Abstract
Depression is the most disastrous mood disorder affecting the health of individuals. Conventional treatments with chemical compounds for depression have limitations, while herbal medicine has unique therapeutic effects. This paper introduces the pharmacological basis and biological mechanisms underlying the botanical antidepressants over the past 5 years. Based upon the specific therapeutic targets or mechanisms, we analyzed the pathological roles of monoamine neurotransmitters, the hypothalamic–pituitary–adrenal axis, inflammation, oxidative stress, synaptic plasticity performed in antidepressant of the botanicals. In addition, gut flora and neurogenesis were also preferentially discussed as treatment approaches. Based on the complex pathogenesis of depression, we suggested that mixed use of botanicals, namely prescription would be more suitable for treatment of depression. In addition, neural circuit affected by botanicals or active components should also attract attention as the botanicals have potential to be developed into fast-acting antidepressants. Finally, gut flora might be a new systemic target for the treatment of depression by botanicals. This review would strength botanical medicine as the antidepressant and also provides an overview of the potential mechanisms involved.
Similar content being viewed by others
Background
Depression is a devastating psychiatric disorder, generally characterized by loss of interest, anxiety, sleep disturbance, lack of energy, and suicidal thoughts. Epidemiological studies show that the global prevalence of depression and depression-related symptoms is increasing annually [1]. The prevalence of depression is high in women (20% to 25%), while is relatively low in men (7% to 12%) [2]. Depression is one of the major causes for suicide. However, the cause of depression is unclear, and the factors causing the disease are complicated. Current pathogenesis includes abnormal expression of neurotransmitters [serotonin (5-HT), norepinephrine (NE) and dopamine (DA)] or receptors, the hypothalamic–pituitary–adrenal (HPA) axis dysfunction, imbalance of inflammatory cytokines, oxidative stress, impairment of synaptic plasticity [3, 4]. In addition, abnormality of gut flora and epigenetic alteration of genes are also important determinants for the symptoms of depression [5, 6] (Fig. 1). However, the drugs available for depression were restricted in regulating neurotransmitters, including selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, atypical antidepressants, tricyclic antidepressants and monoamine oxidase inhibitors.
Animal models were produced mainly based on the symptoms of depression, including cognition and emotion, behavioral despair, hopelessness, anxiety-like symptoms, anxiety and locomotor activity, and anhedonia [7]. Learned helpless (LH) model, unpredictable chronic mild stress (UCMS) model, early life stress model, olfactory bulbectomy (OBX) model, social defeat model, chronic restraint stress (CRS) model and glucocorticoid/corticosterone model are typical models which are widely used to investigate the pathogenesis and screen therapeutic agents for depression [7]. Additionally, several genetic depression models were also utilized (Tph1−/− mice, Vmat2−/− mice, etc.) [8, 9].
Herbal products are the major constitute of traditional Chinese medicine, which embodies intact theory to treat diseases [10]. Botanicals or their active components have been extensively investigated in the treatment of depression-like behaviors [11]. Especially, the mixed use of botanicals, namely prescription in Chinese medicine has a prior function to ameliorate symptoms of depression [12]. With the discovery of the pathogenesis of depression, therapeutic targets for botanicals have been gradually verified using the depressive animal models. This review comprises of a systematic 5-year update of research of botanicals for the treatment of depression based on the pathogenesis and potential therapeutic targets for depression.
Neurotransmitters and their receptors
Depression has been chemically linked to problems or imbalances in the brain with regard to the neurotransmitters like 5-HT, NE, and DA [13]. Remedy of the depressed neurotransmitters has thus become the primary selection for treatment of depression. The active components from botanicals have the advantages to remedy the abnormalities of neurotransmitters through regulating synthesis of neurotransmitters, reabsorption of neurotransmitters, balancing the ratio of excitatory and inhibitory neurotransmitters, re-uptake of neurotransmitters by neurons, antagonizing 5-HT2A receptor, etc.
Tian et al. [14] found that adhyperforin, a newly-identified active component of H. perforatum exerts strong antidepressant effects by binding to 5-HT and NE transporter and inhibiting their reabsorption. Zirak et al. [15] showed that the anti-depressant effects of hypericin may be related to reduction of NE and 5-HT in the brain. Further, Ji et al. [16, 17] demonstrated that the essential oil from P. frutescens (EOPF) relieved depression-like behaviors in UCMS rats, likely through reversing changes in 5-HT and 5-hydroxyindoleacetic acid (5-HIAA) concentrations. The antidepressant effect of saffron is attributed to the activities of safranal and crocin through the re-uptake of DA, 5-HT, and NE from neurons [18]. In experiments to assess the effects of safranal and crocin on levels of catecholamine and 5-HT in the brain, crocin was demonstrated to be a non-competitive inhibitor of monoamine oxidase (MAO)-A and MAO-B, while safranal did not act on these two isomers [19]. Extract of C. tubulosa can modulate the concentrations of acetate, as well as hexanoic acid, to restore levels of 5-HT in UCMS rats. Oh et al. found that leaf extract from V. bracteatum exerted antidepressant-like effects through regulation of monoaminergic systems and glucocorticoids with neuroprotective effects, alongside antagonism of the 5-HT2A receptor. Furthermore, V. bracteatum exerts neuroprotective effects by decreasing protein levels of MAO-A and serotonin transporter (SERT), and increasing those of tryptophan hydroxylase 2 (TPH2), through upregulation of the extracellular-regulated kinase (ERK)/Akt signaling pathway [20]. Ginsenoside Rb1 and its metabolite, compound K, ameliorate depression-like behaviors in female mice by regulating the 5-HT2A-receptor [21, 22]. Rhodiola has beneficial effects on learning and memory in neonatal rats, through modulation of acetylcholine levels and MAO inhibitory activity [23, 24]. Curcumin has antidepressant effects, which may be related to the inhibition of MAO and enhancement of monoamine neurotransmitters [25]. The antidepressant effects of silymarin may also be due to the decrease of monoamine synthesis (5-HT, NE, etc.) in the hippocampus and cerebral cortex of mice with UCMS-induced depression-like behavior [26, 27].
