Abstract
Background
The most prevalent cause of peripheral nerve entrapment is carpal tunnel syndrome, which is characterized by compression of the median nerve at the wrist as a result of nearby or localized microvascular interference as well as structural alterations to the median nerve or adjacent tissues. However, no special information regarding the median nerve or its surroundings is provided by clinical examination or electrophysiological testing. The purpose of this study is to evaluate the effectiveness of magnetic resonance neurography (MRN) and ultrasound in identifying changes and abnormalities of the median nerve in carpal tunnel syndrome.
Methods
The twenty-five patients in this study ranged in age from 27 to 63 years old, with a mean age of 47. There were 18 female patients and seven male patients. All patients were sent to the radiology department from the orthopedics, neurology, outpatient clinic, and neurology department, at Ain Shams Hospital, Faculty of Medicine, Ain Shams University. All of the patients had clinically manifested pain along the median nerve distribution, each of the sixteen patients had hand paresthesia, and four had thenar muscle atrophy.
Results
In the current study, Ultrasound exhibits low negative predictive value of 67% and specificity of 67%, but high positive predictive value of 95%, sensitivity of 95%, and overall accuracy of 92%. On the other hand, (MRN) exhibits a low negative predictive value of 60% and a high specificity of 75% in the diagnosis of nerve entrapment, but it also displays a high positive predictive value of 95%, sensitivity of 90%, and overall accuracy of 88%. Regarding the assessment of the recurrence cause and post-surgical evaluation is more reliable by Magnetic Resonance Neurography examination.
Conclusions
Magnetic resonance neurography and high-resolution ultrasonography can be utilized to diagnose patients with median nerve entrapment and patients who cannot be diagnosed electrophysiologically.
MRN is a more accurate method for detecting the exact location of nerve entrapment and evaluating nerve recovery after surgical intervention than nerve conduction studies and electromyography. Additionally, MRN can be used to identify causes that were not previously recognized based on physical examination and electrophysiological tests.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Carpal tunnel syndrome involves median nerve compression (dysfunction) at the wrist due to localized microvascular interference and structural changes in the median nerve or adjacent tissues. Median nerve compression syndrome usually occurs when the carpal tunnel becomes a tight tunnel formed by stiff tissue boundaries due to different etiology. The resultant 'confined space' limits tissue movement and can lead to sustained tissue pressure gradients [1].
As an osteo-fibrous tunnel, the carpal tunnel is a tiny anatomical channel that reroutes the median nerve's path in addition to tendons and blood vessels. Throughout the wrist joint. In order to prevent traumatic damage and dislocation of the structures within the carpal tunnel during joint activity, the roof of this tunnel is composed of focal transverse thickening of the deep fascia, specifically the flexor retinaculum, which is anchored at both ends to osseous prominences. Compared to other places along its path, the median nerve is more susceptible to compression or entrapment in this tunnel [2].
The presence of abnormal tissue inside the narrow space of the carpal tunnel can cause either internal or external compression of the median nerve. Chronic irritation or pressure damage to the median nerve can interfere with the intraneural microvasculature. This can lead to venous congestion, disruption of the blood-nerve barrier, and ischemia from compression of the vasa nervosum. In turn, this can cause epineural edema and elevated endoneural fluid pressure. In the early stages, symptoms might be occasional or even disappear with activity, which would also help the intraneural edema to drain and the intraneural circulation to heal. Chronic nerve constriction may be exacerbated as the disease progresses by the prolonged edema of the epineurium developing into fibrotic changes [3].
When diagnosing carpal tunnel syndrome (medial nerve compression), clinical examination an electrophysiological testing are the main methods used shows the level and severity of the lesion [4].
However these studies don't offer any unique details about the median nerve or its surroundings, which might be helpful for figuring out the reason. By giving precise information about the nature of constricting findings, direct visualization of median nerve abnormalities with imaging modalities may improve the diagnosis and surgical outcomes. This is especially true in cases with confusing clinical pictures or equivocal or contradictory results at the electrophysiological studies [5].
The median nerve's anatomical route, as well as pathological features and changes of compression and entrapment of the median nerve in the carpal tunnel is clear demonstrated on ultrasound imaging [1].
At most centers, magnetic resonance (MR) remains to be the gold standard for evaluating the peripheral nervous system because image acquisition is not operator dependent, as it is in ultrasound (U/S), and interpretation is easier. On the other hand, high-resolution (U/S) imaging is faster, less expensive, and offers distinct benefits over magnetic resonance imaging (MR) in this area, including the capability for increasing resolution and the ability to explore long segments of nerve trunk in a single study and examine tissues in both the static and dynamic states [6].
