Abstract
Background
Pain is one of the most common reasons for seeking medical care. The purpose of this study was to characterize patients visiting the complementary medicine clinic for a pain complaint.
Methods
This is a cross-sectional study. The study took place at Clalit Health Services (CHS) complementary clinic in Beer-Sheva, Israel. Patients visiting the complementary clinic, aged 18 years old and older, Hebrew speakers, with a main complaint of pain were included. Patients were recruited consecutively on random days of the month during a period of six months. Main outcome measures were: pain levels, location of pain, and interference with daily activities. Once informed consent was signed patients were interviewed using a structured questionnaire by a qualified nurse. The questionnaire included socio-demographic data, and the Brief Pain Inventory (BPI).
Results
Three-hundred and ninety-five patients were seen at the complementary medicine clinic during the study period, 201 (50.8%) of them met the inclusion criteria. Of them, 163 (81.1%) agreed to participate in the study and were interviewed. Pain complaints included: 69 patients (46.6%) with back pain, 65 (43.9%) knee pain, and 28 (32.4%) other limbs pain. Eighty-two patients (50.3%) treated their pain with complementary medicine as a supplement for their conventional treatment, and 55 (33.7%) felt disappointed from the conventional medicine experience. Eighty-three patients (50.9%) claimed that complementary medicine can result in better physical strength, or better mental state 51 (31.3%). Thirty-seven patients (22.7%) were hoping that complementary medicine will prevent invasive procedures.
Conclusion
Given the high proportion of patients with unsatisfactory pain relief using complementary and alternative medicine (CAM), general practitioners should gain knowledge about CAM and CAM providers should gain training in pain topics to improve communication and counsel patients. More clinical research to evaluate safety and efficiency of CAM for pain is needed to provide evidence based counseling.
Similar content being viewed by others
Background
Pain is one of the most common reasons for seeking medical care. It is known to affect general health [1], psychological health [2–4], and economic well-being [5, 6].
The prevalence of chronic pain in the general population ranges from 10% to over 40%, depending on the study and definition [7]. Patients with chronic pain use health services up to five times more than patients without pain [8, 9]. Although in the last years we have witnessed an impressive improvement in acute and chronic pain treatment still many patients do not get appropriate pain relief. Thus, people use complementary medicine in aim of finding an approach that combines their philosophy of mind-body-spirit and in interest of participating actively in their medical process [10]. One cross-sectional survey of patients with chronic pain disorders conducted in 12 primary care clinics in USA found that 52% reported using complementary and alternative therapies to assist with pain relief [11]. In the subgroup of Canadian adults reporting chronic back pain CAM use was by about 39% [12].
In a study from United Kingdom among patients who had reported having musculoskeletal pain and who had consulted about their pain in primary care in the previous 12 months, 84% had used at least one CAM treatment for pain in the previous year and 65% were current users of CAM. Most CAM treatments were scored by these patients as being helpful, and users indicated that they intended to use again 87% of the CAM treatments they had already used [13]. In another large study [14] the most popular alternative therapies for low back pain noted were spinal manipulation, acupuncture and massage. The American College of Physicians and the American Pain Society have issued joint clinical practice guidelines recommending that clinicians consider acupuncture as one possible treatment option for patients with chronic low back pain who do not have a response to self-care [15, 16]. Acupuncture was also found to be effective in improving symptoms of osteoarthritis of the knees, and for chronic headache mainly migraine [17].
In Israel, 6 to 10 percent of Israelies reported using complementary and alternative medicine [18, 19] and the rate of use increases [20] . The popularity of complementary medicine in Israel is reflected in the opening of complementary medicine clinics by the different Health Maintenance Organizations (HMOs) and hospitals. Clalit Health Services (CHS), the largest HMO in Israel holds about 40 clinics for complementary medicine throughout the country.
In a study conducted among patients of CHS's complementary medicine clinic in Beer-Sheva, Israel, we found that the most common reason for visiting the complementary clinic were musculoskeletal conditions (47%). Acupuncture and shiatsu massage therapy were the preferred treatments (61% of all treatment provided in the clinic) [21].
As conventional medicine often fails at addressing many patients with a pain experience, and many patients seek other treatment methods. It is important to understand the characteristics of patients attending complementary medicine clinics for a pain complaint.
Methods
Design
This is a cross-sectional study.
Setting
The national health insurance system implemented in Israel in 1995, provides health care to the entire population through non-profit health maintenance organizations (sick funds). The present study was conducted within the framework of the complementary medicine clinic of CHS in Southern Israel, treats annually about 3,000 patients who receive about 15,000 treatments. The treatments offered include acupuncture, reflexology, shiatsu, massage therapy, homeopathy, chiropractic, feldenkreiss, bio feedback, naturopathy, herbal medicine, medical hypnosis and Bach flowers. Patients have a preliminary screening meeting with a physician who recommends the appropriate therapy. The treatments are not included in the national basket of health services, thus patients are required to pay out-of-pocket for these treatments.
