Abstract
Introduction
Historically, patients recently (≤ 6 months) diagnosed with pulmonary arterial hypertension (PAH; incident) have had poorer survival than those with a longer (> 6 months) time from PAH diagnosis (prevalent). Despite guideline recommendations for initial combination therapy for most patients with PAH, many are initiated and maintained on monotherapy. Real-world evidence to evaluate the benefit of early combination treatment in newly-diagnosed patients is lacking.
Methods
Patients with PAH initiating combination therapy with the endothelin receptor antagonist macitentan and the phosphodiesterase-5 inhibitor tadalafil (M+T) were identified from the combined dataset of the US, multicenter OPUS (prospective, observational drug registry; NCT02126943) and OrPHeUS (retrospective, medical chart review; NCT03197688) studies (2013–2020). Descriptive analyses were performed for the incident and prevalent cohorts, as well as the subcohort of incident patients who received M+T as first-line combination therapy (incident initial combination).
Results
In OPUS/OrPHeUS, 1336 patients with PAH received M+T during the observation period. For the incident [n = 453 (33.9%)], incident initial combination [n = 272 (20.4%)], and prevalent [n = 837 (62.6%)] cohorts: median (Q1, Q3) M+T exposure was 14.2 (4.2, 27.5), 12.2 (3.2, 25.5), and 14.7 (4.5, 28.0) months. 12-month Kaplan–Meier estimates (95% confidence limits) for survival were 91.2% (87.7, 93.7), 88.5% (83.2, 92.2), and 92.9% (90.6, 94.6), for patients free from hospitalization were 59.4% (54.1, 64.4), 56.3% (49.1, 62.9), and 62.3% (58.5, 65.9), and for patients persisting on combination therapy were 68.6% (63.9, 72.8), 65.0% (58.8, 70.6) and 66.9% (63.5, 70.0). Adverse events (OPUS only) were reported in 77.8%, 80.2%, and 80.3% of patients, respectively, with no unexpected adverse events observed.
Conclusions
Despite a historically worse prognosis, incident patients receiving M+T, including as initial combination therapy, had similar survival and hospitalization as prevalent patients. Safety profiles were similar across cohorts. Together, these data support the use of early combination therapy with macitentan and tadalafil.
Graphical Abstract

Plain Language Summary
In earlier studies, patients diagnosed with pulmonary arterial hypertension (PAH) within the past 6 months (newly-diagnosed PAH, called ‘incident patients’ in this article) had worse health than patients diagnosed with PAH more than 6 months before (long-standing PAH, called ‘prevalent patients’ in this article). This is because some newly-diagnosed patients have very advanced disease and do poorly within the first 6 months. The OPUS (NCT02126943) and OrPHeUS (NCT03197688) studies collected information on patients with PAH treated in US clinics between 2013 and 2020. We identified patients that were treated with a combination of two PAH medications, macitentan and tadalafil. We then grouped them as newly-diagnosed (453 patients) or long-standing (837 patients). We also looked at the subgroup of newly-diagnosed patients who received the combination as their first treatment (272 patients, called ‘incident initial combination patients’ in this article). We then looked at how these patients did over time. Patients were treated with macitentan and tadalafil for an average of 12–14 months. We found that after 1 year of combination treatment, results were similar between the groups: patient survival was 91%, 89%, and 93% for those with newly-diagnosed, newly-diagnosed and previously untreated, and long-standing PAH; the proportion remaining hospitalization-free was 59%, 56%, and 62%; and the proportion remaining on combination treatment was 69%, 65%, and 67%, respectively. Side effects were in line with the known safety profiles of the medications. Despite historically having worse health outcomes, newly-diagnosed patients receiving the macitentan and tadalafil combination had similar survival and hospitalization as patients with long-standing PAH. These data suggest that there is a benefit to starting this combination of medicines early in the treatment of PAH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Historically, patients newly diagnosed (incident) with pulmonary arterial hypertension (PAH) are at higher risk of death than those with a longer time from diagnosis (prevalent). |
To improve outcomes, current guidelines recommend initial oral combination therapy with an endothelin receptor antagonist (ERA) and phosphodiesterase 5 inhibitor (PDE5i) for most patients newly diagnosed with PAH. However, recent studies have shown that many patients with PAH are still initiated and maintained on monotherapy. |
What did the study ask? |
This descriptive analysis of the real-world OPUS/OrPHeUS dataset sought to describe the safety and outcomes of the combination of macitentan (ERA) and tadalafil (PDE5i) in incident (including those who were treatment-naïve and received the combination as first-line PAH-targeted therapy) and prevalent patients with PAH. |
What was learned from the study? |
Survival and time to first all-cause hospitalization were similar for incident, incident initial combination, and prevalent patients treated with macitentan and tadalafil, possibly due to the significant use of initial combination therapy in incident patients. |
The observed safety and tolerability profiles were similar for all cohorts, with no unexpected safety signals observed. |
Introduction
Pulmonary arterial hypertension (PAH) is a severe and progressive disease that, if untreated, can lead to right heart failure and death. Historically, patients with PAH who are within 6 months of diagnosis (incident) have had a poorer prognosis in terms of survival and disease progression compared to patients who are further out from diagnosis (prevalent) [1, 2], an observation that is often attributed to the fact that prevalent populations are prone to survivor bias [3]. However, analyses from the more recent US-based PHAR registry have shown no difference in all-cause mortality between incident and prevalent patients [4]. Although the reasons for this shift are presumably multifactorial, more contemporary registries likely reflect advances made in the management of PAH, including greater and earlier use of combination therapy, which has been demonstrated to improve patient outcomes [5, 6].
