutgeerts P, et al. Vedolizumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2013;369(8):711–21.
Sandborn WJ, Rutgeerts P, Enns R, et al. Adalimumab induction therapy for Crohn disease previously treated with infliximab: a randomized trial. Ann Intern Med. 2007;146(12):829–38.
Sandborn WJ, Feagan BG, Marano C, et al. Subcutaneous golimumab induces clinical response and remission in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2014;146(1):85–95.
Moss AC, Farrell RJ. Infliximab for induction and maintenance therapy for ulcerative colitis. Gastroenterology. 2006;131(5):1649–51.
Sandborn WJ, Su C, Sands BE, et al. Tofacitinib as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2017;376(18):1723–36.
Sandborn WJ, Van Assche G, Reinisch W, et al. Adalimumab induces and maintains clinical remission in patients with moderate-to-severe ulcerative colitis. Gastroenterology. 2012;142(2):257–65.
Sands BE, Sandborn WJ, Panaccione R, et al. Ustekinumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2019;381(13):1201–14.
Feagan BG, Rutgeerts P, Sands BE, et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013;369(8):699–710.
Johnson RM, Orme BK, editors. A new approach to adaptive CBC. In: Sawtooth Software Conference, Citeseer, 2007
Pearmain D, Kroes EP. Stated preference techniques: a guide to practice. 1990. London: Steer Davies Gieave, Hague Consulting Group.
Reed F, Lancsar E, Marshall D, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR conjoint analysis experimental design good research practices task force. Value Health. 2013;16:3–13.
Horne R. Patients’ beliefs about treatment: the hidden determinant of treatment outcome? J Psychosom Res. 1999;47(6):491–5.
Wilke T, Müller S, Morisky DE. Toward identifying the causes and combinations of causes increasing the risks of nonadherence to medical regimens: combined results of two German self-report surveys. Value Health. 2011;14(8):1092–100.
Conrad S, Hüppe A, Raspe H. Zu welchen Themen wünschen Patientinnen und Patienten mit Morbus Crohn oder Colitis ulcerosa mehr Informationen und welche eigene Rolle bevorzugen sie bei medizinischen Behandlungsentscheidungen? Ergebnisse einer Betroffenenbefragung in Deutschland. Z Gastroenterol. 2012;50(04):364–72.
Van Der Pol M, Hennessy D, Manns B. The role of time and risk preferences in adherence to physician advice on health behavior change. Eur J Health Econ. 2017;18(3):373–86.
van Overbeeke E, Forrester V, Simoens S, Huys I. Use of patient preferences in health technology assessment: perspectives of Canadian, Belgian and German HTA representatives. Patient. 2021;14(1):119–28.
Ho M, Saha A, McCleary KK, et al. A framework for incorporating patient preferences regarding benefits and risks into regulatory assessment of medical technologies. Value Health. 2016;19(6):746–50.
Puhan MA, Singh S, Weiss CO, Varadhan R, Boyd CM. A framework for organizing and selecting quantitative approaches for benefit-harm assessment. BMC Med Res Methodol. 2012;12(1):1–12.
Holko P, Kawalec P, Mossakowska M. Quality of life related to oral, subcutaneous, and intravenous biologic treatment of inflammatory bowel disease: a time trade-off study. Eur J Gastroenterol Hepatol. 2018;30(2):174–80.
Almario CV, Keller MS, Chen M, et al. Optimizing selection of biologics in inflammatory bowel disease: development of an online patient decision aid using conjoint analysis. Am Coll Gastroenterol. 2018;113(1):58–71.
Gregor JC, Williamson M, Dajnowiec D, Sattin B, Sabot E, Salh B. Inflammatory bowel disease patients prioritize mucosal healing, symptom control, and pain when choosing therapies: results of a prospective cross-sectional willingness-to-pay study. Patient Prefer Adher. 2018;12:505.
MacKenzie-Smith L, Marchi P, Thorne H, Timeus S, Young R, Le Calvé P. Patient preference and physician perceptions of patient preference for oral pharmaceutical formulations: results from a real-life survey. Inflamm Intest Dis. 2018;3(1):43–51.
Lai C, Sceats L, Qiu W, Park K, Morris A, Kin C. Patient decision-making in severe inflammatory bowel disease: the need for improved communication of treatment options and preferences. Colorectal Dis. 2019;21(12):1406–14.
Boeri M, Myers K, Ervin C, et al. Patient and physician preferences for ulcerative colitis treatments in the United States. Clin Exp Gastroenterol. 2019;12:263.
Hagelund LM, Elkjær Stallknecht S, Jensen HH. Quality of life and patient preferences among Danish patients with ulcerative colitis–results from a survey study. Curr Med Res Opin. 2020;36(5):771–9.
Hazlewood GS, Pokharel G, Deardon R, et al. Patient preferences for maintenance therapy in Crohn’s disease: a discrete-choice experiment. PLoS ONE. 2020;15(1):e0227635.
van Deen WK, Kiaei B, Weaver SA, et al. A qualitative inquiry into patients’ perspectives on individualized priorities for treatment outcomes in inflammatory bowel diseases. Qual Life Res. 2020;29(9):2403–14.
