Abstract
Impaired wound healing, imbalanced fibroblast proliferation, and extracellular matrix synthesis are associated with aberrant scarring. The impact of impaired wound healing can be tremendous due to physical restrictions, high recurrence rates, stigmatization, and secondary infections in chronic wounds. It is therefore essential to develop alternative treatment regimens to those that are currently used. The highly diverse influence of water-filtered infrared-A (wIRA) on cell metabolism, bacterial colonisation, wound healing, and its high tissue penetration – reaching the subcutis without inducing harmful increases in skin surface temperature or pain – led to the investigation of the influence of the spectral and thermal component of wIRA on normal and keloid fibroblasts in vitro. Data show the potential value of the spectral and the thermal component of wIRA as an adjuvant therapy for aberrant scarring due to its differential influence on the proliferation, migration, and collagen type I synthesis of normal and keloid fibroblasts. The observed aspects in the context of hypertrophic scar treatment need to be evaluated in further basic research and clinical studies.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
1 Introduction
“Wound healing” describes a complex process which consists of tissue homeostasis, inflammation, proliferation, and scar-remodelling [1]. Development of chronic wounds, chronic inflammation, and aberrant scarring are the consequences of an imbalanced cell proliferation, cytokine secretion, and extracellular matrix synthesis and degradation. There are two types of aberrant scarring: hypertrophic scars and keloid scars. In contrast to hypertrophic scarring, keloid development is considered to have a genetic background, and scarring is not limited to the initial defect area. Physical restrictions, stigmatization, and chronic wounds are only some aspects that have a high impact on patients´ lives. Although a broad variety of treatment regimens, such as conservative approaches (e.g., compression therapy), invasive approaches (e.g., cryotherapy, surgical procedures, and laser ablation), and combination therapies using pharmacological agents (e.g., glucocorticoids, chemotherapeutics and immunomodulators) are used, a high recurrence rate of keloids is observed [2]. Consequently, there remains a great need to develop alternative therapeutic options.
One of these options is the application of water-filtered infrared-A (wIRA) irradiation which is considered by the European Society for Hyperthermic Oncology (ESHO) to be an ‘external non-contacting IR heating system’. wIRA is known for its high tissue penetration, reaching the subcutis without inducing harmful increases in skin surface temperature or pain. Clinical, pre-clinical, and in vitro studies have demonstrated its capacity to (a) influence cell metabolism, angiogenesis, thermoregulation, local blood flow, oxygen partial pressures, pain management, bacterial colonisation, total wound infection, and to (b) shorten healing time of acute and chronic wounds [1]. These aspects, together with a potential influence on collagen synthesis, support wIRA as being a promising therapeutic approach to treat hypertrophic scars, in particular keloids. In this study, we have compartmentalised and investigated the thermal and spectral components of wIRA separately and in combination with water bath heating.
2 Methods and Results
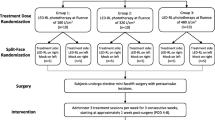
Aberrant scarring, sometimes solely initiated by micro-fissures, is characterised by an imbalanced wound healing. The treatment of aberrant scarring often results in secondary wounds, for example, after injection or surgical removal of scar tissue and might, therefore, trigger a recurrence. We have been interested in how wIRA irradiation may influence different aspects of aberrant scars, such as cell proliferation, migration, metabolic activity, and the synthesis and degradation of extracellular matrix proteins, specifically collagen type I. Our studies have focussed on investigating the influence of the spectral and thermal components of wIRA irradiation. Therefore, cells were either kept light-protected or were irradiated with 360 J/cm2 (780 nm–1400 nm; 106 mW/cm2) using a wIRA radiator (Hydrosun® 750, Hydrosun Medizintechnik, Müllheim, Germany) equipped with an optical filter eliminating wavelengths <780 nm, for 56–120 min. During irradiation, samples were kept in a temperature-controlled water bath at 37–46 °C (Fig. 16.1).
