Abstract
Background
Sleep disturbance, state anxiety, and cognitive complaints (CCs) have been recognized as important issues in public health. Although the mediating role of CCs has been proposed, their role in the relationships between sleep disturbance, state anxiety, and subjective well-being (SWB) and subjective ill-being (SIB) are not yet fully understood. This study used path analyses to investigate whether CCs mediate these relationships.
Methods
The study recruited 523 Japanese adult volunteers using convenience sampling. Participants completed the Pittsburgh Sleep Quality Index, State–Trait Anxiety Inventory (Form Y), Cognitive Complaints in Bipolar Disorder Rating Assessment, and Subjective Well-Being Inventory to evaluate sleep disturbance, state anxiety, CCs, and SWB and SIB, respectively. Path analyses were conducted to assess the mediating effects of CCs.
Results
The path analyses showed significant indirect associations of sleep disturbance and state anxiety with SWB (p = 0.024 and p = 0.012) and SIB (p < 0.001 and p < 0.001), respectively, mediated by CCs. Furthermore, there were significant indirect associations of sleep disturbance with CCs (p < 0.001), SWB (p < 0.001), and SIB (p < 0.001), via state anxiety, respectively.
Conclusions
This study suggests that CCs mediate the associations of sleep disturbance and state anxiety with SWB and SIB, respectively, in adult community volunteers. To address SWB and SIB associated with sleep disturbance and state anxiety, evaluating CCs may be useful in public mental health. Our findings will encourage health care workers to assess CCs more systematically. Future studies may need to target CCs to develop interventions for SWB and SIB.
Similar content being viewed by others
Background
Health is a state of complete physical, mental and social well-being and not merely an absence of disease or infirmity [1]. Both subjective well-being (SWB) and subjective ill-being (SIB) influences mental health [2], in which SWB correlates with the cognitive process of contentment [3] and SIB correlates with the negative psychological constructs [4]. Hence, SWB has been defined as positive affect, whereas SIB has been defined as negative affect [2]. However, the absence of SWB does not necessarily lead to SIB, and vice versa [5]. Therefore, important factors that affect mental health should be evaluated in not only SIB but also in SWB [6].
Both sleep disturbance and state anxiety are currently important issues in mental health. Sleep disturbance has been defined as poor quality sleep, and state anxiety has been defined as transient emotional anxiety [7, 8]. A close relationship between sleep disturbance and state anxiety has been shown, and sleep disturbance increases state anxiety [7, 8]. In occupational mental health, cognitive impairments caused by sleep disturbance increase the risk of workplace accidents [9,10,11]. Not only sleep disturbance but also state anxiety affect cognitive functioning, which in turn influences work performance [12]. Recent research also suggests that reducing anxiety may improve sleep quality and cognitive function [13]. In this context, cognitive impairment is a crucial factor in considering the influences of sleep disturbance and state anxiety on mental health.
Cognitive complaints (CCs) are defined as subjective cognitive problems that are perceived in daily life [14]. CCs consist of the following perceived cognitive functions; executive function, processing speed, working memory, verbal learning and memory, attention/concentration, and mental tracking [14]. For example, feeling that it takes longer than usual to complete a daily task suggests subjective impairment in processing speed. Various factors such as neurocognitive dysfunction and depressive symptoms affect CCs [14,15,16]. Furthermore, CCs influence the quality of life for individuals with psychiatric illnesses as well as for those in the general adult population [17,18,19]. Thus, CCs have been considered one of the important current issues in mental health [19,20,21].
The mediating role of CCs has recently been reported in several settings. First, CCs mediate the relations of depressive symptoms on work productivity and life quality [19, 22]. Second, CCs mediate the influence of affective factors on social function [23]. Third, CCs mediate the associations of having the history of childhood maltreatment with adulthood functional disability [24]. Recent studies reported that sleep disturbance and state anxiety directly affected CCs, and CCs directly affected SIB [25, 26]. However, whether CCs mediate the relations of sleep disturbance and state anxiety with SWB and SIB is not yet fully understood. Our study aimed to assess the mediating role of CCs on the relationships among sleep disturbance, state anxiety, SWB and SIB using mediation analyses in our path models. Furthermore, we also aimed to provide key insights into the role of CCs on mental health problems associated with sleep disturbance and state anxiety.
Methods
Study participants
The research used convenience sampling to recruit 597 adult volunteers from Tokyo between April 2017 and April 2018. This investigation was part of a larger research, in which some questionnaires were conducted to evaluate the relations of CCs with social functioning in Japanese adults [19].
