Abstract
Background
Although elevated heart rate is a risk factor for cardiovascular morbidity and mortality in healthy people, the association between resting heart rate and major cardiovascular risk in patients after acute ischemic stroke remains debated. This study evaluated the association between heart rate and major adverse cardiovascular events after ischemic stroke.
Methods
We conducted a retrospective cohort study analyzing data from the Chang Gung Research Database for 21,655 patients with recent ischemic stroke enrolled between January 1, 2010, and September 30, 2018. Initial in-hospital heart rates were averaged and categorized into 10–beats per minute (bpm) increments. The primary outcome was the composite of hospitalization for recurrent ischemic stroke, myocardial infarction, or all-cause mortality. Secondary outcomes were hospitalization for recurrent ischemic stroke, myocardial infarction, and heart failure. Hazard ratios and 95% confidence intervals (CIs) were estimated using Cox proportional hazards models, using the heart rate < 60 bpm subgroup as the reference.
Results
After a median follow-up of 3.2 years, the adjusted hazard ratios for the primary outcome were 1.13 (95% CI: 1.01 to 1.26) for heart rate 60–69 bpm, 1.35 (95% CI: 1.22 to 1.50) for heart rate 70–79 bpm, 1.64 (95% CI: 1.47 to 1.83) for heart rate 80–89 bpm, and 2.08 (95% CI: 1.85 to 2.34) for heart rate ≥ 90 bpm compared with the reference group. Heart rate ≥ 70 bpm was associated with increased risk of all secondary outcomes compared with the reference group except heart failure.
Conclusions
Heart rate is a simple measurement with important prognostic implications. In patients with ischemic stroke, initial in-hospital heart rate was associated with major adverse cardiovascular events.
Similar content being viewed by others
Background
Elevated heart rate is associated with a prothrombotic state [1], increased myocardial oxygen demand [2], plaque rupture [3], increased shear stress on the endothelium [4], and atherosclerosis [5], which provides possible pathophysiological mechanisms for the development of cardiovascular diseases. Accumulative evidence from a meta-analysis of prospective cohort studies showed that an increase in heart rate by 10 beats per minute (bpm) was associated with a 17% higher risk of all-cause mortality and a 14% risk of clinical cardiovascular disease in the general population [6].
However, the association between resting heart rate and cardiovascular risk after ischemic stroke remains controversial. In a study employing the Virtual International Stroke Trials Archive Database, elevated heart rate (> 86 bpm) was linked to mortality, heart failure (HF), and a higher degree of dependence but not to recurrent stroke, transient ischemic attack, or myocardial infarction (MI) within 90 days of stroke onset in patients with ischemic stroke [7]. In the PRoFESS trial, recurrent stroke and MI were not significantly associated with baseline heart rate in patients with noncardioembolic ischemic stroke [8]. In the PERFORM study, for patients with recent noncardioembolic ischemic stroke, heart rate ≥ 70 bpm was associated with increased relative risk of MI, ischemic stroke, and a composite of ischemic stroke, MI, or other vascular death [9].
These inconsistent results have left clinicians uncertain about the relationship between resting heart rate and major cardiovascular prognosis after ischemic stroke. Compared with other cardiovascular diseases, ischemic stroke shows a variety of pathogenic mechanisms not present in other cardiovascular diseases [10]. The aim of this study was to investigate the association between heart rate and a variety of cardiovascular outcomes in a large cohort of patients with various subtypes of ischemic stroke, which may provide further evidence when considering secondary prevention strategies for patients with ischemic stroke.
We hypothesized that elevated initial in-hospital heart rate is associated with increased risk of major cardiovascular outcomes after ischemic stroke.
Methods
Study design and population
We conducted this retrospective cohort study by using data from the Chang Gung Research Database, the largest multi-institutional electronic medical records collection in Taiwan [11].