Study population
Patients visiting the complementary medicine clinic, aged 18 year old and older, Hebrew speakers, with a main complaint of pain. Patients were recruited consecutively on random days of the month during a period of six months.
Data collection
The screening physician recruited patients for the study. Once informed consent was signed patients were interviewed using a structured questionnaire by a qualified nurse. The personal interview with the patient included socio-demographic data, and the Brief Pain Inventory (BPI) questionnaire that had been translated and validated in our previous work [22]. The BPI questionnaire evaluates pain levels on a 0-10 Visual Analogue Scale (VAS), (0-indication no pain; 10-worst possible pain), as well as interference with different aspects of everyday life.
Statistical analysis
Data was coded and entered into Epidata 2.1 and was analyzed using SPSS 14.0 software (statistical Package for the Social Sciences, SPSS Inc, Chicago).
The study was approved by the institutional review board of Soroka University Medical Center (Approval num 3992).
Results
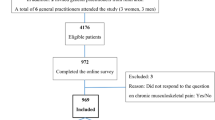
Out of 395 patients seen at the complementary medicine clinic during the study period, 201 (50.8%) met the inclusion criteria. Of them, 163 (81.1%) agreed to participate in the study and were interviewed.
The study population characteristics are described in Table 1. The majority were women (66.9%), born in Israel (46.6%), married (73.6%), and the average age was 51.9 ± 15.6. Sixty-four patients (39.3%) were self referred. Fifty one patients (31.3%) were referred by the medical staff and 38 (23.3%) were referred by a friend or family member. Of the patients reported to have chronic diseases (51%) the most common was hypertension with 51.3%, followed by diabetes 19.2%, and heart disease 15.4%.
Sixty-nine patients (46.6%) had a back pain, 65 (43.9%) had a knee pain and 28 (32.4%) other limbs pain. One-hundred-and six patients (68.4%) reported a moderate pain level on average (VAS 4-7), and 28% reported a severe pain level (VAS 8-10). The average level of pain during the last pain attack was 5.6 ± 1.9 points of the VAS and the "conventional" treatment helped relief less than half of pain severity (Table 2).
Pain impact on daily activities is presented in Table 3. Fifty-eight patients (35.6%) reported that their pain severely influenced their daily routine. Pain caused for 54 (33.1%) patients inability to work or severely interrupted their ability to work. The life impact index was calculated for this group. Pain had high influence on the life impact index for 29 patients (17.8%), (Table 3). The impact of pain on daily activities was evaluated against the socio-demographic characteristics of the study population. In general, older age was found significantly associated with the impact of pain on mood, ability to walk, and relationships with other people (p = 0.05, p = 0.05, p = 0.001 respectively). All other variables, country of birth, gender, religiousness, and education were not found associated with the impact of pain on daily living. The life impact index was also evaluated against all socio-demographic characteristics and was not found significant.
The most common symptoms reported in addition to pain (more than one could be marked) were: sleep disorders (55.2%), tiredness (54.6%) and dizziness (21.5%). Eighty-two patients (50.3%) treated their pain with complementary medicine as a supplement for their conventional treatment, and 55 (33.7%) felt disappointed from the conventional medicine experience. Eighty-three patients (50.9%) claimed that complementary medicine can result in better physical strength, or better mental state 51 (31.3%). Thirty-seven patients (22.7%) were hoping that complementary medicine will prevent invasive procedures. Thirty-eight patients (23.3%) experienced, in the past, acupuncture treatment, 27 (16.6%) had reflexology treatment and 18 (11%) shiatsu treatment (Table 4).
Discussion
Our findings indicate that approximately half the patients attending the complementary clinic for treatment visited due to a pain complaint, where back pain was the leading cause. The majority were women (66.9%), and the average age was 51.9 ± 15.6. Sixty-four patients (39.3%) were self referred. About two thirds reported a moderate pain level on average (VAS 4-7), and a quarter reported on severe pain level (VAS 8-10). The "conventional" treatments helped relief less than half of pain severity.
Our patients visiting the complementary medicine clinic indicated that the pain impacted their daily routine, caused work disturbance and influenced considerably their daily life. In many cases, people concurrently used complementary medicine with conventional medicine in hope of finding the "magic bullet" cure, though also realizing they need to find other ways to cope and to improve their quality of life [23].