Study inclusion criteria were: age ≥ 20 years; no current serious physical illness; no organic brain damage; and ability to provide agreement to participate in this investigation. We excluded 74 recruited individuals who did not complete the questionnaire. The final analysis included the data of 523 participants. They were volunteers for this research and completed the questionnaires at home or their workplace. The questionnaires were answered using paper and pen. They took approximately 40–60 min to complete the assessments, which included providing demographic information.
Measures
Demographic characteristics
We assessed the participants’ demographic characteristics using self-administered questionnaires. Psychiatric history was evaluated using the following question: “Do you have any mental illness that you have treated by going to the hospital or taking prescription medications in the past?” Ongoing psychiatric treatment was evaluated using the following question: “Do you have any mental illnesses that you are currently treating, such as by going to the hospital or taking prescription medications?” In the present study, the word “drinking” refers to the consumption of alcohol at least once a month, and the word “smoking” refers to smoking at least one cigarette per day.
Sleep disturbance
The Pittsburgh Sleep Quality Index (PSQI) was used to evaluate various aspects of subjective sleep disturbance during the previous month [27]. The index comprises 7 subscales, and each subscale score ranged from 0–3 points. The PSQI global score was obtained by summing all component scores. For instance, the PSQI item 1 was “During the past month, what time have you usually gone to bed at night?” This research used the Japanese version of the PSQI, which was developed after obtaining permission from the original authors [28]. The content and language validity of the PSQI Japanese version has been confirmed [28, 29]. The overall reliability coefficient of the Japanese version was high (Cronbach's alpha = 0.77) [28]. For the PSQI global score in this version, a score of 5.5 was the considered as the cutoff point, which provided 85.7% sensitivity and 86.6% specificity for primary insomnia [29]. This study also used a clinical cutoff point of 5.0, meaning that a PSQI global score > 5 indicated poor quality sleep [30].
State anxiety
The State–Trait Anxiety Inventory (Form Y) (STAI-Y) was used to evaluate the severity of state and trait anxiety. The inventory was composed of 40-items using a 4-point scale for each item in the 20-item state anxiety section and the 20-item trait anxiety section [31]. For instance, the STAI-Y item 1 was “I feel calm.” The STAI-Y scores were analyzed separately for state and trait anxiety, with scores for either section ranging from 20 to 80 points. The Japanese version was conducted in this research, the content and language validity of which has been confirmed [32]. In the present study, only the STAI-Y score for state anxiety was used. In the Japanese version, the reliability of state anxiety for male (Cronbach’s alpha = 0.92) and female (Cronbach’s alpha = 0.92) was high, and the mean scores of male (47.3 ± 10.4) and female (45.9 ± 10.2) were also reported [33].
CCs
The Cognitive Complaints in Bipolar Disorder Rating Assessment (COBRA) measures CCs that are perceived in daily life [14]. The COBRA evaluates executive function, processing speed, working memory, verbal learning and memory, attention/concentration, and mental tracking. It is composed of 16 items and uses a 4-point scale for each item. For instance, COBRA item 1 was “Do you have difficulty remembering peoples’ names?” The total score was obtained by adding the scores for each item [14]. The Japanese version of COBRA was developed after obtaining permission from the original authors [34]. This research used the COBRA Japanese version, for which the content and language validity has been confirmed [34]. COBRA had one-factor structure [14, 34], and the overall reliability coefficient of the Japanese version was high (Cronbach's alpha = 0.887) [34]. The COBRA total score of > 14 indicates moderate-to-severe CCs [19, 20].
SWB and SIB
The Subjective Well-Being Inventory (SUBI) measures SWB and SIB and consists of 2 domains and 40 items—19 items for SWB and 21 items for SIB [2]. The inventory for SWB consisted of 6 subscales and for SIB consisted of 4 subscales. The subscales of SWB are as follows: “general well-being” (positive affect), “expectation-achievement congruence,” “confidence in coping,” “transcendence”, “family group support,” and “social support.” The subscales of SIB are as follows: “inadequate mental mastery,” “perceived ill-health,” “deficiency in social contacts,” and “general well-being” (negative affect). The “primary group concern” subscale is included in both SWB and SIB axes. For instance, the SUBI item 1 was “Life-interesting.” A 3-point Likert scale (ranging from 1 to 3) was used for scoring each item—the higher the score, the better the state in both SWB and SIB. In other words, the higher score of SWB indicates high level of SWB, while the higher score of SIB indicates low level of SIB. This research used the Japanese version, for which the validity and reliability has been confirmed [35, 36]. In the Japanese version, the reliability of SWB (Cronbach's alpha = 0.89) and SIB (Cronbach's alpha = 0.86) were high [36]. In the present study, 19 items for SWB and 21 items for SIB (SWB scores range from 21 to 57 and SIB scores range from 28 to 63) were used for statistical analysis. In the Japanese version, the scores below 31 for SWB and 43 for SIB indicate bad conditions for SWB and SIB, respectively [36].
