Abstract
Oxygen diffusion across the air-blood barrier in the lung is commensurate with metabolic needs and ideally allows full equilibration between alveolar and blood partial oxygen pressures. We estimated the alveolo-capillary O2 equilibration in 18 healthy subjects at sea level at rest and after exposure to increased O2 demand, including work at sea level and on hypobaric hypoxia exposure at 3840 m (PA ~ 50 mmHg). For each subject we estimated O2 diffusion capacity (DO2), pulmonary capillary blood volume (Vc) and cardiac output (\(\dot{Q}\)). We derived blood capillary transit time \({\boldsymbol{(}}{\boldsymbol{T}}{\boldsymbol{t}}{\boldsymbol{=}}\frac{{\boldsymbol{V}}{\boldsymbol{c}}}{\dot{{\boldsymbol{Q}}}}{\boldsymbol{)}}\) and the time constant of the equilibration process (\({\boldsymbol{\tau }}{\boldsymbol{=}}\frac{{\boldsymbol{\beta }}{\boldsymbol{V}}{\boldsymbol{c}}}{{\boldsymbol{D}}{{\boldsymbol{O}}}_{{\boldsymbol{2}}}}\), β being the slope of the hemoglobin dissociation curve). O2 equilibration at the arterial end of the pulmonary capillary was defined as \({{\bf{L}}}_{{\bf{e}}{\bf{q}}}{\boldsymbol{=}}{{\bf{e}}}^{{\boldsymbol{-}}\frac{{\bf{T}}t}{{\boldsymbol{\tau }}}}\). Leq greately differed among subjects in the most demanding O2 condition (work in hypoxia): lack of full equilibration was found to range from 5 to 42% of the alveolo-capillary PO2 gradient at the venous end. The present analysis proves to be sensible enough to highlight inter-individual differences in alveolo-capillary equilibration among healthy subjects.
Similar content being viewed by others
Introduction
The interaction between diffusion and perfusion in determining oxygen flow across the air-blood barrier is a fundamental factor sustaining metabolic oxygen need. Further, an efficient O2 diffusion-transport implies perfect equilibration for O2 partial pressure between the alveolar compartment and the blood flowing in the pulmonary capillary, that, in turn, allows to perfuse tissues with an optimal arterialization. The importance of this point becomes relevant when balanced against an increase in cells metabolic requirement, namely the increased oxygen demand, as in exercise, as well as in conditions causing a limitation to oxygen delivery (environmental hypoxia and cardio-pulmonary disorders). Recent work from our group revealed considerable inter-individual differences in the adaptive response of the air-blood barrier to work in normoxia and hypoxia1,2,3 and further the adaptations correlated with the morpho-functional phenotype of the air-blood barrier4.
Piiper and Scheid5 proposed an analysis to define the efficiency of the functional coupling for diffusion of oxygen with its blood transport capacity. This approach was strongly grounded on the principle of mass conservation whereby, under steady state conditions, the mass transfer of diffused O2 equals that received by the mixed venous blood affluent to the lung which, in turn, corresponds to the oxygen consumed by the tissues6. In this study we further developed the original model of Piiper and Scheid5 aiming at evaluating inter-individual differences in the efficiency of the lung O2 diffusion-perfusion mechanism among healthy subjects. To this aim, we defined the time constant of the O2 alveolo-capillary equilibration (τ), resulting from the complex interaction between the factors involved in the gas diffusion/transport function, namely: pulmonary capillary blood transit time (Tt), the overall lung diffusive capacity for O2 (DO2), cardiac output (\(\dot{Q}\)), and lung capillary blood volume (Vc). This approach led us to highlight remarkable differences among subjects in the O2 equilibration and to discuss the reasons for diffusion limitation.
Materials and Methods
The research project was approved by the ethical committee of University of Milano Bicocca and was conducted in accordance with the Helsinki Declaration for research on humans to assure ethical standards were met. Participants were instructed about the experimental procedure and related discomfort, as well as of the risks of acute exposure to hypoxia. All individual participants included in the study received and signed an informed written consent.
