Abstract
Background
Germline mutations of BRCA1/2 are associated with hereditary breast and ovarian cancer. Recent data suggests excess mortality in mutation carriers beyond that conferred by neoplasia, and recent in vivo and in vitro studies suggest a modulatory role for BRCA proteins in endothelial and cardiomyocyte function. We therefore tested the association of BRCA2 variants with clinical cardiovascular disease (CVD).
Methods
Using data from 1,170 individuals included in two multi-ethnic population-based studies (SHARE and SHARE-AP), the association between BRCA2 variants and CVD was evaluated. 15 SNPs in BRCA2 with minor allele frequencies (MAF) > 0.01 had been previously genotyped using the cardiovascular gene-centric 50 k SNP array. 115 individuals (9.8%) reported a CVD event, defined as myocardial infarction (MI), angina, silent MI, stroke, and angioplasty or coronary artery bypass surgery. Analyses were adjusted for age and sex. The SNPs rs11571836 and rs1799943 were subsequently genotyped using the MassARRAY platform in 1,045 cases of incident MI and 1,135 controls from the South Asian subset of an international case-control study of acute MI (INTERHEART), and rs11571836 was imputed in 4,686 cases and 4500 controls from the Pakistan Risk of Myocardial Infarction Study (PROMIS).
Results
Two BRCA2 SNPs, rs11571836 and rs1799943, both located in untranslated regions, were associated with lower risk of CVD (OR 0.47 p = 0.01 and OR 0.56 p = 0.03 respectively) in the SHARE studies. Analysis by specific ethnicities demonstrated an association with CVD for both SNPs in Aboriginal People, and for rs11571836 only in South Asians. No association was observed in the European and Chinese subgroups. A non-significant trend towards an association between rs11571836 and lower risk of MI was observed in South Asians from INTERHEART [OR = 0.87 (95% CI: 0.75-1.01) p = 0.068], but was not evident in PROMIS [OR = 0.96 (95% CI: 0.90-1.03) p = 0.230]. Meta-analysis of both case-control studies resulted in a combined OR of 0.94 (95% CI: 0.89-1.004, p = 0.06).
Conclusions
Although there was an association between two SNPs in BRCA2 and CVD in a multi-ethnic population, these results were not replicated in two South Asian case-control studies of incident MI. Future studies exploring the association between BRCA variants and cardiovascular disorders are needed to clarify the role, if any, for BRCA variants in CVD pathogenesis.
Similar content being viewed by others
Background
Germline mutations of the genes BRCA1 (breast cancer 1, early onset) and BRCA2 (breast cancer 2, early onset) are the most common cause of hereditary breast and ovarian cancer. Autosomal dominant mutations in BRCA1/2 are associated with a lifetime risk of breast and ovarian cancer of up to 85% and 45% respectively [1]. In addition, mutation carriers are at increased risk of several additional cancers including male breast cancer, pancreatic adenocarcinoma, prostate cancer, and melanoma [2]. A recent publication has suggested BRCA mutation carriers have an excess risk of mortality compared to non-carriers beyond that explained by the development or treatment of malignancy [3]. Mai et al. utilized a kin-cohort analysis to estimate the effect of BRCA1/2 mutations on mortality. When deaths related to cancer diagnosis were excluded, the difference in life expectancy was 5.7 years lower for women and 3.7 years for men with mutations compared to age matched non-mutation carriers. The etiology of this excess mortality is currently unknown. However, BRCA1 and BRCA2 are members of a complex network of proteins involved in DNA repair and genomic stability [4], suggesting their role could extend beyond regulation of neoplasia.
Recently, a cardiomyocyte specific BRCA1 knockout mouse was developed, which showed increased susceptibility to myocardial ischemia and genotoxic agents (doxorubicin), suggesting BRCA dysfunction might play a role in cardiac damage during myocardial infarction and genotoxin induced cardiotoxicity [5]. In a separate study, cardiomyocyte specific BRCA2 knockout mice exhibited similar susceptibility to genotoxic agents [6]. There was an association between increased double stranded DNA breaks and cardiac damage in both reports irrespective of the precipitating cause, alluding to the possibility of similarities in pathogenesis [5, 6]. The idea of overlapping functions for BRCA1 and BRCA2 is further supported by evidence that the two proteins co-localize in the nucleus and play crucial roles in DNA repair [4]. In addition, the cancer phenotypes expressed by germline mutations in both genes are similar [7].