Inclusion and exclusion criteria
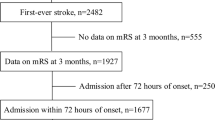
Patients whose first two discharge diagnoses included the International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM] code 433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, or 434.91 or International Classification of Diseases, 10th Revision, Clinical Modification [ICD-10-CM] code I63 [12, 13] and who were accrued consecutively between January 1, 2010, and September 30, 2018, were included. The exclusion criteria were patients: 1) hospitalized for less than 3 days; 2) admitted to a rehabilitation unit; 3) admitted through outpatient clinics; 4) with recurrent stroke during the study period; and 5) with less than one record of heart rate per day in the first three days of hospitalization. In addition, those without catastrophic illness cards were also excluded (beneficiaries of the National Health Insurance system in Taiwan would have been given a catastrophic illness card for 1 month because of their acute ischemic stroke). The first-ever ischemic stroke during the study period was defined as the index stroke. The patient selection process is illustrated in Fig. 1.
Data collection
Key demographic and clinical characteristics were collected. Estimated glomerular filtration rate was determined using the Modification of Diet in Renal Disease equation [14]. To minimize bias, the mean heart rate, systolic blood pressure, and diastolic blood pressure in the first 3 days of hospitalization was used instead of a single measurement value for further analysis. The claims-based stroke severity index (SSI) was used to assess stroke severity. SSI scores were transformed into estimated National Institutes of Health Stroke Scale (eNIHSS) scores by using the equation 1.1722 × SSI − 0.7533 [15].
Outcome
Clinical data extracted from the Chang Gung Research Database were linked to the National Health Insurance Research Database and National Registry of Deaths provided by the Ministry of Health and Welfare in Taiwan for the period January 1, 2010, to December 31, 2018. The National Health Insurance system in Taiwan covers more than 99.9% of the entire population [16]. Therefore, hospitalization records for ischemic stroke, MI, and HF were reliable in this study.
The primary outcome of the study was the time to earliest major adverse cardiovascular event (MACE), which included hospitalization for recurrent ischemic stroke, MI, or all-cause mortality after index stroke. The secondary outcomes were hospitalization for recurrent ischemic stroke, MI, and HF after index stroke. The diagnosis of hospitalization for ischemic stroke (ICD-9-CM codes 433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, and 434.91; ICD-10-CM code I63) [12, 13], MI (ICD-9-CM code 410; ICD-10-CM codes I21 and 22) [17, 18], and HF (ICD-9-CM code 428; ICD-10-CM code I50) [19] was determined from the first two discharge diagnoses.
Statistical analysis
Descriptive statistics are presented as number (percentage) for categorical data and mean (standard deviation) and median (interquartile range) for continuous data. The patients were stratified into five subgroups in accordance with their mean heart rate level: < 60, 60 to 69, 70 to 79, 80 to 89, or ≥ 90 bpm. Differences between the groups were tested using the Kruskal–Wallis rank test for continuous data and the chi-square test for categorical data. Cox proportional hazards models were used to evaluate the relationship between heart rate and cardiovascular outcomes. Analyses were performed using mean heart rate as both a continuous and categorical variable. Because a heart rate ≥ 60 bpm has been shown to be associated with an increased risk of all-cause mortality and cardiovascular death in patients with ischemic stroke or coronary artery disease (CAD) [20, 21], patients with a heart rate < 60 bpm were selected as the reference group in this analysis. In addition to crude hazard ratios (HRs), adjusted HRs and 95% confidence intervals (CIs) were calculated with the reference group and estimated after adjusting for potential confounding factors in the Cox proportional hazards models. Model 1 included age and sex, whereas Model 2 included age; sex; eNIHSS score; history of hypertension, diabetes mellitus, dyslipidemia, atrial fibrillation, CAD, HF, and cancer before admission; smoking status; body mass index; total cholesterol level; triglyceride level; chronic kidney disease stage; alanine aminotransferase level; glycated hemoglobin level; mean systolic blood pressure; mean diastolic blood pressure; and use of antithrombotics, statins, and beta-blockers. Unless specified, all results are given for Model 2. Data were analyzed as recorded without any imputation for missing data. For adjustment variables for which a large amount of data was missing, a category for missing data was included to minimize the effect of missing data on the analysis.
The restricted cubic spline smoothing technique was employed to explore the overall trend of associations through the range of heart rate values. Subgroup analyses for the primary outcome were performed with mean heart rate used as a continuous variable. HRs and 95% CIs for each subgroup were calculated for every increment of 1 standard deviation in mean heart rate. All analyses were performed with SAS (version 9.4, Cary, NC, USA) and R software version 4.2.0 (R Foundation for Statistical Computing, Vienna, Austria). This study is reported according to STROBE guidelines [22].