Initial oral combination therapy with an endothelin receptor antagonist (ERA) and phosphodiesterase 5 inhibitor (PDE5i) was first recommended for the treatment of newly diagnosed patients with PAH in the 2015 European Society of Cardiology/European Respiratory Society (ESC/ERS) treatment guidelines [7, 8], and continues to be supported in the current 2022 guidelines for the majority of patients with PAH, with the strongest recommendations for a PDE5i in combination with an ERA [9, 10]. Despite these guideline recommendations, many patients with PAH are still initiated and maintained on monotherapy in clinical practice [4, 11, 12]. Real-world insights into the effectiveness and safety of ERA and PDE5i combination therapy in the clinical setting would therefore be a valuable complement to existing data from randomized controlled trials (RCTs).
The OPsumit® USers (OPUS) Registry and OPsumit® Historical USers cohort (OrPHeUS) provide real-world data for patients with PAH newly initiated on macitentan. Although these studies were initiated to further characterize the safety profile of macitentan as part of a US Food and Drug Administration (FDA) post-marketing requirement, the breadth of data collected provides an opportunity to gather additional insights into this patient population and clinical practice in the US. The current analysis uses real-world data from the OPUS/OrPHeUS dataset to describe the demographics, clinical characteristics, safety, tolerability, and outcomes associated with initiation of the ERA macitentan and the PDE5i tadalafil in incident (including those who were treatment-naïve and receiving the combination as first-line PAH-targeted therapy) and prevalent patients with PAH.
Methods
Study Design
The OPUS and OrPHeUS studies have been previously described [11]. Briefly, OPUS was a prospective, multicenter, US, observational drug registry (April 2014–June 2020; NCT02126943) and OrPHeUS was a retrospective, multicenter, US, medical chart review (October 2013–March 2017; NCT03197688). OPUS enrolled consecutive patients newly initiating macitentan and excluded patients enrolled in any ongoing clinical trial. OrPHeUS enrolled patients newly initiating macitentan who were not enrolled in OPUS or participating in a clinical trial involving macitentan. Data collection was designed to be similar in OPUS and OrPHeUS.
Ethical Approval
The OPUS and OrPHeUS studies were conducted according to Good Pharmacoepidemiology Practices [13] and the 2008 Declaration of Helsinki ethical principles. Ethical approval was received from independent ethics committees/institutional review boards (IRB) of participating centers (Supplementary Appendix I). The protocols were reviewed by the FDA with written informed consent obtained from all patients in OPUS, including for publication of anonymized patient data (informed consent was not required in OrPHeUS as an IRB waiver was obtained). The Informed Consent Form in OPUS included a confidentiality clause that all records and documents pertaining to the participation of patients in the OPUS registry would be held strictly confidential and their names would not be reported in any publications resulting from the OPUS registry. IRB approvals were provided by WIRB and Quorum (now Advarra) (OPUS registry; WIRB approval number 2014-0816, Quorum Review File number 29120/Advarra Pro00035124) and WCG-IRB (OrPHeUS study; IRB numbers 2017-8051 and 2017-2348).
Observations and Assessments
For this analysis, the index date was defined as the start date of macitentan and tadalafil combination therapy, i.e., the date of initiation of the second drug. The observation period was from index date to the first of death, loss to follow-up, withdrawal of consent, discontinuation of tadalafil and/or macitentan plus 30 days (whichever is earlier), or study end. Data collection in OPUS and OrPHeUS (including demographics, baseline characteristics, treatment patterns, safety, hospitalizations, and deaths) have been previously described [11]. Information was collected per routine clinical practice and no assessments were mandated. The date of PAH diagnosis was investigator-reported. For this analysis, baseline assessments were defined as the closest assessment within the 6 months (12 months for right heart catheterization measurements) prior to and including the index date. Follow-up data were defined as at least one observation after the index date. In OPUS, adverse events (AEs) and serious AEs (SAEs) were recorded. In OrPHeUS, hepatic AEs (HAEs) were identified from the clinical data collected; however, no other AEs were collected. Hepatic safety data were reviewed by an Independent Liver Safety Data Review Board (Supplementary Appendix II) as previously described. Further analyses were performed to characterize adverse events of special interest (AESI), including serious hepatic events, as this was one of the primary objectives of the OPUS and OrPHeUS studies, and events of edema and anemia, as these are common side effects (occurring in ≥ 1 in 10 patients) associated with ERA and macitentan use [14, 15]. The definitions of these grouped terms are provided in Supplementary Appendix III.
