Abstract
Cutaneous allodynia (CA) has been described in migraine and has been related to treatment failure. There are little data about the incidence of CA in other primary headache syndromes such as cluster headache (CH). The objectives of this study are to evaluate the prevalence of dynamic mechanical (brush) allodynia (BA) in CH patients attending a tertiary headache clinic, and to assess its relation to disease characteristics. Adult patients with episodic or chronic CH were recruited. We obtained demographic data and data on disease characteristics through a structured questionnaire, and tested the patients for brush allodynia BA by applying a 4 × 4 gauze pad over the V1, C2/C3 and C8 skin areas bilaterally. The prevalence of allodynia in the entire study population and in the different sub-groups was calculated. We also examined the association between CA and demographic parameters, and its association with disease characteristics. Forty-one patients were recruited (22 men, 19 women; mean age 44.9 years). Twenty-two had chronic CH (CCH) and 19 had episodic CH (ECH). Mean disease duration was 14.1 years (12.3 the CCH group and 15.7 in the ECH group). Overall, 20 (49%) patients were allodynic. There was no statistically significant association between the presence of allodynia and age, gender, diagnosis (episodic vs. chronic CH), disease duration or disease severity. In conclusion, BA was common in this CH patient sample. The therapeutic implications of the presence of BA in CH need to be further studied.
Similar content being viewed by others
Introduction
Cutaneous allodynia (CA) is the experience of pain when a non-noxious stimulus is applied to normal skin [1]. Studies have shown that up to 80% of patients with episodic migraine experience allodynia during an acute attack [1, 2]. Some of these studies used a questionnaire to identify allodynic migraine patients [3, 4], while in others, patients were tested for mechanical or thermal allodynia using quantitative sensory testing (QST) or other methods [5, 6]. Allodynia is also common in patients with chronic migraine, [7] and these patients may exhibit allodynia even when they do not experience acute headache exacerbations [8]. Allodynia in migraine is the clinical correlate of central sensitization of neurons in the trigeminal nucleus caudalis [9]. The identification of allodynia in migraine may have therapeutic implications [10], although this notion has been debated [11].
Cluster headache (CH) is a severe primary headache syndrome. The pathogenesis of CH is not completely understood but neuroimaging data suggest involvement of the hypothalamus [12]. The trigeminovascular and autonomic nervous systems are also thought to be involved [13]. In a previous study, we found that 40% of our CH patients experienced CA, and that median disease duration was longer in allodynic, as compared with non-allodynic, patients [14]. Another recent study, however, failed to confirm these results [15]. CA can occur during acute CH attacks [16] and successful acute CH treatment with oxygen may reduce CA associated with an attack [17].
Since the current data on the occurrence of allodynia in CH are inconsistent, we sought to further investigate this question in a larger number of patients. The goal of this study was to evaluate the prevalence of dynamic mechanical (brush) allodynia (BA) in CH patients attending a tertiary headache clinic, and to assess its relation to disease characteristics. We hypothesized that BA will be common in our CH patients.
Methods
Study participants
This study was approved by the Institutional Review Board of Thomas Jefferson University. All subjects signed an informed consent form prior to enrollment. We studied adult (age > 18 years) patients with episodic CH (ECH) or chronic CH (CCH), as defined by ICHD-2 criteria [18], recruited from our out-patient clinic.
Exclusion criteria were as follows: abnormal sensory symptoms or findings on neurological examination, performed by one of the authors, other than allodynia (e.g., hypoesthesia, numbness, paresthesias); any neurological disease that could affect skin sensation, such as multiple sclerosis, stroke or peripheral neuropathy; co-existent migraine; treatment with peripheral nerve block within the 4-week period prior to enrollment; treatment with Botulinum neurotoxin within the 4-month period prior to enrollment; and the use of any acute pain medication, in the 24-h period before allodynia testing. Subjects were allowed to be on headache preventive medications during the study period. However, those who were using opioid drugs on a daily basis were excluded. Subjects who had participated in our previous pilot study [14] were allowed to participate in the current study.
We obtained demographic data and data on disease characteristics through a structured oral questionnaire. We determined the diagnosis through the results of a 10-item questionnaire that was based on ICHD-2 criteria [18] and on previous studies [19]. We used these data to diagnose subjects with either ECH or CCH, and to determine disease severity and duration. We recorded all acute and preventive medications used by the patients for headache or for other conditions.
