Abstract
Background
Patients with severe aortic stenosis and left ventricular systolic dysfunction have a poor prognosis, and this may result in inferior survival also after aortic valve replacement. The outcomes of transcatheter and surgical aortic valve replacement were investigated in this comparative analysis.
Methods
The retrospective nationwide FinnValve registry included data on patients who underwent transcatheter or surgical aortic valve replacement with a bioprosthesis for severe aortic stenosis. Propensity score matching was performed to adjust the outcomes for baseline covariates of patients with reduced (≤ 50%) left ventricular ejection fraction.
Results
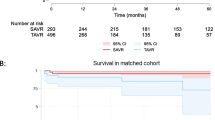
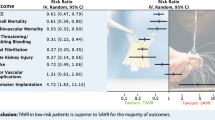
Within the unselected, consecutive 6463 patients included in the registry, the prevalence of reduced ejection fraction was 20.8% (876 patients) in the surgical cohort and 27.7% (452 patients) in the transcatheter cohort. Reduced left ventricular ejection fraction was associated with decreased survival (adjusted hazards ratio 1.215, 95%CI 1.067–1.385) after a mean follow-up of 3.6 years. Among 255 propensity score matched pairs, 30-day mortality was 3.1% after transcatheter and 7.8% after surgical intervention (p = 0.038). One-year and 4-year survival were 87.5% and 65.9% after transcatheter intervention and 83.9% and 69.6% after surgical intervention (restricted mean survival time ratio, 1.002, 95%CI 0.929–1.080, p = 0.964), respectively.
Conclusions
Reduced left ventricular ejection fraction was associated with increased morbidity and mortality after surgical and transcatheter aortic valve replacement. Thirty-day mortality was higher after surgery, but intermediate-term survival was comparable to transcatheter intervention.
Trial registration The FinnValve registry ClinicalTrials.gov Identifier: NCT03385915.
Similar content being viewed by others
Introduction
The prevalence of aortic stenosis (AS) and left ventricular (LV) dysfunction is increasing due to the aging population [1, 2]. Patients with AS and associated LV systolic dysfunction have a poor prognosis, even if they are asymptomatic [3]. This condition may result in inferior survival even after aortic valve replacement [4]. The outcomes after both transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (SAVR) have improved over the last decade [5], but the incidence of congestive heart failure and mortality after both interventions remains high among patients with LV dysfunction [4, 6]. The feasibility of TAVR is documented in AS patients with high surgical risk [7].
In patients with AS and reduced LV ejection fraction (LVEF) the optimal treatment modality choice is unclear. The purpose of this comparative analysis was to investigate the short- and intermediate-term outcome of this patient group treated with TAVR or SAVR in a nationwide patient cohort.
Materials and methods
The FinnValve registry is a nationwide registry (ClinicalTrials.gov Identifier: NCT03385915) containing data from consecutive and unselected patients who underwent TAVR or SAVR with a bioprosthesis for severe AS at Finnish university hospitals from 2008 to 2017 [5]. Patients with AS with or without aortic valve regurgitation, aged > 18 years, and who underwent primary TAVR or SAVR with a bioprosthesis with or without concomitant coronary artery revascularization were included. Patients with prior TAVR or surgical intervention on the aortic valve, concomitant procedure on the ascending aorta and/or other heart valves or structures, TAVR or SAVR for isolated aortic valve regurgitation, and/or acute endocarditis were excluded. The Finnish Institute for Health and Welfare provided data on date and causes of mortality, which is routinely collected from death certificates issued by physicians. The last date of follow-up was December 31, 2018. Secondary early outcomes were recorded during the index hospitalization. The echocardiographic assessments were made by experienced cardiologists and/or cardiac anesthesiologists depending on the local institute practice. The pre- and perioperative timing for echocardiographic assessment varied between the cohorts and institutions. The exact method for determining LVEF for each patient was not captured to the FinnValve registry data.