Recently magnetic resonance neurography (MRN) by using diffusion tensor imaging (DTI) played a useful diagnostic tool in assessing carpal tunnel syndrome The ability to see the median nerve on diffusion tensor imaging and tractography, as well as the automated calculation of the median nerve's diffusion values, can all be helpful in the assessment, diagnosis, and follow up of entrapment, trauma, and regeneration of the median nerve [7].
Methods
Patient demographics
This retrospective study was conducted from February 2021 to November 2023 after obtaining approval from the ethics committee of our university.
Twenty-five patients were included (18 females, 7 males) with age ranges from 27 to 63 years (mean age 47 years). All patients were referred to the radiology department from the outpatient clinic of the orthopedics, neurology, and neurosurgery department, faculty of Medicine Ain Shams Hospital, Ain Shams University. All the patients presented clinically with pain at the distribution of the median nerve, four of them showed wasting of the thenar muscles; while sixteen patients were suffering from hand paresthesia.
Patients were subjected to the following:
-
History taking and clinical provisional diagnosis.
-
Electrophysiological studies (23 patients).
-
Radiological investigations:
-
Ultrasonographic examination.
-
Magnetic resonance neurography (MRN) by using diffusion-tensor imaging (DTI).
Inclusion criteria: All patients with the diagnostic criteria of carpal tunnel syndrome (clinically and by previous nerve conduction velocities), age group (18–60 years old),males and females are included. Exclusion criteria: Patients with contraindications to MRI examination (e.g. pacemaker, metallic implant, severe claustrophobia), Patients with bad general condition needing life support, Patients with wrist congenital abnormalities, Patients with brachial plexus/median nerve paralysis.
Ultrasound examination
The patient was positioned comfortably facing the sonographer throughout every examination, which was conducted using the Philips ultrasonography scanner. The wrist is positioned in hyperflexion. The distal skin crease will be the point at which the sonographic probe is positioned. The ulnar artery is conveniently placed medially in the axial plane, and it can guarantee that the axial pictures maintain a constant orientation. The surface of the flexor tendons must be perpendicular to the sonographic beam. The median nerve is seen as an oval hypoechoic structure situated superficially to the echogenic flexor tendons. Its dimensions, shape, echogenicity, and connection to the retinaculum overlying and underlying tendons are recorded. The median nerve range of motion can be evaluated by moving the finger and wrist.
Interpretation data
Cross-sectional area: was computed at the level of the scaphoid-pisiform proximal carpal tunnel. It usually shouldn't be more than 10 mm. The median nerve's flattening was measured using the flattening ratio, or D1/D2, which is the major to minor axis ratio of the nerve. A typical flattening ratio is less than two. Flexor retinaculum bowing: the distal tunnel (hamate-trapezium level) is where the ligament bulges and can be assessed by U/S. A line is drawn tangential to the hook of the hamate and the tubercle of the trapezium once they have been located. Next, the distance is calculated from this line to the transverse carpal ligament's most anterior portion. Most of the time, the distance is less than 4 mm. Changes in the echotextural properties of the compressed median nerve as the nerve loses its fascicular pattern and becomes uniformly hypoechoic. It is important to record the quantity of synovial fluid as well as the existence or absence of masses.
Magnetic resonance neurography (MRN) examination
All examinations were performed using 1.5 T MAGNET (PHILIPS) at the radiology department of Ain Shams University Hospitals with the patient`s arm on the side of the head resting there in the prone position. The magnet's coronal plane and the hand's dorsum are parallel. Using a circular coil (C 200), the wrist joint was covered, wrapped, and secured with rubber bands. Scout localizers were conducted in sagittal, coronal, and axial planes. DTI (diffusion tractography imaging) was performed using a single-shot spin-echo echo-planar technique with time repetition (TR)/time to echo (TE) = 4600/90 ms. Angle of flip: 90°, field of view: 140 mm size of the matrix: 128 × 128 Avarage number of signals: three A picture free of diffusion gradients will also be recorded, together with data from 35 axial slices of 4 mm thickness without gaps. Diffusion weighting with a b value of 1,000 s/mm2 will be applied in 32 directions. The sequence took seven minutes and forty-nine seconds to complete. A T1-weighted axial sequence was acquired for anatomic reference with TR/TE: 382/20 ms, flip angle: 90°, field of view: 140 mm, and averaged number of signals: 2. After transferring the DTI data to a PC, fiber tracking was performed using manufacturer-supplied software (PRIDE, Philips Medical Systems). After anatomic confirmation of the median nerve tract, the mean Fractional Anisotropy (FA), and mean Apparent Diffusion Coefficient (ADC) values were calculated with the software. The ADC calculated was one-third of the trace of the diffusion tensor. The mean FA and ADC values were obtained from the whole median nerve and focal measurements.