Participants
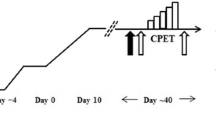
Data were obtained from 18 healthy participants (13 males, 5 females), average age 36.4 ± 8.2 (mean ± SD), and regularly practicing mountaineering and/or mountain hiking. All participants were no smokers or mild smokers (5 participants, smoking less than 4 cigarettes/day) and their spirometric parameters were above 90% of predicted values. Smokers were instructed to refrain from smoking 24 h before the test. All measurements were performed at sea level (SL, Monza Italy, 170 m, PIO2 157 mmHg) and at high altitude (HA, Aiguille du Midi, 3840 m, PIO2 90 mmHg), at rest and during work. Participants reached the laboratory at HA by cable car (about 30 minutes) and measurements were done after 4–6 hours from reaching the laboratory at HA. The four conditions considered in the study were defined as: SLrest, SLwork, HArest and HAwork.
Exercise protocol
Incremental test
At sea level (SL) an incremental exercise test was performed on a cycloergometer1 (Ergoline 900, Cosmed, Italy). After 2 min of unloading pedaling, the workload was increased every 60 s until voluntary exhaustion. The initial workload at SL was set at 60–90 W (according to an estimated level of physical fitness) and increments of 15–25 W/min were given, up to exhaustion. The gas exchange threshold (GET) was determined as the point where the slope of the \(\dot{V}{O}_{2}\) vs \(\dot{V}E\) relationship increased7 and the corresponding heart rate was determined.
Constant workload test
To ensure a correct measurement of lung diffusive capacity for carbon monoxide (DLCO) and its subcomponents during exercise (see below), all participants performed a steady-state test lasting no less than 18 minutes. For each subject, the test was performed at a workload of 70% (at SL) and 60% (at HA) of that corresponding to the GET determined at SL. This condition assured that the oxygen flow was constant and equal along the transport chain6.
For each participant, at rest and during exercise we determined with a portable metabolic cart (K4b2, Cosmed, Roma, Italy): pulmonary ventilation (\(\dot{V}E\), in BTPS), end tidal O2 and CO2 partial pressure (PetO2, PetCO2). Heart rate (HR) was continuously monitored and determined with a 12-lead electrocardiographic interfaced to the metabolic cart. Arterial blood O2 saturation (%SatO2) was monitored continuously through oximetry at the finger (RAD 9 Signal Extraction Pulse Oximeter: Masimo Corporation, Irvine - California, USA)1.
Diffusion measurement
We relied on the Roughton and Forster8 model, according to the equation:
where DLCO is the overall diffusion capacity of the lung, Dm and Vc are the diffusion subcomponent representing alveolar membrane diffusive capacity and lung capillary blood volume, respectively; θ is the binding rate of Hb with CO, (Hb) is the ratio between individual hemoglobin concentrations over reference values of hemoglobin concentration for men and women9.
Measurement of DLCO and subcomponents were performed according to standardized procedures9, in sitting position at total lung capacity (TLC) by single breath method (QUARK PFT, Cosmed, Roma, Italy), at SLrest and HArest and at a workload at GET (SLwork and HAwork). Participants inspired 3 gas mixtures containing 0.3% CH4 (tracer to measure alveolar lung volume, VA), 0.3% CO and 20, 40 and 60% O2, respectively. Each maneuver was performed at least 6 min after the previous one. For determination of DLCO during work, the subject stopped pedaling, on the average for less than 1 minute, at 6, 12 and 18 minutes to allow measurements to be done using 20, 40 and 60% O2, at the three time points, respectively.
DLCO values measured at HA were adjusted according to a recently developed method that accounts for the inter-individual differences of the effect of hypoxia exposure on diffusion subcomponents2, an approach allowing to maintain the validity of Eq. 1 on numerical basis. Blood samples were taken once to determine Hb concentration and haematocrit.
CO binding reflects individual Hb concentration, yet aiming to consider only the inter-individual differences in DLCO as reflecting the diffusive properties of the alveolar membrane, we standardized Hb concentration to reference values of 14.6 g/dl in men and 13.4 g/dl in women9. We relied on θ values from Forster10 according to the relationship 1/θ = 0.75 + (0.0057 · PA), where PA is alveolar O2 partial pressure assumed equal to the measured end tidal O2 pressure.