In addition to the active components, Chinese formula revealed prior activities in regulating neurotransmitters. Ma et al. found that Xiao Chaihu decoction exerts antidepressant effects by increasing the level of monoamine neurotransmitters in mouse hippocampus microdialysis solution, in mice subjected to social isolation, and inhibiting the conversion of 5-HT (5-HIAA/5-HT) [28]. In depressive mice, the expression of monoamine neurotransmitter synthase (TPH2 and TH) is enhanced, while that of SERT is inhibited, and the expression of hippocampal monoamine neurotransmitter synthase reduced [29]. Yang et al. [30] also demonstrated that Chaihu Shugan San can effectively improve the symptoms of depression by increasing 5-HT1A receptor expression in the dentate gyrus of the hippocampus in epileptic rats with depression. Huang et al. [31] focused on the expression of monoamine neurotransmitters and 5-HT receptor subtypes and found that Kaixin Jieyu San could normalize 5-HT and NE levels and regulate the balance of 5-HT1A and 5-HT2A receptor expression in rat brain. Wu et al. [32] showed that Danzhi Xiaoyao San can ameliorate depression-like behaviors in a UCMS-induced rat model. The mechanism underlying the effects of Danzhi Xiaoyao San against depression involves regulation of monoamine levels and amino acid neurotransmitters in the hippocampus. Zhang et al. [33] showed that the antidepressant action of flavonoids in Xiaobuxin Decoction is related to the regulation of extracellular serotonin levels the in central nervous system, and inactivation of the rate of limiting enzyme in the synthesis of 5-HT and tryptophan hydroxylase (Fig. 2).
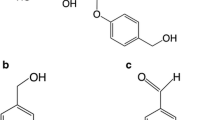
Botanicals and active components for the treatment of depression with the aspect of neurotransmitters. C. tubulosa and silymarin influence synthesis of neurotransmitters; hypericin and saffron affect re-uptake of neurotransmitters by neurons; adhyperforin and Danzhi Xiaoyao San effect on reabsorption of neurotransmitters; V. bracteatum, Kanxin Jieyu San, etc. could antagonize 5-HT receptor; Rhodiola curcumin etc. could balance excitatory and inhibitory neurotransmitters
Hypothalamic–pituitary–adrenal axis
HPA axis is an interactive neuroendocrine unit comprising of the hypothalamus, the pituitary gland, and the adrenal glands. The HPA axis has been revealed in pathophysiology of a series of mood and cognitive disorders [34]. Hyperactivation of HPA axis is thought to be a major cause of major depression [35]. Botanicals and their active components have been extensively investigated regarding their functions in regulating HPA axis in depression. EGb761, catalpol, geniposide, R. glutinosa, Xiao Chaihu decoction, Danzhi Xiaoyao San have been reported to normalize the HPA axis in depression [32, 36,37,38,39]. The anti-depressive effects of ginsenoside Rg1 are mainly through improvement of corticosterone and testosterone levels, modulating protein levels of glucocorticoid receptor (GR) and androgen receptor (AR), and mediating recovery of the HPA axis [40]. Moreover, geniposide can also upregulate GRα expression in the hypothalamic paraventricular nucleus to treat depression-like behaviors [41]. Therefore, GR in hypothalamic paraventricular nucleus is potential target for repair of HPA in depression. Saikosaponin A can also have antidepressant-like effects, by inhibiting hyperactivity of the HPA axis [42]. It can also possible that botanicals and their active components prohibit inflammation, which subsequently eliminates HPA axis hyperactivation [43]. In depression, HPA axis is out of control due to a down-regulation of its negative feedback controls. Corticotrophin is hypersecreted from the hypothalamus and triggers the release of adrenocorticotropic hormone (ACTH) from the pituitary and uncontrollable release of cortisol [44]. Thereafter, cortisol receptors become desensitized leading to increased activity of the pro-inflammatory immune mediators and disturbances in neurotransmitter transmission [45]. The impairment of HPA could also damage neuronal synaptic transmission or neurogenesis, which contributes to depression-like behaviors. For an example, Li et al. [46] reported that Saikosaponin D can counter UCMS-induced depressive behaviors in rats by increasing the phosphorylation of cAMP response element-binding protein (CREB) and promoting brain-derived neurotrophic factor (BDNF) expression, which was mediated by enhancement of HPA axis function and consolidation of hippocampal neurogenesis. Nevertheless, the exact mechanisms underlying the recovery of the HPA axis by botanicals still require clarification.
Inflammation
Evidence is accumulating to show that depression and inflammation are closely connected and may fuel each other [45]. Anti-inflammation has become an important stratagem for treatment of depression. Varieties of botanicals have the potential to anti-inflammation and ameliorate the depression-like behaviors. Astragaloside IV (ASIV), ginsenosides, quercetin, naringenin, saikosaponin A, EGb761, resveratrol, T. lythroides, curcumin, Rhizoma Gastrodiae, Xiaobuxin decoction were well-known for their anti-inflammation in depressive models [21, 22, 36, 47,48,49,50,51,52,53,54,55,56,57].
The antidepressant effects of ASIV are also associated with modulation of neuroinflammation via promotion of peroxisome proliferators-activated receptors γ expression [58]. Quercetin also suppresses oxidative-nitrosamine stress mediated neuroinflammation, via tumor necrosis factor-α (TNF-α) and interleukin 6 (IL-6), and showed neuroprotective effects through the microglial inhibitory pathway [59]. Zhang et al. reported that EGb761 can attenuate depression-like behaviors induced by long-term light avoidance treatment in mice. The underlying mechanism may be associated with inactivation of nuclear factor-κB (NF-κB) signaling pathway-related inflammation in the hippocampus [60]. In a rodent model of CRS-induced depression, P. Ginseng upregulated the Nrf2-heme oxygenase-1 pathway and down-regulates the neuroinflammatory system (MAPK and NF-κB pathways) in the amygdala [61]. Li et al. [62] suggested that Xiaoyao San can alleviate hippocampal neuronal injury and reverse effects measured using the hypertension labyrinth test, through activation of the TNF-α/Janus Kinase 2/Signal Transducer and Activator of Transcription 3 (JAK2/STAT3) pathway in a rat model of chronic immobilization stress-induced anxiety.
Oxidative stress
Causative factors for major depression include inflammation, autoimmune tissue damage and prolonged psychological stress, which lead to oxidative stress [63]. Inflammation and damage of mitochondria generate free radicals. With the accumulation of free radicals or consume of antioxidant system, reactive oxygen species (ROS) react with macromolecules (fatty acid, DNA, protein, etc.) and cause damage to these macromolecules. Brain is one of the most vulnerable organs to the damaging effects of ROS, which may explain ROS involvement in several neuropsychiatric diseases, especially depression [64]. To this end, anti-oxidative stress is also supposed as a treatment stratagem for botanicals. Zhao et al. [36] found that EGb761 can ameliorate lipopolysaccharides (LPS)-induced depression-like behaviors possibly through reduction of oxidative stress. With a strong anti-oxidative ability, ginsenoside Rg3 [65, 66], ASIV [47,48,49], geniposide [67], saikosaponin [46], resveratrol [68], quercetin [50, 51], naringenin [52], Thymelaea lythroides [53], Polygala japonica [69], Rhizoma Gastrodiae [56, 70], silymarin [71,72,73,74] may also ameliorate depression-like behaviors through the anti-oxidative action.