Statistical Analyses
Statistical and other analyses in OPUS and OrPHeUS have been previously described [11]. Following heterogeneity analyses, patient and treatment characteristics were found to be similar in the OPUS and OrPHeUS studies, allowing for combination of the datasets [11]. All analysis cohorts described here were derived from the OPUS/OrPHeUS PAH population, which included patients with follow-up data who had PAH identified as a reason for macitentan prescription. This analysis includes all patients who received combination therapy with macitentan and tadalafil, in either order, at any time during the study (overall cohort). Three additional cohorts were also defined: the incident cohort comprised those with a time from PAH diagnosis of ≤ 6 months; the incident initial subcohort comprised patients in the incident cohort who were naïve to PAH-targeted treatment and initiated macitentan plus tadalafil within 60 days of each other (i.e., those treated with initial combination therapy as recommended in the ESC/ERS guidelines [7,8,9,10)]; and the prevalent cohort comprised patients with a time from PAH diagnosis to initiation of macitentan and tadalafil combination therapy of > 6 months.
All analyses were descriptive, and no formal statistical comparisons were made between the cohorts; analyses were conducted until the end of the observation period. Patient demographics, baseline characteristics, safety information, treatment patterns, and outcomes (hospitalization and survival) are described for patients in all cohorts. Investigator assessments were not adjudicated. Incidence rates for AEs (OPUS only), and AESIs, discontinuation of macitentan, hospitalization, and death were calculated using time to the first event and adjusted for exposure. Patients were included in each analysis until the first occurrence of the specified event, or until the end of the observation period, whichever occurred first. All Poisson models included log (exposure time) as an offset to account for the varying length of patients’ time on treatment. 95% confidence limits (CL) for rates per person-year were estimated using an unadjusted Poisson model. Time to first events for macitentan or tadalafil discontinuation, patients free from hospitalization and survival are presented using Kaplan–Meier (KM) estimates; curves were truncated at the time point when < 10% of patients were at risk in any of the cohorts, in accordance with the Pocock stopping rule [16]. Imputation rules for missing dates are detailed in Supplementary Appendix III; no other data imputations were made.
Results
Baseline Characteristics
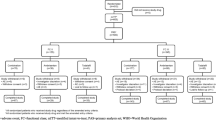
In the combined OPUS and OrPHeUS database [11], 4626 patients had a diagnosis of PAH (Fig. 1). In this analysis, there were 1336 patients with PAH who received macitentan and tadalafil double combination therapy (overall cohort); 453 (33.9%) were incident, of whom 272 (20.4%) were incident with initial combination, the remaining 181 incident patients had initiated combination therapy > 60 days apart or had a previous PAH-targeted therapy prior to initiating macitentan and tadalafil combination therapy and were not included as a separate subcohort. There were 837 (62.6%) prevalent patients and 46 patients were missing a time from diagnosis and were included in the overall cohort only. The majority of patients in all cohorts initiated tadalafil prior to macitentan (range 59.9–76.0%; Table S1).
Patient disposition: 155 sites contributed to the combined OPUS and OrPHeUS database which contained n = 5654 patients at closure. a 46 patients did not have a time from diagnosis and were not included in the incident or prevalent data. b Time from diagnosis to initiation of combination M+T therapy ≤ 6 months. c Time from diagnosis to initiation of combination M+T therapy > 6 months. M+T macitentan and tadalafil combination therapy, PAH pulmonary arterial hypertension
Patient demographics and baseline characteristics at index date are reported in Table 1. At index date, the median [interquartile range (Q1, Q3)] age [overall cohort; 60 (49, 70)] and age distribution (Fig. S1) were similar across cohorts. The proportion of female patients (overall cohort; 76.0%) and race distribution (overall cohort; 75.7% white, 15.6% Black or African American) were also well balanced across all cohorts. The median (Q1, Q3) time from diagnosis to index was 1.8 (0.7, 3.5) months for the incident cohort, 1.1 (0.5, 2.0) months for the incident initial combination subcohort, and 36.9 (15.6, 70.9) months for the prevalent cohort. Compared to the prevalent cohort, the incident cohort and incident initial combination subcohort had a higher proportion of patients with PAH associated with connective tissue disease (CTD-PAH; 26.2% vs. 32.2% and 32.0%) or portal hypertension (PoPH; 4.3% vs. 6.2% and 6.3%), whereas the prevalent cohort had a higher proportion of patients with PAH associated with congenital heart disease (CHD-PAH; 7.8% vs. 3.1% and 1.8%). Compared to the prevalent cohort, the incident cohort and incident initial combination subcohort had higher proportions of patients with diabetes (19.6% vs. 26.0% and 25.4%), obesity (20.4% vs. 23.8% and 25.4%), and edema (17.9% vs. 23.8% and 26.1%), and fewer with anemia (17.9% vs. 12.6% and 12.5%).
Information on PAH severity at index date is presented in Table 2 (missing data ranging from 50.1 to 60.7% in the overall cohort; summarized in Table S2). For those with data, versus prevalent patients, incident and incident initial combination patients had a lower median 6-min walk distance [6MWD; 332 m (n = 354) vs. 274 m (n = 166) and 268 m (n = 93)], worse World Health Organization functional class [WHO FC; III/IV: 58.2% (n/N = 234/402) vs. 72.5% (n/N = 185/255) and 74.2% (n/N = 115/155)], were more likely to be in the high-risk brain natriuretic peptide/n-terminal pro-brain natriuretic peptide (BNP/NT-proBNP) category [26.7% (n/N = 82/307) vs. 42.9% (n/N = 88/205) and 46.2% (n/N = 54/117)], and had more severe hemodynamics, including higher median pulmonary vascular resistance [6.6 Wood Units (WU) (n = 244) vs. 8.1 WU (n = 283) and 8.7 WU (n = 178)] and higher median mean pulmonary arterial pressure [44 mmHg (n = 276) vs. 46 mmHg (n = 331) and 48 mmHg (n = 206)].