BRCA mutations that are associated with a markedly increased risk of cancer (most often resulting in protein truncation) are extremely rare in the general population [8]. There are however, several hundred single nucleotide polymorphisms (SNPs) in BRCA1/2, many of which are common [9]. We hypothesized that common polymorphisms in BRCA genes may be associated with cardiovascular disease (CVD), another complex trait, with molecular evidence (see above) suggesting a role for the BRCA genes.
To test this hypothesis, we assessed the association between SNPs in BRCA and CVD in individuals from the multi-ethnic SHARE and SHARE-AP studies [10, 11]. These cross-sectional, randomly sampled, population-based studies explored differences in CVD risk factors and prevalence in South Asian, European, Chinese, and Aboriginal ethnic groups residing in Canada. The SHARE studies demonstrated that Aboriginal people and South Asians had the highest prevalence of CVD amongst the four ethnic groups [10, 11].
Methods
Overall approach
We analyzed SHARE and SHARE-AP data that was available from the prior genotyping of 50,000 SNPs from candidate genes and pathways for cardiovascular, inflammatory and metabolic phenotypes in these study populations [12–14]. The Illumina HumanCVD beadchip array includes twenty-one SNPs in BRCA2 with MAF >0.01 but does not include any SNPs in BRCA1.
Due to the availability of DNA samples from South Asians, we examined the association between rs11571836 and rs1799943 and incident MI in South Asians from the INTERHEART. INTERHEART is a large, global, standardized case-control study of incident MI from 52 countries [15]. We next became aware of genome wide genotyping data from the PROMIS study, a similar case-control study of incident MI amongst South Asians residing in urban regions of Pakistan [16]. Since our analysis of INTERHEART showed a trend towards an association between MI and rs11571836, but no association between MI and rs1799943, we examined the association of rs11571836 and MI using imputation in the PROMIS analysis.
Informed consent and REB approval
All studies were approved by appropriate research ethics boards. In addition, all participants provided informed consent, including consent for the collection and processing of genetic material in accordance with TriCouncil guidelines.
SHARE studies
The methodology and results of the SHARE studies are described in detail elsewhere [10, 11]. At the time of enrolment, no participant had a diagnosis of cancer. Canadians were classified as South Asian if their ancestors originated from India, Pakistan, Sri Lanka, or Bangladesh; Chinese if their ancestors originated from China, Taiwan, or Hong Kong; and European if their ancestors originated from Europe. Aboriginal people were identified as such if they were members of the Six Nations Band. CVD was defined as prevalent cases of myocardial infarction, angina, coronary angioplasty or CABG, silent myocardial infarction defined by major Q waves on ECG, and stroke as previously described. The ascertainment of CVD events was from self-administered questionnaires, medical records, and electrocardiograms [17].
Genotyping of the SHARE and SHARE-AP samples on the Illumina HumanCVD beadchip had been previously carried out, utilizing standard protocols at two locations, as described in detail elsewhere [13, 14]. The three ethnic groups in SHARE were genotyped at The Centre for Applied Genomics (Hospital for Sick Children, Toronto, Ontario; http://www.tcag.ca), and the Aboriginal people from SHARE-AP were genotyped at the McGill University and Genome Quebec Innovation Centre (Montreal, Quebec;http://www.genomequebec.com).
Replication studies (INTERHEART and PROMIS)
The methodology and results of the INTERHEART and PROMIS studies are described in detail elsewhere [15, 16]. For both studies, individuals presenting to hospitals with acute MI defined cases, while controls were generally patients from the same hospital with no history of cardiovascular disease. The identification of South Asian ethnicity in INTERHEART was based on self-reported ethnicity. However, individuals with self-reported ethnicity that differed from genetically inferred ancestry were excluded from the analysis as previously described [18]. Genotyping of rs11571836 in 1,143 cases and 1,218 controls of South Asian ethnicity from INTERHEART was performed at the McGill University and Genome Quebec Innovation Centre (Montreal, Quebec;http://www.genomequebec.com) using the MassARRAY platform as previously described [19].
