Abstract
wIRA has been shown to reduce chlamydial infections in vitro and in vivo and might therefore offer an innovative therapeutic approach for fighting trachoma. However, since the eye is a highly temperature- and radiation-sensitive organ, a safety assessment of the ocular structures affected by wIRA treatment is required to establish wIRA as a potentially successful treatment option for clinical application. A prerequisite for this is to demonstrate that wIRA does not have adverse side-effects such as inducing a non-physiological temperature increase which causes cell stress and damage to ocular tissues and which, in turn, is ultimately associated with impaired vision. Likewise, the potential negative impact of non-thermal photochemical effects of wIRA irradiation needs to be investigated. Data from our ex vivo studies in pig and mouse models, as well as in vivo data in a guinea pig model, provide good evidence for the safe use of wIRA to treat chlamydial infections. These studies have excluded a non-physiological temperature rise as well as the activation of heat and stress-induced proteins after wIRA irradiation with therapy-relevant irradiances. Nevertheless, additional detailed in vitro and in vivo studies are needed to further advance the clinical use of wIRA.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 The Eye as a Highly Sensitive Structure for Thermal Interventions
Temperature is of utmost importance for all biological functions, with temperature changes in tissues influencing the kinetics of biological processes and consequently slowing or accelerating metabolism. Non-physiological increases in temperature in tissues can result in protein denaturation and cell death and thus contribute to the onset of pathological changes.
Eyes are considered to be the most vulnerable to even small temperature changes for the following reasons. Some of the inner posterior parts of the eye lack sufficient blood flow for the removal of excess heat, whereas the anterior part is only temporarily covered by the eyelid as a protective skin layer [1]. Hence, environmental conditions such as humidity, airflow and thermal radiation can have a massive impact on ocular temperature and contribute to pathological changes in the eye. For this reason, the safety of medical treatments which induce temperature changes in the eye, including water filtered infrared-A (wIRA) irradiation, require special attention. However, direct temperature measurements in the interior of the human eye are technically challenging and almost impossible. Up to now, in vivo temperature measurements of the interior eye is confined to animal experiments and often involve potentially damaging invasive or direct contact-based procedures or is limited to simulated eye models [2].
2 Histological Structures of the Eye and Their Contribution to Thermal Regulation of the Ocular Compartments
The human eye is a complex organ consisting of several histological compartments having different biological properties and a complex geometry (Fig. 22.1). In the posterior part of the eye, the outermost layer consists of the sclera. The sclera is a white coloured, protective layer containing mainly collagen and some elastic fibers. Beneath the sclera lies the choroid, which is the vascular layer of the eye and supplies the underlying retina layer. The choroid has the highest blood flow in the body, and this is believed to protect the retina from heat stress [3]. Together with the sclera, the choroid can contribute to convective heat transport in the ocular compartments [4]. During this process, the blood absorbs energy from warmer regions and releases it to cooler regions and vice versa. The retina is the photoreceptive tissue of the eye and is believed to be highly thermosensitive. Although it is also vascularized, the contribution to its own temperature regulation is much lower when compared to the choroid [5]. The sclera in the anterior part of the eye becomes transparent – the cornea. This avascular tissue is constantly wetted by tear fluid and, together with other ocular compartments, contributes to the refraction of light that gives the eye its optical power. The conjunctiva, a highly vascularized tissue that lines the inside of the eyelids and covers the sclera, can contribute to the regulation of the corneal temperature [6]. Although not a direct component of the eye, the eyelid also significantly contributes to the temperature regulation of the cornea by blinking during the waking cycle and by constantly covering it during sleep [1]. The lens, as part of the anterior eye, is a transparent biconvex structure surrounded by vitreous humour which, with the cornea, contributes to the refraction of light on the photosensitive retina. The lens lacks vascularization and is well known to be a highly temperature-sensitive structure. The vitreous body is a transparent gelatinous mass consisting of 98–99% water that fills the inner space between the lens and the retina. The vitreous membrane, which consists of collagen, separates the vitreous body from the other parts of the eye. The high amount of water in the vitreous body gives this structure a high ‘heat storing’ potential.