Definition criteria of baseline risk factors
Severe AS was defined according to current guidelines [8, 9] by echocardiography. LV dysfunction was defined as LVEF ≤ 50% according to the EuroSCORE II criteria [10]. LVEF ≤ 50% was further dichotomized in to LVEF 30–50% and LVEF < 30% groups. Baseline variables were defined according to the EuroSCORE II criteria. The operative risk was stratified according to the EuroSCORE II and STS [11] risk scores. Frailty was defined according to the Geriatric Status Scale (GSS) [12] grades 2–3. Severe coronary artery disease was defined as any stenosis ≥ 50% of the main coronary branches. Critical preoperative state was defined as ventricular tachycardia or ventricular fibrillation or aborted sudden death, preoperative cardiac massage, preoperative ventilation before anesthetic room, preoperative inotropes or intra-aortic balloon pump (IABP) insertion and/or preoperative acute renal failure. Patients with critical preoperative state were included in patients with recent acute heart failure.
Outcome measures
The primary outcomes were 30-day, 1-year and 4-year survival. The secondary outcomes during the index hospitalization were stroke, use intra-aortic balloon pump (IABP) and/or extracorporeal membrane oxygenation (ECMO), red blood cell (RBC) transfusions, transfusion of > 4 units of RBC and/or re-sternotomy for bleeding [13], and/or transfusion of > 4 units of RBC and/or any reoperation for intrathoracic or peripheral bleeding, major and life threatening bleeding [13], major vascular complication [13], moderate-to-severe paravalvular regurgitation, implantation of permanent pacemaker, acute kidney injury (AKI) and postoperative length of index hospital stay.
Definition of outcomes
Major vascular complications were defined according to Valve Academic Research Consortium-2 consensus document (VARC-2) criteria [13]. Stroke was defined as any neurological deficit lasting ≥ 24 h with a new brain infarct or hemorrhage at neuroimaging, or a neurological deficit resulting in death. Major and life-threatening bleeding were defined according to VARC-2 criteria excluding perioperative decline in the hemoglobin levels because a perioperative decrease of hemoglobin levels is observed in most of patients undergoing SAVR and this does not always reflect a condition of major perioperative blood loss. European Coronary Artery Bypass Grafting (E-CABG) bleeding grades 2–3 was defined as transfusion of > 4 units of red blood cells and/or resternotomy for bleeding [14]. AKI was defined according to the Kidney Disease: Improving Global Outcomes (KDIGO) classification criteria [15]. Cardiac death was defined as any death occurring from coronary artery disease, valvular heart disease, heart failure, conduction disturbances, endocarditis, sudden cardiac death or death during the index procedure.
Statistical analysis
Statistical analysis was performed using SAS statistical package, version 9.2 (SAS Institute Inc, Cary, NC), SPSS v. 26.0 statistical software (IBM Corporation, New York, USA) and Stata v. 15.0 (SAS Institute Inc., Cary, NC, USA).
Continuous variables were summarized as mean and standard deviation and categorical variables as counts and percentages. Normal distribution of continuous variables was assessed with the Shapiro–Wilk’s test. In the unmatched main cohort, Chi-squared test, Fisher’s exact test and Mann–Whitney U-test were used for univariable analysis. The Kaplan–Meier method was used to estimate late survival. Outcomes were adjusted in logistic regression and Cox proportional hazards models, using the enter mode and including the following covariates: age, gender, body mass index, glomerular filtration estimated according to the MDRD equation (eGFR), LVEF ≤ 50%, diabetes, dialysis, prior stroke, recent myocardial infarction, pulmonary disease, oxygen therapy, atrial fibrillation, extracardiac arteriopathy, frailty, recent acute heart failure, systolic pulmonary artery pressures, New York Heart Association (NYHA) class IV symptoms, urgency of the procedure, severe coronary artery disease, left main disease, number of diseased coronary arteries, prior cardiac surgery, prior percutaneous coronary intervention, planned concomitant revascularization, active malignancy, prior pacemaker, mitral regurgitation (mild, moderate and severe individually) and anemia. These regression analyses were performed separately for the unmatched TAVR and SAVR cohorts.