Image analysis
-
Two radiologists with 21 and 12 years of experience evaluated MRI images of patients, correlated to clinical data and laboratory investigations, using a standard clinical picture archiving and diagnostic system workstation.
-
Inter-observers agreement was achieved after correlation with the clinical data and imaging analysis was done successfully.
-
Conventional MRI sequences were evaluated to determine any changes in MN signal intensity and as anatomic reference.
-
A single-shot spin-echo echo-planar DTI sequence was done.
-
Echo- planar post processing diffusion-tractography imaging data were extracted and computed on an offline workstation for evaluation to identify any abnormal signal intensity.
-
Fractional anisotropy (FA) and apparent diffusion coefficient (ADC) maps were calculated from the raw DTI data. Circular regions of interest (ROI) were placed, according to the information from coronal and axial color-coded maps, at the anatomic locations of the median nerve.
-
These locations will be anatomically confirmed using T1 or T2-weighted reference images with an ROI.
-
The distal radioulnar junction (DRUJ) and the pisiform level were the two regions of interests (ROIs) that were put across the median nerve, and quantitative analysis with the average mean value was used to calculate the apparent diffusion coefficient (ADC) and fractional anisotropy (FA) semi-automatically.
-
The average value's apparent diffusion coefficient (ADC) and fractional anisotropy (FA) were determined. The value of FA was decreased and ADC was increased. The cutoff value of FA threshold of 0.47 and ADC threshold of 1.054 × 10−3 mm2/s might be used in the diagnosis of carpal tunnel syndrome.
Statistical analysis
-
Data were input using SPSS (Statistical Package for Social Sciences) version 28 for Windows® (IBM SPSS Inc., Chicago, IL, USA).
-
The mean, standard deviation )SD(, and range were used to present quantitative data. We utilized the student's t-test (t). To evaluate the Ultrasound and MRN for CTS diagnostic sensitivity, specificity, and accuracy, Receiver Operation Characteristic (ROC) curves were built.
-
P-values < 0.05 are considered significant.
Results
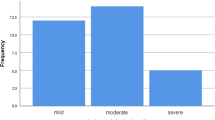
The patients included in the study consisted of 18 females (72%) and seven males (28%), their ages ranging from 27 to 63 years old (mean 47). Patients presented with pain, 64% of cases had paresthesia in addition, 16% showed muscle wasting, while 84% of the studied cases were clinically diagnosed as carpal tunnel syndrome as shown in the Table 1. Regarding the electrophysiological studies results 36% of the studied cases were diagnosed as mild cases 32% were diagnosed as moderate cases and 24% were diagnosed as severe cases as shown in Table 2.
Ultrasound was overall positive in 84% of the analyzed patients, however, 16% of the studied cases were non-positive (negative and false results) as shown in Table 3.
Positive Magnetic resonance neurography (MRN) study represents 92% and 76% of the studied cases as shown in Table 4.
A highly significant association was identified between U/S versus MRN in the diagnosis of nerve entrapment by using the paired Fisher exact test as shown in Table 5.
Ultrasound has a high positive predictive value (95%), sensitivity (95%), and overall accuracy (92%). However, it has a low negative predictive value (67%), and specificity (67%). Magnetic resonance neurography (MRN) has a 95% positive predictive value, 90% sensitivity, and 88% overall accuracy for diagnosing nerve entrapment. However, it has a poor negative predictive value of 60% and a specificity of 75% as shown in Table 6.
Discussion
Carpal tunnel syndrome is a syndrome referring to the clinical presentation of sensory abnormalities (pain, paresthesia, numbness) or motor weakness in the expected distribution of the median nerve [8].
Carpal tunnel syndrome occurs because of anatomic constraints. The carpal tunnel is a common fibro-osseous tunnel that may trigger nerve entrapment syndrome [9].
Carpal tunnel syndrome is caused by abnormalities that compress the median nerve, such as ganglion or amyloidosis. Imaging modalities identify abnormalities causing entrapment, such as masses, anomalous muscles, and fibrous bands, and confirm or support the diagnosis with secondary findings. Secondary signs of carpal tunnel syndrome include the consequences of the entrapment on the median nerve itself, such as focal flattening, proximal swelling, or hypoechogenicity on sonography and abnormal diffusion values (decreased fractional anisotropy and high ADC values) in MRN. In some cases, ultrasound might give an alternate diagnosis by revealing abnormalities other than nerve entrapment that can explain the patient's symptoms (for example, tenosynovitis) [10].
