Abstract
Background
Ensuring the availability of safe drinking water remains a critical challenge in developing countries, including Ethiopia. Therefore, this paper aimed to investigate the prevalence of fecal coliform and E. coli bacteria and, geographical, children availability, and seasonal exposure assessment through a meta-analysis.
Methods
Two independent review groups extensively searched internet databases for English-language research articles published between 2013 and 2023. This systematic review and meta-analysis followed PRISMA guidelines. The methodological quality of each included study was evaluated using the STROBE guidelines. Publication bias was assessed by visual inspection of a funnel plot and then tested by the Egger regression test, and meta-analysis was performed using DerSimonian and Laird random-effects models with inverse variance weighting. Subgroup analyses were also conducted to explore heterogeneity.
Results
Out of 48 potentially relevant studies, only 21 fulfilled the inclusion criteria and were considered for meta-analysis. The pooled prevalence of fecal coliform and E. coli was 64% (95% CI: 56.0–71.0%, I2 = 95.8%) and 54% (95% CI: 45.7–62.3%, I2 = 94.2%), respectively. Subgroup analysis revealed that the prevalence of fecal coliform bacteria increased during the wet season (70%) compared to the dry season (60%), particularly in households with under-five children (74%) compared to all households (61%), in rural (68%) versus urban (66%) areas, and in regions with high prevalence such as Amhara (71%), Gambela (71%), and Oromia (70%). Similarly, the prevalence of E. coli was higher in households with under-five children (66%) than in all households (46%).
Conclusions
The analysis highlights the higher prevalence of fecal coliform and E. coli within households drinking water, indicating that these bacteria are a significant public health concern. Moreover, these findings emphasize the critical need for targeted interventions aimed at improving drinking water quality to reduce the risk of fecal contamination and enhance public health outcomes for susceptible groups, including households with under-five children, in particular geographical areas such as the Amhara, Gambela, and Oromia regions, as well as rural areas, at point-of-use, and during the rainy season.
Registration
This review was registered on PROSPERO (registration ID - CRD42023448812).
Similar content being viewed by others
Introduction
An essential requirement for the health and well-being of people is access to safe drinking water. However, most of the world’s population lacks access to adequate, sustainable, and safe water [1, 2]. Considering this, in 2015, the United Nations ratified different developmental goals, including the Sustainable Development Goal (SDG) 6.1, which aspires to achieve universal and equitable access to safe and affordable drinking water for all by 2030 [3]. This goal emphasizes having access to safe drinking water for every household [4]. To monitor this phenomenon, most countries, including Ethiopia, have adopted the World Health Organization’s (WHO) guidelines for drinking water quality [1].
Worldwide, water-related diseases account for approximately 80% of all illnesses and diseases and, in turn, cause an estimated 505,000 diarrheal deaths each year [5]. Children are more susceptible to microbiological pollutants and develop an illness due to their immature immune systems [6]. As a result, waterborne diseases continue to be major health problems worldwide. Particularly in most developing nations where access to potable water is scarce, water-borne diseases are a serious public health concern as a result of bacterial contamination of drinking water [7]. Water-borne pathogenic bacteria could infect or harm humans by secreting toxins that could harm human tissue, living as parasites within human cells, or colonizing within the body to interfere with regular bodily processes. Numerous harmful bacteria, such as fecal coliforms, Escherichia coli, Salmonella typhi, and Vibrio cholerae, have been identified in water [8]. These bacteria can lead to various waterborne diseases, including cholera, typhoid, and diarrhea [5].
In developing countries, the main causes of diarrheal diseases are bacteria, protozoa, viruses, and helminths [9]. Specifically, in rural areas of most developing countries, where water sources are communally shared and exposed to several fecal-oral transmission channels within their local boundaries, fecal contamination of drinking water is a primary cause of water-borne diseases, including fatal diarrhea [10]. This could be detected by examining the presence of potential indicator organisms such as fecal coliforms [11, 12].
Several pathogenic bacteria can be transmitted via polluted drinking water [13, 14]. Drinking water can be polluted at the source, distribution line, and/or household level, and such polluted water can be a vehicle for several pathogens [2, 15]. In Ethiopia, poor environmental health conditions resulting from subpar water quality and inadequate hygiene and sanitation standards are responsible for more than 60% of infectious diseases [16]. Studies conducted in Ethiopia revealed that the prevalence of fecal contamination in drinking water, including Escherichia coli (E. coli), total coliforms (TC), and fecal coliforms, have been extremely high [17,18,19,20,21,22].