Results
Baseline characteristics
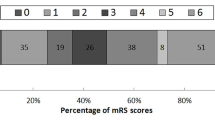
A total of 21,655 adult patients with recent ischemic stroke were included in the analysis (mean age, 67.35 ± 12.93 years; 61.88% men). The mean systolic blood pressure and diastolic blood pressure were 151.04 ± 19.64 and 84.81 ± 11.17 mm Hg, respectively, and the mean heart rate was 74.84 ± 11.27 bpm. The demographics and baseline clinical characteristics of the overall patient cohort and for the subgroups defined by 10-bpm increments in heart rate are given in Table 1. In total, 436,376 measurements of heart rate were collected. The median number of measurements per patient was 13 (interquartile range: 9–18). After a median follow-up of 3.2 years (interquartile range: 1.4–5.6 years), 7762 patients (35.8%) experienced a MACE, the primary outcome. Hospitalization for recurrent ischemic stroke, MI, and HF occurred in 3913 (18.1%), 625 (2.9%), and 1149 (5.3%) patients, respectively. Compared with the patients with a high mean heart rate, those with a low mean heart rate were more likely to be male, currently smoke, use a statin or antithrombotic agent, not use a beta-blocker, and have dyslipidemia, mild stroke severity, and a lower baseline level of alanine aminotransferase; in addition, the baseline incidences of atrial fibrillation and HF were lower in these patients (Table 1).
Associations between heart rate and outcomes
The crude and adjusted HRs for the mean heart rate subgroups are illustrated in Fig. 2. Compared with the reference group (mean heart rate < 60 bpm), the adjusted HRs for a MACE in Model 2 were 1.13 (95% CI: 1.01 to 1.26) for a mean heart rate of 60 to 69 bpm, 1.35 (95% CI: 1.22 to 1.50) for a mean heart rate of 70 to 79 bpm, 1.64 (95% CI: 1.47 to 1.83) for a mean heart rate of 80 to 89 bpm, and 2.08 (95% CI: 1.85 to 2.34) for a mean heart rate ≥ 90 bpm (Fig. 2A and Table 2).
Forest plots of crude and adjusted hazard ratios (95% CIs) of the primary outcome (major adverse cardiovascular events) and secondary outcomes (ischemic stroke, myocardial infarction, and heart failure) by mean initial in-hospital heart rate increments. The analyses were adjusted for age and sex in model 1, and all of the variables in the fully adjusted model (model 2), including age, sex, estimated National Institutes of Health Stroke Scale, history of hypertension, diabetes mellitus, dyslipidemia, atrial fibrillation, coronary artery disease, heart failure, cancer before admission, smoking status, body mass index, total cholesterol, triglycerides, chronic kidney disease stage, alanine aminotransferase, glycated hemoglobin, mean systolic blood pressure, mean diastolic blood pressure, antithrombotics, statins, and beta-blockers. Abbreviations: N, number; HR, hazard ratio; CI, confidence interval; bpm, beats per minute
Age, male sex, high stroke severity (eNIHSS score > 5), diabetes mellitus, CAD, HF, history of cancer before admission, currently smoking, and chronic kidney disease stages 2 to 5 were also all positively associated with risk of a MACE. Conversely, history of hypertension or dyslipidemia, abnormal body mass index, alanine aminotransferase and mean diastolic blood pressure levels, and use of antithrombotics and statins had a protective effect (Table 2).