Traditionally, physicians evaluated carpal tunnel syndrome using a clinical history, physical examination, electromyography, nerve conduction studies, and somatosensory evoked potential recordings. However, because such diagnostic tests and investigations do not give specific information about the median nerve and its surrounding tissues, the information they may be insufficient to provide a proper diagnosis. So, clinicians may request for additional imaging modalities for full evaluation. The imaging modality utilized for additional work-up for carpal tunnel syndrome is determined by the anatomic location of the abnormality, the clinician's preference, local availability, and the radiologist experience with each modality [11].
Ismail et al. [12] mentioned that nerve conduction investigations and Electromyography (EMG) are essential for diagnosing carpal tunnel syndrome due to their higher sensitivity than objective physical exams. However, this technique also produces false negative values in about 10% of patients.
According to Bennett and Sears [13], most of the studies accept EMG as the gold standard and attempt to determine the accuracy of other tests compared to the EMG.
Magnetic resonance neurography (MRN) can provide valuable information on nerve diffusion values (FA, ADC) in addition to clinical evaluation and electrophysiological tests. In patients with a diagnosis of median neuropathy, MRN results make the diagnosis of carpal tunnel syndrome of high confidence. As regard to Elkima et al. [14]. M.R.Neurography demonstrates mechanical distortion of nerves using measuring the proton diffusion values and comparing them to the normal known parameters, this feature reveals distortion of nerves at entrapment locations. These findings are typically clinically relevant and should be fully considered in the diagnosis process. They provide reliable diagnoses that complement electrodiagnostic testing in clinical diagnosis. Patients with CTS exhibit a specific pattern of DTI abnormalities in their median nerve. Fibrosis may be causing these functional alterations. MRN may be a viable tool for studying median nerve anatomy in recurrent CTS, since it correlates with nerve conduction velocity giving more accuracy [15].
Although electrodiagnostic techniques are considered the single most accurate diagnostic test, their false negative and false positive rates have been well documented together, nerve conduction studies and electromyography can confirm a CTS diagnosis with 85% sensitivity and specificity. However, the combined 85% and symptoms characteristics provide this accuracy is not optimal. Therefore more accurate diagnostic techniques are needed; MRN by using DTI measurements, the FA, and ADC values may provide helpful complementary diagnostic information [16].
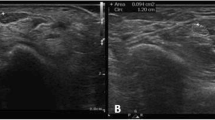
U/S has been used as an easily available method in the diagnosis of musculoskeletal abnormalities in a variety of clinical settings due to the development and continuing improvement of its technology. Also, the combination of high-resolution U/S and color Doppler in carpal tunnel syndrome provides noninvasive accurate means of diagnosis [16] (Figs. 1, 2).
35 years old female patient, complaining of tingling, numbness, and burning pain localized in the left thumb, index, middle finger, and radial half of the ring finger. With the agreement of the two inter-observer radiologist reported that: Magnetic resonance tractography (a–d) images of the left median nerve showing decreased FA values at the distal radioulnar joint (ruj) = 0.36, proximal carpal tunnel = 0.45 and distal carpal tunnel = 0.47( n > 0.47). And increased ADC values at distal radioulnar joint (ruj) = 1.495, proximal carpal tunnel = 1.433 and distal carpal tunnel = 1.518 (n < 1.054 × 10−3 mm2/s). E Transverse U/S scanning shows left median nerve compression with increased hypoechogenicity, flattening ratio < 2, and increased cross-sectional area measuring 14 mm2
32 years old female patient complaining of tingling, numbness, and burning pain localized in the right thumb, index, middle finger, and radial half of the ring finger. After the inter-observation of the two radiologists agree that a–d images show: MRI axial T2 WI’s of the carpal tunnel showing a bilobed median nerve with early bifurcation at the distal end of the carpal tunnel denoting incomplete bifid median nerve. e MRI axial T1 WI’s at the level of hamate bone showing bilobed median nerve with flattening ratio 3.2 (left image) ([m/n], normal ratio less than three) and bowing of the flexor retinaculum with ratio 0.18 (right image)([z/x], normal ratio less than 0.14). f Post-processing diffusion-weighted MR fiber nerve imaging and tractography of the right median nerve showing decreased FA values at the distal radioulnar joint (ruj) = 0.30, proximal carpal tunnel = 0.45, and distal carpal tunnel = 0.32 (n > 0.47). And increased ADC values at distal radioulnar joint (ruj) = 1.268, proximal carpal tunnel = 1.735 and distal carpal tunnel = 1.407 (n < 1.054 × 10−3 mm2/s). g Transverse U/S scanning of the carpal tunnel showing bilobed median nerves (arrows). T: tendon, arrows: median nerve
The use of U/S in clinical practice has become common place, influencing the diagnosis and the clinical management in the symptomatic patient. Current high-end U/S systems equipped with modern linear array transducers in the 5–15 MHz range have given radiologists the opportunity to generate high conspicuity images of most nerves in the body. These instruments permit the delineation of the normal fascicular structure of the median nerve, its vascularity, the recognition of specific and sometimes treatable abnormalities, the differentiation of endoneural and extraneural pathology, the evaluation of the extent of lesions, and the assessment of involved median nerve at follow-up examination [17].