In summary, the eye comprises various structures that can function as heat sinks or as heat stores. With the cornea, the lens and the retina, the eye is therefore comprised of highly temperature-sensitive tissues. Accordingly, exposure to elevated temperatures risks impairment of visual perception. Regarding which elements of the electromagnetic spectrum interact with the eye, it is known that visible light (≈ 400–780 nm) and infrared-A (780–1400 nm) pass through all the thermosensitive layers of the eye before reaching the photosensitive retina (Fig. 22.1) [7]. Although a small amount of ultraviolet-A radiation can still penetrate to the retina, most of the shorter wavelengths <400 nm and the longer wavelengths >1400 nm are absorbed by the cornea and the lens. This is of importance to all medical applications that are based on radiation and can result in photothermal reactions in the ocular structures. As a consequence, treating chlamydial eye infections using wIRA irradiation requires a detailed analysis of the thermal effects occurring in the eye.
3 Effects of Radiation-Induced Photothermal and Photochemical Events on Ocular Structures
Considering wIRA as a potential treatment option for chlamydial eye infections, it is important to note that in recent studies, this approach is most effective when using wIRA-irradiation (780–1400 nm) in combination with visible light (VIS) in the range of 400–780 nm. Both of these components have been described to potentially damage ocular tissues through photothermal or photochemical reactions, depending on exposure time and energy [8].
As the most anterior structure of the eye, the cornea is particularly exposed to temperature changes and radiation. In the infrared-A range of 780–1400 nm which is delivered during wIRA treatment, the cornea transmits up to 96% of the incoming radiation. Thus, damage resulting in immediate pain, vascularization, and eventually a loss of corneal transparency requires the application of high irradiances of infrared radiation to the cornea [9]. For the VIS part of the electromagnetic spectrum, the high energy short-wave blue light between 415 and 455 nm is considered to be the most harmful for ocular structures, and thereby also for the cornea. Blue light can severely impact the survival and function of corneal cells and promote pathological changes, including the development of dry eye syndrome [10].
The lens, as the second structure involved in the refraction of light and contributing to the visual power of the eye, is sensitive to infrared irradiation and exposure to thermal stress. As an example, cataract formation has been frequently observed in humans exposed to high levels of infrared irradiation (>1400 nm) such as glassblowers or ironworkers [11]. Cataract formation associates with clouding of the lens and is, on the molecular level, caused by the disturbed arrangement of crystalline proteins which are the major components of the lens [12]. However, it is assumed that infrared-induced cataract formation is not only caused by the direct heating of the lens but also by the indirect heating of neighbouring ocular structures [9]. For this reason, wIRA may contribute to cataract formation by indirect heating of adjacent ocular structures, even if the wavelengths of 780–1400 nm are not absorbed by the lens. With regard to a combined therapy involving wIRA and VIS components, it should also be noted that blue light has been shown to induce the production of reactive oxygen species (ROS) in the mitochondria of lens epithelial cells, which may also promote the development of cataracts [10].
The retina, as the innermost layer of the posterior eye, converts light stimuli into the nerve signals to the brain, and thereby provides visual capacity. This nervous tissue is probably the most complicated in terms of its sensitivity to thermal and visual stimulation. Infrared radiation that is transmitted through the transparent ocular structures to the retina is not absorbed by the retina itself, but by the adjacent cells of the so-called retinal pigment epithelium [9]. Consequently, thermal injury of retinal cells does not occur directly, but by indirect heating from the pigment epithelium. The induction of thermal damage depends on multiple factors such as the pupil size, the exposure duration, the nature and spectral distribution of the radiation source, as well as the rate of energy delivery. In this context, the exposure time inversely correlates with the radiation power that is necessary to damage the retina. With regard to the threshold of a non-critical temperature increase, a rise of 10 °C above the body temperature will produce permanent damage to the retina and also the underlying choroid by inducing protein denaturation. However, even thermal effects significantly below this limit can alter gene expression in the retina and adjacent pigment epithelium, and therefore risk long-term tissue damage [13, 14]. In addition to the possible hyperthermia effects of wIRA treatment in ocular structures, attention must also be paid to the phenomenon of retinal damage if light of the visible spectrum is included. Photochemical reactions caused by light stress can lead to the degeneration of specific cell types in the whole retina [15]. For this, the visual pigment rhodopsin, which is localized in the light-sensitive photoreceptor cells, plays a decisive role. Rhodopsin regulates the conversion of optical stimuli into the electrochemical signals which initiate the visual cascade via a cycle of changes in the protein configuration. Overloading this cycle by delivering a continuous light stress degenerates the photoreceptors and can lead to a degeneration of the entire retina, and thus to blindness. Since the absorption maximum of rhodopsin lies within the range of 500 nm, blue light represents the most critical photochemical action spectrum for inducing retinal damage [10]. Although blue light has a clear negative effect on the retina, the red light directly adjacent to the wIRA spectrum may have a protective effect on this tissue. For example, wavelengths of 670 nm have been shown to counteract white light-induced lipid oxidation in photoreceptors and their degeneration [16]. In addition, it may contribute to the reduced inflammatory processes in mice with age-related macular degeneration and enhance neuroprotective effects by retinal cells [17,18,19,20].