Participants of PROMIS were recruited from hospitals of four large urban centres in Pakistan. South Asians were defined as those with ancestry from the Indian subcontinent. As part of PROMIS, 4,686 cases of incident MI and 4,500 controls had been previously genotyped at the Center for Non-Communicable Diseases (Karachi, Pakistan) using the Illumina 660 genome wide association platform as described elsewhere [20]. This array has SNPs spaced at an average of approximately 4 kb intervals. The genotype of rs11571836 was imputed in cases and controls using the software IMPUTE [21]. The Hapmap Phase 2 population (270 individuals) combined with the South Asian samples from Phase 3 (90 individuals) served as the reference samples for the imputation (hapmap.ncbi.nlm.nih.gov).
Statistical analysis
Analyses were performed using SAS (version 8.2; SAS Institute, Cary, NC) and PLINK [22]. Linkage disequilibrium (LD) maps and r 2 values were produced using Haploview 4.0 [23]. In SHARE and SHARE-AP BRCA2 SNPs were tested for their association with prevalent CVD, in each ethnicity, using logistic regression analysis assuming an additive model. Analyses were adjusted for age and sex. The association results for each ethnicity were thereaftercombined utilizing a fixed-effect meta-analysis, adjusted for multiple comparison. The association between incident MI and rs11571836 and rs1799943 was tested in South Asians from the INTERHEART study using logistic regression with an additive model, adjusted for age and sex. Association testing of imputed genotypes with MI in the PROMIS study was performed using SNPTEST [23, 24] utilizing a logistic regression model adjusted for age and sex. A fixed effects meta-analysis combining the association results for rs11571836 and CVD (for the SHARE studies) or MI (for INTERHEART AND PROMIS) from all three studies was performed using PLINK.
Quality control
Of the 21 BRCA2 SNPs present on the HumanCVD beadchip with MAF greater than 0.01 six were excluded as call rates were less than 95% in one or more ethnicities. For the remaining 15 SNPs call rates were in excess of 97% in all ethnicities. In addition, 15 individuals were excluded because of genotype call rates less than 95% for the 15 SNPs. There was no significant deviation from Hardy Weinberg equilibrium as tested within each ethnic group (all p values >0.1). Genotyping of rs11571836 in the INTERHEART samples resulted in a call rate of 98%. The quality of imputation of rs11571836 from PROMIS, as measured by the SNPtest info score was 0.978. No samples were excluded due to poor imputation confidence.
Results
SHARE and SHARE-AP
Of 1,178 individuals with complete genotyping, 115 individuals had at least one CVD outcome (9.8%). Tables 1 and 2 show CVD associations by ethnicity for rs11571836 and rs1799943. CVD was more prevalent in the Aboriginal and South Asian groups compared with the European and Chinese groups. In the case of rs11571836 (Table 1) the association was statistically significant for the Aboriginal and South Asian sub-groups while for rs1799943 (Table 2) the association was statistically significant only in the Aboriginal group. Both SNPs were associated with CVD in meta-analyses that the combined association results for all four ethnicities. For rs11571836 the combined OR was 0.56 (p value 0.009) while for rs1799943 the combined OR was 0.60 (p value 0.01). The I2 test for heterogeneity was 0% for both meta-analyses. There was no association between CVD and any of the other BRCA2 SNPs examined (Additional file 1: Table S1).
Figure 1 shows the LD patterns by ethnicity for SNPs in BRCA2 genotyped in this study. There are significant differences in LD distribution, as defined by LD blocks, between the four ethnic groups. Additionally, there is more LD in this region in the Chinese, South Asian and Aboriginal groups compared to the European group. However, there was no significant LD between rs1799943 and rs11571836 (r2 <0.2) in any ethnicity. The SNP rs11571836 is located in the 3’ UTR of BRCA2, while rs1799943 is in the 5’UTR.
Replication studies (INTERHEART AND PROMIS)
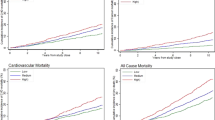
Figure 2 illustrates the results of association analyses between rs11571836 and incident MI in the South Asian INTERHEART and PROMIS studies, including meta-analysis combining the two studies. There was a trend towards an association between rs11571836 and MI in the INTERHEART analysis [OR = 0.87 (95% CI: 0.75-1.01], which did not reach statistical significance (p = 0.068). In contrast, there was no association between MI and rs1799943, p = 0.3 [OR-0.93 (95% CI 0.821-1.062)]. There was no significant association between rs11571836 and incident MI in the PROMIS association study [OR = 0.96 (95% CI: 0.90-1.03) p = 0.23].
