Abstract
A case is reported of a female patient who presented with a fulminant spread of an infection of odontogenic origin. The infection extended into the orbit where orbital abscess formation developed which resulted in loss of the affected globe.
Different routes of spread of an infection of the dentition, per continuitatem and by venous facial vasculature are discussed.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Odontogenic infection
- Spread of infection by facial veins
- Loss of globe as a result of orbital abscess
-
Be alert of post extractionem signs and symptoms
-
Do not always consider removal of dentition as final treatment as the infection may have developed into an independent process
-
Watch carefully when, after the removal of an infected tooth-molar the patient returns with complaints in or around the eye
-
If there is suspicion of orbital involvement of an original dentogenic infection, do not hesitate to employ early intervention
Introduction
A 50-year-old female, otherwise healthy patient visited the dentist because she suffered from mild toothache problems in the left upper jaw since 6 days. The dentist diagnosed a deeply carious non-vital upper molar which was subsequently removed. The molar removal did not result in an apparent oro-antral communication. In the days following the removal, the patient developed swelling of the ipsilateral side of the face, reason for the dentist to start antibiotic therapy: amoxicillin 500 mg 3 times per day orally. Despite the antibiotics, the infection continued to spread progressively, including swelling around the eye. Once fever developed, the patient decided to visit the general practitioner (GP). The GP directly referred the patient to the outpatient clinic of oral and maxillofacial surgery for further evaluation and treatment.
Physical Examination
On her visit to the clinic, we saw a moderately sick woman, in mild distress, with a body temperature of 37.8 °C, a blood pressure of 140/85, blood values showed a CRP 185, and leucocytes 16.8, including a left shift. Intraorally, there was an undisturbed alveolus healing without discharge. An oro-antral communication could not be demonstrated.
Visual inspection showed an erythematous swelling of the left half of the face with impressive ipsilateral eyelid involvement (Figs. 20.1 and 20.2). On palpation, there was a tense swelling of the left upper eyelid. There was spontaneous discharge of purulent material from the medial canthal region. The patient was not able to open the eye spontaneously and after manual opening of the eyelids, the pupil was not reactive to direct light stimulus, and in addition, the patient denied vision. The globe felt firm on pressure while the iris showed a cloudy aspect. There was extreme limitation of globe motility, and ductions were not possible.
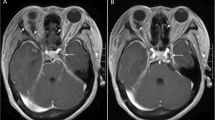
Radiological Examination
The orthopantomogram showed obscuration of the left maxillary sinus (Fig. 20.3). Additional computer tomography (CT) examination of the head and neck area showed a fluid level of the maxillary sinus on the left-hand side, which is consistent with an inflammatory process cranial of the alveolus of the removed upper left first molar. The inflammation extended, through the nasal infundibulum superiorly into the left ethmoid sinus and, after perforation of the extremely thin lamina papyracea, in the orbital space (Fig. 20.4). In the orbit, a pus pocket was visible under the inferior rectus muscle with gas formation. Another pus pocket was diagnosed in the upper eyelid which was connected to the supra- and retrobulbar space. There was no evidence of intracranial spread-extension of the infection (Fig. 20.4).
Spread route odontogenic infection: (a) I via maxillary sinus—infundibulum nasi—ethmoid sinus—perforation lamina papyracea—orbit. II via maxillary sinus—erosion orbital floor—orbit. III via subperiosteal route along the canine fossa or buccal vestibule—perforate eyelid septum—orbital septum—orbit. (b) Via pterygopalatine fossa—infra-temporal fossa—infra-orbital-fissure—orbit. (c) Via retrograde venous flow through valveless facial plexus—orbit/cavernous sinus (Courtesy of Serge Steenen)
Therapy
The patient was subsequently taken to the operating theatre to carry out an emergency incision and evacuation of the pus pockets under general anaesthesia, leaving drains both intraorally at the location of alveolus upper left first molar where an oro-antral opening was created for adequate drainage of the maxillary sinus and at the location of the lower and upper eyelid in the orbit (Fig. 20.5).
The drainage material was sampled and sent for microbiology culture. The culture outcome showed growth of Streptococcus anginosus and Bacteroides, both sensitive to Augmentin (amoxicillin + clavulanic acid). Due to insufficient clinical improvement of the swelling and pupil reaction, the patient was transferred to an academic hospital. Unfortunately, it turned out that bulb rupture had already taken place and vision of the left eye had been lost. It was then decided to perform evisceration of the left eye while retaining the sclera and the extraocular eye musculature (Fig. 20.6). After extensive intravenous antibiotic treatment during a period of 2 weeks hospitalization, the patient made a good clinical recovery. At a later stage, an acrylic implant was placed in the vacant eye cavity (Figs. 20.7 and 20.8).
