Abstract
We studied a Malian family with parental consanguinity and two of eight siblings affected with late-childhood-onset progressive myoclonus epilepsy and cognitive decline, consistent with the diagnosis of Lafora disease. Genetic analysis showed a novel homozygous single-nucleotide variant in the NHLRC1 gene, c.560A>C, producing the missense change H187P. The changed amino acid is highly conserved, and the mutation impairs malin's ability to degrade laforin in vitro. Pathological evaluation showed manifestations of Lafora disease in the entire brain, with particularly severe involvement of the pallidum, thalamus, and cerebellum. Our findings document Lafora disease with severe manifestations in the West African population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lafora disease (LD) was first described in 1911 as a fatal form of progressive myoclonus epilepsy with onset in the late first or second decade of life [1]. LD is an autosomal recessive disease and causes progressive tonic-clonic seizures, myoclonic jerks, loss of motor control, and intellectual decline. The diagnosis is based on clinical findings, the presence of intracellular polyglucosan inclusions (Lafora bodies, LBs) in neurons and other cell types, including liver and skin [2, 3], and genetic analysis. At least three genes are associated with LD, of which two have been identified: EPM2A and NHLRC1 (NHL repeat containing 1, EPM2B) [4]. The EPM2A gene product, laforin, is a carbohydrate phosphatase, and NHLRC1 encodes the protein malin, an E3 ligase that ubiquitinates and promotes the degradation of laforin and other proteins involved in glycogen metabolism [5–8]. Mutations in laforin and malin lead to the production of LBs, which are deposits of starch-like polyglucosans, insufficiently branched and, hence, insoluble glycogen molecules [9]. The mechanism of neurotoxicity has not been elucidated, but the activity of complexed malin–laforin in the degradation of misfolded protein could explain why recessive mutations in either gene lead to Lafora disease [10]. Lafora disease is a rare disease encountered worldwide, including Eastern and Northern Africa [11–17]. However, to our knowledge, no case has been reported in West Africa. In this paper, we report a Malian family affected by Lafora disease with a novel mutation in the NHLRC1 gene.
Materials and methods
All adult subjects and parents of minors gave written consent before participation in the research protocol used for this study. The protocol was reviewed and approved by the NINDS Institutional Review Board and the Ethical Committee at the University of Bamako. All subjects provided a detailed medical and family history and underwent neurological evaluation and genetic counseling. Computed tomography (CT) brain scan, electroencephalogram (EEG), blood chemistries, and genetic testing were performed. DNA was extracted from peripheral blood with the Qiagen PAXgene Blood DNA kit (Qiagen, Valencia, CA USA) and was sent to Athena Diagnostics, Inc., Worcester, MA, USA, for genetic analysis. Direct sequencing of the EPM2A and NHLRC1 genes was done with polymerase chain reaction-amplified genomic DNA obtained from one sib. Pathological studies were done with brain tissue obtained postmortem from the other sib. The tissue was received in formalin in excellent fixed condition. After external examination, the brain was serially sectioned in the coronal plane for gross examination and extensively sampled for histopathologic evaluation. Tissues were embedded in paraffin and all sections were stained initially with hematoxylin and eosin. Selected sections were then stained with luxol fast blue/periodic acid Schiff (LFB/PAS), and immunohistochemical stains for CD68 and leucocyte common antigen.
The effect of the mutation on malin and laforin expression levels was investigated. Malin and laforin DNA constructs were the kind gift of Matthew Gentry and Jack Dixon. The malin H187P mutant was made using the QuikChange XL site-directed mutagenesis kit (Stratagene) and confirmed by sequencing. Cos7 cells in a six-well dish were transfected with 5 µg of FLAG-laforin or empty pcDNA3.1 and 5 µg wild-type Malin-Myc, mutant Malin-Myc, or empty pcDNA3.1 using 10 µL of Lipofectamine 2000 (Invitrogen). Cells were then collected by centrifugation and lysed on ice in 1% NP-40 lysis buffer supplemented with protease inhibitor cocktail (Roche) and 10 µM MG132 (Sigma). Total protein concentration was quantitated using the Bio-Rad protein assay (Bio-Rad). Twenty micrograms total protein was resolved on 10% Tris–glycine gel (Novex, Invitrogen) and transferred to an Invitrolon polyvinylidene fluoride membrane (Invitrogen) for Western blot analysis. Membranes were blocked with 5% skim milk in Tris-buffered saline Tween-20 (TBST) and incubated with primary antibody overnight at 4°C. To detect levels of laforin, the monoclonal ANTI-FLAG M2 antibody (Sigma) was used, while malin was detected using Myc-Tag Mouse mAb (Cell Signaling); both were diluted 1,000-fold in blocking solution. After three washes in TBST, membranes were incubated for 2 h with peroxidase-conjugated AffiniPure goat anti-mouse IgG (Jackson ImmunoResearch) diluted 5,000-fold in blocking solution.