2.1 Morphological Changes and Metabolic Activity
When considering potential new treatment regimens, investigations on cellular morphology, viability, and cytotoxicity are prerequisites. The rhomboid morphology of normal and keloid fibroblasts was not altered neither by the spectral component of wIRA nor by water bath heating up to 44 °C (Fig. 16.1). Independent of the fibroblast origin, the rhomboid cell shape changed to a more spherical shape after light-protected exposure to 46 °C. Fibroblast cells treated with the spectral component of wIRA at 46 °C were significantly less spherical. The lack of spherical cell morphology in the co-treated cultures might be associated with reverse pro-apoptotic effects, for example, by upregulating Bcl-2 (data not shown). The spectral wIRA component might antagonize mitochondrial membrane destabilisation, cytochrome C release, and consequently downregulate anoikis, a cell adhesion-dependent associated programmed cell death which is known to be induced (a) intrinsically through mitochondrial membrane permeabilization, as well as (b) extrinsically via death receptor signalling.
A moderate, exclusively temperature-dependent reduction of the metabolic activity without inducing cytotoxic effects was observed in all fibroblasts. Comparable effects have been observed after application of pulsed or prolonged hyperthermia by laser or convective heat [3, 4]. Therefore, it is unlikely that the in vitro observed reduced metabolic activity is clinically relevant.
2.2 Wound Closure
In normal fibroblast cultures, treatment is conducted with the spectral component of wIRA at 37 °C stimulated proliferation, as indicated by an increased incorporation of a thymidine analogue during mitosis, and an increase in the binucleate index, cytokinesis, and total cell number. Photo-documentation of the respective scratch closure additionally showed that the induced scratch closed faster in the wIRA at 37 °C exposed cultures compared to sham-irradiated cultures. These results indicated that the spectral component of wIRA promoted proliferation and migration without inducing pro-inflammatory cytokines and had only a moderate effect on the production of reactive oxygen species (ROS) [5]. Thereafter, we investigated whether scratch closure for normal and keloid fibroblasts differed. In a previous study we observed that wIRA differentially influenced normal and keloid fibroblasts under hyperthermic conditions [6]. Scratch closure in cultures exposed to 37 °C wIRA and 46 °C wIRA occurred earlier than that in the respective non-irradiated cultures (37 °C and 46 °C). There was a quantitative difference in scratch closure at 37 °C and 46 °C between the light-protected/non-irradiated (open symbols) and the cultures treated with the spectral wIRA-component only (closed symbols). Normal fibroblast cultures (Fig. 16.2a) treated with the spectral wIRA component at 37 °C exhibited a significantly faster area closure after 6 h and 12 h compared to the non-irradiated cultures, whereas such an effect could not be observed in keloid cultures (Fig. 16.2b). Under extreme hyperthermia conditions (wIRA at 46 °C), the spectral component of wIRA induced a significant increase in the scratch area closure compared to the respective light-protected cultures in normal or keloid fibroblast cultures. Direct comparison of the scratch closure capacity upon wIRA at 46 °C in normal and keloid fibroblasts (Fig. 16.2c) revealed that normal fibroblasts covered a significantly larger scratch area between 6 h and 36 h after scratch induction than keloid fibroblasts. Thereafter, almost the complete area was covered in both experimental conditions.
Scratch closure of normal and keloid fibroblasts depending on wIRA-irradiation. Quantitative analysis of the wound closure of normal fibroblasts (a) and keloid fibroblasts (b). Comparison of scratch closure of normal (cross) and keloid (dot) fibroblasts after wIRA irradiation at 46 °C (c). * p ≤ 0.05, ** p ≤ 0.01 compared to non-irradiated control cultures (a, b) *** p ≤ 0.001 compared to irradiated normal fibroblast cultures (c)
In the studies presented, wound-healing velocity was likewise influenced after treatment with the spectral component of wIRA under hyperthermic (40–46 °C) and normothermic conditions (37 °C). It has previously been reported that irradiation with different irradiances (doses) of low-intensity red light (dominant wavelength 628 nm) upregulates genes involved in proliferation [7]. Another indicator supporting wIRA treatment is that under various thermal conditions, wavelengths of the NIR spectrum and LLLT influence mitochondrial mass, mitochondrial membrane potential, and moderate ROS-induction, all of which are likely responsible for proliferation and the induction of migration [5, 8].