This could be due to many reasons, as water safety depends on various factors, from the quality of the source water to its storage and handling practices in the home [23]. Even if the source is clean, the process of collecting, transporting, storing, and drawing water in the household can all lead to fecal contamination [17]. In addition, pollutants in drinking water sources include human excreta, animal waste, effluent agricultural practices, and floods, as well as a lack of knowledge among end-users about hygiene and environmental cleanliness [17, 24]. Due to inadequate access and frequent interruptions in the piped water supply [25], drinking water is commonly stored, often for considerable lengths of time, resulting in gross contamination [26].
Therefore, understanding the extent and epidemiological variation of bacterial contamination in household drinking water is vital for policymakers and public health officials to allocate resources efficiently and target interventions effectively to reduce the burden of waterborne illnesses in Ethiopia. Despite individual studies on contamination levels, there is a notable research gap due to the lack of a national systematic review and meta-analysis. Existing research does not fully examine how contamination varies with factors such as children’s availability, geographic regions, water sources, and seasonal changes. This study aims to address this gap by offering a comprehensive review and meta-analysis, providing essential insights for policymakers to effectively allocate resources and target interventions to reduce waterborne illnesses and support vulnerable groups.
Methodology
Data sources and search strategy
The review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [S1] and the protocol of this study was registered with the International Prospective Register of Systematic Reviews (PROSPERO), with protocol registration number CRD42023448812. With a focus on English-language materials, we conducted an exhaustive search across numerous electronic databases, including PubMed, Web of Science, Google Scholar, ScienceDirect, ProQuest, Directory of Open Access Journals, POPLINE, African Journals Online, and the Cochrane Library. The search strategy included a combination of keywords and controlled vocabulary related to Ethiopia, drinking water, and specific indicators of pathogenic bacteria. Moreover, the search strategies for Google Scholar were [Microbiological OR Microorganisms OR Organisms OR Bacteriological OR pathogens] AND [“Water quality” OR “Water contamination”] AND [household OR domestic OR residential OR home] AND [“Drinking water”] AND [intitle: Ethiopia], and those for Pubmed were ((Microbiological OR Microorganisms OR Organisms OR Bacteriological OR pathogens) AND (“Water quality” OR “Water contamination”)) AND (household OR domestic OR residential OR home)) AND (“Drinking water”)) AND (Ethiopia [Title]). we have provided a detailed breakdown of the query [S5].
Study selection criteria
Studies were included if they met the following criteria: (i) Original research was conducted in Ethiopia, and only peer-reviewed journal articles, as they undergo rigorous review processes and were more likely to meet high-quality standards; (ii) Focus on the prevalence of those specific indicators of pathogenic bacteria in household drinking water; (iii) Published in English; (vi) Articles with a cross-sectional study, had freely available full texts and were published between 2013 and 2023. However, articles with no clear data were excluded.
Methodological quality of the included studies
Two groups independently assessed the methodological rigor of every study included, employing the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [27]. Each study was then classified based on its quality: “Good” (G) if it achieved a score of at least 70% of the total points, “Fair” (F) if it scored between 50% and 69%, and “Poor” (P) if its score was below 50% [S2].
Extraction and analysis
Following the selection of pertinent articles, two investigators individually screened the titles and abstracts to determine their suitability for full-text review. Subsequently, these investigators utilized a standardized data extraction template in Microsoft Office Excel 2021 to collect study characteristics, prevalence, sample sizes, season, child availability, water sources, and geographic locations. In the event of any disagreements between the two investigators, a third investigator intervened, and their decision was considered final. The data analysis was performed using STATA 16.0 software. Random effects meta-analysis models were used to investigate the pooled prevalence of indicators of pathogenic bacterial contaminants using DerSimonian and Laird’s approach with 95% confidence intervals (CIs) [28]. The inverse of the Freeman-Tukey double arcsine transformation was used to stabilize the variance of each study [29].
A forest plot was generated to visually assess the pooled prevalence estimates and corresponding 95% confidence intervals (CIs) across the included studies. For statistical heterogeneity across studies, the I2 statistic was used [30]. Heterogeneity was considered high, moderate, or low, with I2 values of 75, 50, and 25%, respectively. To identify potential sources of heterogeneity, subgroup analyses were conducted in under-five children’s availability, seasons, residential, water sources, and regional settings. Publication bias was assessed by visual inspection of the funnel plot and tested by the Egger regression test [31, 32].