Compared with the reference group (mean heart rate < 60 bpm), the adjusted HRs for recurrent ischemic stroke in Model 2 were 1.13 (95% CI: 0.99 to 1.30) for a mean heart rate of 60 to 69 bpm, 1.23 (95% CI: 1.08 to 1.41) for a mean heart rate of 70 to 79 bpm, 1.33 (95% CI: 1.15 to 1.53) for a mean heart rate of 80 to 89 bpm, and 1.41 (95% CI: 1.19 to 1.67) for a mean heart rate of ≥ 90 bpm (Fig. 2B and Supplementary Table S1). The adjusted HRs for MI in Model 2 were 1.12 (95% CI: 0.84 to 1.48) for a mean heart rate of 60 to 69 bpm, 1.38 (95% CI: 1.05 to 1.81) for a mean heart rate of 70 to 79 bpm, 1.97 (95% CI: 1.48 to 2.62) for a mean heart rate of 80 to 89 bpm, and 1.88 (95% CI: 1.37 to 2.57) for a mean heart rate of ≥ 90 bpm (Fig. 2C and Supplementary Table S2). The correlation between heart rate and HF was less robust; only a mean heart rate of 80 to 89 bpm was associated with increased risk of HF compared with the reference group (adjusted HR 1.34, 95% CI: 1.06 to 2.14; Fig. 2D and Supplementary Table S3).
Even after multiple adjustments for potential confounding factors, no J-shaped curve was discovered for the occurrence of the primary composite outcome, or secondary outcomes for MI and recurrent ischemic stroke. A higher mean heart rate was significantly associated with increased HRs of a MACE, recurrent ischemic stroke, and MI but not HF (Fig. 3).
Restricted cubic splines are represented for the associations between mean initial in-hospital heart rate levels and study outcomes (major adverse cardiovascular events, ischemic stroke, myocardial infarction, and heart failure). The analyses were adjusted for all of the variables in the fully adjusted model, including age, sex, estimated National Institutes of Health Stroke Scale, history of hypertension, diabetes mellitus, dyslipidemia, atrial fibrillation, coronary artery disease, heart failure, cancer before admission, smoking status, body mass index, total cholesterol, triglycerides, chronic kidney disease stage, alanine aminotransferase, glycated hemoglobin, mean systolic blood pressure, mean diastolic blood pressure, antithrombotics, statins, and beta-blockers. Abbreviation: bpm, beats per minute
Subgroup and sensitivity analyses
The results of subgroup analyses for the primary outcome are presented in Fig. 4. An association between mean heart rate and the primary outcome was discovered in all analyzed subgroups, which indicated a consistent relationship between mean initial in-hospital heart rate and MACEs.
Subgroup analyses of major adverse cardiovascular events for every increment of 1 SD in heart rate (11.3 bpm). Abbreviation: eNIHSS, estimated National Institutes of Health Stroke Scale; DM, diabetes mellitus; CAD, coronary artery disease; CKD, chronic kidney disease; HR, hazard ratio; CI, confidence interval; SD, standard deviation
Discussion
This observational study, conducted in a contemporary medically optimized population with recent ischemic stroke (95.73% patients taking antithrombotics and 52.55% patients taking statins at discharge), revealed that initial in-hospital heart rate was independently associated with significant increases in MACEs, recurrent ischemic stroke, and MI but less robust for HF. This result provides novel insight into the effect of heart rate on cardiovascular risk because it specifically focuses on a population with recent cerebral ischemic events.
In the present study, resting heart rate ≥ 70 bpm was found to place patients with ischemic stroke at increased risk of recurrent ischemic stroke and MI compared with resting heart rate < 60 bpm (Fig. 2B and C). Nevertheless, the increased risk for the composite outcome, a MACE, was already observed in patients with heart rate ≥ 60 bpm (Fig. 2A). This implies that heart rates at a level often perceived as normal may be detrimental to making a prognosis for patients with ischemic stroke.
Previous observational studies have yielded conflicting results regarding the role of heart rate in the risks of ischemic stroke and MI in different populations. In a prospective population study, resting heart rate was positively associated with the risk of ischemic stroke in participants who were free of stroke at the time of enrollment [23]. However, another prospective population study showed that, in a Chinese general population, resting heart rate was independently positively associated with the risk of MI but not with ischemic stroke or hemorrhagic stroke [24]. In an analysis of the Treating to New Targets trial, in 9580 patients with stable CAD, the increased risks of stroke or MI at heart rates above 70 bpm did not achieve significance after adjustment for potential confounders [25]. A post hoc analysis of the ONTARGET/TRANSCEND trials found that in patients with stable chronic cardiovascular disease, heart rate was positively correlated with the incidence of major vascular events, stroke, HF, cardiovascular death, and all-cause death across heart rate quintiles but was not associated with MI [26].