Results
Patients
Nineteen- and 16-year-old brothers with consanguineous parents (Fig. 1) were evaluated for seizures and difficulty walking.
Their medical history showed no problems at birth, and psychomotor development was normal until the beginning of adolescence. At ages 12 and 9, respectively, they developed generalized tonic clonic seizures with visual auras and aggressive behavior, for which they saw a psychiatrist. The seizures occurred about once a month initially and up to three to eight times per day over the last 2 years. They developed progressive difficulty with walking and use of the hands. Later, they had reduced verbal responsiveness, memory decline, and difficulty with feeding and dressing. Memory and attention became severely affected 4 to 5 years after symptom onset, and they were no longer able to attend school. They developed myoclonic jerks in the extremities, atonic seizures, increasing clumsiness, and falls. The clinical exam showed psychomotor retardation, dull expression, and little to no vocalization. Occasional myoclonic jerks, worse with action and sudden noise, were noted in the face, head, trunk, and extremities. One patient required much assistance in rising to a stand and was grossly ataxic, and the other was bedridden during the examination. Reflexes were normal to reduced, and there was increased tone in the legs. Laboratory evaluations, including blood counts, sedimentation rate, and serum chemistries such as liver enzymes and electrolytes, were normal. An EEG showed generalized spikes, polyspikes, and slow waves. A CT brain scan was normal. Ophthalmologic examination was normal.
The seizures were initially controlled with valproic acid, and later, when they recurred, clonazepam was added. Despite this treatment, both patients continued to have seizures, and by 6 months after the initial exam, both were bedridden. They were admitted to the hospital multiple times for status epilepticus and respiratory infections. They died at ages 20 and 16, respectively (8 and 7 years after onset), with respiratory failure despite intensive care.
Family members reported that a cousin, also from a consanguineous marriage, died from the same symptoms at age 17. The clinical features and pattern of inheritance in the family, as well as the EEG findings and the resistance to anticonvulsant treatment, all suggested the diagnosis of hereditary progressive myoclonus epilepsy.
Genetic analysis
Genetic analysis showed that the older sibling was homozygous for a novel sequence variant (c.560A>C) in the NHLRC1 gene. This nucleotide change is predicted to result in a non-conservative amino acid substitution at codon 187 (H187P). Analysis of this amino acid substitution with the BLOSUM similarity matrix gave a score of −2, suggesting that the sequence variant alters the protein structure and thus likely represents a deleterious mutation [18]. In addition, this amino acid is highly conserved across a broad range of different species, including mammals, fruit fly, plants, and bacteria (Suppl. Fig. 1).
Functional analysis
In order to detect functional changes in malin with the H187P mutation, we examined its ability to reduce steady-state levels of laforin. Recombinant tagged laforin was overexpressed in Cos7 fibroblast cells with tagged variants of malin or empty vector. The steady-state levels of laforin were observed 24 h after transfection. Compared with empty vector, wild-type malin led to a marked reduction in steady-state levels of laforin. Equivalent amounts of malin with the H187P mutation failed to reduce levels of laforin as effectively as wild-type malin. Malin with two other disease-causing mutations (C26S and E280K) also failed to reduce levels of laforin as efficiently as wild-type protein. This demonstrates that the H187P mutation, which lies in the second NHL domain, impairs malin's degradation of laforin in vitro.
Brain pathology
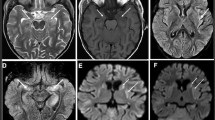
Histologically, the brain tissue revealed scattered areas of diffuse neuronal loss, mild gliosis, and variably sized PAS-positive inclusions involving the entire cortex, basal ganglia, brainstem, and cerebellum to varying degrees, both within neuronal perikarya and free in the neuropil (Suppl. Fig. 2). The numerous intraperikaryonal inclusions showed targetoid architecture with a basophilic core, frequently associated with a surrounding amphophilic zone and/or radial striae, consistent with Lafora bodies. The most severely affected areas were the pallidum and thalamus, followed by the cerebellum. The affected areas showed a prominent diffuse microglial activation (confirmed by immunohistochemistry for CD68 antigen); lymphoid infiltration was absent (confirmed by immunohistochemistry for leucocyte common antigen).