We derived the DO2 values from measured DLCO multiplied by the constant 1.2311; this procedure was validated by measurement based on mass spectrometry using oxygen isotopes11, as well as with those calculated by Hammond and Hempleman12 and Hempleman and Gray13 based on MIGET (Multiple Inert Gas Elimination Technique).
Echocardiography and cardiac output
As in previous study from our group3, standard 2D echocardiography was performed at rest in supine position using a portable echo machine with a 2.5–3.5 MHz cardiac probe (Vivid I, General Electric Healthcare Clinical System) by a single experienced cardiologist, both at SL and HA. Care was taken to ensure that the position of the participants and the transducer were similar in all examinations. Stroke volume was obtained from apical 4 chamber view. Cardiac output (\(\dot{Q}\)) was measured multiplying Left Ventricle outflow tract time-velocity integral, measured using pulse wave Doppler, by its cross-sectional area and heart rate14. To derive \(\dot{Q}\) during exercise we assumed an increase in stroke volume of 40%, as from data provided by Poliner15 and Stöhr16.
Estimate of O2 equilibration
We define the limitation of O2 equilibration at the exit of pulmonary capillary as Leq (see Appendix):
where DO2 is the oxygen diffusive capacity, \(\dot{Q}\) is the cardiac output and β is the hemoglobin binding capacity for oxygen, expressing the mean slope of the Hb-O2 dissociation curve (see Appendix).
Knowing blood transit time in the pulmonary capillaries (Tt) and the time constant of the equilibration process (τ), one can express diffusion limitation also as:
that allows to draw the exponential profile of the alveolo-capillary O2 equilibration as a function of time.
Results
Correlation between diffusive and perfusive variables involved in O2 equilibration
Table 1 reports means (±SD) and median (IQR 25–75) values of %SatO2 and PA in the four conditions studied.
No significant differences were found for hemoglobin concentration (14 ± 0.5 g/dl) and haematocrit (42 ± 0.9) at SL and HA, suggesting similar hydration conditions.
Figure 1a shows the overall relationship between DO2 and cardiac output in the four conditions considered as indicated. Figure 1b shows the changes in DO2 and \(\dot{Q}\) relative to SLrest that allows to appreciate that the relative increase in \(\dot{Q}\) is greater than that of DO2. Figure 1c shows the distribution of Tt vs \(\dot{Q}\) in the four conditions; the figure also reports the calculated iso-Vc lines as indicated. The light grey area, encompassing the open points referring to resting condition, suggests that exposure to HA leads to a decrease in Tt essentially related to a decrease in Vc. Conversely, the dark grey area referring to working conditions both at SL and HA suggests that the decrease in Tt mostly relates to the increase in \(\dot{Q}\).
Correlation between diffusive and perfusive variables involved in O2 equilibration. (a) Correlation between O2 diffusive capacity (DO2) and cardiac output (\(\dot{Q}\)) for all subjects at SLrest (open circles), SLwork (closed circles), HArest (open squares) and HAwork (closed squares). (b) Correlation between DO2 and \(\dot{Q}\), normalized to values at sea level rest (SLrest). (c) Correlation between Tt and \(\dot{Q}\): figure also reports three calculated Iso-Vc dotted lines as labelled. Light grey and dark grey areas encompass rest and work data respectively.
Time-dependence of alveolo-capillary equilibration
In Fig. 2a we plotted for one subject the time course of the equilibration process to reach the final Leq value attained at the exit of the pulmonary capillary in the four conditions (as indicated by symbols): the rightward displacement of the curves reflects the progressive increase in τ shifting from SLrest to SLwork, HArest and HAwork. The final value of Leq clearly results from the matching of τ and Tt. Figure 2b shows the wide spectrum of the increase in Leq when plotted vs the increase in τ. A stronger correlation was found between Leq and Tt (Fig. 2c).