The effect of resting heart rate on the risk of cardiovascular events in patients with ischemic stroke is also controversial [7,8,9]. Unlike the PRoFESS and PERFORM studies, which focused on noncardioembolic ischemic stroke, this study enrolled patients with various subtypes of ischemic stroke. In the present study, a higher heart rate significantly increased the risks of recurrent ischemic stroke and MI in ischemic stroke patients (Fig. 2). This association with the primary outcome persisted regardless of atrial fibrillation status (Fig. 4). While scholars have suggested a J-shaped curve for heart rate and adverse cardiovascular outcomes [27, 28], this study found a positive association between heart rate and risks of MACE, recurrent ischemic stroke, and MI, with no clear evidence of a J-shaped curve (Fig. 3).
The correlation between heart rate and HF was less robust; only a mean heart rate of 80 to 89 bpm was associated with an increased risk of HF compared with the reference group (adjusted HR 1.51, 95% CI: 1.06 to 2.15; Fig. 2D and Supplementary Table S3). Since HF is a clinical syndrome rather than a disease, the diagnosis of HF requires a clinical evaluation that incorporates the clinical history, signs discovered during physical examination, and diagnostic testing. Therefore, the diagnosis of HF may be less precise than ischemic stroke and MI according to the administrative database in this study, which may confound the analysis of the risk of hospitalization for HF.
Heart rate is negatively associated with cardiovascular and cerebrovascular morbidity and mortality [6], and increased heart rate from sibutramine is linked to nonfatal MI in overweight patients with diabetic cardiovascular disease [29]. However, the effectiveness of heart rate–lowering agents in reducing adverse cardiovascular events is unclear. Ivabradine (If channel blocker) did not improve outcomes in stable CAD patients without HF [30]. Beta-blocker therapy for ≥ 1 year post-MI reduced all-cause mortality in acute MI patients without HF, but this benefit lost significance beyond 3 years [31]. Current heart rate–lowering agents, including beta-blockers, If channel blockers, and nondihydropyridine calcium channel blockers, have not been shown to reduce cardiovascular risk through heart rate reduction in patients with ischemic stroke.
Heart rate is determined by the intrinsic activity of the sinus node, modified by parasympathetic and sympathetic nervous system activity. Therefore, another way to reduce resting heart rate is to use a parasympathomimetic agent. Acetylcholinesterase inhibitor therapy, which can augment the parasympathetic efferent signal, was associated with negative chronotropic effects and decreased risk of cardiovascular events in patients with dementia [32]. Future studies are warranted on improvement of cardiovascular outcomes through heart rate reduction by using parasympathomimetic agents.
The present study has several limitations. One limitation is the absence of stroke etiologic classification data, such as the TOAST (Trial of ORG 10172 in Acute Stroke Treatment) classification [10]. Without this data, our analysis focuses on general cardiovascular risk factors and stroke severity, potentially missing the nuanced impacts of different stroke subtypes on long-term cardiovascular morbidity and mortality. Second, to collect the mean heart rate during the first three days of hospitalization, patients with less than three days of hospitalization were excluded from the study. Consequently, some patients with mild or extremely severe strokes may have been missed. Finally, heart rate values during follow-ups were not included in the analysis. Therefore, whether resting heart rate and the risk of major cardiovascular events are causally related cannot be concluded from this observational study.
Conclusions
Although heart rate is an easily attainable and cost-effective biomarker, it is not currently part of risk assessment in patients after ischemic stroke. Further research is needed to investigate whether using appropriate medications (such as cholinesterase inhibitors) to reduce heart rate can play a role in improving cardiovascular outcomes after ischemic stroke in the future.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- bpm:
-
Beats per minute
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- eNIHSS:
-
Estimated National Institutes of Health Stroke Scale
- HF:
-
Heart failure
- HR:
-
Hazard ratio
- ICD-9-CM:
-
International Classification of Diseases, 9th Revision, Clinical Modification
- ICD-10-CM:
-
International Classification of Diseases, 10th Revision, Clinical Modification
- MACE:
-
Major adverse cardiovascular events
- MI:
-
Myocardial infarction
References
Tofler GH, Massaro J, Levy DA, Sutherland PA, Buckley T, D’Agostino RB. Increased heart rate is associated with a prothrombotic state: the Framingham heart study. Eur J Prev Cardiol. 2017;24(4):382–8.