Statistical analysis
Pearson correlation analysis was conducted using Bonferroni adjustment to investigate the associations between PSQI global score (sleep disturbance), STAI-Y state anxiety score (state anxiety), COBRA total score (CCs), and the SUBI scores for both SWB and SIB. Two multiple regression analyses were conducted with the forced-entry method as follows: the dependent factors were SUBI SWB and SIB scores; the independent factors were sociodemographic characteristics, PSQI score, STAI-Y state anxiety score, and COBRA total score. Before conducting multiple regression analyses, linearity was verified using a normal probability plot. Path analyses were performed to investigate the relations of sleep disturbance, state anxiety, and CCs with SWB and SIB. Because of the saturation model, the study did not refer to the goodness-of-fit index. Our path model was a saturation model; hence, the sample size was calculated to be a minimum of 100 [37, 38]. The standardized path coefficients indicated the strengths of direct, indirect, and total effects. For statistical analysis, the study used STATA/MP 16 (StataCorp, College Station, TX, USA), except for the path analysis, which was conducted using Mplus version 8.4 (Stata Corp). p < 0.05 was considered to be statistically significant.
Results
The sociodemographic characteristics and clinical assessments are presented in Table 1. The number of study participants with a PSQI score > 5 was 246 (47.04%), which indicated that they had poor sleep quality, and the number of study participants with a COBRA total score > 14 was 88 (16.83%), which indicated that they had moderate to severe CCs. Notably, the proportion of participants with poor sleep quality was higher than that in a previous study in Japan [30].
The results of Pearson correlation analysis are presented in Additional file 1. Sleep disturbance was positively related with state anxiety and CCs, whereas sleep disturbance was negatively correlated with high level of SWB and low level of SIB. State anxiety was positively related with CCs, whereas state anxiety was negatively related with high level of SWB and low level of SIB. CCs were significantly and negatively related with high level of SWB and low level of SIB. High level of SWB was significantly and positively correlated with low level of SIB.
Multiple regression analysis
Significant positive predictors of high level of SWB were female sex, married status, years of education, and undergoing current psychiatric treatment (Table 2). Significant negative predictors of high level of SWB were age, sleep disturbance, state anxiety, and CCs. Significant positive predictors of low level of SIB were age and married status. Significant negative predictors of low level of SIB were having psychiatric history, sleep disturbance, state anxiety, and CCs.
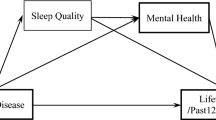
Path analysis of SWB
The associations among sleep disturbance, state anxiety, CCs, and SWB are presented in Table 3. The R2 of SWB was 0.275, meaning that the model explained 27.5% of variability in SWB, and all the paths were statistically significant (Fig. 1).
Regarding direct effects, sleep disturbance predicted state anxiety, CCs, and SWB. State anxiety predicted CCs and SWB. Further, CCs predicted SWB. Regarding indirect effects, sleep disturbance predicted CCs via state anxiety. Sleep disturbance also predicted SWB via state anxiety, via CCs, and via both state anxiety and CCs. State anxiety predicted SWB via CCs. Therefore, the mediating roles of state anxiety and CCs were shown in the model.
Path analysis of SIB
The associations among sleep disturbance, state anxiety, CCs, and SIB are presented in Table 4. The R2 of SIB was 0.433, meaning that the model explained 43.3% of variability in SIB, and all the paths were statistically significant (Fig. 2).
Regarding direct effects, sleep disturbance predicted state anxiety, CCs, and SIB. State anxiety predicted CCs and SIB, and CCs predicted SIB. Regarding indirect effects, sleep disturbance predicted CCs via state anxiety. Sleep disturbance predicted SIB via state anxiety, via CCs, and via both state anxiety and CCs. State anxiety predicted SIB via CCs. Consequently, the mediating roles of state anxiety and CCs were shown in the model.