In this study, we are trying to assess the musculoskeletal ultrasound and MRN (DTI) as reliable, noninvasive, recent, and accurate methods that can investigate the median nerve in the carpal tunnel in the upper extremity as the commonest site of nerve entrapment and can give a clue to the etiology of the carpal tunnel syndrome.
To our knowledge, there are a lot of papers that have discussed the musculoskeletal ultrasound but unfortunately, very few papers discussed the role of MRN in the assessment of the median nerve in carpal tunnel syndrome.
According to Omole et al. [18], carpal tunnel syndrome is the most prevalent upper limb entrapment syndrome, with an estimated frequency of 125 × 106 new cases each year. In combination with other investigations, 23 patients (out of 25 cases, 92%) in our research were clinically diagnosed and electrophysiologically confirmed as carpal tunnel syndrome.
Our study consisted of 25 patients, with 18 females and seven men ranging in age from 27 to 63 years old.
All of them were presented clinically with pain at the distribution of the median nerve, where four of them showed wasting of the thenar muscles; while sixteen patients were suffering from hand paresthesia.
Fifteen patients had right-sided lesions, while ten patients had left-sided lesions. In addition, associated medical conditions were appreciated in our cases as five cases were diabetic; and five cases were known to have rheumatoid arthritis.
Nerve conduction studies were done for twenty-three patients confirming nerve conduction abnormalities at the carpal tunnel with nine cases diagnosed as mildly affected, eight cases were moderately affected and six cases were severely affected.
In our study, the criteria used for diagnosis of median nerve entrapment in the carpal tunnel at the upper extremity as regards ultrasound and MRN were as follows:
-
U/S features coinciding with those used by Yoshii Y, Zhao C, and Amadio PC [19]:
-
Increased median nerve cross-section area at the level of maximum nerve swelling along the carpal tunnel directly correlates with electrophysiological signs of CTS.
-
A median nerve ratio > 1.4—cross-section taken at the wrist crease by a normal cross-section taken 12 cm is diagnostic of CTS. The ratio ‘normalizes’ the measurement to the figure/BMI of the individual patient.
-
Loss of fascicular texture and hyperechoic epineurium reflex is a direct sign of median nerve edema.
-
Hypervascularization seen with color Doppler may be a direct sequel of CTS.
-
Bowing of the flexor retinaculum with a distance equal to or more than 4 mm.
-
-
MRN ( DTI) criteria which were coinciding with those used by [20]:-
-
Decreased fractional anisotropy (FA) value less than 0.47
-
Increased ADC value more than 1.054 × 10−3 mm2/s.
-
According to the previously mentioned criteria in our study, a highly significant association was identified between U/S and MRN in the diagnosis of median nerve entrapment with a P value < 0.001, where nineteen patients were diagnosed as true positive in both modalities, while one patient was negative in both modalities and two patients was positive by U/S and negative by MRN.
In addition, while comparing the MRN results to those of the ultrasound; true positive results were present in 76% of the studied cases, and true negative results were seen in 8%, while 4% were false positive and 12% were false negative.
So according to our study, we concluded that MRN findings showed a maximum sensitivity of 80.7% and a maximum specificity of 80%, ultrasound showed high positive predictive value of 89%, sensitivity of 91%, and overall accuracy of 87.5% but showed low negative predictive value of 58% and specificity of 67% in the diagnosis of nerve entrapment in the carpal tunnel.
Our results agreed with those of [21] concluding that a meta-analysis study performed on 32 studies of median nerve DTI at the wrist that the most studied peripheral nerve with DTI is the median nerve because of the potential application to CTS. In their studies, they discovered a decreased FA and increased ADC are the most commonly observed findings in the median nerve compression, the micro-structural changes including disruption of axonal architecture and poor or lost myelination, lead to a decrease of the property of anisotropy which is indicated by increased ADC and decreased FA.