Patients with LVEF ≤ 50% were the subjects of a propensity score matching analysis comparing the outcomes after TAVR and SAVR. The propensity score was estimated using a non-parsimonious logistic regression model including the covariates as follows: age, gender, body mass index, anemia, eGFR, prior dialysis, diabetes, stroke and transient ischemic attack, pulmonary disease, oxygen therapy, extracardiac arteriopathy, porcelain aorta, atrial fibrillation, frailty, active malignancy, LVEF classes, systolic pulmonary artery pressure, mitral regurgitation, coronary artery disease, left main coronary stenosis, number of diseased coronary arteries, prior pacemaker, prior percutaneous coronary intervention, prior cardiac surgery, recent myocardial infarction, recent acute heart failure, NYHA class 4 symptoms, urgency, planned concomitant revascularization, EuroSCORE II and STS scores. One-to-one propensity score matching was performed employing the nearest neighbor method and a caliper width of 0.2, which was the 0.2 of the standard deviation of the logit of the propensity score, i.e. 1.068. To evaluate the balance between the matched groups, the t-test for paired samples for continuous variables and the McNemar test for dichotomous were used. Standardized differences < 0.10 were considered an acceptable imbalance between the groups. Baseline characteristics and early outcomes in the propensity score matched cohorts were evaluated using the paired t-test and the McNemar test. Differences in the long-term survival of matched pairs was evaluated by the Kaplan–Meier method. Since the proportional hazard assumption did not hold as assessed graphically and based on Schoenfeld’s residuals (global test: p = 0.080), the impact of treatment method on 4-year survival in propensity score-matched pairs was estimated using the restricted mean survival time (RMST) method. All tests were two-sided and p < 0.05 was set for statistical significance.
Results
The FinnValve registry includes data from 6463 patients who underwent TAVR or SAVR with bioprosthesis for severe AS. After excluding patients who underwent transapical TAVR and those without data on the LVEF and pulmonary artery pressures, 5854 patients were available for the present analysis (Fig. 1). The prevalence of LVEF ≤ 50% was 20.8% (876 patients) in the SAVR cohort and 27.7% (452 patients) in the TAVR cohort. However, among patients with LVEF ≤ 50%, TAVR was the most common procedure for AS since 2016 (Additional file 1: Fig. S1). The mean length of follow-up was 2.9 ± 1.8 years after TAVR and 4.4 ± 2.9 years after SAVR cohort.
The characteristics and outcomes of the main cohort are presented in Additional file 1: Tables S1 and S2. In the entire cohort, LVEF ≤ 50% was associated with decreased intermediate survival (adjusted HR 1.215, 95%CI 1.067–1.385). However, when adjusted for baseline variables, LVEF ≤ 50% was not associated with increased 30-day mortality after SAVR (OR 0.999, 95%CI 0.647–1.540, p = 1.000) or TAVR (OR 1.171, 95%CI 0.508–2.698, p = 0.71). The risk of death at intermediate follow-up was increased after SAVR (HR 1.238, 95%CI 1.060–1.445, p = 0.007), but not after TAVR (HR 1.080, 95%CI 0.840–1.388, p = 0.548). There was no difference in baseline LVEF levels between these procedures (Additional file 1: Table S3). Furthermore, the degree of reduction in LVEF did not affect survival in patients with LVEF ≤ 50% (Additional file 1: Table S4).
Propensity score matching analysis in patients with LVEF ≤ 50%
Propensity score matching resulted in 255 pairs with balanced baseline risk factors (Table 1). SAVR patients underwent more frequently planned concomitant coronary artery revascularization compared to TAVR patients (29.4 vs. 5.1%, p < 0.0001), despite similar prevalence (SAVR 36.5% vs. TAVR 38.4%) and severity of coronary artery disease (Table 1). Mean aortic valvular gradient was 46 ± 16 mmHg in TAVR patients and 46 ± 14 mmHg in SAVR patients (p = 0.848) (Table 1).
