Abstract
Background
The aim of this study is to determine the prevalence of anti-HCV among injecting drug users (IDUs) in Lebanon, to establish the current prevalence of HCV genotypes in this population and to determine whether demographic characteristics and behavioral variables differ between participants who were HCV-RNA positive and those who were HCV-RNA negative or between the different genotypes. Participants were recruited using respondent-driven sampling method. The blood samples were collected as dried blood spots and then eluted to be tested for HCV, HBV and HIV by ELISA. Anti-HCV positive samples were subjected to RNA extraction followed by qualitative detection and genotyping.
Results
Among 106 IDUs, 56 (52.8%) were anti-HCV-positive. The two groups did not differ in terms of age, marital status, and nationality. As for the behavioral variable, there was a trend of increased risky behaviors among the HCV-RNA positive group as compared to the HCV-RNA negative group but none of the variables reached statistical significance. Half (50%) of the 56 anti-HCV-positive were HCV-RNA positive. Genotype 3 was the predominant one (57.1%) followed by genotype 1 (21%) and genotype 4 (18%).
Conclusions
The predominance of genotype 3 seems to be the predominant genotype among IDUs in Lebanon, a situation similar to that among IDUs in Western Europe. This study provides a base-line against possible future radical epidemiological variant that might occur in IDUs.
Similar content being viewed by others
Background
The prevalence of HCV antibody (anti-HCV) among intravenous drug users (IVDUs) who share injecting equipment exceeds 50% [1, 2]. This has now become a critical public health threat [3]. The lack of availability of an effective vaccine allowed education programs to be the most suitable interventions in the control of HCV spread [4, 5].
Hepatitis C virus has been classified into 6 major genotypes (1-6) and into several subtypes (a, b, c etc) [6] and additional genotypes have been recently proposed [7, 8]. The genotypes have a geographically distinct distribution [9, 10] which carries important implications such as treatment decisions, possible transmission route and vaccine development. For example the response to therapy observed in patients infected with genotypes 1 and 4 is lower than that infected with genotypes 2 and 3 [11, 12]. Genotype 3a was shown to be more common in Europe among young injecting drug users, compared to genotype 1b which is associated with transfusion-related HCV [13]. Recently we have shown genotype 4 to be the predominant genotype among HCV-infected Lebanese patients (34.2%-53.3%) [10].
The aim of this study is to determine the prevalence of anti-HCV among injecting drug users (IDUs) in Lebanon, to establish the current prevalence of HCV genotypes in this population and to determine whether demographic characteristics and behavioral variables differ between participants who were HCV-RNA positive and those who were HCV-RNA negative or between the different genotypes.
Methods
Study Population and Sampling Methods
Participants included in this study were part of a bio-behavioral surveillance study done to assess HIV prevalence among four vulnerable groups (men who have sex with men, injecting drug users, female sex workers, and prisoners). Two well established Lebanese non-governmental organizations (NGOs) that work with IDUs helped in the study.
Participants in this study were recruited using a relatively new technique entitled respondent-driven sampling (RDS) that has been shown to be effective in reaching difficult to reach or invisible populations for which there is not sampling-frame [14]. A total of 106 eligible IDUs participated in the main study and all were males. After obtaining informed consent, participants completed the questionnaire and an HIV rapid test were offered in addition to proper pretest and post test counseling.
Laboratory Methods
Sample collection
Peripheral blood was collected by a finger prick with a single use Lancet and then blotted onto a high quality filter paper (Schleicher & Schuell 903). The blood spot was allowed to air dry to be used as a dried blood spot (DBS) for further testing at the Molecular Biology Research Laboratory at the Faculty of Health Sciences, American University of Beirut (AUB).
Elution procedure
For each serological test, one DBS disc was cut and placed in the well of a flat-bottomed uncoated micro plate. The blood was then eluted as described previously by Parker and Gublit [15].
Anti-HCV detection and RNA extraction
Eluates were tested for anti-HCV by ELISA using a modified protocol for Ortho HCV 3.0 SAVe (Ortho Clinical Diagnostics, Johnson & Johnson). Anti-HCV positive DBS samples were then subjected to RNA extraction using QIAamp MiniElute Virus Spin (QIAGEN) for further qualitative HCV detection and genotyping.
HCV qualitative detection and HCV genotyping
COBAS AMPLICOR Hepatitis C Virus Test, version 2.0 (v2.0) was used for qualitative in vitro diagnostic HCV detection in the RNA extracted samples using COBAS AMPLICOR Analyzer (Roche). Qualitatively positive HCV aliquots of denatured amplicon by Cobas Amplicor were genotyped using a single LINEAR ARRAY HCV Genotyping strip (LINEAR ARRAY Hepatitis C Virus Genotyping Test - Roche) which is coated with a series of oligonucleotide probes specific for various HCV genotypes.