Discussion
The present study suggests that CCs mediate the relations of sleep disturbance and state anxiety with SWB and SIB. Consistent with the previous study in Japan, both sleep disturbance and state anxiety directly affected CCs in our path models [25]. Nevertheless, to the authors’ best knowledge, these mediating roles of CCs are new findings.
A recent research reported the associations among sleep quality, anxiety, and neurocognitive function in a U.S. sample, including various races (e.g., Caucasian; 52.8%, Asian; 1.7%), in which both sleep disturbance and anxiety were found to decrease neurocognitive function [13]. Our results confirm these findings and suggest that sleep disturbance and anxiety are not only related to decreased performance on neurocognitive tests, but also predict subjective cognitive problems. In the future, the mediating role of cognitive function (as measured by neurocognitive tests) in the relationship between sleep disturbance, anxiety, and CCs in a Japanese sample needs to be investigated.
Our findings suggest the importance of assessing CCs for public health. In Japan, CCs have been gradually noted in mental health because subjective cognitive problems are detected in daily living and affect psychological and social problems [19]. However, the assessment of CCs in general adults has not yet been fully established in public health. By using a brief instrument to evaluate CCs, such as COBRA, health care workers can assess CCs more systematically. Our results indicate that it may be important to assess sleep quality and mental health, particularly anxiety, among individuals who report CCs. Addressing the underlying sleep and mental health concerns may help reduce subjective cognitive problems. A recent study suggested that internet-delivered computerized cognitive behavioral therapy may improve sleep disturbance and related symptoms, including anxiety, as well as the quality of life of individuals with insomnia in Japan [39]. Considering our findings, CCs could mediate the effectiveness of online cognitive behavioral therapy for improving the quality of life of individuals with sleep disturbance and anxiety. Thus, in the future, assessing CCs may help elucidate the mechanism of action of interventions. Currently, online cognitive behavioral therapy should be applied with care because the cost effectiveness and applicability to a given population is not yet fully investigated in Japan [40]. In considering the intervention strategy to minimize CCs, the area of cognitive dysfunction and the personal lifestyle may need to be considered together. Namely, simultaneous interventions for both cognitive dysfunction and environmental adjustments may be useful. The present study may provide useful insights into the development of intervention strategies for CCs among the Japanese population.
Regarding the characteristics of our sample, notably, most of the participants were employed at the time of the assessment. In a previous Japanese study, CCs mediated the influence of insomnia and anxiety on loss of work productivity [25]. Additionally, a recent study suggested that the loss of work productivity mediates the influence of CCs on SWB and SIB in Japanese adult workers [41]. Therefore, sleep disturbance and anxiety might lead to poorer CCs, and CCs might decrease work productivity, and consequently, SWB and SIB might be exacerbated in Japanese workers. In future studies, the role of CCs in the relationship of sleep disturbance and anxiety with work productivity, SWB, and SIB in Japanese workers needs to be investigated.
In terms of sleep disturbance, the participants of this study tended to report poor sleep quality compared with that in a previous study in Japan [30]. The present research included some individuals with ongoing psychiatric treatment, which may also affect sleep quality. Previous studies suggested that sleep disturbance endangers the health and safety of workers, and insomnia is the most important predictor of work accidents [42,43,44]. Occupational stress and violence also affect sleep disturbance of workers [45, 46]. With regard to the geographic location, living in the urban area was correlated with poor sleep in prior studies in Japan [47, 48]. In this study, all participants were recruited in urban areas, which could have influenced the participants’ sleep quality. In the future, working and living environments need to be assessed in more detail to develop health promotion activities for individuals with sleep disturbance.
Finally, it is important to discuss the mediating role of CCs on SWB and SIB. Previous studies in Japan reported the mediating roles of CCs in the relationship between depressive symptoms and work productivity, between affective factors and social function, and between having history of childhood maltreatment and functional disability [22, 23, 24]. Furthermore, affective factors mediated the relationship of having history of childhood abuse with SWB and SIB in a Japanese sample [6]. Hence, the influence of affective factors may be as important as that of CCs when evaluating individuals' quality of life, including SWB and SIB. Regarding the relationship of affective factors with CCs in Japanese population, depressive symptoms have been found to mediate the relationship of affective temperaments (cyclothymic, depressive, irritable, and anxious temperament) with CCs [49]. To the best of our knowledge, the mediating role of CCs in the relationship of affective factors with SWB and SIB is yet to be fully understood. Therefore, in future studies, the roles of CCs and affective variables in well-being should be explored in more detail.