Reil JC, Custodis F, Swedberg K, Komajda M, Borer JS, Ford I, et al. Heart rate reduction in cardiovascular disease and therapy. Clin Res Cardiol. 2011;100(1):11–9.
Heidland UE, Strauer BE. Left ventricular muscle mass and elevated heart rate are associated with coronary plaque disruption. Circulation. 2001;104(13):1477–82.
Custodis F, Schirmer SH, Baumhakel M, Heusch G, Bohm M, Laufs U. Vascular pathophysiology in response to increased heart rate. J Am Coll Cardiol. 2010;56(24):1973–83.
Whelton SP, Blankstein R, Al-Mallah MH, Lima JA, Bluemke DA, Hundley WG, et al. Association of resting heart rate with carotid and aortic arterial stiffness: multi-ethnic study of atherosclerosis. Hypertension. 2013;62(3):477–84.
Aune D, Sen A, o’Hartaigh B, Janszky I, Romundstad PR, Tonstad S, et al. Resting heart rate and the risk of cardiovascular disease, total cancer, and all-cause mortality - a systematic review and dose-response meta-analysis of prospective studies. Nutr Metab Cardiovasc Dis. 2017;27(6):504–17.
Nolte CH, Erdur H, Grittner U, Schneider A, Piper SK, Scheitz JF, et al. Impact of heart rate on admission on mortality and morbidity in acute ischaemic stroke patients - results from VISTA. Eur J Neurol. 2016;23(12):1750–6.
Bohm M, Cotton D, Foster L, Custodis F, Laufs U, Sacco R, et al. Impact of resting heart rate on mortality, disability and cognitive decline in patients after ischaemic stroke. Eur Heart J. 2012;33(22):2804–12.
Fox K, Bousser MG, Amarenco P, Chamorro A, Fisher M, Ford I, et al. Heart rate is a prognostic risk factor for myocardial infarction: a post hoc analysis in the PERFORM (Prevention of cerebrovascular and cardiovascular Events of ischemic origin with teRutroban in patients with a history oF ischemic strOke or tRansient ischeMic attack) study population. Int J Cardiol. 2013;168(4):3500–5.
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41.
Tsai MS, Lin MH, Lee CP, Yang YH, Chen WC, Chang GH, et al. Chang Gung Research Database: a multi-institutional database consisting of original medical records. Biomed J. 2017;40(5):263–9.
Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(7):2064–89.
Hsieh MT, Hsieh CY, Tsai TT, Wang YC, Sung SF. Performance of ICD-10-CM diagnosis codes for identifying acute ischemic stroke in a national health insurance claims database. Clin Epidemiol. 2020;12:1007–13.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann Intern Med. 1999;130(6):461–70.
Sung SF, Hsieh CY, Lin HJ, Chen YW, Chen CH, Kao Yang YH, et al. Validity of a stroke severity index for administrative claims data research: a retrospective cohort study. BMC Health Serv Res. 2016;16(1):509.
Cheng TM. Reflections on the 20th anniversary of Taiwan’s single-payer National Health Insurance System. Health Aff (Millwood). 2015;34(3):502–10.
Cheng CL, Lee CH, Chen PS, Li YH, Lin SJ, Yang YH. Validation of acute myocardial infarction cases in the national health insurance research database in taiwan. J Epidemiol. 2014;24(6):500–7.
Metcalfe A, Neudam A, Forde S, Liu M, Drosler S, Quan H, et al. Case definitions for acute myocardial infarction in administrative databases and their impact on in-hospital mortality rates. Health Serv Res. 2013;48(1):290–318.
McCormick N, Lacaille D, Bhole V, Avina-Zubieta JA. Validity of heart failure diagnoses in administrative databases: a systematic review and meta-analysis. PLoS One. 2014;9(8): e104519.
Lee JD, Kuo YW, Lee CP, Huang YC, Lee M, Lee TH. Initial in-hospital heart rate is associated with long-term survival in patients with acute ischemic stroke. Clin Res Cardiol. 2022;111(6):651–62.