In their study, the use of a cutoff value < 0.48 at the level of pisiform bone gave the best results with 96.67% sensitivity and 90% specificity, which is nearly the same cutoff value.
In their study, the best cutoff value of ADC for diagnosis of CTS is the highest ADC value regardless of the level of measurement was > 1.24 × 10 − 3 mm2/s as a cutoff value, the sensitivity was 96.67% with 100% specificity.
Vo [18] concluded that DTI-related metrics at different locations to find out the best discriminators. In our results, FA was the best predictor of CTS. Moreover, FA was able to distinguish different severity stages. Their cutoff values of FA at CT are similar to those of other published studies, which range from 0.42 to 0.54.
Also Ku et al. [22]. the study included 47 CTS patients identified with clinical examination with positive Tinel's and Phalen's s signs, followed by NCS and electromyography (EMG). Diffusion-weighted MRN (DW-MRN) can immediately detect median nerve lesions in CTS patients' wrists, although other diagnostic methods may raise suspicion. DW-MRN demonstrated significant median nerve hyperintensity, and compression as well as the enhanced flexor retinaculum. The CTS group showed significantly higher median nerve ADC (1.13 × 10–3 mm2/s) compared to the control group (1.06 × 10–3 mm2/s) (p < 0.01). These ADC values might be used to establish ADC cutoffs and/or contralateral comparison.
Bagga et al. [1] the study included 26 patients with CTS and 19 age and 6 matched healthy volunteers as controls, as detailed in the methodology.
Phalen's test was positive in 73.3% of CTS patients, whereas Tinel's sign was positive in 31.1% of afflicted wrists. Nerve conduction investigations revealed that most patients (48.9%) had severe CTS. The study indicated that CSA and relative signal intensity of the median nerve on MRI differed significantly between patients and controls. The cutoff value of CSA > 0.165 cm2 provided the best sensitivity and specificity (91% and 87%, respectively). At three of the four levels, there was a statistically significant difference in median nerve CSA between wrists of CTS patients and controls. The cutoff of CA value is greater than 0.091 cm2 resulted in the best sensitivity (88.9%) and specificity (90.6%). Flexor retinacular bowing, with a cutoff value > 0.139, has a sensitivity of 80% and specificity of 90.6% in detecting carpal tunnel syndrome.
The chi-square test revealed that the median nerve was hypoechoic in texture of the affected CTS`s wrist (p-value < 0.001).
Only one out of 45 wrists with CTS showed increased vascularity on power Doppler, while none of the control group did.
The study examined the cross-sectional area assessed on MRI at 1 cm proximal to the pisiform and USG at the pisiform level, which had the biggest areas under the curve on ROC analysis. The results showed no significant difference (p-value = 0.946). Increased cross-sectional area, whether using US or MR, effectively detects and excludes CTS.
Although increased median nerve signal intensity and retinacular bowing on MRI are statistically significant, they do not reliably predict CTS. However, retinacular bowing assessments in the US giving good diagnosis.
Alkaphoury and Dola [23] concluded that Increased CSA was observed in 30 of the 32 (93.7%) patients, whereas 59.4% of them showed synchronous increases in both the distal nerve flattening and flexor retinaculum bowing indices. In the US, decreased nerve echotextures were observed in 29 of the 32 (90.6%) patients and changes in muscle atrophy were observed in two.
The mean CSA was 14.96 mm2 ± 4.2 (range 4–24 mm2), the mean bowing index was 15.11 ± 4.42 (range 8.32–27.00), and the mean flattening index was 2.97 ± 0.69 (range 1.54–4.20).
Also [24] The study consisted of 46 patients, with an average age of 70 years and a range of 16–91 years. In 42 individuals with CTS, US results were typical of CTS, including a significant rise in CSA and CSA ratio.
In the CTS group, there were 25 men and 17 women. Twenty-seven were right hands, while 15 were left. The mean CSA value was 21 mm2, with a range of 14 to 36 mm2. The average CSA ratio was 2.9. The average diameter ratio was 2.03.
According to these results, MRN and high-resolution ultrasonography can be used as an ancillary method to the electrophysiologic tests in diagnosing patients in whom the median nerve is compressed at the carpal tunnel. Also, those patients who cannot be diagnosed electrophysiologically, because of the false negativity of the NCS will be able to be diagnosed.