Time-dependence of alveolo-capillary equilibration. (a) Profile of alveolo-capillary (A–c) equilibration as a function of time along the pulmonary capillary for one subject at SLrest (open circles), SLwork (closed circles), HArest (open squares) and HAwork (closed squares); see Appendix for the definition of 1-Leq. (b) Plot of Leq vs time constant (τ) for all subjects at SLrest, SLwork, HArest and HAwork. (c) Correlation between Leq vs transit time (Tt) in all conditions.
Dependence of Leq from O2 diffusion and transport
Considering the β values for the four conditions, we calculated from Eq. 3 the Leq values that were plotted in Fig. 3 vs DO2/β\(\dot{Q}\) (that is equal to Tt/τ according to equation A.6). Clearly, the relationship shows that a remarkable increase in Leq occurs shifting from SL to HA when the value of abscissa drops below 3–4 (vertical dashed line).
Dependence of Leq from O2 diffusion and transport. Relationship between diffusion equilibration (Leq) and DO2/β\(\dot{Q}\) (that is equal to Tt/τ) at SLrest (open circles), SLwork (closed circles), HArest (open squares) and HAwork (closed squares). The vertical dashed line for DO2/β\(\dot{Q}\) = 4 is a cutoff value below which a remarkable increase in Leq occurs.
Figure 4 shows that the cardiac output increases with increasing Leq. Note that data referring to HA lay on a relationship that is displaced to the right.
Discussion
In general, O2 equilibration is considered to reflect the heterogeneity of regional distribution of \({\dot{V}}_{A}/\dot{Q}\) ratio17,18,19 as well as regional distribution of the diffusion/perfusion ratio20, both remaining difficult to be assessed. The model of alveolo-capillary equilibration that we considered circumvents this complication, and is open to different functional readings. An invasive approach, requiring an arterial and venous blood draw, would allow to define the ratio \(\frac{{P}_{A}-{P}_{a}}{{P}_{A}-{P}_{\bar{v}}}\) (equation A.2). Conversely, a non-invasive approach would allow to estimate DO2/β\(\dot{Q}\) that highlights the ratio between O2 diffusion capacity to O2 transport capacity; further, this approach allows to provide a time-based interpretation of the alveolo-capillary equilibration process based on τ and Tt.
As from Table 1, the average values of %SatO2 and PA are in line for a group of healthy subjects and do not show remarkable variability. Yet, the individual values of Leq varied subtantially reaching a value of 0.42 in the most demanding oxygen condition. This reveals considerable inter-individual differences concerning the efficiency of the O2 diffusion-transport system, that can be detected by the present approach.
The equilibrium reached at the exit of the pulmonary capillary results from a complex interaction of the functional parameters involved in the adaptive response to match O2 uptake with metabolic needs. The increase in DO2 favors the increase in O2 uptake and furthermore the increase in cardiac output favors oxygen delivery to the periphery (Fig. 1a): yet, in general, cardiac output (\(\dot{Q}\)) increased more than DO2 (Fig. 1b), so that the ratio DO2/\(\dot{Q}\) inevitably decreased. Figure 1c allows to focus on some functional relationship between the three key parameters analyzed, namely Tt, \(\,\dot{Q}\) and Vc when facing an increase in metabolic O2 requirement. The suggestion is that, on exposure to HA at rest (light grey area), the factor mostly affecting the lack of equilibration is the decrease in Tt due to a decrease in Vc, reflecting in turn pulmonary vasoconstriction3. Considering a cutoff of Vc = 200 ml, one can note that during work at SL (Fig. 1c, closed circles) 72% of the subjects had a Vc > 200 ml, while at SLrest (Fig. 1c, open circles) they amounted only to 22%: accordingly, SLwork led, on the average, to an increase in Vc. Despite some inter-individual variability, the increase in Vc appears useful to limit a decrease in Tt (levelling, on the average, to ~0.75 sec) due to the remarkable increase in \(\dot{Q}\). Considering now HAwork (closed squares), it appears that Tt and corresponding Vc remain in the lower range of measured values.