In summary, the possible severe impact of thermal and light-based therapies on different compartments of the eye, and thereby impaired vision needs to be considered. This also includes the anti-chlamydial therapy with wIRA alone or in combination with VIS.
4 Effect of wIRA on the Eye: Ex Vivo Models
4.1 Temperature Effects of wIRA on Pig Eyes Ex Vivo
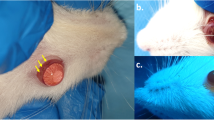
Given the risks of thermal exposure to ocular structures, we considered it necessary to gain a better understanding of the development of the thermal field in the eye during wIRA irradiation as a prerequisite for its subsequent application within the framework of therapeutic treatment approaches. For this, we established an experimental model which allowed us to reproducibly study temperature changes in the cornea and the vitreous body of isolated, perfused pig eyes during exposure to different wIRA irradiances [21]. Pig eyes were chosen as they are similar in size to human eyes and have similar histological and physiological features. Briefly, the experimental model involves the perfusion of whole pig eyes with Krebs solution via the ciliary artery and the placement of the eyes within a temperature-regulated water bath which mimics blood flow and the physiological environment of the eye (Fig. 22.2a). The cornea was not covered by the water bath but constantly washed with Krebs solution to mimic tear flow. Finally, temperature development was measured using two temperature probes that were placed on the cornea and within the vitreous body of the eyes.
Temperature measurements during wIRA irradiation of perfused pig eyes (modified from [21]). (a) Pig eyes were placed in a water bath and perfused with Krebs solution via the ciliary artery. Temperature probes were placed on top of the cornea and inside the vitreous body during wIRA irradiation. (b and c) Temperature measurements during wIRA treatment in the vitreous body (left panel) and on the cornea (right panel). Initial temperature was set to ≈34 °C before eyes were irradiated. (b) Eyes were irradiated with different wIRA irradiances (500, 370, 210 and 100 mW/cm2) (595–1400 nm) for 30 min. During irradiation, an irradiance-dependent temperature increase (except for 100 and 210 mW/cm2 in the cornea) is shown, with a rapid rise in the first 10 min before reaching a plateau. (c) Eyes were irradiated with either wavelengths of 595–1400 nm at an irradiance of 210 mW/cm2 or wavelengths of 780–1400 nm at an irradiance of 200 mW/cm2. In the vitreous body, a mild but significant lower temperature increase was shown upon irradiation with 595–1400 nm compared to wIRA alone (780–1400 nm). The corneal temperature generally shows a slight increase without any differences between the irradiation spectrum of 595–1400 nm and 780–1400 nm
In this ex vivo study, the perfused pig eyes were irradiated with a spectrum of 595–1400 nm for 30 min with irradiances of 100, 210, 370 and 500 mW/cm2 (Fig. 22.2b). Before irradiation was started, the vitreal and corneal temperature was adjusted to 34 °C, which has been reported to be the physiological temperature of pig eyes [22]. As expected, the measured temperature significantly increased with increasing irradiances, before reaching a plateau after 10 min. The temperature of the vitreous body was 41.3 °C (± 0.7 °C) after an irradiance of 500 mW/cm2. In contrast, the temperature after treatment at 100 mW/cm2 was 35.8 °C (± 0.4 °C). Contrary to the results in the vitreous body, corneal temperatures only increased after treatments at irradiances of 370 and 500 mW/cm2 (38.6 °C ± 1.13 °C; 41.13 °C ± 0.93 °C, respectively).