Finally, meta-analysis of the replication studies (PROMIS and INTERHEART) for rs111571836 resulted in a combined OR of 0.94 (95% CI: 0.89-1.004, p = 0.066). The I2 test for heterogeneity was 28% (low to moderate). We also performed a meta-analysis utilizing the CVD association results for the South Asian subgroup of SHARE, combined with the association results for acute MI from the two replication studies. Although the resulting odds ratio (OR = 0.9) and p-value (p = 0.05) were marginally lower, the level of heterogeneity was much higher (I2 = 68%, Chi-squared heterogeneity statistic >3 with 2 degrees of freedom). We therefore did not include the SHARE results in the final meta-analysis and resulting forest plot (Figure 2).
Discussion
To our knowledge, this report is the first to suggest a possible association between variants in BRCA1/2 and CVD in human populations. However this observation requires confirmation, given that the effect size appears to be small, and our meta-analysis did not reach statistical significance. It is possible that the association we observed in the SHARE studies was due to chance alone, and is not a true association.
Very little has been published with respect to shared genetic predisposition to cancer and CVD. However, mechanistically, several common pathways are emerging. Most prominent in recent publications is the endothelin axis, with reports linking endothelin-1 to prostate cancer tumorigenesis [25]. Additionally, animal models demonstrate upregulation of DNA repair mechanisms in heart failure induced by ischemic damage [26]. As an example, topoisomerase-II-alpha, a protein involved in various aspects of DNA repair, is overexpressed in unstable plaque from human carotid atheromas [27]. Given its integral role in genomic stability and DNA repair, a similar role in the pathogenesis of coronary atherosclerosis, plaque rupture, and response to ischemic damage may exist for BRCA1/2. Finally, several SNPs associated with metabolic diseases, identified through genome wide association studies, have roles in cancer and chronic disease predisposition. For example, variants in TCF7L2 predispose to both colon cancer and type 2 diabetes while variants in HNF1B predisposes to type 2 diabetes and prostate cancer [28].
Our study suggested a possible association between rs11571836 and rs1799943 and CVD in a multi-ethnic population. Analysis by ethnicity confirmed a statistically significant association with Aboriginal and South Asian ethnicities for rs11571836, while for rs1799943 the association was statistically significant only in the Aboriginal group. It is worth noting however, that with the exception of the Chinese group, all odds ratios trended in the same direction (ie. below 1) for both SNPs. This supports the possible explanation that the current analysis was underpowered to detect an association by individual ethnicity. In fact, only 17% and 6.9% of individuals with CVD in the study were European or Chinese respectively. Alternatively, lack of association between these SNPs and CVD in specific ethnicities may represent differences in LD in the region encompassing BRCA2, as there are significant differences in LD structure in this region among ethnicities (Figure 1). In silico analysis of these two SNPs suggests both may modulate BRCA2 transcript levels [29], but there have been no published functional studies to date. Similarly, neither SNP has been definitively associated with breast cancer susceptibility. Thus, it is quite possible that rs11571836 and rs1799943 are not directly associated with CVD, but instead are in LD with other functional variants associated with CVD. Finally, there may be ethnic-specific differences in the pathogenesis of CVD such that BRCA variation is only relevant to CVD in certain ethnicities, although this seems unlikely given the consistency of other risk factors for CVD across ethnicities [15].
We were unable to demonstrate a statistically significant association between rs11571836 and incident MI in two large case controls studies of incident MI in South Asians, although a trend towards an association was present in INTERHEART. It is possible in INTERHEART that a larger sample size may have resulted in a statistically significant association, as the current sample size was underpowered (44% power) to detect a 15% risk reduction in MI risk for allele frequencies of 20%. A sample size of approximately 2600 cases and a similar number of controls is required to reach 80% power. Based on sample size, the PROMIS analysis was adequately powered, however, it is possible that utilizing imputation to infer the genotype of rs11571836 may have resulted in divergent results from what would have been observed had the SNP been directly genotyped. While the literature suggests good concordance between imputation and direct genotyping [30], it is possible that the HapMap reference samples were not adequate for this region. Alternatively, subtle differences in LD patterns between South Asian populations could explain the lack of a reproducible association between rs11571836 and acute MI in the SHARE, INTERHEART and PROMIS studies. Conversely, the lack of replication would be anticipated if the association between BRCA2 variants and CVD demonstrated in the SHARE studies occurred by chance. One means of further clarifying this possibility is to examine the association between BRCA2 variants and CAD in published GWAS studies. There was no association between either rs11571836 or rs1799943 and CAD in the Wellcome Trust Case Control Consortium (WTCCC) GWAS study [31]. However, the WTCCC study was composed exclusively of White Europeans, unlike our multi-ethnic or South Asian study populations. Unfortunately, lack of publically available data from addition multi-ethnic or South Asian GWAS studies limited our ability “look-up” these SNPs directly in additional studies.