Treatment Patterns
The breakdown of PAH-targeted therapy prior to and at index is shown in Table 3, with the specific combinations at index shown in Table S3. At least one prior PAH-targeted therapy was reported for 11.0% of incident and 33.5% of prevalent patients. The median (Q1, Q3) time from diagnosis to initiation of the first drug in the macitentan and tadalafil combination was 0.4 (0.0, 1.2) months, 0.4 (0.0, 1.3) months, and 8.2 (0.9, 34.9) months for incident, incident initial combination, and prevalent patients, respectively. The median (Q1, Q3) time from first drug to initiation of the second drug in the combination (i.e., index date) was 0.9 (0.2, 2.6) months, 0.4 (0.1, 0.9) months, and 16.0 (6.0, 36.9) months, for incident, incident initial combination, and prevalent patients, respectively. At index, the majority of patients were receiving macitentan and tadalafil; for those who were taking another PAH-targeted therapy, a prostacyclin pathway agent (PPA) was the most common in all cohorts (intravenous/subcutaneous [range 4.4–15.1%] and oral/inhaled [range 0−15.9%)]. For patients who escalated therapy during follow-up, the majority in all cohorts initiated an oral or inhaled PPA (Table 3). KM estimates of time to therapy escalation are shown in Fig. 2. The median (Q1, Q3) number of months for escalation from first to second drug of the macitentan and tadalafil combination was 0.9 (0.2, 2.6), 0.4 (0.1, 0.9), and 16.0 (6.0, 36.9), and from macitentan and tadalafil combination to next PAH-targeted therapy was 5.2 (1.8, 11.6), 3.4 (1.0, 7.1), and 8.2 (3.5, 16.2), for incident, incident initial combination, and prevalent patients, respectively.
KM estimates of escalation from a first to second drug of the macitentan and tadalafil combination and b macitentan and tadalafil combination therapy to additional PAH-targeted therapy. CL confidence limits, KM Kaplan–Meier, M+T macitentan plus tadalafil combination, PAH pulmonary arterial hypertension
Survival and Hospitalizations
The median (Q1, Q3) exposure to macitentan and tadalafil combination therapy was similar between the cohorts, at 14.2 (4.2, 27.5), 12.2 (3.2, 25.5), and 14.7 (4.5, 28.0), months for the incident, incident initial combination, and prevalent patients, respectively. The 12-month KM estimates (95% CL) of survival were 91.2% (87.7, 93.7) in the incident, 88.5% (83.2, 92.2) in the incident initial combination, and 92.9% (90.6, 94.6) in the prevalent cohorts; the 24-month KM estimates were 83.7% (78.5, 87.7), 81.1% (73.7, 86.7), and 84.9% (81.4, 87.7), respectively (Table 4; Fig. 3). The proportion of patients who experienced an all-cause hospitalization, as well as the incidence rate (per person-year, 95% CL), was similar in the incident [45.7%, 0.47 (0.39, 0.57)], incident initial combination [44.9%, 0.51 (0.41, 0.65)], and prevalent [41.5%, 0.39 (0.34, 0.45)] cohorts (Table 4). The 12-month KM estimates (95% CL) for patients free from hospitalization were 59.4% (54.1, 64.4) in the incident, 56.3% (49.1, 62.9) in the incident initial combination, and 62.3% (58.5, 65.9) in the prevalent cohorts; the 24-month KM estimates were 40.4% (34.5, 46.2), 39.5% (31.7, 47.1), and 49.1% (44.7, 53.3), respectively (Table 4; Fig. 4).
Safety and Tolerability
Safety data are presented in Table 5. In OPUS, the proportions of patients experiencing an AE (range 77.8–80.3%) or SAE (range 48.1–49.7%) were similar between all cohorts, but with a higher AE incidence rate (per person-year, 95% CL) in the incident initial combination [1.82 (1.38, 2.39)] compared to the incident ([1.46 (1.15, 1.84)] and prevalent cohorts [1.37 (1.10, 1.70)] (Table 5). The most common AEs were dyspnea, headache, and anemia in the incident cohort, dyspnea, headache, anemia, and hypoxia in the incident initial combination subcohort, and dyspnea, headache, and nausea in the prevalent cohort (Table 5). There was a higher proportion of patients in the incident cohort (14.8%) and incident initial combination (13.6%) subcohort who experienced an AESI (grouped terms) of anemia/hemoglobin decrease compared to the prevalent (7.1%) cohort, whereas the proportions of patients with an AESI of edema or hepatic events were similar between the cohorts (ranges 26.3–28.2% and 4.7–8.5%, respectively; Table 5).
The proportion of patients that discontinued combination therapy for any reason during the observation period was 47.5%, 50.0% and 47.3% in the incident, incident initial combination subcohort and prevalent cohorts (Table 5); the 12-month KM estimates (95% CL) for patients persisting on combination therapy were 68.6% (63.9, 72.8), 65.0% (58.8, 70.6), and 66.9% (63.5, 70.0), respectively (Table 5). The proportion of patients discontinuing macitentan, tadalafil, or both drugs, as well as the reasons for macitentan discontinuation (not collected for tadalafil), are presented in Table S4. Of patients discontinuing macitentan (range 34.9–36.8%), roughly the same proportion discontinued due to an AE (range 13.9–15.4%) versus another reason (range 13.6–15.1%), in all cohorts.