It is noteworthy in this respect that pulmonary capillary vasomotion in hypoxia, as deduced from changes in Vc, was found to be variable among individuals3, being interpreted as vasoconstriction or vasodilation. Recent data on in vivo imaging of alveolar units in an animal experimental model of hypoxia exposure clearly indicate heterogeneous alveolar blood flow distribution, with a more pronounced vasoactive response in larger alveolar units showing signs of interstitial edema21. Vasoconstriction may in fact be regarded as the main mechanism aimed at preventing the aggravation of developing edema, an interpretation pivoting around the perturbation induced by hypoxia on the capillary interstitial fluid dynamics in the lung22,23.
The role of Tt has been considered either as a non limiting24 or a potentially limiting25,26 factor to blood oxygenation. As Fig. 2a suggests, the alveolo-capillary O2 equilibration depends from the relative changes of both τ and Tt. Figure 2b shows a great dispersion by plotting the increase in Leq with increase in τ, reflecting the variability of the individual ratio Vc/DO2 (equation A.5). Yet, a more significant correlation was found by plotting Leq vs Tt (Fig. 2c). The increase in Leq obviously reflects the decrease of the DO2/\(\dot{Q}\) and of Tt/τ ratio (Fig. 3): this figure, although representing a “truism”, wishes to emphasize the remarkable increase in Leq when Tt/τ drops below ~4 (dashed vertical line).
It is noteworthy that, both at SL and HA, the highest cardiac output increased with increasing individual Leq (Fig. 4) revealing the need for a greater O2 transport to the tissues in face of increasing lack of O2 equilibration. Further, it is noteworthy that such response is highly variable among individuals. Bradycardia at SLrest favors O2 equilibration on increasing oxygen metabolic need to buffer the decrease in Tt/τ.
Comparison with Previous Models of Oxygen Uptake and Transport
The quantitative interaction between diffusive and convective factors along the oxygen transfer pathway led to the development of functional models aiming to identify factors causing a potential limitation to the maximum oxygen consumption (\(\dot{V}{O}_{2max}\)). The present analysis is not primarily considering the point of \(\dot{V}{O}_{2max}\), that includes the oxygen transport from the lungs to the mitochondria; it only considers the diffusive/convective function at alveolar level in subthreshold exercises. It appears therefore reasonable to compare the present results with predictions from two relevant models of oxygen transport, referred here as Wagner’s and di Prampero’s models, as reviewed by Ferretti27. Wagner’s model28 described oxygen transport by derivation of Roughton and Forster8 equation (Eq. 1) to express O2 uptake as a function of membrane diffusion for O2 and capillary blood volume Vc, ignoring the alveolar-capillary coupled diffusion/transport for O2. Just considering this last point, we are able to estimate inter-individual differences of transit time (Tt) and time constant (τ) of the alveolo-capillary O2 equilibration. Our data, compared to predictions from Wagner’s model, indicate transit times about 3 times longer and equilibration kinetics remarkably slowed down. To specifically deal with hypoxia, Wagner’s model evolved further29 by setting a 3-equations algebraic system to include the role of ventilation, of the alveolar diffusive/transport5 and of O2 diffusion at the periphery. The model goes on to speculate on maximum exercise at top of Mount Everest, 8848 m. Data fed into the algebraic system were: lung ventilation of 150 L · min−1, DO2 of 160 ml · min−1 · Torr−1 and cardiac output \(\dot{Q}\) of 18 L · min−1. A comment concerning these assumptions is due. The limit to the increase in maximum ventilation beyond which any increase in ventilation does not result in O2 available for useful external work, was set, based on respiratory mechanics studies30 and energy cost as well as efficiency of breathing31 at about 120 L · min−1. Furthermore, actual measurements done at high altitude confirmed that the energy cost of extra ventilation outstripped the interest for increasing oxygen transfer32. The assumption of DO2 = 160 ml · min−1 · Torr−1 appears exceedingly high and moreover, the decrease in cardiac output at Everest summit was assumed at 23% relative to sea level value of 25 L · min−1, rather