Discussion
LD has been well described in the Mediterranean basin, the Middle East and Asian countries, and North America, and mutations in NHLRC1 are generally more common than in EPM2A [11–14, 19, 20]. Patients have been reported in Africa [15–17]; however, the diagnosis was based on skin biopsy, which may have false positive results [21, 22]. Genetic analysis was recently reported in two African families and showed a mutation in the NHLRC1 gene in one (individual F5) but no definitive mutation in the other (individual F6) [23]. To our knowledge, there has been no clinically and genetically confirmed LD reported in West Africa. Limited access to medical evaluation and genetic testing may explain the lack of reports of the disease in this region.
Studies have shown that patients with mutation in the NHLRC1 gene in general have milder disease course and later age of death compared to those with mutation in the EPM2A gene [11, 19, 21, 24]. The ages of onset and cognitive decline in the family reported here did not differ from previous reports. However, the clinical course was considerably more progressive than in most previously reported patients with NHLRC1 mutations who generally lose independence in activities of daily living at about 26 to 32 years of age and develop respiratory difficulties about 20 years after symptom onset [24]. Some patients with EPM2B manifested symptoms at age 25 and completed higher education [17, 23]; others had rare generalized tonic-clonic seizures (one to four/year), moderate cognitive impairment, and overall preservation of their activities of daily living after reaching the third decade [25].
There is no treatment for LD other than anticonvulsants and respiratory assistance. The patients in the family reported here were given valproic acid and clonazepam, and they had better follow-up than the general population in Mali. Nonetheless, this does not exclude the possibility that a lower level of medical care contributed to the severity of the disease course. A larger comparison study of other families with NHLRC1 in the region might be informative in this regard.
The H187P mutation we found is in the second NHL domain of the NHLRC1 product malin. Of the 51 NHLRC1 published mutations seen at least 156 times in unrelated families [21, 26, 27], three are located in the second NHL domain. Clinical details are not available; however, one patient was reported to have symptoms at age 25 (G194C) [23] and another presented with loss of cognitive function at age 12 [11]. The ages of respiratory compromise and death were not mentioned. No clinical information was available for the third patient (D195N) [24].
Others have shown that pathogenic mutations, and in particular mutations in the NHL domains, impair the association of malin and laforin. While the mode of toxicity is not well defined, it is clear that malin's association with laforin is critical for the health of neurons. One measure of this association is malin's ability to degrade laforin. We have demonstrated that malin with the H187P mutation is unable to promote the degradation of laforin as well as the wild-type protein; this deficiency resembles the functional change observed in two previously reported mutations.
Our neuropathologic findings are generally consistent with other LD patients, including another recently reported case with NHLRC1 mutation [28]. Comparative neuropathologic studies of patients with different EPM2A and NHLRC1 mutations in association with clinical assessment may help to determine to what extent the phenotype correlates with structural neuropathology. To this end, identification of novel mutations with unusual clinical manifestations can help in further characterizing the mechanism of the disease.