Limitations
Regarding data collection, this study excluded 74 recruited individuals who did not complete the questionnaire. Another limitation in this study is that the sample potentially included some individuals with untreated and clinically undiagnosed psychiatric symptoms. All study subjects were recruited from a community in Japan; consequently, the results could not be generalized to other communities and countries. All participants were adults aged ≥ 20 years; thus, the results may not be generalized to children and adolescents. Regarding the factors that affect CCs, childhood maltreatment, affective temperaments, and depressive symptoms were previously established [23, 24]; hence, these factors may affect the mediating role of CCs. In addition, CCs are perceived in daily life [14], hence, they are susceptible to psychosocial factors. However, the path models in the current study could not evaluate the influence of psychosocial functioning on CCs, which could be a study limitation. Further, the volunteers were not asked about their cognitive status-MCI, dementia, etc. Also, the absence of objective cognitive assessment could be a limitation of this study. The test–retest reliability analysis of the questionnaire was not done in this study. The definition of "smoking" lacked the information about timeline, which could be a study limitation. We included some individuals with ongoing psychiatric treatment, which may also affect sleep quality. Finally, a cross-sectional survey research could not determine causality among the parameters.
Conclusion
To address SWB and SIB as related to sleep disturbance and state anxiety, assessing CCs may be useful for public mental health. Our findings point to the importance of assessing CCs more systematically by the health care workers. Future studies may need to develop interventions that target CCs to ameliorate SWB and alleviate SIB.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CCs:
-
Cognitive complaints
- COBRA:
-
Cognitive Complaints in Bipolar Disorder Rating Assessment
- PSQI:
-
Pittsburgh Sleep Quality Index
- R 2 :
-
Coefficient of determination
- SD:
-
Standard deviation
- SIB:
-
Subjective ill-being
- SUBI:
-
Subjective Well-Being Inventory
- SWB:
-
Subjective well-being
- VIF:
-
Variance inflation factor
References
World Health Organization. Definition of health in preamble to the constitution of the World Health Organization. Geneva: World Health Organization; 1946.
Sell H, Nagpal R. Assessment of subjective well-being. The subjective well-being inventory (SUBI). Regional Health Paper. SEARO, 24. New Delhi: Regional Office for South-East Asia, World Health Organization; 1992. https://apps.who.int/iris/handle/10665/204813.
Lindert J, Bain PA, Kubzansky LD, Stein C. Well-being measurement and the WHO health policy Health 2010: systematic review of measurement scales. Eur J Public Health. 2015;25:731–40.
Howell RT, Kern ML, Lyubomirsky S. Health benefits: meta-analytically determining the impact of well-being on objective health outcomes. Health Psychol Rev. 2007;1:83–136.
Keyes CLM. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002;43:207–22.
Kanai Y, Takaesu Y, Nakai Y, Ichiki M, Sato M, Matsumoto Y, et al. The influence of childhood abuse, adult life events, and affective temperaments on the well-being of the general, nonclinical adult population. Neuropsychiatr Dis Treat. 2016;12:823–32.
Pires GN, Bezerra AG, Tufik S, Andersen ML. Effects of acute sleep deprivation on state anxiety levels: a systematic review and meta-analysis. Sleep Med. 2016;24:109–18.
Bigalke JA, Greenlund IM, Carter JR. Sex differences in self-report anxiety and sleep quality during COVID-19 stay-at-home orders. Biol Sex Differ. 2020;11:56.
Shahly V, Berglund PA, Coulouvrat C, Fitzgerald T, Hajak G, Roth T, et al. The associations of insomnia with costly workplace accidents and errors: results from the America Insomnia Survey. Arch Gen Psychiatry. 2012;69:1054–63.
Uehli K, Mehta AJ, Miedinger D, Hug K, Schindler C, Holsboer-Trachsler E, et al. Sleep problems and work injuries: a systematic review and meta-analysis. Sleep Med Rev. 2014;18:61–73.
Guglielmi O, Jurado-Gámez B, Gude F, Buela-Casal G. Occupational health of patients with obstructive sleep apnea syndrome: a systematic review. Sleep Breath. 2015;19:35–44.
Sheikh MH, Waqas A, Naveed S, Shoaib M, Yousuf S, Butt SR, Tahir MH. Association of cognitive impairment with sleeping difficulties, anxiety and depression among Pakistani physicians. J Pak Med Assoc. 2018;68:932–5.