than an expected 40%33. Based on the assumptions29, one could estimate Leq ~0.5 at summit of Everest, a rather low value being essentially equal to that corresponding to sub-threshold workload at ~4000 m (Fig. 4, HA), a much lower altitude. Nevertheless, there is agreement with Wagner’s model that in normoxia a limitation of the alveolo/capillary function is essentially low, while in severe hypoxia, the diffusion limitation may account for 80% of the alveolar-capillary PO2 difference19. Di Prampero’s model34,35, based on an electrical analogue, considers O2 flow to occur down a system of resistances placed in series. The finding of low Leq values in normoxia confirms the conclusion from di Prampero’s model that ventilation has a minimal role to limit \(\dot{V}{O}_{2max}\), due to the flatness of the Hb-O2 relationship at normoxic PO235. Di Prampero and Ferretti35 introduced the concept of non-linear behaviour of the respiratory system in hypoxia (PIO2 ~ 90 Torr) when shifting to the vertical part of the Hb-O2 dissociation curve35. Our model implies mathematically the non linearity of O2 transport at the alveolar-capillary level when shifting from normoxia to hypoxia, as shown by the exponential increase in Leq (see Fig. 3): this occurs because the increase in O2 diffusion, due to the greater binding capacity of the blood, is less than the increase in cardiac output. As shown in Fig. 4, this discrepancy becomes larger with increasing the metabolic requirement. Finally, our conclusions agree with those from Di Prampero and Ferretti35 that in hypoxia the limitation imposed by diffusion exceeds that of the cardiovascular transport.
Limitations of the Study
-
The same β values were used for all subjects according to the condition considered. At SL inter-individual differences in slope (tangent of the function) may well exist, although they must remain on mathematical ground within narrow limits due to the low slope of the Hb-dissociation curve; at HA below PO2 of 55 mmHg the slope of Hb-dissociation curve is obviously higher than at SL but fairly constant.
-
The estimate of cardiac output in exercise, relative to supine, based on a fixed 40% increase for stroke volume multiplied by heart rate introduces a noise into the analysis, whose degree cannot be quantitated.
-
The present analysis allows to quantitate the inter-individual differences in alveolo-capillary oxygen equilibration but is unable to quantitate the relative contribution of the factors leading to such differences, namely: the heterogeneity in ventilation/perfusion ratio, the shunt effect as well as the actual values of Pa and \({P}_{\bar{v}}\).
Data availability
Authors declare no restrictions on the availability of materials or information at the time of submission from the corresponding author on reasonable request.
References
Bartesaghi, M. et al. Inter-individual differences in control of alveolar capillary blood volume in exercise and hypoxia. Respir Physiol Neurobiol. 190, 96–104, https://doi.org/10.1016/j.resp.2013.08.021 (2014).
Beretta, E. et al. Reappraisal of DLCO adjustment to interpret the adaptive response of the air blood barrier to hypoxia. Respir. Physiol. Neurobiol. 238, 59–65 (2017).
Beretta, E. et al. Air blood barrier phenotype correlates with alveolo-capillary O2 equilibration in hypobaric hypoxia. Respir. Physiol. Neurobiol. 246, 53–58 (2017).
Miserocchi, G. et al. Mechanisms behind inter-individual differences in lung diffusing capacity. Eur. J. Appl. Physiol. 102, 561–8, https://doi.org/10.1007/s00421-007-0625-2 (2008).
Piiper, J. & Scheid, P. Model for capillary-alveolar equilibration with special reference to O2 uptake in hypoxia. Respir. Physiol. 46, 193–208 (1981).
Ferretti, G., Fagoni, N., Taboni, A., Bruseghini, P. & Vinetti, G. The physiology of submaximal exercise: the steady state concept. Respir. Physiol. Neurobiol. 246, 76–85, https://doi.org/10.1016/j.resp.2017.08.005 (2017).
Beaver, W. L., Wasserman, K. & Whipp, B. J. Computer analysis and breath-by-breath graphical display of exercise function tests. J. Appl. Physiol. 34, 128–132 (1973).
Roughton, F. & Forster, R. E. Relative importance of diffusion and chemical reaction rates in determining rate of exchange of gases in the human lung with special reference to true diffusing capacity of pulmonary membrane and volume of blood in the lung capillaries. J. Appl. Physiol. 11, 290–302 (1957).