2.3 Extracellular Matrix Synthesis
As described above, the thermal component of the wIRA irradiation was eliminated and all applied thermal stimuli were exclusively administered using a temperature-controlled water bath. This enabled the influence of the spectral component of wIRA irradiation to be separated from its thermal component. As described in Sect. 16.2.2 that normal fibroblasts close an artificial wound faster than keloid fibroblasts after treatment with the spectral component of wIRA, it is also important to validate the synthesis of the extracellular matrix, which is closely balanced under physiological conditions. Monitoring collagen synthesis is an important criterion for developing a possible keloid therapy. As a consequence, we assessed the dependence of collagen type I synthesis in normal and keloid fibroblast on the spectral and/or the thermal components of wIRA [6]. As depicted in Fig. 16.3, keloid fibroblasts (black columns) can be clearly distinguished from normal fibroblasts (white columns) due to higher collagen synthesis. Whereas collagen type I synthesis of normal fibroblasts was neither influenced by the spectral component of wIRA nor by increasing the water-bath temperature during treatment from 37 °C up to 44 °C; a distinct decrease of the collagen type I concentration was observed in keloid fibroblast cultures that had been treated at 44 °C. At the latter temperature, there was no difference between the hyperthermia treatment (44 °C) and the co-treatment (wIRA at 44 °C). Increasing the water-bath temperature to 46 °C significantly reduced collagen type-I synthesis in normal and keloid fibroblasts (Fig. 16.3). The relative reduction of collagen type I synthesis of keloid fibroblasts after treatment at 46 °C was four times higher than the observed reduction in normal fibroblasts. Collagen type I synthesis in cells exposed to wIRA at 46 °C was partially reconstituted. The restored collagen type I synthesis remained proportionally lower than the collagen type I synthesis of the normal fibroblasts under these conditions.
Further investigations focussing on transforming growth factor-β1 (TGF-β1), a well-known promoter of collagen synthesis, revealed a temperature-related reduction of TGF-β1 secretion in normal and in keloid fibroblasts. In keloid fibroblasts, this temperature-induced reduction in secretion was completely restored in cultures exposed to wIRA at 46 °C. In our studies, we observed neither a temperature nor a spectral wIRA component-related effect on the secretion of the matrix metalloproteinase-1 (MMP-1).
3 Conclusions
The rationale for the treatment of hypertrophic scars/keloids is (a) to increase the catabolism of extracellular matrix proteins and their de novo synthesis and (b) to inhibit cells, especially fibroblasts, that are responsible for their synthesis in order to regain a physiological equilibrium. The results presented indicate that applying moderate to extreme hyperthermia with wIRA qualifies as a potential approach due to its capacity to inhibit TGF-β1 secretion. This in turn influences signal transduction pathways which impact migration, proliferation, and collagen type I synthesis, such as p38, MAPK. The wIRA-related rescue of the TGF-β1 secretion in keloid cells after incubation at high temperatures is not able to neutralize the temperature-induced reduction of collagen type I synthesis. Although the wIRA-related upregulation of TGF-β1 is beneficial and desirable during wound healing [9], its relevance in the clinical application in keloid treatment needs to be further validated. Direct comparison of the wound/scratch closure capacity between normal and keloid fibroblasts that had been wIRA irradiated under hyperthermic conditions showed that normal fibroblasts reduced the remaining scratch/wound area faster than keloid fibroblasts. Therefore, the data presented herein suggest both the spectral and thermal components of wIRA as potential adjuvant therapy options for promoting normal wound healing after keloid surgery due to the observed differential responses of the fibroblast species in the wound scratch assay. The therapeutic benefits of wIRA involve an increased proliferation of normal fibroblasts, a moderate induction of ROS, stimulation of cell migration, and the low risk of thermal tissue damage.