Results
Search results
A total of 992 articles were identified from the nine databases, and an additional 14 articles were identified through additional manual searching. Three hundred forty-two studies were removed due to being duplicates found both within the same database and across different databases. A total of 616 studies were determined to be ineligible during title and abstract screening. At the full-text review stage, 27 articles were excluded because they did not measure microbial indicators of interest. The flow chart of the study selection process is presented in Fig. 1, generated using the PRISMA flow diagram [33].
Characteristics of the included studies
This study included 16 studies with 4,193 samples for fecal coliform [17, 34,35,36,37,38,39,40,41,42,43,44,45,46,47,48], and eight studies with 2,594 samples for E. coli analysis [38, 46, 48,49,50,51,52,53]. The main characteristics of the selected studies are summarized in the article matrix [S2]. All the articles were cross-sectional studies and followed a random sampling procedure. The articles included in the study were conducted between 2013 and 2023 and sample sizes ranged from 42 to 538 for E. coli and from 42 to 736 for fecal coliforms.
The data were collected from seven regions of Ethiopia. Nine studies in Amhara region [35, 36, 40, 42,43,44,45, 49, 51], one study each in Sidama [47], Somali [53] and Gambela [41] regions, two studies each in Oromia [17, 46], and Tigray [34, 38] regions, four studies in SNNPR [37, 39, 48, 52], and one study in all over Ethiopia [50] were conducted. Moreover, six studies were conducted in households with under-five children only [41, 42, 44, 49, 51, 53].
Pooled meta-analysis
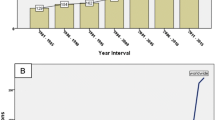
The forest plot of the prevalence estimates and the corresponding 95% confidence intervals (CIs) of the contaminants are presented in Figs. 2 and 3. The pooled prevalence of fecal coliform was 63.7% (95% CI: 56.0–71.0%, I2 = 95.8%, based on 16 studies) in a total sample of 4193 households. Additionally, the pooled prevalence of E. coli was 54.0 (95% CI: 45.7–62.3%, I2 = 94.2%, based on 8 studies) in a total sample of 2,594 households. The funnel plot [S3] showed almost no publication bias, which was confirmed by the Egger regression test for both fecal coliform (p = 0.10) and E. coli (p = 0.18). Moreover, no publication bias was confirmed by the ‘Trim and Fill’ sensitivity analysis, as we did not find any hypothetical missing studies. A leave-one-out sensitivity analysis found that excluding any single study resulted in an average variation of 1% in the pooled prevalence of fecal coliforms and 1.93% for E. coli, indicating no substantial impact on the overall results.
Heterogeneity and subgroup analysis
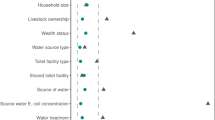
The pooled prevalence of fecal coliform among the dry seasons samples was 60.1% (95% CI: 47.4–72.1), while for the wet seasons samples, it was 70.3% (95% CI: 63.8–76.3). When stratified by residence, the pooled prevalence in rural and urban areas were 68.0% [95%CI: 59.0–76.3] and 66.4% [95%CI: 49.1–81.7], respectively. Specifically, households with under-five children had a higher prevalence of fecal coliform (73.8% [95% CI: 63.9–82.7%]) than all households without any restrictions (61.0% [95% CI: 51.8–69.8]). When stratified by regions, the prevalence of fecal coliform was highest (71.4%) in Amhara, 71.2% in Gambela, and 70.1% in Oromia, compared with 58.1% in SNNP, 31.7% in Sidama, and 42.0% in Tigray. Regarding sample collection sources, the prevalence of fecal coliform is higher at the point of use (66.4% [95% CI: 57.3–74.9]) compared to the point of source (57.8% [95% CI: 42.0-72.3]). No significant publication bias was observed in any of the subgroup analyses (Table 1).
The pooled prevalence of E. coli (Fig. 4) among only households with under-five children was 65.9% (95% CI: 57.9–73.4), while for all households, it was 45.9% (95% CI: 35.2–56.9). The detailed distribution of the pooled prevalence of E. coli in household drinking water is shown in a table [S4].