Discussion
Historically, incident patients with PAH have had poorer survival compared to prevalent patients. In contrast, in this analysis of patients receiving combination macitentan and tadalafil therapy in the combined OPUS and OrPHeUS datasets, the observed survival estimates were comparable. This occurred despite patients in the incident cohort having a higher proportion of PAH etiologies associated with poorer prognosis, more severe disease at baseline, and a higher comorbidity burden. We hypothesize that the growing use of early combination therapy may be contributing to improved outcomes in this cohort.
Although there was a high degree of missing data, it appears that incident, especially incident initial combination, patients, had more severe PAH disease than prevalent patients at the initiation of macitentan and tadalafil combination therapy. This includes more severe hemodynamics and worse WHO FC, 6MWD, and natriuretic peptide levels. This difference in PAH severity between incident and prevalent patients is consistent with previous observations in both disease registries [1, 2] and RCTs [17]. Incident patients in OPUS and OrPHeUS were also more likely to have been diagnosed with CTD-PAH and PoPH, both of which generally have poorer outcomes versus other forms of PAH versus a higher proportion of patients with CHD-PAH in the prevalent cohort. Incident patients had a median time from diagnosis to macitentan and tadalafil combination therapy of under 2 months, while the median was over 3 years for prevalent patients. Given this, the difference in PAH etiology and severity may be reflective of more aggressive treatment approaches being taken for patients with profiles associated with worse outcomes [18].
Despite these differences, survival estimates were similar between the incident and prevalent cohorts in this unadjusted, descriptive analysis. Recent analyses of the US PHAR and the Europe/Canada based EXPOSURE registry also show similar mortality rates between incident and prevalent patients [4, 19]. These findings are in contrast to earlier publications from the French and US REVEAL PAH registries, where survival rates for recently diagnosed patients were poorer than for those previously diagnosed [1, 2]. This appears to have occurred with improvements in reported survival for incident patients, rather than worsening in survival for prevalent patients. Specifically, 3-year survival rates for prevalent patients are similar across the five registries (ranging from 71 to 78%) while those for incident patients were greater in OPUS/OrPHeUS (72%), EXPOSURE (71%) [19], and PHAR (81%) [4] versus the French (51%) [1, 20] and REVEAL (69%) [2] registries. The characteristics of incident and prevalent patients were generally comparable across the studies and are unlikely to have led to this difference in survival. However, the observation periods for the French (2002–2006) [1, 20] and the REVEAL (2006–2013) [2] analyses occurred over a time when fewer targeted therapies were available, while the majority of the observation periods for OPUS/OrPHeUS (2013–2020), EXPOSURE (2017–2022) [19], and PHAR (2015–2020) [4] occurred after the release of the 2015 ESC/ERS guidelines [7, 8], which recommended initial combination therapy for most patients, rather than monotherapy. We therefore hypothesize that the similar survival rates of incident and prevalent patients observed in the more contemporary registries may in part be driven by the adoption of more aggressive treatment strategies following updated guideline recommendations, including earlier combination therapy/rapid escalation at follow-up. Although the proportions of patients receiving combination therapy are not available over the span of the REVEAL and French registries to confirm this, our hypothesis is supported by findings from analyses of the overall OPUS/OrPHeUS PAH population, which indicate increased use of double combination therapy and reductions in monotherapy from 2014 to 2019 [11].
One might also expect higher hospitalization rates for newly-diagnosed patients, as has been observed in US claims data analyses, where a higher number and longer duration of hospital visits were observed for incident patients versus prevalent patients [21]. However, in this analysis, the all-cause hospitalization rates were similar between the cohorts and high overall. Although the specific reasons for hospitalization are not available, hospital admission in general is most often related to PAH, and is one of the most common clinical worsening events in PAH trials [22]. While macitentan treatment has been shown to reduce all-cause hospitalizations in clinical trials [23], these observations highlight the need for continued risk assessment and proactive treatment escalation, in order to further optimize outcomes.
In this analysis, the median time from initiation of first to second drug in the macitentan and tadalafil combination was much longer for prevalent patients (16.0 months) than incident patients (0.9 months). Some of this lag can be explained by the fact that a third of the prevalent cohort were already on background PAH-targeted therapy (i.e., already on a form of combination therapy), and that this cohort appeared to have less severe PAH; however, this also indicates that many patients with PAH are being initiated and maintained on monotherapy.
Across cohorts, approximately half (range 47.3–50.0%) of patients discontinued macitentan and tadalafil combination therapy over a similar observation period. When looking at the reasons for macitentan discontinuation (this information was not collected for tadalafil), the proportion of patients who discontinued due to an AE was similar across the cohorts (range 13.9–15.4%). The safety profile of macitentan and tadalafil observed in this analysis was consistent between cohorts and with the known safety profiles of the two drugs [24, 25]; however, the incidence rates (adjusted for exposure to combination therapy) of AEs and SAEs were slightly higher in the incident and incident initial cohorts, as were the rates of anemia/hemoglobin decrease (grouped terms). Decreased hemoglobin levels have previously been observed following treatment with macitentan and other ERAs, which then tend to stabilize over time [26,27,28]. As approximately 20% of prevalent patients had previously been treated with an ERA, they would be less likely to experience this effect. Together, these data indicate similar safety and tolerability of macitentan and tadalafil double combination therapy in both incident and prevalent patients, including as initial combination in patients naïve to PAH-targeted therapy.