An earlier study (from different countries, including Israel) showed that more women, more educated people and more married people [12, 20] are referred to complementary medicine [20, 24, 25]. Middle age (between 40 to 60-65) was considered a predictor to attending complementary medicine [12, 25, 26]. In our sample, the average age was 51.9. In a survey by Shmueli and Shoval [18] the typical patient in complementary medicine is older (average age was 57.7). However, this is still considered "middle age", and the difference is probably due to the fact that the population in Beer-Sheva is younger than in the rest of the country.
One of the predictors to attendance to complementary medicine according to the literature is the existence of chronic diseases [24, 26, 27]. Similar findings were shown in our study, with 51% of patients recruited suffering from a chronic illness.
The main reason for attending complementary medicine clinic among patients in our survey was to supplement conventional medicine treatments (50.3% participants). Moreover, in our study, a third of our study population was referred to the complementary medicine clinic by medical teams. It is known, that only a minority of patients report CAM use to their physicians [27, 28]. Thus, there is an increasing need to improve efforts and communication between conventional physicians and complementary therapists [19].
The complementary medicine clinic in Beer Sheva offers a large spectrum of treatment modalities. Complementary medicine includes several methods of treatment, all of which aim to promote health and quality of life [29]. The main reason for nearly half of those attended to the CAM clinic was in aim of seeking treatment for their pain. The most frequent treatment for this complaint was acupuncture [21].
In designing this study, we adopted recommendations to increase the compliance rate for completion of questionnaires [30]. The response rate of 81.1% was achieved by virtue of the data collection method that included personal interview with each patient, using a short questionnaire that carried the logo of the University Research Center, and use of relatively high-motivated study population.
Our study's results in the complementary medicine clinic in Beer-Sheva reflect the characteristics of the patients that used the complementary clinic for their pain. Since the population in Beer-Sheva is younger than in the rest of the country we cannot be certain of their generalization to other countries and health care systems. However, the age difference is not clinical significant and the results were similar to previous studies.
Conclusions
Patients visiting the complementary medicine clinic indicated that the pain impacted their daily routine, caused work disturbance and influenced considerably their daily life. The most common reasons for patients with a pain complaint visiting the complementary medicine clinic were: as a supplement for conventional treatment, disappointment from conventional medicine and successful previous experience with complementary medicine by a family member or a friend. Given the high proportion of patients with unsatisfactory pain relief using CAM, general practitioners should gain knowledge about CAM and CAM providers should gain training in pain topics to improve communication and counsel patients. More clinical research to evaluate safety and efficiency of CAM for pain is needed to provide evidence based counseling.
We hope that our data can promote understanding the meaning of complementary medicine for painful patients.
References
Becker N, Bondegaard Thomsen A, Olsen AK, Sjogren P, Bech P, Eriksen J: Pain epidemiology and health related quality of life in chronic non-malignant pain patients referred to a Danish multidisciplinary pain center. Pain. 1997, 73: 393-400. 10.1016/S0304-3959(97)00126-7.
Magni G, Marchetti M, Moreschi C, Merskey H, Luchini SR: Chronic musculoskeletal pain and depressive symptoms in the National Health and Nutrition Examination. I. Epidemiologic follow-up study. Pain. 1993, 53: 163-168. 10.1016/0304-3959(93)90076-2.
Gureje O, Von Korff M, Simon GE, Gater R: Persistent pain and well-being: a World Health Organization Study in Primary Care. JAMA. 1998, 280: 147-151. 10.1001/jama.280.2.147.
Turk DC, Rudy TE: Toward an empirically derived taxonomy of chronic pain patients: integration of psychological assessment data. J Consult Clin Psychol. 1988, 56: 233-238.
Latham J, Davis BD: The socioeconomic impact of chronic pain. Disabil Rehabi. 1994, 16: 39-44. 10.3109/09638289409166435.
Locker D: Disability and disadvantage. 1983, Tavistock Publications, London
Nickel R, Raspe HH: Chronic pain: epidemiology and health care utilization. Nervenarzt. 2001, 72: 897-906. 10.1007/s001150170001.
Von Korff M, Dworkin SF, Le Resche L: Graded chronic pain status: an epidemiologic evaluation. Pain. 1990, 40: 279-291. 10.1016/0304-3959(90)91125-3.
Von Korff M, Wagner EH, Dworkin SF, Saunders KW: Chronic pain and use of ambulatory health care. Psychosom Med. 1991, 53: 61-79.
Astin JA: Why patients use alternative medicine: results of a national study. JAMA. 1998, 279: 1548-1553. 10.1001/jama.279.19.1548.
Rosenberg EI, Genao I, Chen I, Mechaber AJ, Wood JA, Faselis CJ, Kurz J, Menon M, O'Rorke J, Panda M, Pasanen M, Staton L, Calleson D, Cykert S: Complementary and alternative medicine use by primary care patients with chronic pain. Pain Med. 2008, 9: 1065-1072. 10.1111/j.1526-4637.2008.00477.x.