Discussion
This systematic review and meta-analysis aimed to compile all available data reporting the prevalence and epidemiological distribution of indicators of pathogenic bacteria in households’ drinking water in Ethiopia. The study findings help enhance public health interventions in Ethiopia by identifying vulnerable groups and suggesting appropriate measures to reduce the impact of waterborne diseases. This knowledge enables more targeted interventions to mitigate the effects of such diseases effectively. The findings of this systematic review and meta-analysis revealed that the pooled prevalence of fecal coliforms in households’ drinking water in the 16 cross-sectional studies with 4193 samples was 63.7% (95% CI: 56.0, 71.0%).
This is lower than that found in a similar systematic review and meta-analysis in developing countries, where the fecal contamination of household drinking water was 75% (95% CI: 64, 84%) [54]. Differently, this is comparably high compared to the pooled prevalence in Africa (53%, 95% CI: 42, 63%); and also, significantly higher than the study conducted in South-East Asia (35%, 95% CI: 24, 45%) [55]. This variation might come from differences in how samples are collected and could also be because South-East Asia has better water quality rules and improvements compared to Ethiopia. In addition, the pooled prevalence of E. coli in households’ drinking water in the 8 cross-sectional studies with a total of 2,594 samples was 54% (95% CI: 45.7, 62.3%). This pooled prevalence is lower than a systematic review and meta-analysis conducted in Africa (2000–2021) where the pooled prevalence of E. coli in drinking water was 71.7% (95% CI: 56.2, 83.3%) [56]. Regional variations in water contamination in Ethiopia, compared to other African countries, can be influenced by factors like the types of water sources, the effectiveness of sanitation and water treatment practices, local environmental conditions, and differences in public health standards.
In this study, the prevalence of fecal coliform in households drinking water in the wet season was higher (70.3%) than in the dry season (60.1%). Similarly, a study conducted in Ghana found that the proportion of the population at risk of fecal contamination in the rainy season (41.5%) was higher compared to the dry season (33.1%) [57]. Furthermore, the pooled prevalence of fecal coliform was higher (73.8%) among households with only under-five children than in other households, this might be because of improper disposal of child feces. The pooled prevalence of fecal coliform was lower (66.4%) among urban households than rural (68%). Similarly, a systematic review and meta-analysis study on fecal contamination of drinking water globally, and in low-and-middle-income countries found that drinking water is more contaminated in rural areas than in urban areas [55, 58]. This might be because urban areas have better infrastructure, like improved water sources and improved sanitation, which help to keep lower contamination levels.
Finally, the pooled prevalence of fecal coliform was higher at the point of use (66.4%) compared to the source point (57.8%). Similarly, a study conducted in Bangladesh found a lower contamination rate of 28% in water samples taken from the source compared to a significantly higher contamination rate of 73.96% in samples from stored household sources (point of use) [59]. The higher pooled prevalence of contamination observed in stored household water, compared to source water, is likely due to poor storage conditions, inadequate hygiene practices, and exposure to environmental contaminants. Future research should explore how Ethiopian water management practices and infrastructure impact fecal coliform and E. coli prevalence to identify effective interventions. Longitudinal studies could track changes in water quality over time. Additionally, more research in underrepresented regions is needed to understand water contamination patterns and improve policies for safer drinking water in Ethiopia.
Conclusion
The findings of this systematic review and meta-analysis point to a higher prevalence of E. coli and fecal coliform in Ethiopia, raising serious concerns about public health that require attention. There are variations within the country by season, residence, region, sources of sample collection and availability of under-five children. Subgroup assessments revealed an increased risk during the wet season, among only households with under-five children, at point-of-use, residing in rural areas, notably in the Amhara, Gambella, and Oromia regions. These findings emphasize the critical necessity for targeted interventions in vulnerable populations and specific geographic areas to address the risks posed by drinking water contamination and improve public health outcomes promptly.
Strengths and limitations of this study
We employed appropriate methods to stabilize variability across studies and enhance the reliability of our overall findings. The generalizability of our study might be constrained because of the restricted regional coverage within the country.
Data availability
No datasets were generated or analysed during the current study.
References
WHO. (2021). A global overview of national regulations and standards for drinking-water quality.
WHO and UNICEF. Progress on Drinking Water, Sanitation and Hygiene: 2017 Update and SDG Baselines, World Health Organization, Geneva, Switzerland, 2017.
UN. 2016., Transforming our world: The 2030 agenda for sustainable development.