Oxidative stress plays a crucial role in the development of inflammation and anti-oxidants thus could prohibit inflammation. Vice versa, inflammation could also initiate oxidative stress [63]. The interrelationship between inflammation and oxidative stress explain that most botanicals exert anti-depressive action through inhibiting both inflammation and oxidative stress [50, 51, 55, 75] (Fig. 3).
Synaptic plasticity
Synaptic plasticity is one of the most important physiological features of neurons [76]. It is not only related to memory, motor, etc., but also the important determinant of psychiatric disorders. In fact, synaptic regulation has been proposed as one of the most important mechanisms to find antidepressants [77]. Synaptic regulators, such as BDNF/tropomyosin receptor kinase B (TrkB), N-methyl-d-aspartate (NMDA), glutamate, estrogen, insulin, or their downstream signaling pathways, like PI3K/AKT/mTor are crucial therapeutic targets for depression [78]. In recent years, botanicals have attracted extensive attention regarding their functions in synaptic plasticity in depression models. Therefore, synaptic plasticity has been proposed as new insights for screening antidepressants, especially rapid-acting antidepressants [79, 80].
BDNF
Geniposide [67], saikosaponin D [46], resveratrol [81, 82], paeonol [83, 84], ginsenosides [85,86,87], geniposide [67], naringenin [88], Perilla seed oil [89], the water extract of saffron [90], catalpol [37], extract of C. tubulosa [91], Rehmannia glutinosa [38], silymarin [92], Xiaoyao San [93], Chaihu Shugan San [94], Yueju [95], etc. could prevent depression-like behaviors through increasing BDNF expression. At present, our lab also found that curculigoside prevented depression-like activities through increasing hippocampal BDNF level [96]. Interestingly, most of botanicals and active components facilitate BDNF expression through promoting cAMP/PKA/CREB signaling way. Yu et al. revealed that ginsenoside Rg1 has neuroprotective and antidepressant roles through activation of the CREB/BDNF system in the basolateral amygdala and regulation of the synapse-associated factor, miR-134, in a rat model of depression [97]. Botanicals and active components increase BDNF expression, thereafter activating BDNF/TrkB-ERK/Akt to regulate neuronal apoptosis [94], BDNF-Rac1-RhoA pathway to regulate genesis of dendritic spines [83], and BDNF/TrkB/NF-κB pathway to regulate inflammation [84] (Fig. 4).
The synthesis of BDNF and potential downstream involved in the effects of botanicals and active components on depression. In brain, botanicals and active components promote BDNF synthesis through cAMP-PKA-CREB signaling pathway. The downstream of BDNF/TrkB pathway include PI3 K/AKT/mTOR-regulated synaptic plasticity, ERK/AKT-regulated neuronal apoptosis, NF-κB-regulated inflammation and Rac1/RhoA-regulated dendritic spine genesis
NMDA
Accumulating evidence indicates that NMDA receptors are involved in the pathophysiology of depression and implicated as therapeutic targets [98]. In an olfactory bulbectomy model, the antidepressant effects of quercetin act through reinforcement of NMDA receptor inhibition, synthesis of nitric oxide, and reduction of lipid hydroperoxide content in the hippocampus [99]. Xia et al. found that Yueju may confer acute and long-lasting antidepressant effects by favorably modulating the function of NMDA receptors in the hippocampus however, its antidepressant effects were different from those of ketamine, in that Yueju was not influenced by blockade of amino-3-hydroxy-5-methyl-4-isoxazole propionate receptor [100].
Others
Gut flora
Gut flora is the complex community of microorganisms that live in the digestive tracts of humans and animals. Gut flora was not only related to food digestion and gastrointestinal diseases, but also modulates a variety of diseases, including psychiatric disorders [101]. Recent advances point that botanicals and active components regulate gut flora to ameliorate depression-like behaviors, including Xiaoyaosan [102], berberine [103], resveratrol [104], Cistanche tubulosa extract [105]. The gut metabolites, including l-threonine, isoleucine, alanine, serine, tyrosine, and oxidized proline were supposed as the major cause for depression-like behaviors [106, 107]. Gut–brain-axis was also thought to one of the mechanisms for depression [108, 109].
Neurogenesis
Neurogenesis is important way for the recovery of neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s disease, and stroke [110]. Nevertheless, neurogenesis was also reported as a useful method to ameliorate depression by botanicals. Saikosaponin D can counter UCMS-induced depressive behaviors in rats by promoting hippocampal neurogenesis [46]. The aqueous extract of P. japonica can alleviate depression-like behaviors by stimulating neurogenesis in the adult dentate gyrus. Silymarin may also promote neurogenesis in the hippocampus and cerebral cortex of mice with UCMS-induced depression-like behavior [26, 27]. Xiao Chaihu decoction may also promote neurogenesis in CORT-induced depression mouse model [39]. Gao et al. [111] demonstrated that Xiaoyao San reduced depression-like behaviors in a CUMS-induced depression model by improving hippocampal neurogenesis and reversing cerebral blood oxygen level-dependent (BOLD) activation. Pan et al. [112] showed that Kaixin Jieyu San functioned to reduce depressive behavior and improve cerebral hypoperfusion, which may be related to up-regulation of neurogenesis and balance of the fibrinolysis system.
Future prospects
This paper summarizes the therapeutic effects of botanicals on depression, with the aim of providing information about drugs for use in clinical practice. We also concluded and detailed the potential therapeutic targets for botanicals. According to the literatures, botanicals and their active components could fight against depression from the following aspects: neurotransmitters and receptor, inflammation, HPA axis, oxidative stress, synaptic plasticity, and others. These information provide that botanicals have broad therapeutic targets for depression, implicating valuable significance to develop anti-depressants from botanicals.
Medication for depression includes selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, atypical antidepressants, tricyclic antidepressants and monoamine oxidase inhibitors. However, antidepressant medications also come with strong side effects and safety concerns, and withdrawal can be very difficult. Interestingly, some botanicals and active components have the effects to regulate neurotransmitters. As we all know, active components or botanicals are naturally- formed. Toxicity or side effects are relatively mild. Therefore, the active components possess the potential to be developed into antidepressants. Moreover, besides regulating neurotransmitters, some botanicals and active components (like curcumin) also have other pharmacological activities, such as antioxidative, anti-inflammation, and regulating synaptic plasticity. These agents would be more suitable to be developed into antidepressants because of the complex pathogenesis of depression [113]. Interestingly, some prescriptions exhibit superior antidepressive activity through regulating multiple pathways or cascades. For an example, Xiao Chaihu decoction is described in the book, “Treatise on Febrile and Miscellaneous Diseases”, by Zhang Zhongjing. It is composed of Bupleurum chinense, Radix Scutellariae, Ginseng, Pinellia ternata, Glycyrrhiza uralensis, Ginger, and Jujube. The components of the prescription could balance neurotransmitters, ameliorate HPA axis, regulate synaptic plasticity to treat depression [28, 29, 39]. Moreover, some active components from the prescription could also fight against oxidative stress. Therefore, Xiao Chaihu decoction, Xiaoyao San, Chaihu Shugan San, Kaixin Jieyu San, Danzhi Xiaoyao San, Xiaobuxin decoction should attract more attentions to treat depression [28, 32, 33, 62, 112, 114,115,116,117]. On the one hand, the complex pathogenesis of depression would benefit from the multiple components with the corresponding targets. On the other hand, depression is featured by different complications. The prescription of different botanicals would better treat depression based upon the theory of syndrome differentiation and treatment [28].