Since visible light in a range of 380–780 nm has been shown to contribute to the increase in intra-well temperatures during in vitro experiments, we examined the impact of the 780–1400 nm spectrum on temperature development in the vitreous body and cornea [23]. For this measurement, an irradiance of 200 mW/cm2 was used. This corresponds with the irradiance of 210 mW/cm2 when the visible part (595–780 nm) is included. However, irradiation for 30 min led to significantly lower temperatures in the vitreous body, including the visual component (37.6 °C ± 0.3 °C), than irradiation with wIRA alone (38.4 °C ± 0.7 °C) (Fig. 22.2c). In contrast, the temperature in the cornea did not exceed 35 °C and was the same for irradiation at 595–1400 nm and 780–1400 nm.
In conclusion, our results show a wIRA-irradiance-dependent increase in the temperature of ocular structures, which is more pronounced in the vitreous body than on the cornea. These findings are consistent with the fact that the vitreous body represents a closed system in which excess heat accumulates and is difficult to be removed. Even more important with respect to the use of wIRA against chlamydial eye infections, our results showed that the temperature increase after treating with a therapy-relevant irradiance of 210 mW/cm2 did not exceed physiological temperatures for both the cornea and the vitreous body. This therapy-relevant irradiance has also been shown to be effective in reducing chlamydial infectivity in vitro and in vivo [21, 24, 25].
Hence, wIRA exposure of ocular structures at moderate irradiances represents a promising approach for treating chlamydial infections, and thus for the prevention of trachoma-induced blinding diseases without increasing ocular temperatures to non-physiological levels.
4.2 Impact of wIRA on the Mouse Retina Ex Vivo
The wIRA-irradiance-dependent temperature increase in the vitreous body of pig eyes might suggest that structures adjacent to the vitreous body, such as the retina, are also heated up during irradiation. Since the retina is a heat- and radiation-sensitive tissue, we investigated the expression of heat- and stress-induced proteins in retinal explants of adult mice. For this, we incubated mouse retina explants at 37 °C or 40 °C for 30 min in the presence or absence of wIRA (595–1400 nm) at an irradiance of 100 mW/cm2, after which we analysed the levels of phosphorylated stress kinases p38, Akt, Erk1/2 and SAPK/JNK by ELISA and found no significant changes immediately (0 h), 3 h or 24 h following treatment (Fig. 22.3a). Consistent with this observation, Western blot analysis for stress-induced proteins HSP70, HSP90, p-p38, NfκB, pErk 1/2 and Erk 1/2 showed no changes in expression levels 3 h after treatment (Fig. 22.3b). In addition, immunolabeling for cell type specific retina markers (glutamine synthetase for Müller glia cells, cone arrestin for cones) to evaluate maintenance of the retina structure indicated no changes in their expression patterns 1 h or 24 h after hyperthermia or a combination of hyperthermia and wIRA (Fig. 22.3c).
wIRA effects on the mouse retina. Explants of adult mouse retina were incubated at 37 °C (Ctrl = control) or 40 °C in cell culture media in the presence and absence of wIRA (595–1400 nm) using an irradiance of 100 mW/cm2. (a, modified from [21]) Levels of phosphorylated stress proteins (p-p38, pAkt, pErk1/2, pSAPK/JNK) were analysed by ELISA, immediately (0 h), 3 h or 24 h after wIRA irradiation. Neither hyperthermia alone nor in combination with wIRA induces any significant changes in protein levels. (b) Western blot analyses of HSP70, HSP90, p-p38, NfκB, pErk 1/2 and Erk 1/2 showed no changes in expression 3 h after the treatments. α-Tubulin serves as loading control. (c) Immunolabeling of cell type specific markers (glutamine synthetase (green) = Müller glia cells, cone arrestin (red) = cones) in mouse retina sections. Cell nuclei were stained with DAPI (blue) in all retinal layers (ONL-outer nuclear layer, INL-inner nuclear layer, GCL-ganglion cell layer). Regardless of treatment, all immunolabeling patterns after 1 h and 24 h were similar
Consequently, our analysis showed that the heat- and radiation-sensitive retina is unaffected by wIRA exposures using an irradiance of 100 mW/cm2 in terms of activation of stress proteins and maintenance of the retinal structure. Together with the results of the temperature measurements, these findings support the use of wIRA irradiation as a novel and safe therapeutic approach for treating chlamydial infections.