MRN is a more accurate tool than NCS or EMG for diagnosing the specific location of nerve entrapment and measuring nerve recovery after surgery. Furthermore, when symptoms persist despite the interventions, MRN can be utilized to confirm the diagnostic criteria and reveal diseases that were previously unknown on physical examination and NCS/EMG.
Conclusions
In clinical practice, nerve conduction investigations remain the most reliable way to diagnose carpal tunnel syndrome. However, magnetic resonance neurography is one of the most important and recent imaging modalities which has an exceeding role in the diagnosis of carpal tunnel syndrome due to its effective ability in tracking the median nerve and has a great role in following up carpal tunnel syndrome patients post operatively as it was more accurate in assessing the respond of the nerve fibers after removal the cause of the compression.
Also, a high-resolution ultrasound examination is an effective, satisfactory modality in the diagnosis of median nerve entrapment syndrome within the carpal tunnel. Its low cost, minimal time requirements, and general availability favor its use as the initial study in evaluating the median nerve entrapment syndrome. Sonography has the additional advantage of being a dynamic study. Yet, it is still operator dependent.
We recommend increasing the sample size with longer observation, and postoperative follow-up, for further inspecting the significance of diffusion indices in evaluating CTS.
Availability of data and materials
All are available with the authors upon request.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- ADC:
-
Apparent diffusion coefficient
- FA:
-
Fractional anisotropy
- CTS:
-
Carpal tunnel syndrome
- CSA:
-
Cross-sectional area
- DWI:
-
Diffusion-weighted image
- DRUJ:
-
Distal radioulnar joint
- EMG:
-
Electromyography
- MN:
-
Median nerve
- NCS:
-
Nerve conduction studies
- ROI:
-
Region of interest
- SIR:
-
Signal intensity ratio
- TE:
-
Time to echo
- SD:
-
Standard deviation
- FP:
-
False positive
- FN:
-
False negative
- NPV:
-
Negative predictive value
References
Bagga B, Sinha A, Khandelwal N, Modi M, Ahuja CK, Sharma R (2020) Comparison of magnetic resonance imaging and ultrasonography in diagnosing and grading carpal tunnel syndrome: a prospective study. Curr Probl Diagn Radiol 49(2):102–115. https://doi.org/10.1067/j.cpradiol.2019.04.004
Ibrahim I, Khan WS, Goddard N, Smitham P (2012) Carpal tunnel syndrome: a review of the recent literature. Open Orthop J 6:69–76
Chen IJ, Chang KV, Lou YM, Wu WT, Özçakar L (2020) Can ultrasound imaging be used for the diagnosis of carpal tunnel syndrome in diabetic patients? A systemic review and network meta-analysis. J Neurol 267(7):1887–1895. https://doi.org/10.1007/s00415-019-09254-8
Elnady B, Rageh EM, Ekhouly T (2019) Diagnostic potential of ultrasound in carpal tunnel syndrome with different etiologies: correlation of sonographic median nerve measures with electrodiagnostic severity. BMC Musculoskelet Disord 20:634
Ghasemi M, Masoumi S, Ansari B, Fereidan-Esfahani M, Mousavi SM (2017) Determination of cut-off point of cross-sectional area of median nerve at the wrist for diagnosing carpal tunnel syndrome. Iran J Neurol 16:164–167
Möller I, Miguel M, Bong D, Zaottini F, Martinoli C (2018) The peripheral nerves: An update on ultrasound and magnetic resonance imaging. Clin Exp Rheumatol 114(5):145–158
Edward R, Abdelalim AM, Ashour AS, Afifi L, Al-Athwar A (2020) A study of diffusion tensor imaging of median nerve in diabetic peripheral neuropathy. Egypt J Neurol Psychiatry Neurosurg 56:42
Mangi MD, Zadow S, Lim W (2022) Nerve entrapment syndromes of the upper limb: a pictorial review. Insights Imaging 13:166. https://doi.org/10.1186/s13244-022-01305-5
Preisner F, Behnisch R, Schwehr V, Godel T, Schwarz D, Foesleitner O, Bäumer P, Heiland S, Bendszus M, Kronlage M (2022) Quantitative MR-Neurography at 30T:Inter-Scanner Reproducibility. Front Neurosci 16:817316. https://doi.org/10.3389/fnins.2022.817316
Schwabl C, Schmidle G, Kaiser P, Drakonaki E, Taljanovic MS, Klauser AS (2023) Nerve entrapment syndromes: detection by ultrasound. Ultrasonography 42(3):376–387. https://doi.org/10.14366/usg.22186