For each patient, we also documented the following clinical parameters: headache severity, as measured on a 5-point verbal scale (range 0–4); the proportion of time spent with headache, i.e., the ratio between the time a patient had head pain and the time he/she did not, where 0 means no headache at all and 1 means constant headache (range 0-1); and disease-severity index (defined as the proportion of time spent with headache × mean headache severity) (range 0–4).
Allodynia testing
Allodynia testing was done when the patients were not experiencing an acute CH attack. We tested for BA by folding a 4 × 4 in. gauze pad in half and brushing it lightly over the patient’s skin ten times at a rate of 2 s−1, as we described before [14]. The tested skin areas were the forehead (V1), posterior neck (C2/C3) and inner forearm (C8). For each skin area, allodynia was tested sequentially on both sides. We measured allodynia for the tenth stimulus at each skin area using a 100 mm visual analog scale (VAS). We have previously shown that healthy controls show a score of 0 when tested for allodynia using this method [8]. Therefore, a VAS score greater than 0 was considered a positive result in this study. Using this method in migraine patients, we have previously found an allodynia prevalence of 86% during acute attacks [5], a result similar to that obtained in a study that used QST for the same purpose [1].
The prevalence of BA in the entire study population and in the different sub-groups was calculated.
Statistical analysis
Fisher’s exact test was used to compare nominal variables between groups. The Wilcoxon rank-sum test was used to compare interval and ordinal variables between groups. A P value of <0.05 was considered to reflect statistical significance.
Results
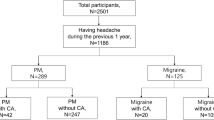
We included 41 subjects in this study [22 (54%) men, 19 (46%) women; mean age 44.9 ± 10.5 years]. Twenty-two subjects (54%) had ECH and 19 (46%) had CCH. Of the ECH patients, 3 (14%) were examined outside their headache cycle. Mean disease duration was 14.1 ± 12 years (ECH 15.7 ± 13.8 years, CCH 12.3 ± 9.6 years.) Disease severity index was significantly higher in subjects with CCH, compared with those who had ECH (0.45 ± 0.51 vs. 0.11 ± 0.11, P < 0.001). The majority of patients (31/41, 76%) were taking preventive prescription medications at the time of the study, including 15/19 (79%) of CCH patients. The most commonly used preventives were verapamil (24/41, 59%), topiramate (9/41, 22%) and divalproex sodium (6/41, 15%).
Twenty (49%) subjects experienced BA (Table 1). There was no significant difference between allodynic and non-allodynic subjects with regard to age, gender or headache severity. BA was more common in subjects with ECH as compared with those who had CCH, but this between-group difference was not statistically significant (55 vs. 42%, P = 0.54). Median disease duration was 10 years in the non-allodynic group and 11 years in the allodynic group (P = 0.83).
The most common site of BA was V1 (18/41, 44%), followed by C2/3 (11/41, 27%) and C8 (8/41, 20%). Only one allodynic subject had BA at a cervical dermatome but not at V1 (Table 2).
Discussion
This is the largest study to date that examined the prevalence of allodynia in CH. We found that CA was common in our CH sample. This study suggests that allodynia and central sensitization may be important in the pathophysiology of CH. These data also suggest that the mechanisms of allodynia in migraine and CH may differ. This hypothesis and the specific mechanisms of allodynia in CH need to be further studied.
Allodynia is likely a result of altered processing of sensory input in the trigeminal nucleus caudalis and may explain why acute migraine treatment is more effective early in an attack (when pain is mild). It has been debated whether the presence of CA modulates the efficacy of triptans in acute migraine treatment [20], as medications such as dihydroergotamine may reverse central sensitization [21]. Clinical features and neuroimaging studies suggest that the hypothalamus is more important in the pathophysiology of CH, than in migraine. Subcutaneous sumatriptan is overwhelmingly effective for most CH patients, despite the fact that they usually do not have the chance to treat the attack when head pain is mild. These observations suggest that the clinical implications of allodynia in these two primary headache disorders may differ. High-flow oxygen is also generally effective in CH, and hyperoxia can affect the extravasation of plasma proteins and decrease levels of calcitonin gene-related peptide [22].