5 Outlook
wIRA may be a promising future therapy for the treatment of chlamydial infections of the eye, as has been suggested by various in vitro studies [21, 26]. However, for clinical delivery, it is essential to ensure the safety of the ocular structures that are exposed to wIRA irradiation during treatment. In our ex vivo pig and mouse model experiments, we have been able to obtain the first evidence that wIRA is likely to be safe [21]. Recently, the first in vivo study also demonstrated the efficacy of wIRA for the treatment of chlamydial infections in guinea pig eyes, a well-established model for trachoma-like diseases [25]. In our accompanying in vivo study into the safety of wIRA irradiation on ocular structures in guinea pig eyes, we have also obtained promising results and have excluded the possibility of adverse side-effects due to wIRA exposure (work in progress). Nevertheless, the effects of wIRA irradiation on Chlamydia and ocular structures need to be investigated in more detail and optimized for clinical application in humans. In order to further increase the efficacy of wIRA in terms of chlamydial reduction, the use of photosensitizers (e.g., indocyanine green) could be a promising possibility, since these compounds have been shown to improve the effectiveness of antimicrobial photodynamic therapy (aPDT) [27]. Such approaches also require parallel studies on the mode of action, applicability and safety of the used photosensitizers, both in vitro and in vivo. For this reason, we are currently conducting initial safety studies on human conjunctival cells, by investigating the impact of the photosensitizer indocyanine green during wIRA-based aPDT.
Abbreviations
- Akt :
-
Serine/threonine kinase
- aPDT:
-
Antimicrobial photodynamic therapy
- DAPI:
-
4′,6-Diamidino-2-phenylindole
- ELISA:
-
Enzyme-linked immunosorbent assay
- ERK1/2:
-
Extracellular signal-regulated kinases 1/2
- GCL:
-
Ganglion cell layer
- HSP70:
-
Heat shock protein 70
- HSP90:
-
Heat shock protein 90
- INL:
-
Inner nuclear layer
- IR-A:
-
Infrared-A
- NfκB:
-
Nuclear factor ‘kappa-light-chain-enhancer’ of activated B-cells
- ONL:
-
Outer nuclear layer
- p38:
-
Mitogen activated protein kinases
- ROS:
-
Reactive oxygen species
- SAPK/JNK:
-
Stress-activated protein kinases/Jun amino-terminal kinases
- UVA:
-
Ultraviolet-A
- VIS:
-
Visible light
References
Gokul KC, Gurung DB, Adhikary PR. Thermal effects of eyelid in human eye temperature model. J Appl Math Informatics. 2014;32(56):649–63.
Regal S, Troughton J, Delattre R, et al. Changes in temperature inside an optomechanical model of the human eye during emulated transscleral cyclophotocoagulation. Biomed Opt Express. 2020;11(8):4548–59.
Parver LM, Auker C, Carpenter DO. Choroidal blood flow as a heat dissipating mechanism in the macula. Am J Ophthalmol. 1980;89(5):641–6.
Flyckt VMM, Raaymakers BW, Lagendijk JJW. Modelling the impact of blood flow on the temperature distribution in the human eye and the orbit: fixed heat transfer coefficients versus the Pennes bioheat model versus discrete blood vessels. Phys Med Biol. 2006;51(19):5007–21.
Geiser MH, Bonvin M, Quibel O. Corneal and retinal temperatures under various ambient conditions: a model and experimental approach. Klin Monatsblätter Augenheilkunde. 2004;221(5):311–4.
Itokawa T, Suzuki T, Okajima Y, et al. Correlation between blood flow and temperature of the ocular anterior segment in normal subjects. Diagnostics. 2020;10(9):695.
Ivanov IV, Mappes T, Schaupp P, et al. Ultraviolet radiation oxidative stress affects eye health. J Biophotonics. 2018;11:e201700377.
Youssef PN, Sheibani N, Albert DM. Retinal light toxicity. Eye. 2011;2011(25):1–14.