UN. 2020., The sustainable development goals report 2020.
WHO., Drinking Water: Key Facts, WHO, Geneva, Switzerland,. 2020, https://www.who.int/en/news-room/fact-sheets/detail/drinking-water.
Simon AK, Hollander GA, McMichael A. Evolution of the immune system in humans from infancy to old age. Proc Biol Sci. 2015;282(1821). https://doi.org/10.1098/rspb.2014.3085.
Ford TE, Hamner S. A perspective on the global pandemic of Waterborne Disease. Microb Ecol. 2018;76(1):2–8.
Momtaz H, Dehkordi FS, Rahimi E, Asgarifar A. Detection of Escherichia coli, Salmonella species, and Vibrio cholerae in tap water and bottled drinking water in Isfahan, Iran. BMC Public Health. 2013;13. https://doi.org/10.1186/1471-2458-13-556.
WHO., Diarrhoeal disease, 7 March. 2024. https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease.
Gwimbi P, George M, Ramphalile M. Bacterial contamination of drinking water sources in rural villages of Mohale Basin, Lesotho: exposures through neighbourhood sanitation and hygiene practices. Environ Health Prev Med. 2019;24(1). https://doi.org/10.1186/s12199-019-0790-z.
Ladokun OA, Oni SO. Physico-Chemical and Microbiological Analysis of Potable Water in Jericho and Molete areas of Ibadan Metropolis. Adv Biol Chem. 2015;05:197–202.
Abebe B, Dejene, Hailu. Bacteriological and Physicochemical Quality of Drinking Water Sources and Household Water Handling Practice among Rural communities of Bona District, Sidama Zone-Zouthern, Ethiopia. Sci J Public Health. 2015;3(5). https://doi.org/10.11648/j.sjph.20150305.37.
Girmay AM, et al. Associations of WHO/UNICEF Joint Monitoring Program (JMP) Water, Sanitation and Hygiene (WASH) Service Ladder service levels and sociodemographic factors with diarrhoeal disease among children under 5 years in Bishoftu town, Ethiopia: a cross-sectional study. BMJ open. 2023;13(7):e071296.
WHO. Guidelines for drinking-water quality: First Addendum to the Fourth Edition. 4th ed. Geneva, Switzerland: World Health Organization; 2017b.
Legesse T, Dessie W, Abera F, Gobena W, Girma S, Muzeyin R, Gonfa A, Desta K. Virological and bacteriological quality of drinking water in Ethiopia. Int J Infect Dis. 2018;73. https://doi.org/10.1016/j.ijid.2018.04.3909.
WHO. Water, Sanitation and Hygiene Links to Health, Facts and Figures, World Health Organization, Geneva, 2004.
Amenu D, Gobena. SMT. Assessment of water handling practices among rural communities of dire dawa administrative council, dire dawa, Ethiopia. Sci Techn Arts Res J. 2013;2(2). https://doi.org/10.4314/star.v2i2.98891.
Fufa BK, Liben M, Dessalegn. Bacteriological quality of drinking tap water in selected districts of north showa zone, Amhara, Ethiopia. Archives Appl Sci Res. 2016;8:23–7.
Yasin M, Bacha KT. Physico-chemical and bacteriological quality of drinking water of different sources, Jimma Zone, Southwest Ethiopia. BMC Res Notes. 2015;8:541. Epub 2015/10/07.
Tsega N, Sahile S, Kibret M, Abera B. Bacteriological and physico-chemical quality of drinking water sources in a rural community of Ethiopia. Afr Health Sci. 2013;13(4). https://doi.org/10.4314/ahs.v13i4.42.
Mengesha A, Baye MW. A survey of bacteriological quality of drinking water in North Gondar. Ethiop J Health Dev. 2004;18(2):112–5.
Girmay AM, et al. Access to water, sanitation and hygiene (WASH) services and drinking water contamination risk levels in households of Bishoftu Town, Ethiopia: a cross-sectional study. Health Sci Rep. 2023;6(11):e1662.
Banda K, Sarkar R, Gopal S, Govindarajan J, Harijan BB, Jeyakumar MB, et al. Water handling, sanitation and defecation practices in rural southern India: a knowledge, attitudes and practices study. Trans R Soc Trop Med Hyg. 2007;101(11):1124–30.
Meride Y. Drinking water quality assessment and its effects on residents health in Wondo Genet campus. Ethiopia Environ Sys Res. 2016;5(1):1.