At present, most of the studies reported BDNF/TrkB signaling pathway as the therapeutic target for depression by the botanicals, which points out the importance of this specific signaling pathway in the pathogenesis of depression [118]. BDNF/TrkB is a crucial synaptic regulator, which not only correlates with memory but also with mood disorders [96, 119]. Therefore, this target should be kept to screen antidepressants. BDNF is a good factor which could nutrition neurons, however with a chronic effect. Depressive-like behaviors, especially depression-related suicide happen fast. Acute antidepressants like ketamine are also urgent or of more significance to fight against depression-related suicide [120]. With the development of photogenetic technology, optical fiber recording technology, neural circuits involved in depression-like behaviors have gradually been discovered [121]. Therefore, we are required to continue seeking the botanicals from the traditional regulators of synaptic. Moreover, these novel techniques should also be applied to screen the potential active components from botanicals which could influence neural circuit involved in depression [122, 123].
Conclusion
As we described above, gut flora is an advanced and hot mechanisms for treatments of brain diseases. From the aspect of gut flora, the holistic view of Chinese medicine could be better reflected. In addition, other changes including epigenetic modification should also be paid more attention, as depression was also supposed as a systemic disease, which is not only related to brain. In the future, with the application of genome-wide investigation techniques, genomics technology, and systems biology, it will be helpful to identify new targets and mechanisms for treatment of depression by verifying different pathways and targets and revealing the biological basis of this condition.
Availability of data and materials
All reported or analyzed data in this review is extracted from published articles.
Abbreviations
- 5-HT:
-
5-hydroxytryptamine
- 5-HIAA:
-
5-hydroxyindoleacetic acid
- ACTH:
-
adrenocorticotropic hormone
- AR:
-
androgen receptor
- ASIV:
-
astragaloside IV
- BOLD:
-
blood oxygen level-dependent
- BDNF:
-
brain-derived neurotrophic factor
- CREB:
-
cAMP responsive element-binding protein
- CRS:
-
chronic restraint stress
- DA:
-
dopamine
- EOPF:
-
essential oil from P. frutescens
- ERK:
-
extracellular-regulated kinase
- GR:
-
glucocorticoid receptor
- HPA:
-
hypothalamic–pituitary–adrenal
- IL-6:
-
interleukin 6
- JAK2/STAT3:
-
Janus Kinase 2/Signal Transducer and Activator of Transcription 3
- LH:
-
learned helpless
- LPS:
-
lipopolysaccharide
- MAO:
-
monoamine oxidase
- MDA:
-
3,4-methylene dioxy amphetamine
- NF-κB:
-
nuclear factor-κB
- NMDA:
-
N-methyl-d-aspartic acid
- OBX:
-
olfactory bulbectomy
- ROS:
-
reactive oxygen species
- NE:
-
norepinephrine
- SERT:
-
serotonin transporter
- SOD:
-
superoxidase dismutase
- TPH2:
-
tryptophan hydroxylase 2
- TNF-α:
-
tumor necrosis factor-α
- TrkB:
-
tropomyosin receptor kinase B
- UCMS:
-
unpredictable chronic mild stress
References
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–602.
Zeng LN, Yang Y, Feng Y, Cui X, Wang R, Hall BJ, et al. The prevalence of depression in menopausal women in China: a meta-analysis of observational studies. J Affect Disord. 2019;256:337–43.
Menard C, Hodes GE, Russo SJ. Pathogenesis of depression: insights from human and rodent studies. Neuroscience. 2016;321:138–62.
Jesulola E, Micalos P, Baguley IJ. Understanding the pathophysiology of depression: from monoamines to the neurogenesis hypothesis model—are we there yet? Behav Brain Res. 2018;341:79–90.
Luca M, Di Mauro M, Di Mauro M, Luca A. Gut microbiota in Alzheimer’s disease, depression, and type 2 diabetes mellitus: the role of oxidative stress. Oxid Med Cell Longev. 2019;2019:4730539.
Park SC. Neurogenesis and antidepressant action. Cell Tissue Res. 2019;377(1):95–106.
Wang Q, Timberlake MA 2nd, Prall K, Dwivedi Y. The recent progress in animal models of depression. Prog Neuropsychopharmacol Biol Psychiatry. 2017;77:99–109.
Gutknecht L, Popp S, Waider J, Sommerlandt FM, Goppner C, Post A, et al. Interaction of brain 5-HT synthesis deficiency, chronic stress and sex differentially impact emotional behavior in Tph2 knockout mice. Psychopharmacology. 2015;232(14):2429–41.
Alvarez C, Vitalis T, Fon EA, Hanoun N, Hamon M, Seif I, et al. Effects of genetic depletion of monoamines on somatosensory cortical development. Neuroscience. 2002;115(3):753–64.
Li HD, Meng XM, Huang C, Zhang L, Lv XW, Li J. Application of herbal traditional chinese medicine in the treatment of acute kidney injury. Front Pharmacol. 2019;10:376.
Fajemiroye JO, da Silva DM, de Oliveira DR, Costa EA. Treatment of anxiety and depression: medicinal plants in retrospect. Fundam Clin Pharmacol. 2016;30(3):198–215.
Wang M, Bi Y, Zeng S, Liu Y, Shao M, Liu K, et al. Modified Xiaoyao San ameliorates depressive-like behaviors by triggering autophagosome formation to alleviate neuronal apoptosis. Biomed Pharmacother. 2019;111:1057–65.
Nutt DJ. Relationship of neurotransmitters to the symptoms of major depressive disorder. J Clin Psychiatry. 2008;69(Suppl E1):4–7.
Tian J, Zhang F, Cheng J, Guo S, Liu P, Wang H. Antidepressant-like activity of adhyperforin, a novel constituent of Hypericum perforatum L. Sci Rep. 2014;4:5632.
Zirak N, Shafiee M, Soltani G, Mirzaei M, Sahebkar A. Hypericum perforatum in the treatment of psychiatric and neurodegenerative disorders: Current evidence and potential mechanisms of action. J Cell Physiol. 2019;234:8496–508.
Ji WW, Li RP, Li M, Wang SY, Zhang X, Niu XX, et al. Antidepressant-like effect of essential oil of Perilla frutescens in a chronic, unpredictable, mild stress-induced depression model mice. Chin J Nat Med. 2014;12(10):753–9.