Limitations of this analysis were that OPUS and OrPHeUS are drug registries with the aim of evaluating the safety of macitentan-treated patients, which may introduce a bias in the patient population and therefore results may not be directly comparable with disease registries. In both studies, many parameters were investigator-assessed and not adjudicated. There was a considerable amount of missing data for the hemodynamic and functional parameters, particularly in the prevalent cohort. Given the incomplete data for important prognostic factors, neither risk assessment calculation nor cohort balancing could be performed for key outcomes, and the descriptive nature of the comparisons precluded interpretation regarding effectiveness. The degree of missing data is not unexpected, given that OPUS and OrPHeUS were safety studies not designed to evaluate effectiveness and no assessments were mandated. This observation is not unique to this study: data from the REVEAL and COMPERA registries showed that the proportion of missing baseline values ranged from 6 to 9% for WHO FC, 20 to 29% for 6MWD, and 23 to 43% for BNP/NT-proBNP [29, 30]. Similarly, the PHAR and SPAHR registries reported missing data for the functional parameters required for risk assessment for approximately 50% and 20% of patients, respectively [4, 31]. It has been shown that, in the clinical setting, patients are more likely to have a full work-up at diagnosis and at some point after initiation of a new therapy, with follow-up at other points in a patient’s journey being far more variable [32, 33]. Combined, these analyses suggest that the frequency with which these assessments are performed in real-world clinical practice is suboptimal.
Conclusions
The OPUS and OrPHeUS combined analyses provide insight into the real-world use of macitentan and tadalafil combination therapy in patients with PAH, including incident and prevalent patients. Survival was similar between the cohorts, despite the incident patients having indicators of more severe PAH versus prevalent patients, which may be due to the significant use of initial combination therapy in newly-diagnosed patients. These data, however, demonstrate that a high hospitalization burden still exists in patients with PAH, and highlight the need to further optimize patient outcomes. The observed safety profile of macitentan and tadalafil was consistent with the known profiles for both drugs and tolerability was similar across cohorts. Together, these data support early combination therapy with macitentan and tadalafil.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Humbert M, Sitbon O, Yaïci A, Montani D, O’Callaghan DS, Jais X, et al. Survival in incident and prevalent cohorts of patients with pulmonary arterial hypertension. Eur Respir J. 2010;36:549–55. https://doi.org/10.1183/09031936.00057010.
Farber HW, Miller DP, Poms AD, Badesch DB, Frost AE, Muros-Le Rouzic E, et al. Five-Year outcomes of patients enrolled in the REVEAL Registry. Chest. 2015;148:1043–54. https://doi.org/10.1378/chest.15-0300.
Miller DP, Gomberg-Maitland M, Humbert M. Survivor bias and risk assessment. Eur Respir J. 2012;40:530–2. https://doi.org/10.1183/09031936.00094112.
Chang KY, Duval S, Badesch DB, Bull TM, Chakinala MM, de Marco T, et al. Mortality in pulmonary arterial hypertension in the modern era: early insights from the pulmonary hypertension association registry. J Am Heart Assoc. 2022;11: e024969. https://doi.org/10.1161/JAHA.121.024969.
Lajoie AC, Lauziere G, Lega JC, Lacasse Y, Martin S, Simard S, et al. Combination therapy versus monotherapy for pulmonary arterial hypertension: a meta-analysis. Lancet Respir Med. 2016;4:291–305. https://doi.org/10.1016/S2213-2600(16)00027-8.
Galiè N, Barberà JA, Frost AE, Ghofrani HA, Hoeper MM, McLaughlin VV, et al. Initial use of ambrisentan plus tadalafil in pulmonary arterial hypertension. N Engl J Med. 2015;373:834–44. https://doi.org/10.1056/NEJMoa1413687.
Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J. 2015;46:903–75. https://doi.org/10.1183/13993003.01032-2015.
Galiè N, Humbert M, Vachiéry JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37:67–119. https://doi.org/10.1093/eurheartj/ehv317.
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43:3618–731. https://doi.org/10.1093/eurheartj/ehac237.
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2023;61:2200879. https://doi.org/10.1183/13993003.00879-2022.
McLaughlin VV, Channick R, Kim NH, Frantz RP, McConnell J, Melendres-Groves L, et al. Safety of macitentan for the treatment of pulmonary hypertension: Real-world experience from the OPsumit® USers Registry (OPUS) and OPsumit® Historical USers cohort (OrPHeUS). Pulm Circ. 2022;12: e12150. https://doi.org/10.1002/pul2.12150.
Hoeper MM, Pausch C, Grünig E, Staehler G, Huscher D, Pittrow D, et al. Temporal trends in pulmonary arterial hypertension: results from the COMPERA registry. Eur Respir J. 2022;59:2102024. https://doi.org/10.1183/13993003.02024-2021.