Wu AA, Barros JRD, Ramdeen M, Baima JP, Saad-Hossne R, Sassaki LY. Fatores associados com a escolha da terapia nos pacientes com doença inflamatória intestinal no Brasil. Arq de Gastroenterol. 2020;57:491–7.
Acknowledgements
We thank the participants of the study.
Funding
Sponsorship for this study and the journal’s Rapid Service and Open Access Fees were funded by Takeda Pharma Vertrieb GmbH & Co. KG.
Medical Writing, Editorial, and Other Assistance
We thank Sabrina Müller (Ingress-Health HWM GmbH) for her contribution to the research design, statistical analysis, and medical writing assistance which was funded by Takeda Pharma Vertrieb GmbH & Co. KG.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Jana Knop, Stefan Schubert, and Nils Picker contributed to the study conception and design. Alisan Kahraman, Wolfgang Mohl, and Stefan Schubert contributed to the data acquisition for this study. Material preparation and formal analysis were performed by Nils Picker. Jana Knop, Stefan Schubert, Taner Cavlar and Nils Picker interpreted the results. The first draft of the manuscript was reviewed by Nils Picker and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Nils Picker participated in this study as a staff member of Ingress-Health HWM GmbH; the work of Ingress-Health HWM GmbH was funded by Takeda Pharma Vertrieb GmbH & Co. KG. Jana Knop is an employee of Takeda Pharma Vertrieb GmbH & Co. KG. Taner Cavlar is an employee of Takeda Pharma Vertrieb GmbH & Co. KG and owner of Takeda shares. Stefan Schubert, Alisan Kahraman, and Wolfgang Mohl were involved in the data collection for this study. Takeda Pharma Vertrieb GmbH & Co. KG provided funding to all participating study sites for this work. Stefan Schubert also received payments from Takeda Pharma Vertrieb GmbH & Co. KG for his participation as a consulting member in the steering board committee of this study.
Compliance with Ethics Guidelines
This cross-sectional survey was a non-interventional study, which was approved by an independent ethics committee (Medical Faculty at the University of Rostock; registered under A 2019-0058). The study was conducted in accordance with the Declaration of Helsinki. Participants provided written informed consent prior to their enrollment in the study.
Data Availability
The data sets generated and/or analyzed during the current study are available on reasonable request to researchers who provide a methodologically sound proposal. The data will be provided after their de-identification, in compliance with applicable privacy laws, data protection, and requirements for consent and anonymization.
List of Investigators
We thank the site investigators of this study for the contribution to the data acquisition: Petra Jessen, Gemeinschaftspraxis im Medicum, Altenholz, Stefan Schubert, MVZ für Gastroenterologie am Bayerischen Platz, Berlin, Lutz Emsen, InnerMed Gemeinschaftspraxis, Bühl, Johannes Janschek, Gastroenterologische Facharztpraxis, Dresden, Alisan Kahraman, Universitätsklinikum Essen, Essen, Thomas Zeisler, Facharztpraxis für Innere Medizin und Gastroenterologie, Halle (Saale), Matthias Kahl, Fachinternistische Schwerpunktpraxis, Hamburg, Stefanie Howaldt, Medizinisches Versorgungszentrum für Immunologie, Hamburg, Jens Müller-Ziehm, Gastroenterologische Schwerpunktpraxis, Hannover, Manfred von der Ohe, GSGH GbR Gastroenterologische Studiengesellschaft Herne, Herne, Jörg Schulze, Praxisgemeinschaft Jerichow , Jerichow, Jan Lammertink, Gastroenterologie am Ettlinger Tor, Karlsruhe, Peter Langmann, Gastroenterologische Gemeinschaftspraxis, Karlstadt, Gero Moog, Gastroenterologische Facharztpraxis, Kassel, Johannes Bethge, Pneumologisch – Gastroenterologische Gemeinschaftspraxis, Kiel, Johanna Dinter, Evangelisches Krankenhaus Kalk gGmbH, Köln, Julia Morgenstern, Evangelisches Krankenhaus Kalk gGmbH, Köln, Daniela Müller, MVZ Innere Medizin Marburg, Marburg, Jens Funda, PS DOCS, Pirmasens, Eric Nörgaard Jörgensen, Magen-Darm-Zentrum Remscheid, Remscheid, Stephan Orlemann, Internistische Gemeinschaftspraxis, Rödermark, Wolfgang Mohl, Zentrum für Gastroenterologie Saar MVZ GmbH, Saarbrücken, Thomas Witthöft, Gastroenterologische Gemeinschaftspraxis, Stade, Thomas Klag, Bauchraum – Gastroenterologisches Zentrum, Stuttgart, Joachim Weber-Guskar, Gastroenterologie Starnberger See, Tutzing.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Schubert, S., Picker, N., Cavlar, T. et al. Inflammatory Bowel Disease Patients’ Treatment Preferences Using a Discrete Choice Experiment Technique: The InPuT Study. Adv Ther 39, 2889–2905 (2022). https://doi.org/10.1007/s12325-022-02143-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02143-z