Ji WW, Wang SY, Ma ZQ, Li RP, Li SS, Xue JS, et al. Effects of perillaldehyde on alternations in serum cytokines and depressive-like behavior in mice after lipopolysaccharide administration. Pharmacol Biochem Behav. 2014;116:1–8.
Rezaee R, Hosseinzadeh H. Safranal: from an aromatic natural product to a rewarding pharmacological agent. Iran J Basic Med Sci. 2013;16(1):12–26.
De Monte C, Carradori S, Chimenti P, Secci D, Mannina L, Alcaro F, et al. New insights into the biological properties of Crocus sativus L.: chemical modifications, human monoamine oxidases inhibition and molecular modeling studies. Eur J Med Chem. 2014;82:164–71.
Oh DR, Kim Y, Choi EJ, Jung MA, Oh KN, Hong JA, et al. Antidepressant-like effects of vaccinium bracteatum in chronic restraint stress mice: functional actions and mechanism explorations. Am J Chin Med. 2018;46(2):357–87.
Zheng X, Liang Y, Kang A, Ma SJ, Xing L, Zhou YY, et al. Peripheral immunomodulation with ginsenoside Rg1 ameliorates neuroinflammation-induced behavioral deficits in rats. Neuroscience. 2014;256:210–22.
Yamada N, Araki H, Yoshimura H. Identification of antidepressant-like ingredients in ginseng root (Panax ginseng C.A. Meyer) using a menopausal depressive-like state in female mice: participation of 5-HT2A receptors. Psychopharmacology. 2011;216(4):589–99.
Panossian A, Wikman G, Sarris J. Rosenroot (Rhodiola rosea): traditional use, chemical composition, pharmacology and clinical efficacy. Phytomedicine. 2010;17(7):481–93.
Vasileva LV, Getova DP, Doncheva ND, Marchev AS, Georgiev MI. Beneficial effect of commercial Rhodiola extract in rats with scopolamine-induced memory impairment on active avoidance. J Ethnopharmacol. 2016;193:586–91.
Kulkarni S, Dhir A, Akula KK. Potentials of curcumin as an antidepressant. Sci World J. 2009;9:1233–41.
Thakare VN, Patil RR, Oswal RJ, Dhakane VD, Aswar MK, Patel BM. Therapeutic potential of silymarin in chronic unpredictable mild stress induced depressive-like behavior in mice. J Psychopharmacol. 2018;32(2):223–35.
Thakare VN, Aswar MK, Kulkarni YP, Patil RR, Patel BM. Silymarin ameliorates experimentally induced depressive like behavior in rats: involvement of hippocampal BDNF signaling, inflammatory cytokines and oxidative stress response. Physiol Behav. 2017;179:401–10.
Ma J, Wang F, Yang J, Dong Y, Su G, Zhang K, et al. Xiaochaihutang attenuates depressive/anxiety-like behaviors of social isolation-reared mice by regulating monoaminergic system, neurogenesis and BDNF expression. J Ethnopharmacol. 2017;208:94–104.
Ma J, Wu CF, Wang F, Yang JY, Dong YX, Su GY, et al. Neurological mechanism of Xiaochaihutang’s antidepressant-like effects to socially isolated adult rats. J Pharm Pharmacol. 2016;68(10):1340–9.
Yang P, Li L, Liu XJ, Cai X, Sun MZ, He JF, et al. Effect of Chaihu-Shugan-San on the mRNA expression of the 5-HT1A receptor and cellular proliferation in the hippocampus of epileptic rats with depression. Exp Ther Med. 2016;11(1):124–30.
Huang SJ, Zhang XH, Wang YY, Pan JH, Cui HM, Fang SP, et al. Effects of Kaixin Jieyu Decoction () on behavior, monoamine neurotransmitter levels, and serotonin receptor subtype expression in the brain of a rat depression model. Chin J Integr Med. 2014;20(4):280–5.
Wu LL, Liu Y, Yan C, Pan Y, Su JF, Wu WK. Antidepressant-like effects of fractions prepared from Danzhi-Xiaoyao-San decoction in rats with chronic unpredictable mild stress: effects on hypothalamic–pituitary–adrenal axis, arginine vasopressin, and neurotransmitters. Evid Based Complement Altern Med. 2016;2016:6784689.
Zhang LM, Wang HL, Zhao N, Chen HX, Li YF, Zhang YZ. Involvement of nitric oxide (NO) signaling pathway in the antidepressant action of the total flavonoids extracted from Xiaobuxin-Tang. Neurosci Lett. 2014;575:31–6.
Bao AM, Swaab DF. The human hypothalamus in mood disorders: the HPA axis in the center. IBRO Rep. 2019;6:45–53.
Juruena MF, Bocharova M, Agustini B, Young AH. Atypical depression and non-atypical depression: is HPA axis function a biomarker? A systematic review. J Affect Disord. 2018;233:45–67.
Zhao Y, Zhang Y, Pan F. The effects of EGb761 on lipopolysaccharide-induced depressive-like behaviour in C57BL/6J mice. Cent Eur J Immunol. 2015;40(1):11–7.
Wang JM, Yang LH, Zhang YY, Niu CL, Cui Y, Feng WS, et al. BDNF and COX-2 participate in anti-depressive mechanisms of catalpol in rats undergoing chronic unpredictable mild stress. Physiol Behav. 2015;151:360–8.
Wang JM, Pei LX, Zhang YY, Cheng YX, Niu CL, Cui Y, et al. Ethanol extract of Rehmannia glutinosa exerts antidepressant-like effects on a rat chronic unpredictable mild stress model by involving monoamines and BDNF. Metab Brain Dis. 2018;33(3):885–92.
Zhang K, Yang J, Wang F, Pan X, Liu J, Wang L, et al. Antidepressant-like effects of Xiaochaihutang in a neuroendocrine mouse model of anxiety/depression. J Ethnopharmacol. 2016;194:674–83.
Mou Z, Huang Q, Chu SF, Zhang MJ, Hu JF, Chen NH, et al. Antidepressive effects of ginsenoside Rg1 via regulation of HPA and HPG axis. Biomed Pharmacother. 2017;92:962–71.
Cai L, Li R, Tang WJ, Meng G, Hu XY, Wu TN. Antidepressant-like effect of geniposide on chronic unpredictable mild stress-induced depressive rats by regulating the hypothalamus–pituitary–adrenal axis. Eur Neuropsychopharmacol. 2015;25(8):1332–41.
Chen XQ, Chen SJ, Liang WN, Wang M, Li CF, Wang SS, et al. Saikosaponin A attenuates perimenopausal depression-like symptoms by chronic unpredictable mild stress. Neurosci Lett. 2018;662:283–9.
Tapp ZM, Godbout JP, Kokiko-Cochran ON. A tilted axis: maladaptive inflammation and HPA axis dysfunction contribute to consequences of TBI. Front Neurol. 2019;10:345.