MacIntyre, N. et al. Standardization of the single breath determination of carbon monoxide uptake. Eur. Respir. J. 26, 720–735 (2005).
Forster, R. E. Diffusion of gases across the alveolar membrane. In Handbook of Physiology (eds Fishman, A. P., Fahri, L. E., Tenney, S. M. & Geiger, S. R.) 71–88 (Washington DC: American Physiological Society, 1987).
Meyer, M., Scheid, P., Riepl, G., Wagner, H. J. & Piiper, J. Pulmonary diffusion capacities for O2 and CO measured by a rebreathing technique. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 51, 1643–50 (1981).
Hammond, M. D. & Hempleman, S. C. Oxygen diffusing capacity estimates derived from measured VA/Q distributions in man. Respir. Physiol. 69, 129–47 (1987).
Hempleman, S. C. & Gray, A. T. Estimating steady-state DLO2 with nonlinear dissociation curves and VA/Q inequality. Respir. Physiol. 73, 279–88 (1988).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 16, 233–270 (2015).
Poliner, L. R. et al. Left ventricular performance in normal subjects: a comparison of the responses to exercise in the upright and supine positions. Circulation 62, 528–34 (1980).
Stöhr, E. J., González-Alonso, J. & Shave, R. Left ventricular mechanical limitations to stroke volume in healthy humans during incremental exercise. Am. J. Physiol. Heart Circ. Physiol. 301, H478–87 (2011).
Hammond, M. D., Gale, G. E., Kapitan, K. S., Ries, A. & Wagner, P. D. Pulmonary gas exchange in humans during exercise at sea level. J. Appl. Physiol. 60, 1590–98 (1986).
Hammond, M. D., Gale, G. E., Kapitan, K. S., Ries, A. & Wagner, P. D. Pulmonary gas exchange in humans during normobaric hypoxic exercise. J. Appl. Physiol. 61, 1749–57 (1986).
Wagner, P. D. et al. Operation Everest II: pulmonary gas exchange during a simulated ascent of Mt. Everest. J. Appl. Physiol. 63, 2348–59 (1987).
Piiper, J. & Scheid, P. Diffusion limitation of O2 supply to tissue in homogeneous and heterogeneous models. Respir. Physiol. 85, 127–36 (1991).
Mazzuca, E., Aliverti, A. & Miserocchi, G. Understanding Vasomotion of Lung Microcirculation by In Vivo Imaging. J. Imaging. 5, 22, https://doi.org/10.3390/jimaging5020022 (2019).
Miserocchi, G. Mechanisms controlling the volume of pleural fluid and extravascular lung water. Eur. Respir. Rev. 18, 244–52, https://doi.org/10.1183/09059180.00002709 (2009).
Mazzuca, E., Aliverti, A. & Miserocchi, G. Computational micro-scale model of control of extravascular water and capillary perfusion in the air blood barrier. J. Theor. Biol. 400, 42–51, https://doi.org/10.1016/j.jtbi.2016.03.036 (2016).
Ayappa, I. et al. Effect of blood flow on capillary transit time and oxygenation in excised rabbit lung. Respir. Physiol. 105, 203–16 (1996).
Hughes, J.M.B. Diffusive gas exchange in Lung Biology. In Health and Disease Volume 52: Exercise, Pulmonary physiology and pathophysiology (eds Whipp, J. & Wasserman, K.) 143–171 (Dekker, 1991).
Pande, J. N. & Hughes, J. M. Regional pulmonary clearance of inhaled C15O and C15O2 in man at rest and during exercise. Clin. Physiol. 3, 491–501 (1983).
Ferretti, G. Maximal oxygen consumption in healthy humans: theories and facts. Eur. J Appl. Physiol. 114, 2007–36, https://doi.org/10.1007/s00421-014-2911-0 (2014).
Wagner, P. D. & West, J. B. Effects of diffusion impairment on O2 and CO2 time courses in pulmonary capillaries. J. Appl. Physiol. 33, 62–71 (1972).
Wagner., P. D. Algebraic analysis of the determinants of VO2max. Respir. Physiol. 93, 221–37 (1993).