Alternatively, variants in BRCA2 may be more relevant to the pathogenesis of other components of the composite CVD outcome utilized in SHARE (for example ischemic stroke), rather than acute MI. One significant limitation of utilizing the composite CVD outcome in genetic association studies is the heterogeneous pathogenesis of the outcomes studied. In the SHARE studies, the low number of events precluded an assessment of individual components of the composite CVD outcome. Testing the association between BRCA variants and measures of CVD other than MI, ideally from multiple ethnicities, could confirm or refute this hypothesis. In addition, experimental data has thus far only demonstrated a role for BRCA1 in the modulation of cardiomyocyte function following ischemic damage. Due to resource constraints, our analysis was limited to SNPs from BRCA2 that had been previously genotyped, however, investigating the role of SNPs in BRCA1 would be desirable. Finally, data from the murine knock-out models described earlier allude to the possibility that BRCA1/2 may play a greater role in modulating the severity of cardiomyocyte damage following an insult, rather than being directly implicated in initiation of cardiac injury. Therefore, testing the association between variants in the BRCA genes and the severity of a CVD outcome might prove more useful.
Conclusions
Our results suggested a possible association between BRCA2 and CVD in the multi-ethnic SHARE study, however we were unable to replicate this association in two large case-control studies of acute MI in South Asians. Future studies exploring the association between BRCA1/2 variants and CVD outcomes, may help clarify the role, if any, of BRCA variants in CVD pathogenesis.
References
King MC, Marks JH, Mandell JB, New York Breast Cancer Study Group: Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science. 2003, 302 (5645): 643-646. 10.1126/science.1088759.
Liede A, Karlan BY, Narod SA: Cancer risks for male carriers of germline mutations in BRCA1 or BRCA2: a review of the literature. J Clin Oncol. 2004, 22 (4): 735-742. 10.1200/JCO.2004.05.055.
Mai PL, Chatterjee N, Hartge P, Tucker M, Brody L, Struewing JP, Wacholder S: Potential excess mortality in BRCA1/2 mutation carriers beyond breast, ovarian, prostate, and pancreatic cancers, and melanoma. PLoS One. 2009, 4 (3): e4812-10.1371/journal.pone.0004812.
Wang W: Emergence of a DNA-damage response network consisting of Fanconi anaemia and BRCA proteins. Nat Rev Genet. 2007, 8 (10): 735-748.
Shukla PC, Singh KK, Quan A, Al-Omran M, Teoh H, Lovren F, Cao L, Rovira II, Pan Y, Brezden-Masley C, Yanagawa B, Gupta A, Deng CX, Coles JG, Leong-Poi H, Stanford WL, Parker TG, Schneider MD, Finkel T, Verma S: BRCA1 is an essential regulator of heart function and survival following myocardial infarction. Nat Commun. 2011, 2: 593-
Singh KK, Shukla PC, Quan A, Desjardins JF, Lovren F, Pan Y, Garg V, Gosal S, Garg A, Szmitko PE, Schneider MD, Parker TG, Stanford WL, Leong-Poi H, Teoh H, Al-Omran M, Verma S: BRCA2 deficiency exaggerates doxorubicin-induced cardiomyocyte apoptosis and cardiac failure. J Biol Chem. 2011
Lynch HT, Silva E, Snyder C, Lynch JF: Hereditary breast cancer: part I, Diagnosing hereditary breast cancer syndromes. Breast J. 2008, 14 (1): 3-13. 10.1111/j.1524-4741.2007.00515.x.
Whittemore AS, Gong G, John EM, McGuire V, Li FP, Ostrow KL, Dicioccio R, Felberg A, West DW: Prevalence of BRCA1 mutation carriers among U.S. non-Hispanic Whites. Cancer Epidemiol Biomarkers Prev. 2004, 13 (12): 2078-2083.