Rice VJB, Schroeder PJ. Self-reported sleep, anxiety, and cognitive performance in a sample of U.S. Military active duty and veterans. Mil Med. 2019;184(Suppl 1):488–97.
Rosa AR, Mercadé C, Sánchez-Moreno J, Solé B, Mar-Bonnin CD, Torrent C, et al. Validity and reliability of a rating scale on subjective cognitive deficits in bipolar disorder (COBRA). J Affect Disord. 2013;150:29–36.
Martínez-Arán A, Vieta E, Colom F, Torrent C, Reinares M, Goikolea JM, et al. Do cognitive complaints in euthymic bipolar patients reflect objective cognitive impairment? Psychother Psychosom. 2005;74:295–302.
Burmester B, Leathem J, Merrick P. subjective cognitive complaints and objective cognitive function in aging: A systematic review and meta-analysis of recent cross-sectional findings. Neuropsychol Rev. 2016;26:376–93.
Sumiyoshi T, Watanabe K, Noto S, Sakamoto S, Moriguchi Y, Tan KHX, et al. Relationship of cognitive impairment with depressive symptoms and psychosocial function in patients with major depressive disorder: Cross-sectional analysis of baseline data from PERFORM-J. J Affect Disord. 2019;258:172–8.
Luo X, Zhu Y, Lu D, Zong K, Lin X. Subjective cognitive dysfunction in patients with bipolar disorder: The prevalence, related factors and effects on predicting psychosocial functioning and suicidal ideation. Psychiatry Res. 2020;284:112669.
Toyoshima K, Inoue T, Masuya J, Ichiki M, Fujimura Y, Kusumi I. Evaluation of subjective cognitive function using the Cognitive Complaints in Bipolar Disorder Rating Assessment (COBRA) in Japanese adults. Neuropsychiatr Dis Treat. 2019;15:2981–90.
Miskowiak KW, Burdick KE, Martinez-Aran A, Bonnin CM, Bowie CR, Carvalho AF, et al. Methodological recommendations for cognition trials in bipolar disorder by the International society for bipolar disorders targeting cognition task force. Bipolar Disord. 2017;19:614–26.
Vieta E, Berk M, Schulze TG, Carvalho AF, Suppes T, Calabrese JR, et al. Bipolar disorders. Nat Rev Dis Primers. 2018;4:18008.
Toyoshima K, Inoue T, Shimura A, Masuya J, Ichiki M, Fujimura Y, Kusumi I. Associations between the depressive symptoms, subjective cognitive function, and presenteeism of Japanese adult workers: a cross-sectional survey study. Biopsychosoc Med. 2020;14:10.
Toyoshima K, Inoue T, Masuya J, Fujimura Y, Higashi S, Kusumi I. Does subjective cognitive function mediate the effect of affective temperaments on functional disability in Japanese adults? Neuropsychiatr Dis Treat. 2020;16:1675–84.
Toyoshima K, Inoue T, Masuya J, Fujimura Y, Higashi S, Tanabe H, et al. Structural equation modeling approach to explore the influence of childhood maltreatment in adults. PLoS One. 2020;15:e0239820.
Toyoshima K, Inoue T, Shimura A, Uchida Y, Masuya J, Fujimura Y, et al. Mediating roles of cognitive complaints on relationships between insomnia, state anxiety, and presenteeism in Japanese adult workers. Int J Environ Res Public Health. 2021;18:4516.
Toyoshima K, Ichiki M, Inoue T, Masuya J, Fujimura Y, Higashi S, et al. The role of cognitive complaints in the relationship between trait anxiety, depressive symptoms, and subjective well-Being and ill-being in adult community volunteers. Neuropsychiatr Dis Treat. 2021;17:1299–309.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Doi Y, Minowa M, Okawa M, Uchiyama M. Development of the Japanese version of the pittsburgh sleep quality index. Japanese Journal of Psychiatry Treatment. 1998;13:755–63 in Japanese.
Doi Y, Minowa M, Uchiyama M, Okawa M, Kim K, Shibui K, et al. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000;97:165–72.
Hori H, Ikenouchi-Sugita A, Yoshimura R, Nakamura J. Does subjective sleep quality improve by a walking intervention? a real-world study in a Japanese workplace. BMJ Open. 2016;6:e011055.
Spielberger CD. Manual for the State-Trait Anxiety Inventory STAI (form Y). Palo Alto: Consulting Psychologists Press; 1983.
Hidano N, Fukuhara M, Iwawaki M, Soga S, Spielberger C. State–trait anxiety inventory-form JYZ. Tokyo: UNI Agency; 2000. in Japanese.