Among propensity score matched pairs, SAVR patients had increased rates of bleeding, AKI, blood transfusion, need of mechanical circulatory support and prolonged hospital stay compared to TAVR. TAVR patients had higher rates of vascular complications requiring operation, whereas SAVR patients had increased rates of resternotomy for bleeding (Table 2). Permanent pacemaker implantation rates were more frequent after TAVR. The incidence of postoperative AF was particularly high after SAVR (SAVR 73.7% vs. TAVR 41.6%, p < 0.0001). Thirty-day mortality was higher in the SAVR cohort (7.8% vs. 3.1%, p = 0.038). One-year and 4-year survival in the TAVR cohort were 87.5% and 65.9% and in the SAVR cohort 83.9% and 69.6% (RMST ratio, 1.002, 95%CI 0.929–1.080, p = 0.964) (Fig. 2). During the first 4 years after intervention, the cause of death was of cardiac nature in 69.1% of patients in the SAVR cohort and 51.7% in the TAVR cohort (p = 0.043).
Discussion
This study provides compelling data on the current treatment practice and outcomes of the patients with severe AS and LVEF ≤ 50% in a nationwide setting. The main findings are: (1) early mortality was increased after SAVR; (2) intermediate-term survival was similar after TAVR and SAVR; (3) non-cardiac death was common in this elderly population with multiple co-morbidities.
Patients with LVEF ≤ 50% have poorer prognosis compared to patients with normal systolic function and the prognosis is impaired even after aortic valve operation [4, 16, 17]. In the present study population, only 69.6% of SAVR patients and 65.9% of TAVR patients survived beyond 4-year follow-up. Similarly, in our earlier study [18] recent acute heart failure was associated with worse 30-day and 5-year survival compared to patients with no recent hospitalization for heart failure.
The development of heart failure in AS patients is of multifactorial nature [19,20,21]. Only 50% of the AS patients with heart failure have reduced LVEF and LVEF reduction in this population is often not caused by AS, but rather myocardial damage due to ischemic heart disease or other cardiomyopathies [22]. Also, the significance of sex, diastolic dysfunction and left bundle branch block are recognized [23]. Still, the ultimate cause of LVEF deterioration in AS remains unresolved. The extent of cardiac damage correlates to worse outcomes [24], even despite still normal LVEF [25,26,27]. The diastolic dysfunction has already developed when LVEF starts to decrease [28]. Data on diastolic function were not collected in our study population.
The risk for mortality and morbidity increases after surgery with worsening LVEF, and decreased LVEF has been shown being an independent predictor of mortality at 5-year [17, 26]. On the other hand, data from the TVT Registry showed that low-gradient severe AS, rather than the level of baseline LV dysfunction, was associated with 1-year mortality after TAVR [16]. In the present study, at 4-year follow-up the degree of LV dysfunction did not affect survival. Even LVEF < 60% is found to be a risk factor for inferior prognosis [26, 27]. Early intervention may be beneficial for asymptomatic patients with very severe AS [29, 30].
The possible benefits of TAVR over SAVR are unclear for intermediate-risk patients with LVEF ≤ 50% [31, 32]. The procedure type did not affect LVEF recovery in the PARTNER trial including patients with moderate LV dysfunction [33]. LVEF ≤ 50% is associated with an increased risk of sudden cardiac death and all-cause mortality after TAVR, despite LVEF postprocedural improvement [21]. New-onset conduction disturbances and/or the need for a new pacemaker after TAVR are associated with a failure of LVEF recovery after TAVR [34].
Coronary artery revascularization was performed more often during SAVR than with TAVR reflecting the contemporary practice and guidelines. Leaving coronary artery disease untreated during SAVR impairs long-term survival regardless of disease severity [35]. Wolff et al. conclude on their meta-analysis on patients with heart failure with reduced LVEF and coronary disease, that revascularization with either CABG or PCI improves the long-term survival [36]. Recent meta-analysis from Sakurai et al. suggests that patients who underwent TAVR with PCI had a higher all-cause mortality than those with SAVR with CABG [37]. Still, data on concomitant revascularization during TAVR is controversial and scarce. The multi-disciplinary Heart team approach remains imperative for patients with AS and coronary artery disease [37].