Voke J. Radiation effects on the eye part 1: infrared radiation effects on ocular tissue. Optom Today. 1999;9:22–8.
Zhao ZC, Zhou Y, Tan G, et al. Research progress about the effect and prevention of blue light on eyes. Int J Ophthalmol. 2018;11(12):1999–2003.
Vos JJ, van Norren D. Thermal cataract, from furnaces to lasers. Clin Exp Optom. 2004;87(6):372–6.
Aly EM, Mohamed ES. Effect of infrared radiation on the lens. Indian J Ophthalmol. 2011;59(2):97–101.
Wakakura M, Foulds WS. Response of cultured Müller cells to heat shock - an immunocytochemical study of heat shock and intermediate filament proteins in response to temperature elevation. Exp Eye Res. 1989;48(3):337–50.
Sekiyama E, Saint-Geniez M, Yoneda K, et al. Heat treatment of retinal pigment epithelium induces production of elastic lamina components and antiangiogenic activity. FASEB J. 2012;26(2):567–75.
Różanowska M, Sarna T. Light-induced damage to the retina: role of rhodopsin chromophore revisited. Photochem Photobiol. 2005;81(6):1305–30.
Rutar M, Natoli R, Albarracin R, et al. 670-nm light treatment reduces complement propagation following retinal degeneration. J Neuroinflammation. 2012;9:257.
Begum R, Powner MB, Hudson N, et al. Treatment with 670 nm light up regulates cytochrome C oxidase expression and reduces inflammation in an age-related macular degeneration model. PLoS One. 2013;8(2):e57828.
Albarracin R, Eells J, Valter K. Photobiomodulation protects the retina from light-induced photoreceptor degeneration. Invest Ophthalmol Vis Sci. 2011;52:3582–92.
Albarracin R, Valter K. 670 nm red light preconditioning supports Müller cell function: evidence from the white light-induced damage model in the rat retina. Photochem Photobiol. 2012;88(6):1418–27.
Heinig N, Schumann U, Calzia D, et al. Photobiomodulation mediates neuroprotection against blue light induced retinal photoreceptor degeneration. Int J Mol Sci. 2020;21(7):2370.
Rahn C, Marti H, Frohns A, et al. Water-filtered infrared A reduces chlamydial infectivity in vitro without causing ex vivo eye damage in pig and mouse models. J Photochem Photobiol B. 2016;165:340–50.
Landers MB, Watson JS, Ulrich JN, et al. Determination of retinal and vitreous temperature in vitrectomy. Retina. 2012;32(1):172–6.
Marti H, Blenn C, Borel N. The contribution of temperature, exposure intensity and visible light to the inhibitory effect of irradiation on acute chlamydial infection. J Photochem Photobiol B. 2015;153:324–33.
Kuratli J, Pesch T, Marti H, et al. Water filtered infrared A and visible light (wIRA/VIS) irradiation reduces chlamydia trachomatis infectivity independent of targeted cytokine inhibition. Front Microbiol. 2018;9:2757.
Inic-Kanada A, Stojanovic M, Miljkovic R, et al. Water-filtered infrared A and visible light (wIRA/VIS) treatment reduces chlamydia caviae-induced ocular inflammation and infectious load in a Guinea pig model of inclusion conjunctivitis. J Photochem Photobiol B. 2020;209:111953.
Marti H, Koschwanez M, Pesch T, et al. Water-filtered infrared A irradiation in combination with visible light inhibits acute chlamydial infection. PLoS One. 2014;9(7):e102239.
Al-Ahmad A, Tennert C, Karygianni L, et al. Antimicrobial photodynamic therapy using visible light plus water-filtered infrared-A (wIRA). J Med Microbiol. 2013;62:467–73.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Frohns, A., Frohns, F. (2022). Safety of Water-Filtered Infrared A (wIRA) on the Eye as a Novel Treatment Option for Chlamydial Infections. In: Vaupel, P. (eds) Water-filtered Infrared A (wIRA) Irradiation. Springer, Cham. https://doi.org/10.1007/978-3-030-92880-3_22
Download citation
DOI: https://doi.org/10.1007/978-3-030-92880-3_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-92879-7
Online ISBN: 978-3-030-92880-3
eBook Packages: MedicineMedicine (R0)