References
Lafora G, Gluck BZ (1911) Beitrag zur histopathologie der myoklonischen epilepsie. Ges Neurol Psychiatry 6:1–14. doi:10.1007/BF02863929
Odor DL, Janeway R, Pearce LA, Ravens JR (1967) Progressive myoclonus epilepsy with Lafora inclusion bodies. II. Studies of ultrastructure. Arch Neurol 16:583–594
Carpenter S, Karpati G (1981) Sweat gland duct cells in Lafora disease: diagnosis by skin biopsy. Neurology 31:1564–1568
Chan EM, Omer S, Ahmed M, Bridges LR, Bennett C, Scherer SW, Minassian BA (2004) Progressive myoclonus epilepsy with polyglucosans (Lafora disease): evidence for a third locus. Neurology 63:565–567
Gentry MS, Worby CA, Dixon JE (2005) Insights into Lafora disease: malin is an E3 ubiquitin ligase that ubiquinates and promotes the degradation of laforin. Proc Natl Acad Sci U S A 102:8501–8506. doi:10.1073/pnas.0503285102
Mittal S, Dubey D, Yamakawa K, Ganesh S (2007) Lafora disease proteins malin and laforin are recruited to aggresomes in response to proteasomal impairment. Hum Mol Genet 16:753–762. doi:10.1093/hmg/ddm006
Worby CA, Gentry MS, Dixon JE (2008) Malin decreases glycogen accumulation by promoting the degradation of protein targeting to glycogen (PTG). J Biol Chem 283:4069–4076. doi:10.1074/jbc.M708712200
Solaz-Fuster MC, Gimeno-Alcaniz JV, Ros S, Fernandez-Sanchez ME, Garcia-Fojeda B, Garcia OC, Vilchez D, Dominguez J, Garcia-Rocha M, Sanchez-Piris M, Aguado C, Knecht E, Serratosa J, Guinovart JJ, Sanz P, Rodriguez de Cordoba S (2008) Regulation of glycogen synthesis by the laforin–malin complex is modulated by the AMP-activated protein kinase pathway. Hum Mol Genet 17:667–678. doi:10.1093/hmg/ddm339
Chan EM, Andrade DM, Franceschetti S, Minassian B (2005) Progressive myoclonus epilepsies : EPM1, EPM2A, EPM2B. In: Delgado-Escueta AV (ed) Advances in neurology, vol 95. Myoclonic epilepsies. . Lippincott Williams & Wilkins, Philadelphia, pp 47–57
Garyali P, Siwach P, Singh PK, Puri R, Mittal S, Sengupta S, Parihar R, Ganesh S (2009) The malin–laforin complex suppresses the cellular toxicity of misfolded proteins by promoting their degradation through the ubiquitin–proteasome system. Hum Mol Genet 18:688–700. doi:10.1093/hmg/ddn398
Gomez-Abad C, Gomez-Garre P, Gutiérre-Delicado E, Saygi S, Michelucci R, Tassinari CA, Rodríguez de Córdoba S, Serratosa JM (2005) Lafora disease due to EPM2B mutations: a clinical and genetic study. Neurology 64:982–986
Chang-Seok K, Sun-Young K, Dae WS, Seung BH, Hyung-Jin K, Jong-Won K (2003) Two novel mutations in the EPM2A gene in a Korean patient with Lafora’s progressive myoclonus epilepsy. J Hum Genet 48:51–54. doi:10.1007/s100380300006
Chan EM, Young EJ, Ianzano L, Munteanu I, Zhao X, Christopoulos CC, Avanzini G, Elia M, Ackerley CA, Jovic NJ, Bohlega S, Andermann E, Rouleau GA, Delgado-Escueta AV, Minassian BA, Scherer SW (2003) Mutations in NHLRC1 cause progressive myoclonus epilepsy. Nat Genet 35:125–127. doi:10.1038/ng1238
Serratosa JM, Delgado-Escueta AV, Posada I, Shih S, Drury I, Berciano J, Zabala JA, Antúnez MC, Sparkes RS (1995) The gene for progressive myoclonus epilepsy of the Lafora type maps to chromosome 6q. Hum Mol Genet 4:1657–1663. doi:10.1093/hmg/4.9.1657
Messouak O, Yahyaoui M, Benabdeljalil M, Benomar A, Ouazzani R, Amarti A, Saidi A, Chkili T (2002) Late discovery of Lafora disease: a family study. Rev Neurol (Paris) 158:74–76
Triki C, Bouassida S, Turki H, Zahaf A, Mhiri C (1999) A rare cause of progressive myoclonic epilepsy: Lafora’s disease. Sem Hop Paris 75:1180–1183
Footitt DR, Quinn N, Kocen RS, Oz B, Scaravilli F (1997) Familial Lafora body disease of late onset: report of four case in one family and a review of the literature. J Neurol 244:40–44. doi:10.1007/s004150050048
Hernikoff S, Hernikoff JG (1992) Amino acid substitution matrices from protein blocks. Proc Natl Acad Sci U S A 89:10915–10919. doi:10.1073/pnas.89.22.10915