In contrast to our results, Ladda et al. [15] found increased sensory thresholds (i.e., decreased skin sensitivity) in CH subjects. Using QST, they examined their subjects for allodynia at the V2, but not at the V1, skin area. Our study suggests that allodynia in CH is more common at V1. The pain of CH is most commonly located at the periorbital, frontal and temporal areas. Therefore, by not examining for allodynia at the V1 area, Ladda et al. may have underestimated the occurrence of CA in their CH subjects.
Subjects with CCH in this study had increased disease severity, as demonstrated by higher disease severity index, compared with those with ECH. However, CCH subjects were not more likely to have allodynia than ECH subjects. There was no association between allodynia and disease duration in this study. In contrast, in a study of migraine patients, the presence of allodynia was associated with longer disease duration [7] Further studies should investigate the possible association of allodynia with various characteristics of CH, such as disease severity, response to acute treatment (oxygen, sumatriptan), presence of migraine features during attacks, and the serum levels of biomarkers (e.g., brain-derived neurotrophic factor [23] or calcitonin gene-related peptide).
Women represented nearly half of our study sample, unlike the typical gender distribution in CH patients in the general population. This probably reflects a selection bias of a clinic-based study.
Our study is limited by the fact that the majority of subjects were using preventive medications. Since some headache preventive drugs (e.g., gabapentin) may reduce allodynia [24], this may have confounded our results. The different patterns of use of preventive medication between patients with CCH and ECH may have influenced the results of this study. Although no subject in this study was using opioid maintenance therapy for CH or other conditions, we did not exclude patients with recent opioid use. Since, opioid-induced hyperalgesia is increasingly recognized as a common cause of allodynia [25], this may have affected our results.
In summary, brush allodynia was common in our sample of CH patients. The mechanistic and therapeutic implications of this observation need to be evaluated in future studies. In addition, it will be important to evaluate the possible effect of preventive medications on the prevalence of allodynia in CH, and the possible association between allodynia and response to treatment in this disease.
References
Burstein R, Yarnitsky D, Goor-Aryeh I, Ransil BJ, Bajwa ZH (2000) An association between migraine and cutaneous allodynia. Ann Neurol 47(5):614–624, 10805332, 10.1002/1531-8249(200005)47:5<614::AID-ANA9>3.0.CO;2-N, 1:STN:280:DC%2BD3c3mtlSrsA%3D%3D
Mathew NT, Kailasam J, Seifert T (2004) Clinical recognition of allodynia in migraine. Neurology 63(5):848–852, 15365135
Lipton RB, Bigal ME, Ashina S, Burstein R, Silberstein S, Reed ML, Serrano D, Stewart WF, American Migraine Prevalence Prevention Advisory Group (2008) Cutaneous allodynia in the migraine population. Ann Neurol 63(2):148–158, 18059010, 10.1002/ana.21211
Ashkenazi A, Silberstein S, Jakubowski M, Burstein R (2007) Improved identification of allodynic migraine patients using a questionnaire. Cephalalgia 27(4):325–329, 17376108, 10.1111/j.1468-2982.2007.01291.x, 1:STN:280:DC%2BD2s7ns1egug%3D%3D
LoPinto C, Young WB, Ashkenazi A (2006) Comparison of dynamic (brush) and static (pressure) mechanical allodynia in migraine. Cephalalgia 26(7):852–85, 16776701, 10.1111/j.1468-2982.2006.01121.x, 1:STN:280:DC%2BD28zmtlejtA%3D%3D
Kitaj MB, Klink M (2005) Pain thresholds in daily transformed migraine versus episodic migraine headache patients. Headache 45(8):992–998, 16109112, 10.1111/j.1526-4610.2005.05179.x
Lovati C, D’Amico D, Rosa S, Suardelli M, Mailland E, Bertora P, Pomati S, Mariani C, Bussone G (2007) Allodynia in different forms of migraine. Neurol Sci 28(Suppl 2):S220–S221, 17508175, 10.1007/s10072-007-0781-5