Contemplation
In this specific case, the periapical infectious process had developed into a maxillary sinusitis. In time, the isolated sinus infection extended along the nasal infundibulum into the ethmoid cells. From here, perforation of the lamina papyracea occurred resulting in further spread of the infection into the orbital cavity and upper and lower eyelids. Especially the impressive swelling of the upper eyelid that obscured the eye accordingly was of most concern to the patient. There were no obvious complaints from the mouth; no residual swelling or discharge was reported or seen after the molar removal. The purulent infection which was insufficiently responsive to antibiotic treatment eventually resulted in a pre- and retroseptal and retrobulbar abscess. The course of the illness was further complicated by complete loss of vision, probably due to compression of the vaso nervorum and direct compression of the optic nerve. Bulb rupture resulted as a consequence of increased pressure in and around the eye cavity.
Discussion
Orbital infections (cellulitis and abscess) are infections of orbital tissue with various causes such as trauma, as a complication after eye surgery, tear duct infections, eyelid infections and dental infections. In 1970, Chandler developed a classification method for infections of the orbit which, however, is currently open to debate (Table 20.1) [1]. An apparent distinction here is a preseptal infection (stage I), which often can be treated with antibiotics, compared to retroseptal infection (other stages), which requires more frequent surgical intervention. An odontogenic cause of an orbit infection is very rare. However, should this complicating pathway occur, there is usually retroseptal abscess formation (Stage III or IV) requiring surgical intervention. Successively, the aetiology, symptoms, treatment and outcomes of odontogenic orbit infections will be discussed.
Aetiology
The immune status of the patient appeared to have a predictive role for the causative agent of an odontogenic orbital infection. In patients with a normal functioning immune system (immune competence), there is usually a bacterial agent causing the infection [2]. The most common pathogens are anaerobic bacteria (mouth flora), S. aureus (in some cases multidrug-resistant Staphylococcus aureus, MRSA), S. epidermidis, haemolytic Streptococci, Pseudomonas aeruginosa and S. milleri. In many of the infections, a combination of bacteria are responsible for the infection [2, 3]. In immunocompromised patients, such as patients with disordered diabetes mellitus, chemotherapeutic treatment or use of immunosuppressants, in addition to bacteria, fungi are the secondary cause of orbital infection. Ketoacidosis in a dysregulated diabetes patient leads to a structural change of neutrophils, and both immunosuppressants and chemotherapy reduce the quality and quantity of functioning neutrophils and macrophages. This reduces the immune response in these patients to withstand fungal infections. Common pathogens in immunocompromised patients are Aspergillus and Mucorales [2].
Spread of the Infection
The route along which a dental infection can spread is largely determined by the relationship between the radix, bone, adjacent muscle attachments and fascial blades, air spaces and gravity. In odontogenic orbit infections, four different routes have been identified in which an odontogenic infection can spread towards the orbit [3] (Fig. 20.9). The most common route is from the apices of premolars or molars to the maxillary sinus. The infection then spreads easily to the air-bearing adjacent ethmoid cells (ethmoid sinus) via the infundibulum nasi. Here the infection can spread to the orbit without too much resistance via perforation of the paper-thin lamina papyracea. Also, after having spread to the adjacent maxillary sinus, the infection may travel superiorly to the orbital floor. The infection can spread to the orbit through bone erosion of the orbital floor or via the infraorbital canal [4] (Fig. 20.9a). The second route is along the fossa canina between the bone (the buccal cortical plate) and the periosteum (periosteum) towards the periorbital tissue. In the third route, infection spreads from the molar region through the pterygopalatine fossa and the communicating infra-temporal fossa to the orbit through the cranial inferior orbital fissure (Fig. 20.9b). The last route is through the facial plexus veins. Because the facial veins, eyes and paranasal sinuses are connected without the presence of valves, an infection or a septic thrombo-embolus can spread to the orbit as a result of haematogenic regurgitation [3, 5] (Fig. 20.9c). With this extension pathway: watch for early signs of septic cavernous sinus thrombosis.
Symptoms
Proptosis and periorbital oedema are the most common symptoms of an odontogenic orbit infection [3, 4]. When the infection spreads post-septically, it can result in increased eye pressure, manifested in decreased eye tracking movements, loss of vision or retrobulbar pain, due to pressure on the vasa nervorum orbita [4]. A disturbed pupil reaction is much rarer; this probably occurs as a result of pressure on the ciliary ganglion (efferent pathway), here the indirect pupil response should also be tested. If disturbed, this indicates compression or infection of the optic nerve (afferent trajectory). For the diagnosis, additional imaging by contrast CT scan is indicated to visualize the infection/abscess with edge staining. In addition to periapical radiolucency at the apex of an odontogenic focus, this often shows ipsilateral obscuration of the maxillary sinus. In addition, in the case of a subperiosteal abscess (stage III) or orbit abscess (stage IV), the scan shows the exact pus location [3] (see Chap. 4).