Limitations
The main limitation of this study is its retrospective nature. Second, there may be some degree of interobserver variability in the echocardiographic data and the timing of pre- and perioperative echocardiography varied between the cohorts and institutions. Third, the registry does not capture specific data on the type of aortic stenosis such as high-gradient, low-flow low-gradient, and normal-flow low-gradient AS and an analysis of the subtypes of AS is not feasible. Fourth, the comparison of the study cohorts is based on propensity score matching and its results are potentially biased by unmeasured confounders. Fifth, risks associated with ischemic cardiomyopathy and differences in procedure type related revascularization strategies may affect the results. Finally, the relatively small sample size of this study may affect the reliability of the findings.
Conclusions
This nationwide registry demonstrated that AS patients with LVEF ≤ 50% have high morbidity and mortality after SAVR and TAVR with no difference in intermediate-term survival between these treatment methods. These findings are in line with previous studies evaluating high-risk patients and patients with LV dysfunction. Further studies on the timing of treatment and treatment pathway choice are needed to optimize the outcomes individually.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- AF:
-
Atrial fibrillation
- AKI:
-
Acute kidney injury
- AS:
-
Aortic stenosis
- ECMO:
-
Extracorporeal membrane oxygenation
- KDIGO:
-
Kidney disease: improving global outcomes
- IABP:
-
Intra-aortic balloon pump
- LV:
-
Left ventricle
- LVEF:
-
Left ventricular ejection fraction
- RBC:
-
Red blood cell
- SAVR:
-
Surgical aortic valve replacement
- TAVR:
-
Transcatheter aortic valve replacement
References
Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007;93(9):1137 LP – 1146.
Kupari M, Lindroos M, Iivanainen AM, Heikkila JTR. Congestive heart failure in old age: prevalence, mechanisms and 4-year prognosis in the Helsinki Ageing Study. J Intern Med. 1997;241:387–94.
Henkel DM, Malouf JF, Connolly HM, Michelena HI, Sarano ME, Schaff HV, et al. Asymptomatic left ventricular systolic dysfunction in patients with severe aortic stenosis: characteristics and outcomes. J Am Coll Cardiol. 2012;60(22):2325–9.
Une D, Mesana L, Chan V, Maklin M, Chan R, Masters RG, et al. Clinical impact of changes in left ventricular function after aortic valve replacement: analysis from 3112 patients. Circulation. 2015;132(8):741–7.
Mäkikallio T, Jalava MP, Husso A, Virtanen M, Laakso T, Ahvenvaara T, et al. Ten-year experience with transcatheter and surgical aortic valve replacement in Finland. Ann Med. 2019;51(3–4):270–9.
Passeri JJ, Elmariah S, Xu K, Inglessis I, Baker JN, Alu M, et al. Transcatheter aortic valve replacement and standard therapy in inoperable patients with aortic stenosis and low EF. Heart. 2015;101(6):463 LP – 471.
Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364(23):2187–98.
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. 2021;143(5):e72-227.
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739–91.
Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41:734–45.
The Society of Thoracic Surgeons. Online STS adult cardiac surgery risk calculator. 2017. http://riskcalc.sts.org/stswebriskcalc/#/. Accessed 7 Oct 2018.
Rockwood K, Stadnyk K, MacKnight C, McDowell I, Hébert R, Hogan DB. A brief clinical instrument to classify frailty in elderly people. Lancet. 1999;353:205–6.
Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document (VARC-2). Eur J Cardiothorac Surg. 2012;42:S45–60.
Biancari F, Ruggieri VG, Perrotti A, Svenarud P, Dalen M, Onorati F, et al. European multicenter study on coronary artery bypass grafting (E-CABG registry): study protocol for a prospective clinical registry and proposal of classification of postoperative complications. J Cardiothorac Surg. 2015;10:90.
Kellum J, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, Goldstein SL, et al. Kidney disease: improving Global Outcomes (KDIGO) clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1–138.
Baron SJ, Arnold SV, Herrmann HC, Holmes DR, Szeto WY, Allen KB, et al. Impact of ejection fraction and aortic valve gradient on outcomes of transcatheter aortic valve replacement. J Am Coll Cardiol. 2016;67(20):2349–58.