Ashkenazi A, Sholtzow M, Shaw JW, Burstein R, Young WB (2007) Identifying cutaneous allodynia in chronic migraine using a practical clinical method. Cephalalgia 27(2):111–117, 17257230, 10.1111/j.1468-2982.2006.01255.x, 1:STN:280:DC%2BD2s%2FlsVamuw%3D%3D
Burstein R, Jakubowski M (2004) Analgesic triptan action in an animal model of intracranial pain: a race against the development of central sensitization. Ann Neurol 55(1):27–36, 14705109, 10.1002/ana.10785, 1:CAS:528:DC%2BD2cXhtVOnu7k%3D
Burstein R, Collins B, Jakubowski M (2004) Defeating migraine pain with triptans: a race against the development of cutaneous allodynia. Ann Neurol 55(1):19–26, 14705108, 10.1002/ana.10786, 1:CAS:528:DC%2BD2cXhtVOnu7g%3D
Dahlöf C (2006) Cutaneous allodynia and migraine: another view. Curr Pain Headache Rep 10(3):231–238, 18778579, 10.1007/s11916-006-0051-x
May A, Goadsby PJ (2001) Hypothalamic involvement and activation in cluster headache. Curr Pain Headache Rep 5(1):60–66, 11252139, 10.1007/s11916-001-0011-4, 1:STN:280:DC%2BD3M3os1GrtA%3D%3D
Goadsby PJ, Edvinsson L (1994) Human in vivo evidence for trigeminovascular activation in cluster headache. Neuropeptide changes and effects of acute attacks therapies. Brain 117(Pt 3):427–434, 7518321, 10.1093/brain/117.3.427
Ashkenazi A, Young WB (2004) Dynamic mechanical (brush) allodynia in cluster headache. Headache 44(10):1010–1012, 15546264, 10.1111/j.1526-4610.2004.04195.x
Ladda J, Straube A, Förderreuther S, Krause P, Eggert T (2006) Quantitative sensory testing in cluster headache: increased sensory thresholds. Cephalalgia 26(9):1043–1050, 16919054, 10.1111/j.1468-2982.2006.01134.x, 1:STN:280:DC%2BD28vpsVajtQ%3D%3D
Riederer F, Selekler HM, Sándor PS, Wöber C (2009) Cutaneous allodynia during cluster headache attacks. Cephalalgia. doi: 10.1111/j.1468-2982.2008.01794
Huber G, Lampl C (2009) Oxygen therapy influences episodic cluster headache and related cutaneous brush and cold allodynia. Headache 49(1):134–136, 18624708, 10.1111/j.1526-4610.2008.01187.x
The International Classification of Headache Disorders (2004) Headache Classification Committee of the International Headache Society, 2nd edn. Cephalalgia 24(Suppl 1):1–160
Torelli P, Beghi E, Manzoni GC (2005) Validation of a questionnaire for the detection of cluster headache. Headache 45(6):644–652, 15953296, 10.1111/j.1526-4610.2005.05131.x, 1:STN:280:DC%2BD2Mzgs1WlsQ%3D%3D
Lampl C, Huber G, Haas S, Rittberger E, Diener HC (2008) Difference in triptan effect in patients with migraine and early allodynia. Cephalalgia 28(10):1031–1038, 18624801, 10.1111/j.1468-2982.2008.01642.x, 1:STN:280:DC%2BD1cnjtFyrsg%3D%3D
Schürks M, Diener HC (2008) Migraine, allodynia, and implications for treatment. Eur J Neurol 15(12):1279–1285, 19068510, 10.1111/j.1468-1331.2008.02343.x
Schuh-Hofer S, Siekmann W, Offenhauser N, Reuter U, Arnold G (2006) Effect of hyperoxia on neurogenic plasma protein extravasation in the rat dura mater. Headache 46(10):1545–1551, 17115987, 10.1111/j.1526-4610.2006.00447.x
Blandini F, Rinaldi L, Tassorelli C, Sances G, Motta M, Samuele A, Fancellu R, Nappi G, Leon A (2006) Peripheral levels of BDNF and NGF in primary headaches. Cephalalgia 26(2):136–142, 16426267, 10.1111/j.1468-2982.2005.01006.x, 1:STN:280:DC%2BD28%2Fptlentw%3D%3D
Berry JD, Petersen KL (2005) A single dose of gabapentin reduces acute pain and allodynia in patients with herpes zoster. Neurology 65(3):444–447, 16087911, 10.1212/01.WNL.0000168259.94991.8a, 1:CAS:528:DC%2BD2MXmsVyjtLk%3D
Mitra S (2008) Opioid-induced hyperalgesia: pathophysiology and clinical implications. J Opioid Manag 4(3):123–130, 18717507
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Marmura, M.J., Abbas, M. & Ashkenazi, A. Dynamic mechanical (brush) allodynia in cluster headache: a prevalence study in a tertiary headache clinic. J Headache Pain 10, 255–258 (2009). https://doi.org/10.1007/s10194-009-0124-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10194-009-0124-4