Iwata N, Mishima N, Shimizu T, Mizoue T, Fukuhara M, Hidano T, Spielberger CD. The Japanese adaptation of the STAI Form Y in Japanese working adults–the presence or absence of anxiety. Ind Health. 1998;36:8–13.
Toyoshima K, Fujii Y, Mitsui N, Kako Y, Asakura S, Martinez-Aran A, et al. Validity and reliability of the Cognitive Complaints in Bipolar Disorder Rating Assessment (COBRA) in Japanese patients with bipolar disorder. Psychiatry Res. 2017;254:85–9.
Tonan K, Sonoda A, Ono Y. Production of the subjective well-being inventory Japanese edition: it’s reliability and validity. Jpn J Heal Psychol. 1995;8:12–9.
Ono Y, Yoshimura K. The subjective well-being inventory Japanese version. Tokyo: Kaneko Shobo; 2001.
Boomsma A. Robustness of LISREL against small sample sizes in factor analysis models. In: Joreskog KG, Wold H, editors. Systems under Indirection Observation: Causality, Structure, Prediction (Part I) North Holland. Amsterdam: The Netherlands; 1982. p. 149–73.
Boomsma A. Nonconvergence, Improper solutions, and starting values in LISREL Maximum likelihood estimation. Psychometrika. 1985;50:229–42.
Sato D, Yoshinaga N, Nagai E, Nagai K, Shimizu E. Effectiveness of internet-delivered computerized cognitive behavioral therapy for patients with insomnia who remain symptomatic following pharmacotherapy: randomized controlled exploratory trial. J Med Internet Res. 2019;21:e12686.
Nakao M, Shirotsuki K, Sugaya N. Cognitive-behavioral therapy for management of mental health and stress-related disorders: recent advances in techniques and technologies. Biopsychosoc Med. 2021;15:16.
Toyoshima K, Ichiki M, Inoue T, Shimura A, Masuya J, Fujimura Y, et al. Subjective cognitive impairment and presenteeism mediate the associations of rumination with subjective well-being and ill-being in Japanese adult workers from the community. Biopsychosoc Med. 2021;15:15.
Magnavita N, Garbarino S. Sleep, health and wellness at work: a scoping review. Int J Environ Res Public Health. 2017;14:1347.
Garbarino S, Guglielmi O, Puntoni M, Bragazzi NL, Magnavita N. Sleep quality among police officers: implications and insights from a systematic review and meta-analysis of the literature. Int J Environ Res Public Health. 2019;16:885.
Garbarino S, Tripepi G, Magnavita N. Sleep health promotion in the workplace. Int J Environ Res Public Health. 2020;17:7952.
Magnavita N, Soave PM, Antonelli M. Prolonged stress causes depression in frontline workers facing the COVID-19 pandemic-a repeated cross-sectional study in a COVID-19 hub-hospital in Central Italy. Int J Environ Res Public Health. 2021;18:7316.
Magnavita N, Di Stasio E, Capitanelli I, Lops EA, Chirico F, Garbarino S. Sleep problems and workplace violence: a systematic review and meta-analysis. Front Neurosci. 2019;13:997.
Demura S, Sato S. Urban–rural differences in subjective symptoms of fatigue and their relations with lifestyle factors in young male Japanese students. Environ Health Prev Med. 2003;8:52–8.
Abe Y, Fujise N, Fukunaga R, Nakagawa Y, Ikeda M. Comparisons of the prevalence of and risk factors for elderly depression between urban and rural populations in Japan. Int Psychogeriatr. 2012;24:1235–41.
Toyoshima K, Inoue T, Masuya J, Fujimura Y, Higashi S, Kusumi I. Associations among childhood parenting, affective temperaments, depressive symptoms, and cognitive complaints in adult community volunteers. J Affect Disord. 2020;276:361–8.
World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
Acknowledgements
The authors thank Dr. Nobutada Takahashi of Fuji Psychosomatic Rehabilitation Institute Hospital, Dr. Hiroshi Matsuda of Kashiwazaki Kosei Hospital, deceased Dr. Yasuhiko Takita of Maruyamasou Hospital, and Dr. Yoshihide Takaesu of Izumi Hospital for collecting data. The authors also thank their colleagues at Tokyo Medical University and Hokkaido University. This work was supported by JSPS KAKENHI Grant No. JP20K16662.