Dahl JS, Eleid MF, Michelena HI, Scott CG, Suri RM, Schaff HV, et al. Effect of left ventricular ejection fraction on postoperative outcome in patients with severe aortic stenosis undergoing aortic valve replacement. Circ Cardiovasc Imaging. 2015;8(4): e002917.
Jalava MP, Laakso T, Virtanen M, Niemelä M, Ahvenvaara T, Tauriainen T, et al. Transcatheter and surgical aortic valve replacement in patients with recent acute heart failure. Ann Thorac Surg. 2020;109(1):110–7.
Bavishi C, Kolte D, Gordon PC, Abbott JD. Transcatheter aortic valve replacement in patients with severe aortic stenosis and heart failure. Heart Fail Rev. 2018;23(6):821–9.
Kamperidis V, Delgado V, van Mieghem NM, Kappetein AP, Leon MB, Bax JJ. Diagnosis and management of aortic valve stenosis in patients with heart failure. Eur J Heart Fail. 2016;18(5):469–81.
Steiner J, Rodés-Cabau J, Holmes DRJ, LeWinter MM, Dauerman HL. Mechanical intervention for aortic valve stenosis in patients with heart failure and reduced ejection fraction. J Am Coll Cardiol. 2017;70(24):3026–41.
Spitzer E, Ren B, Kroon H, van Gils L, Manintveld O, Daemen J, et al. Moderate aortic stenosis and reduced left ventricular ejection fraction: current evidence and challenges ahead. Front Cardiovasc Med. 2018;5:111.
Ito S, Miranda WR, Nkomo VT, Connolly HM, Pislaru SV, Greason KL, et al. Reduced left ventricular ejection fraction in patients with aortic stenosis. J Am Coll Cardiol. 2018;71(12):1313 LP – 1321.
Généreux P, Pibarot P, Redfors B, Mack MJ, Makkar RR, Jaber WA, et al. Staging classification of aortic stenosis based on the extent of cardiac damage. Eur Heart J. 2017;38(45):3351–8.
Herrmann HC, Pibarot P, Hueter I, Gertz ZM, Stewart WJ, Kapadia S, et al. Predictors of mortality and outcomes of therapy in low-flow severe aortic stenosis: a placement of aortic transcatheter valves (PARTNER) trial analysis. Circulation. 2013;127(23):2316–26.
Dahl JS, Magne J, Pellikka PA, Donal E, Marwick TH, et al. Assessment of subclinical left ventricular dysfunction in aortic stenosis. JACC Cardiovasc Imaging. 2019;12(1):163–71.
Taniguchi T, Morimoto T, Shiomi H, Ando K, Kanamori N, et al. Prognostic impact of left ventricular ejection fraction in patients with severe aortic stenosis. JACC Cardiovasc Interv. 2018;11(2):145–57.
Elahi MM, Chuang A, Ewing MJ, Choi CH, Grant PW, Matata BM. One problem two issues! Left ventricular systolic and diastolic dysfunction in aortic stenosis. Ann Transl Med. 2014;2(1):10.
Kang DH, Park SJ, Lee SA, Lee S, Kim DH, Kim HK, et al. Early surgery or conservative care for asymptomatic aortic stenosis. N Engl J Med. 2020;382(2):111–9.
Lancellotti P, Magne J, Dulgheru R, Clavel MA, Donal E, Vannan MA, et al. Outcomes of patients with asymptomatic aortic stenosis followed up in heart valve clinics. JAMA Cardiol. 2018;3(11):1060–8.
Reardon MJ, Van Mieghem NM, Popma JJ, Kleiman NS, Søndergaard L, Mumtaz M, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;376(14):1321–31.
Langer NB, Ando M, Simpson M, van Boxtel BS, Sorabella RA, Patel V, et al. Influence of left ventricular ejection fraction on morbidity and mortality after aortic root replacement. J Thorac Cardiovasc Surg. 2019;158(4):984-991.e1.