Franceschetti S, Gambardella A, Canafoglia L, Striano P, Lohi H, Gennaro E, Ianzano L, Veggiotti P, Sofia V, Biondi R, Striano S, Gellera C, Annesi G, Madia F, Civitelli D, Rocca FE, Quattrone A, Avanzini G, Minassian B, Zara F (2006) Clinical and genetic findings in 26 Italian patients with Lafora disease. Epilepsia 47:640–643. doi:10.1111/j.1528-1167.2006.00479.x
Singh S, Suzuki T, Uchiyama A, Kumada S, Moriyama N, Hirose S, Takahashi Y, Sugie H, Mizoguchi K, Inoue Y, Kimura K, Sawaishi Y, Yamakawa K, Ganesh S (2005) Mutations in the NHLRC1 gene are the common cause for Lafora disease in the Japanese population. J Hum Genet 50:347–352. doi:10.1007/s10038-005-0263-7
Turnbull J, Kumar S, Ren ZP, Muralitharan S, Naranian T, Ackerley CA, Minassian BA (2008) Lafora progressive myoclonus epilepsy: disease course homogeneity in a genetic isolate. J Child Neurol 23:240–242. doi:10.1177/0883073807309245
Andrade DM, Ackerley CA, Minett TS, Teive HA, Bohlega S, Scherer SW, Minassian BA (2003) Skin biopsy in Lafora disease: genotype–phenotype correlations and diagnostic pitfalls. Neurology 61:1611–1614
Lohi H, Turnbull J, Zhao XC, Pullenayegum S, Ianzano L, Yahyaoui M, Mikati MA, Quinn NP, Franceschetti S, Zara F, Minassian BA (2007) Genetic diagnosis in Lafora disease: genotype–phenotype correlations and diagnostic pitfalls. Neurology 68:996–1001. doi:10.1212/01.wnl.0000258561.02248.2f
Singh S, Sethi I, Francheschetti S, Riggio C, Avanzini G, Yamakawa K, Delgado-Escueta AV, Ganesh S (2006) Novel NHLRC1 mutations and genotype–phenotype correlations in patients with Lafora’s progressive myoclonic epilepsy. J Med Genet 43:e48. doi:10.1136/jmg.2005.039479
Baykan B, Striano P, Gianotti S, Bebek N, Gennaro E, Gurses C, Zara F (2005) Late-onset and slow-progressing Lafora disease in four siblings with EPM2B mutation. Epilepsia 46:1695–1697. doi:10.1111/j.1528-1167.2005.00272.x
The Lafora progressive myoclonus epilepsy mutation and polymorphism database (2008). Available at http://projects.tcag.ca/lafora/. Accessed February 26
Singh S, Satishchandra P, Shankar SK, Ganesh S (2008) Lafora disease in the Indian population: EPM2A and NHLRC1 gene mutations and their impact on subcellular localization of laforin and malin. Hum Mutat 29:E1–E12. doi:10.1002/humu.20737
Striano P, Zara F, Turnbull J, Girard JM, Ackerley CA, Cervasio M, De Rosa G, Del Basso-De Caro ML, Striano S, Minassian BA (2008) Typical progression of myoclonic epilepsy of the Lafora type: a case report. Nat Clin Pract Neurol 4:106–111. doi:10.1038/ncpneuro0706
Acknowledgements
This work was supported by the intramural program of the National Institute of Neurological Disorders and Stroke at NIH and the Teaching Hospital and Medical School of Point G of the University of Bamako. We are grateful to the patients and their families for participating in this study. We thank Drs. Aldiouma Guindo and Seidina Diakité for the use of their lab in Mali (Malaria Pathogenesis and Protection Unit) and Drs. Matthew Gentry and Jack Dixon for providing the reagents and advice for the functional assays.
We declare that experiments comply with the current laws of Mali and the United States of America.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary materials
Below is the link to the electronic supplementary material.
Suppl. Fig. 1
Alignment of the NHLRC1 sequence including the predicted amino acid change H187P. Note the histidine conservation among species at position 187. (PDF 14 kb)
Suppl. Fig. 2
a Several Lafora bodies in thalamic neurons (arrow; H–E, ×100). b Lafora bodies stain intensely positive for periodic acid Schiff (PAS, arrow). In addition, numerous smaller PAS-positive bodies can be seen throughout the neuropil (arrowhead; LFB/PAS, ×200) (PDF 176 kb)
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Traoré, M., Landouré, G., Motley, W. et al. Novel mutation in the NHLRC1 gene in a Malian family with a severe phenotype of Lafora disease. Neurogenetics 10, 319–323 (2009). https://doi.org/10.1007/s10048-009-0190-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10048-009-0190-4