Daniels SP, De Tolla JE, Azad A, Petchprapa CN (2022) Nerve Imaging in the Wrist. Semin Musculosk Radiol 26(2):140–152. https://doi.org/10.1055/s-0042-1742393
Ismail MM, Hamdy NA, Yehia MA, Saleh RN, Desouky TM, Abdelkader M (2023) Neurophysiological evaluation of patients with carpal tunnel syndrome using different diagnostic methods. Minia J Med Res 34(3):11–18. https://doi.org/10.21608/mjmr.2023.211598.1397
Bennett OM, Sears ED (2023) The impact of reference standard on diagnostic testing characteristics for carpal tunnel syndrome: a systematic review. Plast Reconstruct Surg Glob Open 11(7):5067. https://doi.org/10.1097/gox.0000000000005067
Elkima SEAA, Abdelaziz AA, Alsergany MA, Nagy HA (2023) Diagnostic value of diffusion-weighted MRI using apparent diffusion coefficient (ADC) in evaluation of median nerve in carpal tunnel syndrome. Egypt J Radiol Nucl Med 54(1):46. https://doi.org/10.1186/s43055-023-00996-0
Vo NQ, Hoang NT, Nguyen DD, Nguyen THD, Le TB, Le NTN, Nguyen TT (2022) Quantitative parameters of diffusion tensor imaging in the evaluation of carpal tunnel syndrome. Quant Imaging Med Surg 12(6):1
Nalbant M, Yemişci OÜ, Özen S, Tezcan Ş (2022) Ultrasonographic and electrophysiological outcomes of carpal tunnel syndrome treated with low-level laser therapy: A double-blind, prospective, randomized, sham-controlled study. Arch Rheumatol 37(1):19–30. https://doi.org/10.4697/ArchRheumatol.2022.8605
Landau AJ, Parameswaran P, Fresco R, Simon L, Dy CJ, Brogan DM (2022) Systematic review of the use of power doppler ultrasound in the imaging of peripheral nerve compression neuropathy. Plast Reconstruct Surg 149(1):1
Omole AE, Awosika A, Khan A, Adabanya U, Anand N, Patel T, Edmondson CK, Fakoya AO, Millis RM (2023) An integrated review of carpal tunnel syndrome: new insights to an old problem. Cureus 15(6):1. https://doi.org/10.7759/cureus.40145
Yoshii Y, Zhao C, Amadio PC (2020) Recent advances in ultrasound diagnosis of carpal tunnel syndrome. Diagnostics (Basel) 10(8):596. https://doi.org/10.3390/diagnostics10080596
Pušnik L, Serša I, Umek N, Cvetko E, Snoj Ž (2023) Correlation between diffusion tensor indices and fascicular morphometric parameters of peripheral nerve. Front Physiol 14:1. https://doi.org/10.3389/fphys.2023.1070227
Mohamed Abdullah M, Kamal T, Shalan A, Naby SA, S. (2023) Added value of morphological and functional magnetic resonance neurography in assessment of carpal tunnel syndrome in correlation with nerve conduction studies. Benha Med J 40(2):553–565. https://doi.org/10.2108/bmfj.2023.219205.1844
Ku V, Cox C, Mikeska A, MacKay B (2021) Magnetic resonance neurography for evaluation of peripheral nerves. J Brach Plexus Peripher Nerve Injury 16(1):E17–E23. https://doi.org/10.1055/s-0041-1729176
Alkaphoury MG, Dola EF (2024) Ultrasound and magnetic resonance imaging neurography assessment of diagnostic criteria in patients with carpal tunnel syndrome using electrophysiological tests as gold standard: a prospective study. SAGE Open Med 12:1. https://doi.org/10.1177/20503121231218889
Iyer V (2019) Role of ultrasonography in severe distal median nerve neuropathy. J Clin Neurophysiol 36(4):312–315. https://doi.org/10.1097/WNP.0000000000000590
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
All authors reviewed and approved the final paper before submission. NMH provided the research idea, secured the original figures and data, reduced impediments, connected the study concept and design, and played a key role in the analysis. BSF gathered and analyzed data throughout the writing process.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee of Ain Shams University evaluated and approved the study.
Consent for publication
These cases were published with written consent.
Competing interests
The authors have declared that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Megalaa, B.S., Ghany, A.F.A.E., Hetta, W.M. et al. Role of ultrasound and magnetic resonance neurography in the detection of median nerve abnormalities in carpal tunnel syndrome. Egypt J Radiol Nucl Med 55, 173 (2024). https://doi.org/10.1186/s43055-024-01345-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01345-5