International Society for Pharmacoepidemiology. Guidelines for good pharmacoepidemiology practices (GPP). Pharmacoepidemiol Drug Saf. 2008;17:200–8. https://doi.org/10.1002/pds.3891.
Opsumit® (macitentan). Prescribing Information. Actelion Pharmaceuticals US, Inc, a Janssen Pharmaceutical Company. March 2024.
Opsumit® (macitentan). Summary of Product Characteristics. Janssen Pharmaceuticals Ltd. March 2023.
Pocock SJ, Clayton TC, Altman DG. Survival plots of time-to-event outcomes in clinical trials: good practice and pitfalls. Lancet. 2002;359:1686–9. https://doi.org/10.1016/S0140-6736(02)08594-X.
Simonneau G, Channick RN, Delcroix M, Galiè N, Ghofrani A, Jansa P, et al. Incident and prevalent cohorts with pulmonary arterial hypertension: insight from SERAPHIN. Eur Respir J. 2015;46:1711–20. https://doi.org/10.1183/13993003.00364-2015.
Boucly A, Savale L, Jaïs X, Bauer F, Bergot E, Bertoletti L, et al. Association between initial treatment strategy and long-term survival in pulmonary arterial hypertension. Am J Resp Crit Care. 2021;204:842–54. https://doi.org/10.1164/rccm.202009-3698OC.
Muller A, Escribano-Subias P, Fernandes CC, Fontana M, Lange TJ, Söderberg S, Gaine S. Real-world management of patients with pulmonary arterial hypertension: insights from EXPOSURE. Adv Ther. 2024;41:1103–19. https://doi.org/10.1007/s12325-023-02730-8.
Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, et al. Survival in patients with idiopathic, familial, and anorexigen-associated pulmonary arterial hypertension in the modern management era. Circulation. 2010;122:156–63. https://doi.org/10.1161/CIRCULATIONAHA.109.911818.
Ogbomo A, Tsang Y, Mallampati R, Panjabi S. The direct and indirect health care costs associated with pulmonary arterial hypertension among commercially insured patients in the United States. J Manag Care Spec Pharm. 2022;28:608–16. https://doi.org/10.18553/jmcp.2022.28.6.608.
Tremblay É, Gosselin C, Mai V, Lajoie AC, Kilo R, Weatherald J, et al. Assessment of clinical worsening end points as a surrogate for mortality in pulmonary arterial hypertension: a systematic review and meta-analysis of randomized controlled trials. Circulation. 2022;146:597–612. https://doi.org/10.1161/CIRCULATIONAHA.121.058635.
Channick RN, Delcroix M, Ghofrani HA, Hunsche E, Jansa P, Le Brun FO, et al. Effect of macitentan on hospitalizations: results from the SERAPHIN trial. JACC Heart Fail. 2015;3:1–8. https://doi.org/10.1016/j.jchf.2014.07.013.
Sitbon O, Canuet M, Picard C, Prévot G, Bergot E, Cottin V, et al. Initial combination therapy with macitentan and tadalafil in newly diagnosed patients with pulmonary arterial hypertension: Results from the OPTIMA trial. Eur Respir J. 2020;56:2000673. https://doi.org/10.1183/13993003.00673-2020.
Grünig E, Jansa P, Fan F, Hauser JA, Pannaux M, Morganti A, et al. Randomized trial of macitentan/tadalafil single-tablet combination therapy for pulmonary arterial hypertension. J Am Coll Cardiol. 2024;83:473–84. https://doi.org/10.1016/j.jacc.2023.10.045.
Pulido T, Adzerikho I, Channick R, Delcroix M, Galiè N, Ghofrani A, et al. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N Engl J Med. 2013;369:809–18. https://doi.org/10.1056/NEJMoa1213917.
Wei A, Gu Z, Li J, Liu X, Han Y, Pu J. Clinical adverse effects of endothelin receptor antagonists: insights from the meta-analysis of 4894 patients from 24 randomized double-blind placebo-controlled clinical trials. J Am Heart Assoc. 2016. https://doi.org/10.1161/JAHA.116.003896.
Correale M, Ferraretti A, Monaco I, Grazioli D, Di Biase M, Brunetti ND. Endothelin-receptor antagonists in the management of pulmonary arterial hypertension: where do we stand? Vasc Health Risk Manag. 2018;14:253–64. https://doi.org/10.2147/VHRM.S133921.
Hoeper MM, Pausch C, Olsson KM. COMPERA 2.0: a refined four-stratum risk assessment model for pulmonary arterial hypertension. Eur Respir J. 2022;60:2102311. https://doi.org/10.1183/13993003.02311-2021.
Benza RL, Miller DP, Gomberg-Maitland M, Frantz RP, Foreman AJ, Coffey CS, et al. Predicting survival in pulmonary arterial hypertension: insights from the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL). Circulation. 2010;122:164–72. https://doi.org/10.1161/CIRCULATIONAHA.109.898122.
Kylhammar D, Kjellstrom B, Hjalmarsson C, Jansson K, Nisell M, Soderberg S, et al. A comprehensive risk stratification at early follow-up determines prognosis in pulmonary arterial hypertension. Eur Heart J. 2017;39:4175–81. https://doi.org/10.1093/eurheartj/ehx257.