Szabo C, Masiello A, Ryan JF, Brody LC: The breast cancer information core: database design, structure, and scope. Hum Mutat. 2000, 16 (2): 123-131. 10.1002/1098-1004(200008)16:2<123::AID-HUMU4>3.0.CO;2-Y.
Anand SS, Yusuf S, Jacobs R, Davis AD, Yi Q, Gerstein H, Montague PA, Lonn E: Risk factors, atherosclerosis, and cardiovascular disease among Aboriginal people in Canada: the Study of Health Assessment and Risk Evaluation in Aboriginal Peoples (SHARE-AP). Lancet. 2001, 358 (9288): 1147-1153. 10.1016/S0140-6736(01)06255-9.
Anand SS, Yusuf S, Vuksan V, Devanesen S, Teo KK, Montague PA, Kelemen L, Yi C, Lonn E, Gerstein H, Hegele RA, McQueen M: Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE). Lancet. 2000, 356 (9226): 279-284. 10.1016/S0140-6736(00)02502-2.
Keating BJ, Tischfield S, Murray SS, Bhangale T, Price TS, Glessner JT, Galver L, Barrett JC, Grant SF, Farlow DN, Chandrupatla HR, Hansen M, Ajmal S, Papanicolaou GJ, Guo Y, Li M, Derohannessian S, de Bakker PI, Bailey SD, Montpetit A, Edmondson AC, Taylor K, Gai X, Wang SS, Fornage M, Shaikh T, Groop L, Boehnke M, Hall AS, Hattersley AT, Frackelton E, Patterson N, Chiang CW, Kim CE, Fabsitz RR, Ouwehand W, Price AL, Munroe P, Caulfield M, Drake T, Boerwinkle E, Reich D, Whitehead AS, Cappola TP, Samani NJ, Lusis AJ, Schadt E, Wilson JG, Koenig W, McCarthy MI, Kathiresan S, Gabriel SB, Hakonarson H, Anand SS, Reilly M, Engert JC, Nickerson DA, Rader DJ, Hirschhorn JN, Fitzgerald GA: Concept, design and implementation of a cardiovascular gene-centric 50 k SNP array for large-scale genomic association studies. PLoS One. 2008, 3 (10): e3583-10.1371/journal.pone.0003583.
Lanktree MB, Anand SS, Yusuf S, Hegele RA: SHARE Investigators: Replication of genetic associations with plasma lipoprotein traits in a multiethnic sample. J Lipid Res. 2009, 50 (7): 1487-1496. 10.1194/jlr.P900008-JLR200.
Lanktree MB, Johansen CT, Anand SS, Davis AD, Miller R, Yusuf S, Hegele RA: SHARE Investigators, SHARE-AP Investigators: Genetic variation in hyaluronan metabolism loci is associated with plasma plasminogen activator inhibitor-1 concentration. Blood. 2010, 116 (12): 2160-2163. 10.1182/blood-2010-02-269902.
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L: INTERHEART Study Investigators: Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004, 364 (9438): 937-952. 10.1016/S0140-6736(04)17018-9.
Saleheen D, Zaidi M, Rasheed A, Ahmad U, Hakeem A, Murtaza M, Kayani W, Faruqui A, Kundi A, Zaman KS, Yaqoob Z, Cheema LA, Samad A, Rasheed SZ, Mallick NH, Azhar M, Jooma R, Gardezi AR, Memon N, Ghaffar A, Fazal-ur-Rehman , Khan N, Shah N, Ali Shah A, Samuel M, Hanif F, Yameen M, Naz S, Sultana A, Nazir A, Raza S, Shazad M, Nasim S, Javed MA, Ali SS, Jafree M, Nisar MI, Daood MS, Hussain A, Sarwar N, Kamal A, Deloukas P, Ishaq M, Frossard P, Danesh J: The Pakistan Risk of Myocardial Infarction Study: a resource for the study of genetic, lifestyle and other determinants of myocardial infarction in South Asia. Eur J Epidemiol. 2009, 24 (6): 329-338. 10.1007/s10654-009-9334-y.