Adane M, Mengistie B, Medhin G, Kloos H, Mulat W. Piped water supply interruptions and acute diarrhea among under-five children in Addis Ababa slums, Ethiopia: a matched case-control study. PLoS One, 12, e0181516. (2017).
Chalchisa D, Megersa M, Beyene A. Assessment of the quality of drinking water in storage tanks and its implication on the safety of urban water supply in developing countries. Environ Syst Res. 2017;6:12. https://doi.org/10.1186.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–7.
Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67(11):974–8.
Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10:101–29.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Baye Sitotaw and Molla Nigus. Bacteriological and physicochemical quality of drinking water in Kobo town, Northern Ethiopia. Journal of Water, Sanitation and Hygiene for Development; 2021. 11.2.
Sitotaw B, Geremew M. Bacteriological and Physicochemical Quality of Drinking Water in Adis Kidame Town, Northwest Ethiopia. Int J Microbiol. 2021;2021. https://doi.org/10.1155/2021/6669754.
Sitotaw B, Melkie E, Temesgen D. Bacteriological and Physicochemical Quality of Drinking Water in Wegeda Town, Northwest Ethiopia. J Environ Public Health. 2021;2021. https://doi.org/10.1155/2021/6646269.
Gizachew M, Admasie A, Wegi C, Assefa E. Bacteriological Contamination of Drinking Water Supply from Protected Water sources to point of Use and Water Handling practices among Beneficiary households of Boloso Sore Woreda, Wolaita Zone, Ethiopia. Int J Microbiol. 2020;2020. https://doi.org/10.1155/2020/5340202.
Gebrewahd A, Adhanom G, Gebremichail G, Kahsay T, Berhe B, Asfaw Z, et al. Bacteriological quality and associated risk factors of drinking water in Eastern Zone, Tigrai, Ethiopia, 2019. Trop Dis Travel Med Vaccines. 2020;6. https://doi.org/10.1186/s40794-020-00116-0.
Zemachu A et al. Bacteriological Quality of Drinking Water and Associated Factors at the Internally Displaced People Sites, Gedeo Zone, Southern Ethiopia: A Cross-sectional StudyEnvironmental Health Insights Volume 15: 1–6 2021 DOI: 10.1177/11786302211026469.
Getachew A, Tadie A, Chercos DH, Guadu T, Alemayehu M, Gizaw, Zemichael MG, Hiwot, Cherkos TG. Bacteriological quality of household drinking water in North Gondar Zone, Ethiopia; a community-based cross-sectional study. Appl Water Sci. 2021;11(12). https://doi.org/10.1007/s13201-021-01515-0.
Mekonnen GK, Mengistie B, Sahilu G, Mulat W, Kloos, Helmut. Determinants of microbiological quality of drinking water in refugee camps and host communities in Gambella Region, Ethiopia. J Water Sanitation Hygiene Dev. 2019;9(4):671–82.
Berihun G, Hassen AM, Gizeyatu S, Berhanu A, Teshome L, Walle D, Desye Z, Sewunet B. B and Keleb A Drinking water contamination potential and associated factors among households with under-five children in rural areas of Dessie Zuria District, Northeast Ethiopia. Front. Public Health 11:1199314. doi: 10.3389/fpubh.2023.1199314. (2023).
Birhan TA, Bitew BD, Dagne H, Amare DE, Azanaw J, Andualem Z, et al. Household drinking water quality and its predictors in flood-prone settings of Northwest Ethiopia: a cross-sectional community-based study. Heliyon. 2023;9(4):e15072.
Feleke H, Medhin G, Kloos H, Gangathulasi J, Asrat D. Household-stored drinking water quality among households of under-five children with and without acute diarrhea in towns of Wegera District, in North Gondar, Northwest Ethiopia. Environ Monit Assess. 2018;190(11). https://doi.org/10.1007/s10661-018-7033-4.
Getachew A, Tadie A, Chercos DH, Guadu T. Level of Faecal Coliform Contamination of Drinking Water Sources and its Associated Risk factors in rural settings of North Gondar Zone, Ethiopia: a cross-sectional community based study. Ethiop J Health Sci. 2018;28(2):227–34.
Edessa N, Geritu N, Mulugeta K. Microbiological assessment of drinking water with reference to diarrheagenic bacterial pathogens in Shashemane Rural District, Ethiopia, Vol. 11(6), pp. 254–263, 14 February, 2017 DOI: 10.5897/AJMR2016.8362.