Farber HW, Chakinala MM, Cho M, Frantz RP, Frick A, Lancaster L, et al. Characteristics of patients with pulmonary arterial hypertension from an innovative, comprehensive real-world patient data repository. Pulm Circ. 2023;13: e12258. https://doi.org/10.1002/pul2.12258.
Pugh ME, Hemnes AR, Trammell A, Newman JH, Robbins IM. Variability in hemodynamic evaluation of pulmonary hypertension at large referral centers. Pulm Circ. 2014;4:679–84. https://doi.org/10.1086/678514.
Acknowledgements
We thank the participants of these studies.
Medical Writing, Editorial, and Other Assistance
Medical writing assistance was provided by Emma Connolly and Kate Horne of eluSCIdate ltd (Meggen, Switzerland) and funded by Actelion Pharmaceuticals Ltd, a Johnson & Johnson Company. Graphical abstract support was provided by Clare Lowe and Shaun Hall of Ashfield MedComms, an Inizio Company (Macclesfield, UK), and funded by Actelion Pharmaceuticals Ltd, a Johnson & Johnson Company. Clinical evaluation of hepatic safety was performed by the Independent Liver Safety Data Review Board: Willis Maddrey MD (chairperson), Paul Watkins, MD, and James Freston, MD.
Funding
These studies, and the journal’s Rapid Service and Open Access fee were funded by Actelion Pharmaceuticals Ltd, a Johnson & Johnson Company.
Author information
Authors and Affiliations
Contributions
Kelly M Chin, Richard Channick, Nick H Kim and Vallerie V McLaughlin (members of the study Scientific Committee) contributed to the conception and design of the study in collaboration with the funders and were involved in the collection and interpretation of the data. Gwen MacDonald, Rose Ong, and Assunta Senatore were involved in the interpretation of the data. Nicolas Martin was involved in the statistical analyses and in the interpretation of the data. All authors were involved in development of the manuscript. Actelion Pharmaceuticals Ltd, a Johnson and Johnson Company, funded the study and participated in the design of the study, data analysis, interpretation, and preparation of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Kelly M Chin has served as a Scientific Committee member for Johnson & Johnson; has received research grants / support from Johnson & Johnson, Altavant, Acceleron, United Therapeutics, Pfizer, Merck, Gossamer Bio; has received support for travel to meetings from Johnson & Johnson; and has received consultancy fees from Johnson & Johnson, Altavant, Acceleron, United Therapeutics, Gossamer Bio and Merck. Richard Channick served as a Scientific Committee member for Johnson & Johnson; served on an advisory board for Johnson & Johnson and Bayer; received research grants / support from Johnson & Johnson and United therapeutics; received speaker fees from Johnson & Johnson, and Bayer; received consultancy fees from Johnson & Johnson, Bayer and Third pole. Nick H Kim has served a Scientific Committee member for Johnson & Johnson; has received research grants / support from Enzyvant and Lung Biotechnology; has received consultant fees from Johnson & Johnson, Bayer, Merck, United Therapeutics, Gossamer Bio, Pulnovo, and Polarean; and received speaker fees from Johnson & Johnson, Bayer and Merck. Rose Ong is an employee of Actelion Pharmaceuticals Ltd, a Johnson & Johnson Company, holds stock/stock options in Johnson & Johnson and spouse is an employee of Roche. Gwen MacDonald and Nicolas Martin are employees of Actelion Pharmaceuticals Ltd, a Johnson & Johnson Company and hold stock/stock options in Johnson & Johnson. Assunta Senatore is an employee of Actelion Pharmaceuticals Ltd, a Johnson & Johnson Company. Vallerie V McLaughlin served as a Scientific Committee member for Johnson & Johnson; received research grants from Aerovate, Altavant, Gossamer Bio, Johnson & Johnson, Merck, and SoniVie; and received consultant fees from Aerami, Aerovate, Altavant, Bayer, Caremark, Corvista, Gossamer Bio, Johnson & Johnson, L.L.C, Merck and United Therapeutics.
Ethical Approval
The OPUS and OrPHeUS studies were conducted according toGood Pharmacoepidemiology Practices and the 2008 Declaration of Helsinki ethical principles. Ethical approval was received from independent ethics committees/institutional review boards (IRB) of participating centers (Supplementary Appendix I). The protocols were reviewed by the US FDA with written informed consent obtained from all patients in OPUS, including for publication of anonymized patient data (informed consent was not required in OrPHeUS as an IRB waiver was obtained). The Informed Consent Form in OPUS included a confidentiality clause that all records and documents pertaining to the participation of patients in the OPUS registry would be held strictly confidential and their names would not be reported in any publications resulting from the OPUS registry. IRB approvals were provided by WIRB and Quorum (now Advarra) (OPUS registry; WIRB approval number 2014‐0816, Quorum Review File number 29120/Advarra Pro00035124) and WCG‐IRB (OrPHeUS study; IRB numbers 2017‐8051 and 2017‐2348).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chin, K.M., Channick, R., Kim, N.H. et al. Macitentan and Tadalafil Combination Therapy in Incident and Prevalent Pulmonary Arterial Hypertension: Real-World Evidence from the OPUS/OrPHeUS Studies. Adv Ther (2024). https://doi.org/10.1007/s12325-024-02964-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12325-024-02964-0