Foltz V, St Pierre Y, Rozenberg S, Rossignol M, Bourgeois P, Joseph L, Adam V, Penrod JR, Clarke AE, Fautrel B: Use of complementary and alternative therapies by patients with self-reported chronic back pain: a nationwide survey in Canada. Joint Bone Spine. 2005, 72: 571-577. 10.1016/j.jbspin.2005.03.018.
Artus M, Croft P, Lewis M: The use of CAM and conventional treatments among primary care consulters with chronic musculoskeletal pain. BMC Fam Pract. 2007, 8: 26-10.1186/1471-2296-8-26.
Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL: Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993, 328: 246-252. 10.1056/NEJM199301283280406.
Chou R, Huffman LH, American Pain Society; American College of Physicians: Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007, 147: 492-504.
Chou R, Qaseem A, Owens DK, Shekelle P, Clinical Guidelines Committee of the American College of Physicians: Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians. Ann Intern Med. 2011, 154: 181-9.
Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, Fisher P, Van Haselen R: Acupuncture for chronic headache in primary care: large, pragmatic, randomised trial. BMJ. 2004, 328: 744-10.1136/bmj.38029.421863.EB.
Niskar AS, Peled-Leviatan T, Garty-Sandalon N: Who uses complementary and alternative medicine in Israel?. J Altern Complement Med. 2007, 13: 989-995. 10.1089/acm.2007.0599.
Ben-Arye E, Scharf M, Frenkel M: How should complementary practitioners and physicians communicate? A cross-sectional study from Israel. J Am Board Fam Med. 2007, 20: 565-571. 10.3122/jabfm.2007.06.070119.
Shmueli A, Shuval J: Use of complementary and alternative medicine in Israel: 2000 vs. 1993. Isr Med Assoc J. 2004, 6: 3-8.
Soffer T, Press Y, Peleg A, Friger M, Ganel U, Peleg R: Characteristics of patients at a complementary medicine clinic in Beer Sheva: summary of the first two years of operation. Isr Med Assoc J. 2001, 3: 584-588.
Shvartzman P, Friger M, Shani A, Barak F, Yoram C, Singer Y: Pain control in ambulatory cancer patients--can we do better?. J Pain Symptom Manage. 2003, 26: 716-722. 10.1016/S0885-3924(03)00220-3.
Berman BM: Integrative approaches to pain management: how to get the best of both worlds. BMJ. 2003, 326 (7402): 1280-1281. 10.1136/bmj.326.7402.1280.
Jain N, Astin JA: Barriers to acceptance: an exploratory study of complementary/alternative medicine disuse. J Altern Complement Med. 2001, 7: 689-696. 10.1089/10755530152755243.
Tindle HA, Davis RB, Phillips RS, Eisenberg DM: Trends in use of complementary and alternative medicine by US adults: 1997-2002. Altern Ther Health Med. 2005, 11: 42-49.
Lee GB, Charn TC, Chew ZH, Ng TP: Complementary and alternative medicine use in patients with chronic diseases in primary care is associated with perceived quality of care and cultural beliefs. Fam Pract. 2004, 21: 654-660. 10.1093/fampra/cmh613.
Saydah SH, Eberhardt MS: Use of complementary and alternative medicine among adults with chronic diseases: United States 2002. J Altern Complement Med. 2006, 12: 805-812. 10.1089/acm.2006.12.805.
Hori S, Mihaylov I, Vasconcelos JC, McCoubrie M: Patterns of complementary and alternative medicine use amongst outpatients in Tokyo, Japan. BMC Complement Altern Med. 2008, 8: 14-10.1186/1472-6882-8-14.
Zollman C, Vickers A: ABC of complementary medicine. Complementary medicine and the patient. BMJ. 1999, 319 (7223): 1486-1489.
Smeeth L, Fletcher AE: Improving the response rate to questionnaire. BMJ. 2002, 324: 1168-1169. 10.1136/bmj.324.7347.1168.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6882/11/36/prepub
Acknowledgements
The authors would like to thank the nursing school students who participated in this study for their hard work and dedication.
Source of funding: None
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
RP conceived of the study, and participated in its design and coordination and helped to draft the manuscript. OL conceived of the study, and participated in its design and coordination and helped to draft the manuscript. YP consultation and study design, helped to draft the manuscript. PS coordinating the study, and participated in its design and helped to draft the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Peleg, R., Liberman, O., Press, Y. et al. Patients visiting the complementary medicine clinic for pain: a cross sectional study. BMC Complement Altern Med 11, 36 (2011). https://doi.org/10.1186/1472-6882-11-36
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6882-11-36