Robel SB, Mohammed AT. Physicochemical and microbial quality of drinking water in slum households of Hawassa City. Ethiopia Appl Water Sci (2023) 134 https://doi.org/10.1007/s13201-022-01806-0
Dhengesu D, Lemma H, Asefa L, Tilahun D. Antimicrobial Resistance Profile of Enterobacteriaceae and drinking Water Quality among households in Bule Hora Town, South Ethiopia. Risk Manag Healthc Policy. 2022;15. https://doi.org/10.2147/rmhp.s370149.
Usman MA, Gerber, Nicolas. Irrigation, drinking water quality, and child nutritional status in northern Ethiopia. J Water Sanitation Hygiene Dev. 2020;10(3). https://doi.org/10.2166/washdev.2020.045.
Usman MA, Gerber N, Pangaribowo, Evita H. Drivers of microbiological quality of household drinking water – a case study in rural Ethiopia. J Water Health. 2017;16(2). https://doi.org/10.2166/wh.2017.069.
Gizaw Z, Yalew AW, Bitew BD, Lee J, Bisesi M. Fecal indicator bacteria along multiple environmental exposure pathways (water, food, and soil) and intestinal parasites among children in the rural northwest Ethiopia. BMC Gastroenterol, 2022. 22(1): p.: https://doi.org/10.1186/s12876-022-02174-4
Alemayehu TA, Weldetinsae A, Dinssa DA, Derra FA, Bedada TL, Asefa YB, et al. Sanitary condition and its microbiological quality of improved water sources in the Southern Region of Ethiopia. Environ Monit Assess. 2020;192(5). https://doi.org/10.1007/s10661-020-08297-z.
Muhummed AM, Osman Y, Abdillahi R, Hattendorf J, Zinsstag J, Tschopp, Rea, Cissé G. Water Quality, Sanitation, Hygiene, and Diarrheal Diseases among Children in Adadle District, Somali Region, Eastern Ethiopia. 2023, Research Square(unpublished).
Shields KF, et al. Association of supply type with fecal contamination of source water and household stored drinking water in developing countries: a bivariate meta-analysis. Environ Health Perspect. 2015;123(12):1222–31.
Bain R, Cronk R, Hossain R, Bonjour S, Onda K, Wright J, et al. Global assessment of exposure to faecal contamination through drinking water based on a systematic review. Trop Med Int Health. 2014;19(8):917–27.
Ramatla T, Ramaili T, Lekota KE, Ndou R, Mphuti N, Bezuidenhout, Carlos and, Thekisoe O. A systematic review and meta-analysis on prevalence and antimicrobial resistance profile of Escherichia coli isolated from water in africa (2000–2021). Heliyon, 2023: p.: https://doi.org/10.1016/j.heliyon.2023.e16123
Dongzagla A, Jewitt S, Hara O. Seasonality in faecal contamination of drinking water sources in the Jirapa and Kassena-Nankana municipalities of Ghana. Sci Total Environ. 2021;752. https://doi.org/10.1016/j.scitotenv.2020.141846.
Bain R, Cronk R, Wright J, Yang H, Slaymaker T, Bartram J. Fecal contamination of drinking-water in low- and middle-income countries: a systematic review and meta-analysis. PLoS Med. 2014;11(5):e1001644.
Mahmud ZH, Islam MS, Imran KM, Worth HSAI, Ahmed M. Occurrence of Escherichia coli and faecal coliforms in drinking water at source and household point-of-use in Rohingya camps, Bangladesh. Gut Pathogens. 2019;11(1):52.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
EAA, AW, AMG, ZAA, TT, and AKD conceived, designed the review, and did the data collection and analysis for the study. EAA, AW, and AMG drafted the manuscript. MGW, MGS, KTT, MAK, and GKY reviewed the manuscript. EAA, AW, AMG, MT, and DAD checked the final analysis and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable here, as this is a systematic review and meta-analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Adugna, E.A., Weldetinsae, A., Alemu, Z.A. et al. Prevalence and epidemiological distribution of indicators of pathogenic bacteria in households drinking water in Ethiopia: a systematic review and meta-analysis. BMC Public Health 24, 2511 (2024). https://doi.org/10.1186/s12889-024-20067-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-20067-x