Menke A. Is the HPA axis as target for depression outdated, or is there a new hope? Front Psychiatry. 2019;10:101.
Brakel K, Hook M. SCI and depression: does inflammation commandeer the brain? Exp Neurol. 2019;320:112977.
Li HY, Zhao YH, Zeng MJ, Fang F, Li M, Qin TT, et al. Saikosaponin D relieves unpredictable chronic mild stress induced depressive-like behavior in rats: involvement of HPA axis and hippocampal neurogenesis. Psychopharmacology. 2017;234(22):3385–94.
Wang HL, Zhou QH, Xu MB, Zhou XL, Zheng GQ. Astragaloside IV for experimental focal cerebral ischemia: preclinical evidence and possible mechanisms. Oxid Med Cell Longev. 2017;2017:8424326.
Zhao Y, Li Q, Zhao W, Li J, Sun Y, Liu K, et al. Astragaloside IV and cycloastragenol are equally effective in inhibition of endoplasmic reticulum stress-associated TXNIP/NLRP3 inflammasome activation in the endothelium. J Ethnopharmacol. 2015;169:210–8.
Costa IM, Lima FOV, Fernandes LCB, Norrara B, Neta FI, Alves RD, et al. Astragaloside IV supplementation promotes a neuroprotective effect in experimental models of neurological disorders: a systematic review. Curr Neuropharmacol. 2019;17:648–65.
Mehta V, Parashar A, Udayabanu M. Quercetin prevents chronic unpredictable stress induced behavioral dysfunction in mice by alleviating hippocampal oxidative and inflammatory stress. Physiol Behav. 2017;171:69–78.
Merzoug S, Toumi ML, Tahraoui A. Quercetin mitigates adriamycin-induced anxiety- and depression-like behaviors, immune dysfunction, and brain oxidative stress in rats. Naunyn-Schmiedeberg’s Arch Pharmacol. 2014;387(10):921–33.
Bansal Y, Singh R, Saroj P, Sodhi RK, Kuhad A. Naringenin protects against oxido-inflammatory aberrations and altered tryptophan metabolism in olfactory bulbectomized-mice model of depression. Toxicol Appl Pharmacol. 2018;355:257–68.
Berkiks I, Boulbaroud S, Garcia-Segura LM, Mesfioui A, Ouichou A, Mouden S, et al. Thymelaea lythroides extract attenuates microglial activation and depressive-like behavior in LPS-induced inflammation in adult male rats. Biomed Pharmacother. 2018;99:655–63.
Lee SM, Bae BS, Park HW, Ahn NG, Cho BG, Cho YL, et al. Characterization of Korean Red Ginseng (Panax ginseng Meyer): history, preparation method, and chemical composition. J Ginseng Res. 2015;39(4):384–91.
Fan C, Song Q, Wang P, Li Y, Yang M, Liu B, et al. Curcumin protects against chronic stress-induced dysregulation of neuroplasticity and depression-like behaviors via suppressing IL-1beta pathway in rats. Neuroscience. 2018;392:92–106.
Zhan HD, Zhou HY, Sui YP, Du XL, Wang WH, Dai L, et al. The rhizome of Gastrodia elata Blume—an ethnopharmacological review. J Ethnopharmacol. 2016;189:361–85.
Wang F, Wang J, An J, Yuan G, Hao X, Zhang Y. Resveratrol ameliorates depressive disorder through the NETRIN1-mediated extracellular signal-regulated kinase/cAMP signal transduction pathway. Mol Med Rep. 2018;17(3):4611–8.
Song MT, Ruan J, Zhang RY, Deng J, Ma ZQ, Ma SP. Astragaloside IV ameliorates neuroinflammation-induced depressive-like behaviors in mice via the PPARgamma/NF-kappaB/NLRP3 inflammasome axis. Acta Pharmacol Sin. 2018;39(10):1559–70.
Rinwa P, Kumar A. Quercetin suppress microglial neuroinflammatory response and induce antidepressent-like effect in olfactory bulbectomized rats. Neuroscience. 2013;255(7):86–98.
McKeage K, Lyseng-Williamson KA. Ginkgo biloba extract EGb 761((R)) in the symptomatic treatment of mild-to-moderate dementia: a profile of its use. Drugs Ther Perspect. 2018;34(8):358–66.
Choi JH, Lee MJ, Jang M, Kim HJ, Lee S, Lee SW, et al. Panax ginseng exerts antidepressant-like effects by suppressing neuroinflammatory response and upregulating nuclear factor erythroid 2 related factor 2 signaling in the amygdala. J Ginseng Res. 2018;42(1):107–15.
Li XJ, Ma QY, Jiang YM, Bai XH, Yan ZY, Liu Q, et al. Xiaoyaosan exerts anxiolytic-like effects by down-regulating the TNF-alpha/JAK2-STAT3 pathway in the rat hippocampus. Sci Rep. 2017;7(1):353.
Lindqvist D, Dhabhar FS, James SJ, Hough CM, Jain FA, Bersani FS, et al. Oxidative stress, inflammation and treatment response in major depression. Psychoneuroendocrinology. 2017;76:197–205.
Czarny P, Wigner P, Galecki P, Sliwinski T. The interplay between inflammation, oxidative stress, DNA damage, DNA repair and mitochondrial dysfunction in depression. Prog Neuropsychopharmacol Biol Psychiatry. 2018;80(Pt C):309–21.
Lee B, Sur B, Park J, Kim SH, Kwon S, Yeom M, et al. Ginsenoside rg3 alleviates lipopolysaccharide-induced learning and memory impairments by anti-inflammatory activity in rats. Biomol Ther. 2013;21(5):381–90.
Wang X, Chen L, Wang T, Jiang X, Zhang H, Li P, et al. Ginsenoside Rg3 antagonizes adriamycin-induced cardiotoxicity by improving endothelial dysfunction from oxidative stress via upregulating the Nrf2-ARE pathway through the activation of akt. Phytomedicine. 2015;22(10):875–84.
Ren L, Tao W, Zhang H, Xue W, Tang J, Wu R, et al. Two standardized fractions of Gardenia jasminoides Ellis with rapid antidepressant effects are differentially associated with BDNF up-regulation in the hippocampus. J Ethnopharmacol. 2016;187:66–73.
Shen J, Xu L, Qu C, Sun H, Zhang J. Resveratrol prevents cognitive deficits induced by chronic unpredictable mild stress: Sirt1/miR-134 signalling pathway regulates CREB/BDNF expression in hippocampus in vivo and in vitro. Behav Brain Res. 2018;349:1–7.
Li C, Fu J, Yang J, Zhang D, Yuan Y, Chen N. Three triterpenoid saponins from the roots of Polygala japonica Houtt. Fitoterapia. 2012;83(7):1184–90.