Anand SS, Yusuf S, Vuksan V, Devanesen S, Montague P, Kelemen L, Bosch J, Sigouin C, Teo KK, Lonn E, Gerstein HC, Hegele RA, McQueen M: The Study of Health Assessment and Risk in Ethnic groups (SHARE): rationale and design, The SHARE Investigators. Can J Cardiol. 1998, 14 (11): 1349-1357.
Serre D, Montpetit A, Pare G, Engert JC, Yusuf S, Keavney B, Hudson TJ, Anand S: Correction of population stratification in large multi-ethnic association studies. PLoS One. 2008, 3 (1): e1382-10.1371/journal.pone.0001382.
Ehrich M, Bocker S, van den Boom D: Multiplexed discovery of sequence polymorphisms using base-specific cleavage and MALDI-TOF MS. Nucleic Acids Res. 2005, 33 (4): e38-10.1093/nar/gni038.
http://www.illumina.com/pages.ilmn?ID=248. http://www.illumina.com/pages.ilmn?ID=248
Howie BN, Donnelly P, Marchini J: A flexible and accurate genotype imputation method for the next generation of genome-wide association studies. PLoS Genet. 2009, 5 (6): e1000529-10.1371/journal.pgen.1000529.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, Maller J, Sklar P, de Bakker PI, Daly MJ, Sham PC: PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007, 81 (3): 559-575. 10.1086/519795.
Barrett JC, Fry B, Maller J, Daly MJ: Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005, 21 (2): 263-265. 10.1093/bioinformatics/bth457.
Marchini J, Howie B, Myers S, McVean G, Donnelly P: A new multipoint method for genome-wide association studies by imputation of genotypes. Nat Genet. 2007, 39 (7): 906-913. 10.1038/ng2088.
Weydert CJ, Esser AK, Mejia RA, Drake JM, Barnes JM, Henry MD: Endothelin-1 inhibits prostate cancer growth in vivo through vasoconstriction of tumor-feeding arterioles. Cancer Biol Ther. 2009, 8 (8): 720-729. 10.4161/cbt.8.8.7922.
Yndestad A, Neurauter CG, Oie E, Forstrom RJ, Vinge LE, Eide L, Luna L, Aukrust P, Bjoras M: Up-regulation of myocardial DNA base excision repair activities in experimental heart failure. Mutat Res. 2009, 666 (1–2): 32-38.
Slevin M, Elasbali AB, Miguel Turu M, Krupinski J, Badimon L, Gaffney J: Identification of differential protein expression associated with development of unstable human carotid plaques. Am J Pathol. 2006, 168 (3): 1004-1021. 10.2353/ajpath.2006.050471.
Frazer KA, Murray SS, Schork NJ, Topol EJ: Human genetic variation and its contribution to complex traits. Nat Rev Genet. 2009, 10 (4): 241-251.
Rajasekaran R, Doss GP, Sudandiradoss C, Ramanathan K, Rituraj P, Sethumadhavan R: Computational and structural investigation of deleterious functional SNPs in breast cancer BRCA2 gene. Sheng Wu Gong Cheng Xue Bao. 2008, 24 (5): 851-856.
Hao K, Chudin E, McElwee J, Schadt EE: Accuracy of genome-wide imputation of untyped markers and impacts on statistical power for association studies. BMC Genet. 2009, 10: 27-
Wellcome Trust Case Control Consortium: Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007, 447: 661-678. 10.1038/nature05911.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2350/13/56/prepub
Acknowledgements
Dr. Anand holds the Michael DeGroote Heart and Stroke Chair in Population Health Research and a Canada Research Chair in Ethnicity and Cardiovascular Disease. This work was funded in part by a Juravinski Cancer Centre Foundation grant.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare no competing interests.
Authors' contributions
KZ was involved in conception of the study, data analysis, and drafting the manuscript. CX performed statistical analysis. RY was involved in genotyping and association analyses. MH performed statistical analysis. RM and ADD were involved in data acquisition and study co-ordination. GP, SYand JE were involved in study design, data acquisition, and aided in the drafting and revision of the manuscript. RAH, MBL, DS, and JD were involved in data acquisition, genotyping, and revisions of the manuscript. SSA was involved in conception of the study, data acquisition, statistical analysis, and drafting and revising the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Zbuk, K., Xie, C., Young, R. et al. BRCA2 Variants and cardiovascular disease in a multi-ethnic study. BMC Med Genet 13, 56 (2012). https://doi.org/10.1186/1471-2350-13-56
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2350-13-56