Diaz A, Bourassa MG, Guertin MC, Tardif JC. Long-term prognostic value of resting heart rate in patients with suspected or proven coronary artery disease. Eur Heart J. 2005;26(10):967–74.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–8.
O’Neal WT, Qureshi WT, Judd SE, Meschia JF, Howard VJ, Howard G, et al. Heart rate and ischemic stroke: the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Int J Stroke. 2015;10(8):1229–35.
Wang A, Chen S, Wang C, Zhou Y, Wu Y, Xing A, et al. Resting heart rate and risk of cardiovascular diseases and all-cause death: the Kailuan study. PLoS One. 2014;9(10):e110985.
Ho JE, Bittner V, Demicco DA, Breazna A, Deedwania PC, Waters DD. Usefulness of heart rate at rest as a predictor of mortality, hospitalization for heart failure, myocardial infarction, and stroke in patients with stable coronary heart disease (data from the Treating to New Targets [TNT] trial). Am J Cardiol. 2010;105(7):905–11.
Lonn EM, Rambihar S, Gao P, Custodis FF, Sliwa K, Teo KK, et al. Heart rate is associated with increased risk of major cardiovascular events, cardiovascular and all-cause death in patients with stable chronic cardiovascular disease: an analysis of ONTARGET/TRANSCEND. Clin Res Cardiol. 2014;103(2):149–59.
Ma R, Gao J, Mao S, Wang Z. Association between heart rate and cardiovascular death in patients with coronary heart disease: a NHANES-based cohort study. Clin Cardiol. 2022;45(5):574–82.
Lee KJ, Kim BJ, Han MK, Kim JT, Choi KH, Shin DI, et al. Effect of heart rate on stroke recurrence and mortality in acute ischemic stroke with atrial fibrillation. Stroke. 2020;51(1):162–9. https://doi.org/10.1161/STROKEAHA.119.026847.
James WP, Caterson ID, Coutinho W, Finer N, Van Gaal LF, Maggioni AP, et al. Effect of sibutramine on cardiovascular outcomes in overweight and obese subjects. N Engl J Med. 2010;363(10):905–17.
Fox K, Ford I, Steg PG, Tardif JC, Tendera M, Ferrari R, et al. Ivabradine in stable coronary artery disease without clinical heart failure. N Engl J Med. 2014;371(12):1091–9.
Kim J, Kang D, Park H, Kang M, Park TK, Lee JM, et al. Long-term beta-blocker therapy and clinical outcomes after acute myocardial infarction in patients without heart failure: nationwide cohort study. Eur Heart J. 2020;41(37):3521–9.
Isik AT, Soysal P, Stubbs B, Solmi M, Basso C, Maggi S, et al. Cardiovascular outcomes of cholinesterase inhibitors in individuals with dementia: a meta-analysis and systematic review. J Am Geriatr Soc. 2018;66(9):1805–11.
Acknowledgements
The authors thank the Center for Artificial Intelligence in Medicine, Chang Gung Memorial Hospital, for providing administrative support.
Funding
This work was supported by the Ministry of Science and Technology, Taiwan, R.O.C. (MOST 110–2222-E-182A-001-MY2) and the Chang Gung Memorial Hospital Research Project (CGRPG3L0011).
Author information
Authors and Affiliations
Contributions
J.L. and C.L. designed the research, collected data, analyzed and interpreted data and wrote the manuscript; C.L., J.Z., C.K., and Y.K. performed statistical analysis and contributed to subsequent manuscript discussion; Y.H. and M.L. performed the research and contributed to subsequent manuscript discussion.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the Human Subject Research Program of Chang Gung Medical Foundation (Approval No. 202100979B0C602). All methods were carried out in accordance with relevant guidelines and regulations. All data in the Chang Gung Research Database and National Health Insurance Research Database are anonymized and de-identified to protect individual privacy. The Institutional Review Board of the Human Subject Research Program of Chang Gung Medical Foundation waived the requirement for informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lin, CH., Zhang, JF., Kuo, YW. et al. Assessment of the impact of resting heart rate on the risk of major adverse cardiovascular events after ischemic stroke: a retrospective observational study. BMC Neurol 24, 267 (2024). https://doi.org/10.1186/s12883-024-03772-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-024-03772-3