Zhang JS, Zhou SF, Wang Q, Guo JN, Liang HM, Deng JB, et al. Gastrodin suppresses BACE1 expression under oxidative stress condition via inhibition of the PKR/eIF2alpha pathway in Alzheimer’s disease. Neuroscience. 2016;325:1–9.
Lu CP, Huang CY, Wang SH, Chiu CH, Li LH, Hua KF, et al. Improvement of hyperglycemia in a murine model of insulin resistance and high glucose- and inflammasome-mediated IL-1beta expressions in macrophages by silymarin. Chem Biol Interact. 2018;290:12–8.
Farjad E, Momeni HR. Silymarin ameliorates oxidative stress and enhances antioxidant defense system capacity in cadmium-treated mice. Cell J. 2018;20(3):422–6.
Song X, Zhou B, Zhang P, Lei D, Wang Y, Yao G, et al. Protective effect of silibinin on learning and memory impairment in LPS-treated rats via ROS-BDNF-TrkB pathway. Neurochem Res. 2016;41(7):1662–72.
Kosari-Nasab M, Shokouhi G, Ghorbanihaghjo A, Abbasi MM, Salari AA. Anxiolytic- and antidepressant-like effects of silymarin compared to diazepam and fluoxetine in a mouse model of mild traumatic brain injury. Toxicol Appl Pharmacol. 2018;338:159–73.
An L, Li J, Yu ST, Xue R, Yu NJ, Chen HX, et al. Effects of the total flavonoid extract of Xiaobuxin-Tang on depression-like behavior induced by lipopolysaccharide and proinflammatory cytokine levels in mice. J Ethnopharmacol. 2015;163:83–7.
Zhu G, Briz V, Seinfeld J, Liu Y, Bi X, Baudry M. Calpain-1 deletion impairs mGluR-dependent LTD and fear memory extinction. Sci Rep. 2017;7:42788.
Gerhard DM, Wohleb ES, Duman RS. Emerging treatment mechanisms for depression: focus on glutamate and synaptic plasticity. Drug Discovery Today. 2016;21(3):454–64.
Duman RS, Aghajanian GK, Sanacora G, Krystal JH. Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med. 2016;22(3):238–49.
Duman RS, Shinohara R, Fogaca MV, Hare B. Neurobiology of rapid-acting antidepressants: convergent effects on GluA1-synaptic function. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0400-x.
Chaki S, Fukumoto K. mGlu receptors as potential targets for novel antidepressants. Curr Opin Pharmacol. 2018;38:24–30.
Wang X, Xie Y, Zhang T, Bo S, Bai X, Liu H, et al. Resveratrol reverses chronic restraint stress-induced depression-like behaviour: involvement of BDNF level, ERK phosphorylation and expression of Bcl-2 and Bax in rats. Brain Res Bull. 2016;125:134–43.
Chen WJ, Du JK, Hu X, Yu Q, Li DX, Wang CN, et al. Protective effects of resveratrol on mitochondrial function in the hippocampus improves inflammation-induced depressive-like behavior. Physiol Behav. 2017;182:54–61.
Zhu XL, Chen JJ, Han F, Pan C, Zhuang TT, Cai YF, et al. Novel antidepressant effects of paeonol alleviate neuronal injury with concomitant alterations in BDNF, Rac1 and RhoA levels in chronic unpredictable mild stress rats. Psychopharmacology. 2018;235:2177–91.
Tao W, Wang H, Su Q, Chen Y, Xue W, Xia B, et al. Paeonol attenuates lipopolysaccharide-induced depressive-like behavior in mice. Psychiatry Res. 2016;238:116–21.
You Z, Yao Q, Shen J, Gu Z, Xu H, Wu Z, et al. Antidepressant-like effects of ginsenoside Rg3 in mice via activation of the hippocampal BDNF signaling cascade. J Nat Med. 2017;71(2):367–79.
Xu D, Wang C, Zhao W, Gao S, Cui Z. Antidepressant-like effects of ginsenoside Rg5 in mice: involving of hippocampus BDNF signaling pathway. Neurosci Lett. 2017;645:97–105.
Cui J, Jiang L, Xiang H. Ginsenoside Rb3 exerts antidepressant-like effects in several animal models. J Psychopharmacol. 2012;26(5):697–713.
Yi LT, Liu BB, Li J, Luo L, Liu Q, Geng D, et al. BDNF signaling is necessary for the antidepressant-like effect of naringenin. Prog Neuropsychopharmacol Biol Psychiatry. 2014;48:135–41.
Lee HC, Ko HK, Huang BE, Chu YH, Huang SY. Antidepressant-like effects of Perilla frutescens seed oil during a forced swimming test. Food Funct. 2014;5(5):990–6.
Ghasemi T, Abnous K, Vahdati F, Mehri S, Razavi BM, Hosseinzadeh H. Antidepressant effect of Crocus sativus aqueous extract and its effect on CREB, BDNF, and VGF transcript and protein levels in rat hippocampus. Drug Res. 2015;65(7):337–43.
Lu J, Sheng M, Yao P, Ran C, Liu H, Chen L, et al. High concentration of glucose increases reactive oxygen species generation and apoptosis induced by endoplasmic reticulum stress pathway in rabbit corneal epithelial cells. J Ophthalmol. 2018;2018:8234906.
Song X, Liu B, Cui L, Zhou B, Liu W, Xu F, et al. Silibinin ameliorates anxiety/depression-like behaviors in amyloid beta-treated rats by upregulating BDNF/TrkB pathway and attenuating autophagy in hippocampus. Physiol Behav. 2017;179:487–93.
Ding XF, Liu Y, Yan ZY, Li XJ, Ma QY, Jin ZY, et al. Involvement of normalized glial fibrillary acidic protein expression in the hippocampi in antidepressant-like effects of xiaoyaosan on chronically stressed mice. Evid Based Complement Altern Med. 2017;2017:1960584.
Chen XQ, Li CF, Chen SJ, Liang WN, Wang M, Wang SS, et al. The antidepressant-like effects of Chaihu Shugan San: dependent on the hippocampal BDNF-TrkB-ERK/Akt signaling activation in perimenopausal depression-like rats. Biomed Pharmacother. 2018;105:45–52.
Zou Z, Chen Y, Shen Q, Guo X, Zhang Y, Chen G. Neural plasticity associated with hippocampal PKA-CREB and NMDA signaling is involved in the antidepressant effect of repeated low dose of Yueju pill on chronic mouse model of learned helplessness. Neural Plast. 2017;2017:9160515.
Yang SJ, Song ZJ, Wang XC, Zhang ZR, Wu SB, Zhu GQ. Curculigoside facilitates fear extinction and prevents depression-like behaviors in a mouse learned helplessness model through increasing hippocampal BDNF. Acta Pharmacol Sin. 2019. https://doi.org/10.1038/s41401-019-0238-4.