Therapy
In addition to treatment of the odontogenic focus through extraction of the responsible tooth, direct antibiotic treatment with broad spectrum antibiotics is the cornerstone of the treatment of odontogenic orbital infections. Treatment consists of a combination of antibiotics (augmentin, cefuroxime and/or metronidazole) for adequate coverage, which can be specifically adjusted after cultivation of the responsible bacteria [2, 3, 5]. In addition, corticosteroids (prednisone or dexamethasone) can also be given in the case of orbital cellulitis. The anti-inflammatory medication is said to have a rapid effect on pain, fever, periorbital swelling and reduction of proptosis, although the effect on vision in the long term has not been demonstrated. This makes both the dose and timing of corticosteroid treatment a subject of discussion [6]. In immunocompromised patients, local and systemic antifungal treatment should also be started and any dysregulated glucose level should be treated [2].
In the case of a subperiosteal abscess (stage III) or orbit abscess (stage IV), surgical intervention is necessary. In addition, with an odontogenic orbital infection without evident abscess, one should be wary of a more fulminant course than with an average orbital infection. In cases of an orbital cellulitis (stage II), in addition to antibiotic treatment, surgical treatment is also indicated in a few cases [5]. The approach to an orbital abscess depends on the location of the abscess on the CT scan, but in most cases, it will be an open approach through the conjunctiva (with medial or lateral canthotomy), through the lower eyelid to the orbital floor. In addition, the maxillary sinus often needs to be drained, which can be done via the alveolus of the causal tooth or via a Caldwell Luc approach or a transnasal approach. In the case of a medial orbital abscess, an endoscopic approach is sometimes used with removal of the anterior part of the ethmoid sinus and lamina papyracea by an ENT surgeon [3, 4]. In a rare case of rapidly progressive infection, strong pressure on the eyeball with pain, proptosis and loss of vision, an acute canthotomy is indicated. At the level of the lateral canthus, a sharp preparation is carried out along the temporal part of the orbit in a dorsal direction, so that the dorsal pressure-increasing moment can be acutely relieved or eliminated.
Outcome
If an odontogenic infection of the orbit is recognized too late or left untreated, this can lead to loss of vision. Analysis of 24 patients with an orbital infection showed that half retained moderate to good vision, but the other half retained only light perception or no vision at all. The need for (multiple) surgical intervention by means of incision and drainage is associated with a higher risk of permanent loss of vision. In addition, a more serious visual impairment at presentation such as limited light perception (afferent) or even no light perception appears to be associated with a higher risk of permanent loss of vision [7]. If surgical intervention is necessary, treatment within 24 h seems to give a higher chance of complete visual recovery than treatment after 2–7 days [3]. Loss of the eye, as in this case, is very rare.
Conclusion
Although rare, odontogenic infections may spread into the orbit and can result in loss of vision as a result of orbital abscess development and subsequent necessary globe evisceration.
Despite the removal of the involved molar tooth, the periapical infection had already developed into an independent infectious process.
Although the patient had been treated, fulminant postoperative complications still may occur. Do not underestimate post extractionem signs and or symptoms; once complaints of eye involvement are reported, immediate evaluation and appropriate targeted treatment should be carried out.
References
Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970;80:1414–28.
Leferman CE, Ciubotaru AD, Ghiciuc CM, Stoica BA, Gradinaru I. A systematic review of orbital apex syndrome of odontogenic origin: proposed algorithm for treatment. Eur J Ophthalmol. 2021;31:34–41.
Procacci P, Zangani A, Rossetto A, Rizzini A, Zanette G, Albanese M. Odontogenic orbital abscess: a case report and review of literature. Oral Maxillofac Surg. 2017;21:271–9. https://doi.org/10.1007/s10006-017-0618-1.
Geusens J, Dubron K, Meeus J, Spaey Y, Politis C. Subperiosteal orbital abscess from odontogenic origin: a case report. Int J Surg Case Rep. 2020;73:263–7. https://doi.org/10.1016/j.ijscr.2020.07.014.
DeCroos FC, Liao JC, Ramey NA, Li I. Management of odontogenic orbital cellulitis. J Med Life. 2011;4:314–7.
Pushker N, Tejwani LK, Bajaj MS, Khurana S, Velpandian T, Chandra M. Role of oral corticosteroids in orbital cellulitis. Am J Ophthalmol. 2013;156:178–183.e1.
Youssef OH, Stefanyszyn MA, Bilyk JR. Odontogenic orbital cellulitis. Ophthalmic Plast Reconstr Surg. 2008;24:29–35.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Gooris, P.J.J., Mensink, G., Noorlag, R., Bergsma, J.E. (2023). Orbital Cellulitis as a Result of Spread of Odontogenic Infection. In: Gooris, P.J., Mourits, M.P., Bergsma, J. (eds) Surgery in and around the Orbit. Springer, Cham. https://doi.org/10.1007/978-3-031-40697-3_20
Download citation
DOI: https://doi.org/10.1007/978-3-031-40697-3_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-40696-6
Online ISBN: 978-3-031-40697-3
eBook Packages: MedicineMedicine (R0)