Funding
This work was partly supported by a Grant-in-Aid for Scientific Research from the Japanese Ministry of Education, Culture, Sports, Science and Technology [grant number 16K10194, to T. Inoue], Research and Development Grants for Comprehensive Research for Persons with Disabilities from the Japan Agency for Medical Research and Development [grant number JP18dk0307060, to T. Inoue], SENSHIN Medical Research Foundation (to T. Inoue), and JSPS KAKENHI [no. JP20K16662 to K. Toyoshima]. The funding sources had no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
All authors contributed toward data collection and reviewed and approved this manuscript. KT: Writing—original draft, Data curation, Writing—review & editing. MI: Writing—original draft, Data curation, Writing—review & editing. TI: Writing—original draft, Data curation, Writing—review & editing. AS: Data curation, Writing—review & editing. JM: Data curation, Writing—review & editing. YF: Data curation, Writing—review & editing. SH: Data curation, Writing—review & editing. IK: Data curation, Writing—review & editing. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Local Ethics Committee of Tokyo Medical University approved this study (approval number: SH3502), which was conducted in accordance with the Declaration of Helsinki [50]. All participants provided written informed consent before participating of the present study.
Consent for publication
Not applicable.
Competing of interests
Jiro Masuya has received personal compensation from Otsuka Pharmaceutical, Eli Lilly, Astellas, and Meiji Yasuda Mental Health Foundation, as well as grants from Pfizer. Masahiko Ichiki received personal compensation from Otsuka Pharmaceutical, Pfizer, Eli Lilly, Mitsubishi Tanabe Pharma, Mochida Pharmaceutical, Meiji Seika Pharma, Janssen Pharmaceutical, Takeda Pharmaceutical, MSD, Dainippon Sumitomo Pharma, and Eisai; grants from Otsuka Pharmaceutical, Eli Lilly, Eisai, Shionogi, Takeda Pharmaceutical, MSD, and Pfizer; and is a member of the advisory board of Meiji Seika Pharma. Ichiro Kusumi has received honoraria from Daiichi Sankyo, Dainippon Sumitomo Pharma, Eisai, Eli Lilly, Janssen Pharmaceutical, Lundbeck, Meiji Seika Pharma, Mochida Pharmaceutical, MSD, Mylan, Novartis Pharma, Ono Pharmaceutical, Otsuka Pharmaceutical, Pfizer, Shionogi, Shire, Taisho Toyama Pharmaceutical, Takeda Pharmaceutical, Tsumura, and Yoshitomiyakuhin, and has received research/grant support from Asahi Kasei Pharma, Astellas, Daiichi Sankyo, Dainippon Sumitomo Pharma, Eisai, Eli Lilly, Mochida Pharmaceutical, Novartis Pharma, Otsuka Pharmaceutical, Pfizer, Shionogi, Takeda Pharmaceutical and Tanabe Mitsubishi Pharma. Takeshi Inoue is a member of the advisory boards of Pfizer, Novartis Pharma, and Mitsubishi Tanabe Pharma and has received personal fees from Mochida Pharmaceutical, Takeda Pharmaceutical, Eli Lilly, Janssen Pharmaceutical, MSD, Taisho Toyama Pharmaceutical, Yoshitomiyakuhin, and Daiichi Sankyo; grants from Shionogi, Astellas, Tsumura, and Eisai; and grants and personal fees from Otsuka Pharmaceutical, Dainippon Sumitomo Pharma, Mitsubishi Tanabe Pharma, Kyowa Pharmaceutical Industry, Pfizer, Novartis Pharma, and Meiji Seika Pharma. Yota Fujimura received research and grant support from Novartis Pharma, Otsuka Pharmaceutical, Astellas, Dainippon Sumitomo Pharma, and Shionogi. Shinji Higashi received honoraria from Dainippon Sumitomo Pharma and Novartis Pharma. Akiyoshi Shimura reports personal fees from Eisai, Sumitomo Dainippon Pharma, MSD, Yoshitomi Yakuhin Corporation, and Meiji Seika Pharma, outside the submitted work. Kuniyoshi Toyoshima does not have any actual or potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Pearson Correlation Analysis Using Bonferroni Adjustment (N = 523).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Toyoshima, K., Ichiki, M., Inoue, T. et al. Cognitive complaints mediate the influence of sleep disturbance and state anxiety on subjective well-being and ill-being in adult community volunteers: a cross sectional study. BMC Public Health 22, 566 (2022). https://doi.org/10.1186/s12889-022-12936-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-12936-0