Yu H, Fan C, Yang L, Yu S, Song Q, Wang P, et al. Ginsenoside Rg1 prevents chronic stress-induced depression-like behaviors and neuronal structural plasticity in rats. Cell Physiol Biochem. 2018;48(6):2470–82.
Williams NR, Schatzberg AF. NMDA antagonist treatment of depression. Curr Opin Neurobiol. 2016;36:112–7.
Holzmann I, da Silva LM, Correa da Silva JA, Steimbach VM, de Souza MM. Antidepressant-like effect of quercetin in bulbectomized mice and involvement of the antioxidant defenses, and the glutamatergic and oxidonitrergic pathways. Pharmacol Biochem Behav. 2015;136:55–63.
Tang J, Xue W, Xia B, Ren L, Tao W, Chen C, et al. Involvement of normalized NMDA receptor and mTOR-related signaling in rapid antidepressant effects of Yueju and ketamine on chronically stressed mice. Sci Rep. 2015;5:13573.
Stower H. Depression linked to the microbiome. Nat Med. 2019;25(3):358.
Zhu HZ, Liang YD, Ma QY, Hao WZ, Li XJ, Wu MS, et al. Xiaoyaosan improves depressive-like behavior in rats with chronic immobilization stress through modulation of the gut microbiota. Biomed Pharmacother. 2019;112:108621.
Zhu X, Sun Y, Zhang C, Liu H. Effects of berberine on a rat model of chronic stress and depression via gastrointestinal tract pathology and gastrointestinal flora profile assays. Mol Med Rep. 2017;15(5):3161–71.
Yu YC, Li J, Zhang M, Pan JC, Yu Y, Zhang JB, et al. Resveratrol improves brain–gut axis by regulation of 5-HT-dependent signaling in the rat model of irritable bowel syndrome. Front Cell Neurosci. 2019;13:30.
Li Y, Peng Y, Ma P, Yang H, Xiong H, Wang M, et al. Antidepressant-like effects of Cistanche tubulosa extract on chronic unpredictable stress rats through restoration of gut microbiota homeostasis. Front Pharmacol. 2018;9:967.
Jianguo L, Xueyang J, Cui W, Changxin W, Xuemei Q. Altered gut metabolome contributes to depression-like behaviors in rats exposed to chronic unpredictable mild stress. Transl Psychiatry. 2019;9(1):40.
Li B, Guo K, Zeng L, Zeng B, Huo R, Luo Y, et al. Metabolite identification in fecal microbiota transplantation mouse livers and combined proteomics with chronic unpredictive mild stress mouse livers. Transl Psychiatry. 2018;8(1):34.
Skonieczna-Zydecka K, Marlicz W, Misera A, Koulaouzidis A, Loniewski I. Microbiome—the missing link in the gut–brain axis: focus on its role in gastrointestinal and mental health. J Clin Med. 2018;7(12):521.
Luo Y, Zeng B, Zeng L, Du X, Li B, Huo R, et al. Gut microbiota regulates mouse behaviors through glucocorticoid receptor pathway genes in the hippocampus. Transl Psychiatry. 2018;8(1):187.
Cheyuo C, Aziz M, Wang P. Neurogenesis in neurodegenerative diseases: role of MFG-E8. Front Neurosci. 2019;13:569.
Gao L, Huang P, Dong Z, Gao T, Huang S, Zhou C, et al. Modified xiaoyaosan (MXYS) exerts anti-depressive effects by rectifying the brain blood oxygen level-dependent fMRI signals and improving hippocampal neurogenesis in mice. Front Pharmacol. 2018;9:1098.
Pan J, Lei X, Wang J, Huang S, Wang Y, Zhang Y, et al. Effects of Kaixinjieyu, a Chinese herbal medicine preparation, on neurovascular unit dysfunction in rats with vascular depression. BMC Complement Altern Med. 2015;15:291.
Zhang YW, Cheng YC. Challenge and prospect of traditional chinese medicine in depression treatment. Front Neurosci. 2019;13:190.
Zhu X, Jing L, Chen C, Shao M, Fan Q, Diao J, et al. Danzhi Xiaoyao San ameliorates depressive-like behavior by shifting toward serotonin via the downregulation of hippocampal indoleamine 2,3-dioxygenase. J Ethnopharmacol. 2015;160:86–93.
Dong XZ, Wang DX, Lu YP, Yuan S, Liu P, Hu Y. Antidepressant effects of Kai-Xin-San in fluoxetine-resistant depression rats. Braz J Med Biol Res. 2017;50(10):e6161.
Liu Q, Sun NN, Wu ZZ, Fan DH, Cao MQ. Chaihu-Shugan-San exerts an antidepressive effect by downregulating miR-124 and releasing inhibition of the MAPK14 and Gria3 signaling pathways. Neural Regen Res. 2018;13(5):837–45.
Yan Z, Jiao H, Ding X, Ma Q, Li X, Pan Q, et al. Xiaoyaosan improves depressive-like behaviors in mice through regulating apelin-APJ system in hypothalamus. Molecules. 2018;23(5):1073.
Zhang JC, Yao W, Hashimoto K. Brain-derived neurotrophic factor (BDNF)-TrkB signaling in inflammation-related depression and potential therapeutic targets. Curr Neuropharmacol. 2016;14(7):721–31.
Zhu G, Li J, He L, Wang X, Hong X. MPTP-induced changes in hippocampal synaptic plasticity and memory are prevented by memantine through the BDNF-TrkB pathway. Br J Pharmacol. 2015;172(9):2354–68.
Cui Y, Hu S, Hu H. Lateral habenular burst firing as a target of the rapid antidepressant effects of ketamine. Trends Neurosci. 2019;42(3):179–91.
Chen M, Bi LL. Optogenetic long-term depression induction in the PVT-CeL circuitry mediates decreased fear memory. Mol Neurobiol. 2018. https://doi.org/10.1007/s12035-018-1407-z.
Cardozo Pinto DF, Lammel S. Hot topic in optogenetics: new implications of in vivo tissue heating. Nat Neurosci. 2019;22:1039–41.
Grosenick L, Shi TC, Gunning FM, Dubin MJ, Downar J, Liston C. Functional and optogenetic approaches to discovering stable subtype-specific circuit mechanisms in depression. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4(6):554–66.
Acknowledgements
Not applicable.
Funding
This research was supported by National Natural Science Foundation of China (81601181, 81673716), Anhui Natural Science Foundation (1808085J15).
Author information
Authors and Affiliations
Contributions
ZR, D-TM and W-ML draft the manuscript. Z-AS revised the manuscript, Z-GQ initiated the topic, and finally confirmed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhang, Z., Deng, T., Wu, M. et al. Botanicals as modulators of depression and mechanisms involved. Chin Med 14, 24 (2019). https://doi.org/10.1186/s13020-019-0246-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13020-019-0246-9