Elmariah S, Palacios IF, McAndrew T, Hueter I, Inglessis I, Baker JN, et al. Outcomes of transcatheter and surgical aortic valve replacement in high-risk patients with aortic stenosis and left ventricular dysfunction: results from the Placement of Aortic Transcatheter Valves (PARTNER) trial (cohort A). Circ Cardiovasc Interv. 2013;6(6):604–14.
Nazif TM, Williams MR, Hahn RT, Kapadia S, Babaliaros V, Rodés-Cabau J, et al. Clinical implications of new-onset left bundle branch block after transcatheter aortic valve replacement: analysis of the PARTNER experience. Eur Heart J. 2014;35(24):1599–607.
Thalji NM, Suri RM, Daly RC, Greason KL, Dearani JA, Stulak JM, et al. The prognostic impact of concomitant coronary artery bypass grafting during aortic valve surgery: implications for revascularization in the transcatheter era. J Thorac Cardiovasc Surg. 2015;149(2):451–60.
Wolff G, Dimitroulis D, Andreotti F, Kołodziejczak M, Jung C, Scicchitano P, et al. Survival benefits of invasive versus conservative strategies in heart failure in patients with reduced ejection fraction and coronary artery disease: a meta-analysis. Circ Hear Fail. 2017;10(1):e003255.
Sakurai Y, Yokoyama Y, Fukuhara S, Takagi H, Kuno T. Complete transcatheter versus surgical approach to aortic stenosis with coronary artery disease: a systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2022. https://doi.org/10.1016/j.jtcvs.2022.08.006.
Acknowledgements
None.
Funding
This work was supported by the Department of Clinical Medicine University of Turku, the Finnish Foundation for Cardiovascular Research and the Finnish Cultural Foundation. The FinnValve trial is carried out without funding.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: MPJ, MS, FB, JA, VA. (II) Administrative support: FB, JA, VA, TJ, AV, ME, ML, PR, MN, TM. (III) Provision of study materials or patients: MPJ, MS, TA, TL, MV, MN, PM, AH, SD, JJ, ML, TM, PR, ME, AV, TJ, FB, JA, VA. (IV) Collection and assembly of data: MPJ, TT, PM, AH, EK, SD, JJ, MV, TL. (V) Data analysis and interpretation: MPJ, FB, SR, PDE. (VI) Manuscript writing: All authors. (VII) Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study is approved by the Institutional Review Board of each the institutions. Informed consent was waived due to the retrospective registry nature of the study. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Competing interests
MPJ, received grants from the Department of Clinical Medicine University of Turku, the Finnish Foundation for Cardiovascular Research and the Finnish Cultural Foundation; MS, is proctor for Medtronic, relationship is significant; TA, none; TL, none; MV, none; MN, none; TT, none; PM, none; AH, none; EK, none; SD, none; JJ, none; SR, none; PDE, none; ML, none; TM, none; PR, none; ME, none; AV, none; TJ, none; FB, none; JA, none; VA, none.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Fig. S1.
Frequencies of transcatheter (TAVR) and surgical aortic valve replacement (SAVR) along the study period in patients with severe aortic stenosis and reduced left ventricular ejection fraction (LVEF≤50%). Table S1. Characteristics of unmatched patients with left ventricular ejection fraction >50% and ≤50% undergoing surgical or transcatheter aortic valve replacement. Table S2. Outcomes of unmatched patients with left ventricular ejection fraction >50% and ≤50% after surgical or transcatheter aortic valve replacement. Table S3. Left ventricular ejection fraction and NYHA classes of unmatched patients with left ventricular ejection fraction ≤50% undergoing surgical or transcatheter aortic valve replacement. Table S4. The effect of baseline left ventricular ejection fraction on survival in unmatched patients with LVEF≤50% undergoing surgical or transcatheter aortic valve replacement.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jalava, M.P., Savontaus, M., Ahvenvaara, T. et al. Transcatheter and surgical aortic valve replacement in patients with left ventricular dysfunction. J Cardiothorac Surg 17, 322 (2022). https://doi.org/10.1186/s13019-022-02061-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-022-02061-9