Margaria, R., Milic-Emili, G., Petit, J. M. & Cavagna, G. Mechanical work of breathing during muscular exercise. J. Appl. Physiol. 15, 354–58 (1960).
Milic-Emili, G. & Petit, J. M. Mechanical efficiency of breathing. J. Appl. Physiol. 15, 359–62 (1960).
Cibella, F. et al. Respiratory energetics during exercise at high altitude. J. Appl. Physiol. 86, 1785–92 (1999).
Mourot, L. Limitation of Maximal Heart Rate in Hypoxia: Mechanisms and Clinical Importance. Front. Physiol. 9, 972, https://doi.org/10.3389/fphys.2018.00972 (2018).
di Prampero, P. E. & Ferretti, G. Factors limiting maximal oxygen consumption in humans. Respir. Physiol. 80, 113–128 (1990).
Ferretti, G. & di Prampero, P. E. Factors limiting maximal O2 consumption: effects of acute changes in ventilation. Respir. Physiol. 99, 259–271 (1995).
Dash, R. K., Korman, B. & Bassingthwaighte, J. B. Simple accurate mathematical models of blood HbO2 and HbCO2 dissociation curves at varied physiological conditions: evaluation and comparison with other models. Eur. J. Appl. Physiol. 116, 97–113 (2016).
Acknowledgements
We acknowledge the organizational and logistical support of the Foundation “Montagna Sicura” − Courmayeur in the person of Dr. Micole Trucco. Financial support by project Alcotra No. 114 Resamont 2. Facilities and equipment provided by the University of Milano Bicocca, Sports Medicine School.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the study. G.M. conceived and designed research, contribute to write the manuscript. E.B. designed research, analyzed data, contribute to write the manuscript. G.S.G., G.F. and G.S. analyzed data, contribute to write the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
The oxygen alveolo-capillary equilibration at the exit of the pulmonaty capillary has been described as5:
where, PA, Pa and \({P}_{\bar{v}}\) are the partial pressures of O2 in the alveoli, in the arterial blood leaving the lung and in the mixed venous blood, respectively; DO2 is the oxygen diffusive capacity, \(\dot{Q}\) is the cardiac output and β is the hemoglobin binding capacity for oxygen, expressing the mean slope of the Hb-O2 dissociation curve. This approach is grounded on the equality between O2 diffusion and O2 transport under steady state condition.
The conceptual development of Eq. (2) reported in Methods allows to define the potential limitation of the O2 equilibration at the exit of pulmonary capillary as:
Leq can vary from 0 (the case of perfect equilibration) to 1 (the case of shunt).
Knowing Vc and \(\dot{Q}\), one can derive the average pulmonary blood capillary transit time (Tt) as:
One can therefore reformulate Eq. (2) reported in the Methods as:
So that one can explicit the time constant τ of the exponential equilibration process as:
Knowing Tt and τ, one can re- define Leq at the exit from the pulmonary capillary as:
Knowing the transit time Tt, allows us to describe the O2 equilibration process as a function of time. Revising Eq. (A.4), one has:
for time (t), being a fraction of known transit time (Tt).
For the sake of graphical representation of the alveolo-capillary gradient (see Fig. 2a), we put on the ordinate alveolo-capillary (A-c) equilibration as 1-Leq, meaning that in case of perfect equilibration one has A-c equilibration equal to 1, for Leq = 0.
Estimate of β. We relied on analytical treatment of the hemoglobin dissociation curve36. Average slopes of the curve were estimated considering PCO2 values at SL and HA. For the range of PO2 considered, we derived β values for SLrest, SLwork, HArest and HAwork as follows: 0.83, 1.72, 2.5 and 3.25 ml · L−1 · mmHg−1, respectively.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Beretta, E., Grasso, G.S., Forcaia, G. et al. Differences in alveolo-capillary equilibration in healthy subjects on facing O2 demand. Sci Rep 9, 16693 (2019). https://doi.org/10.1038/s41598-019-52679-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-52679-4
- Springer Nature Limited
This article is cited by
-
A century of exercise physiology: lung fluid balance during and following exercise
European Journal of Applied Physiology (2023)