4 Outlook
To further elucidate the impact of the thermal and the spectral component of wIRA as an anti-fibrotic therapy regimen, it is advisable to employ more complex systems such as tissue cultured skin equivalents [10], which might be adapted to represent scar tissue to monitor extracellular matrix structure and morphological and biochemical properties of the cells. Additionally, ex vivo explants and long-term analysis of the above-described treatment regimen are planned in order to further discriminate between the relevant factors in normal and diseased cells. Considering a broad experience concerning the development of phytochemically based photodynamic treatment regimens, we are currently investigating the influence of photosensitizers in combination with wIRA irradiation on benign keloid fibroblasts, other neoblastic cells, and their normal counterparts. These studies are focussing on the signalling pathways that are involved in proliferation, migration, apoptosis, anoikis, cell cycle progress, and autophagy.
Abbreviations
- Bcl-2:
-
B-cell lymphoma 2
- LLLT:
-
Low-level-light therapy
- MMP 1:
-
Matrix metalloproteinase 1
- NIR:
-
Near infrared
- P1NP:
-
N-terminal domain of procollagen type1
- TGF-β1:
-
Transforming growth factor β1
- wIRA:
-
Water-filtered infrared-A
References
Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res. 2009;37(5):1528–42. https://doi.org/10.1177/147323000903700531.
Danielsen PL, Rea SM, Wood FM, et al. Verapamil is less effective than triamcinolone for prevention of keloid scar recurrence after excision in a randomized controlled trial. Acta Derm Venereol. 2016;96(6):774–8. https://doi.org/10.2340/00015555-2384.
Dams SD, de Liefde-van BM, Nuijs AM, et al. Pulsed heat shocks enhance procollagen type I and procollagen type III expression in human dermal fibroblasts. Skin Res Technol. 2010;16(3):354–64. https://doi.org/10.1111/j.1600-0846.2010.00441.x.
Kalamida D, Karagounis IV, Mitrakas A, et al. Fever-range hyperthermia vs. hypothermia effect on cancer cell viability, proliferation and HSP90 expression. PLoS One. 2015;10:e0116021. https://doi.org/10.1371/journal.pone.0116021.
König A, Missalla S, Valesky EM, et al. Effect of near-infrared photobiomodulation therapy in a cellular wound healing model. Photodermatol Photoimmunol Photomed. 2018;34(4):279–83. https://doi.org/10.1111/phpp.12390.
Zöller N, König A, Butting M, et al. Water-filtered near-infrared influences collagen synthesis of keloid-fibroblasts in contrast to normal foreskin fibroblasts. J Photochem Photobiol B. 2016;163:194–202. https://doi.org/10.1016/j.jphotobiol.2016.08.020.
Zhang Y, Song S, Fong CC, et al. cDNA microarray analysis of gene expression profiles in human fibroblast cells irradiated with red light. J Invest Dermatol. 2003;120(5):849–57. https://doi.org/10.1046/j.1523-1747.2003.12133.x.
Shingyochi Y, Kanazawa S, Tajima S, et al. Low-level carbon dioxide laser promotes fibroblast proliferation and migration through activation of Akt, ERK, and JNK. PLoS One. 2017;12(1):e0168937. https://doi.org/10.1371/journal.pone.0168937.
Danno K, Mori N, Toda K, et al. Near-infrared irradiation stimulates cutaneous wound repair: laboratory experiments on possible mechanisms. Photodermatol Photoimmunol Photomed. 2001;17(6):261–5. https://doi.org/10.1034/j.1600-0781.2001.170603.x.
Zöller NN, Kippenberger S, Thaçi D, et al. Evaluation of beneficial and adverse effects of glucocorticoids on a newly developed full-thickness skin model. Toxicol In Vitro. 2008;22(3):747–59. https://doi.org/10.1016/j.tiv.2007.11.022.
Acknowledgments
Dr. Anke König, Dr. Gabi Reichenbach, Anne Jeute, and Svenja Missalla contributed to the results described in this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Zöller, N., Kippenberger, S. (2022). Influence of wIRA Irradiation on Wound Healing: Focus on the Dermis. In: Vaupel, P. (eds) Water-filtered Infrared A (wIRA) Irradiation. Springer, Cham. https://doi.org/10.1007/978-3-030-92880-3_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-92880-3_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-92879-7
Online ISBN: 978-3-030-92880-3
eBook Packages: MedicineMedicine (R0)