Statistical Analysis
Descriptive statistics including means and standard deviation and frequency distributions were computed for demographic variables and behavioral variables. Comparisons between HCV-RNA positive and HCV-RNA negative groups were performed using the Chi-squared test for categorical variables (for examples, Sharing needles, marital status, imprisonment, and having a tattoo) and t-test for continuous variables (for example age). Significance was set at the 5% level. All analysis were done using SPSS version 16.0 (Chicago, Illinois, USA).
Results
Only 28 (50%) of the 56 anti-HCV-positive were HCV-RNA positive. Characteristics and behaviors of those who were HCV-RNA positive and HCV-RNA negative are summarized in Table 1. The average age of the participants was 40 years. Almost all participant were Lebanese (96%) and a high proportion of them were ever married (61%). The two groups did not differ in terms of age, marital status, and nationality. As for the behavioral variable, there was a trend of increased risky behaviors (such as having tattoos, sharing needles and injecting drugs in prison) among the HCV-RNA positive group as compared to the HCV-RNA negative group but none of the variables reached statistical significance.
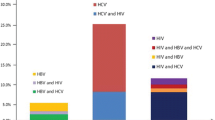
HCV Genotype Distribution
Only HCV genotypes 1, 3 and 4 were detected and one sample showed mixed genotype (1 and 3). The distribution of genotypes is shown in Table 2. Genotype 3 was the predominant (57%) followed by genotype 1 (21%) and genotype 4 (18%).
Characteristics of the HCV RNA-positive sample population (n = 28) according to their genotype is shown in Table 3. The one person with a mixed genotype was not included since no replication is available for comparison reasons.
Discussion
HCV-RNA positivity (50%) detected in our anti-HCV-positive IDUs patients is in agreement with similar studies from different parts of the world including Europe[2, 16], North America[17] and Australia [18]. It has been recently reported that a statistically significant linear relationship could be observed between the mean age and the prevalence of HCV-RNA in IDUs [19]. This linearity however could not be confirmed in our study since most of our studied subjects were relatively young adults and experienced their first injection within roughly the same period of time.
The distribution of HCV genotypes in our IDUs showed that HCV genotype 3 was the predominant genotype (57.1%) followed by genotype 1 (21.4%) and genotype 4 (17.9%). This was surprising and in contrast with our earlier findings where genotype 4 was the predominant genotype (47.5%) in Lebanese patients [10]. The strength of our current data compared to the aforementioned one is that IDUs were recruited in this study by a novel technique (RDS) and that they were from different regions of the country while the earlier study was hospital-based. The predominance of genotype 3 makes the situation in Lebanon similar to that among IDUs in Europe [2, 16] and points to the possibility that genotype 3 could have been introduced to our IDUs Population from Europe. One of the limitations of the study is that the questionnaire did not address socio-economic factors such as income, education and mobility among others.
Since IDUs become infected with HCV in the early phases of drug addiction and most become exposed repeatedly to the virus through needle-sharing, it is expected that infection with more than one genotype would be common [20]. Mixed infections of genotypes were detected in only one sample in our study (3.6%). The higher incidence of mixed infections reported by others could possibly be due to the older age of IDUs in these studies and hence more multiple exposures to HCV infection by sharing of injection material.
Data on major HCV genotypes circulating among injecting drug users in neighboring Middle Eastern countries is still limited [21, 22]. This information would be of importance in contributing to a regional network for the surveillance of HCV genotypes in Middle Eastern countries, an information that could have epidemiological significance. Furthermore, our data might also have therapeutic implications. It has been reported that the response to therapy in patients infected with genotypes 1 and 4 is lower than that noticed in patients infected with genotypes 2 and 3 [11, 12]. It is believed that appropriate treatment may play a role in containing the HCV epidemic that is now being described in IDUs all over the world.
Conclusions
Despite the small number of patients investigated, it can be concluded that genotype 3 seems to be the predominant genotype among IDUs in Lebanon, a situation similar to that among IDUs in Western Europe. However, the authors would like to acknowledge that the sample method used (RDS) was not random as is the situation for population-based surveys such as the National Health and the Examination Survey and thus our findings may or may not be representative of the entire population of IDUs in Lebanon. This study provides a base-line against possible future radical epidemiological variant that might occur in IDUs.
References
Lucidarme D, Decoster A, Fremaux D, Harbonnier J, Jacob C, Vosgien V, Josse P, Villeger P, Henrio C, Prouvost-Keller B, Saccardy C, Lemaire M, Vazeille G, Duchene C, Thuillier M, Colbeaux C, Lefebvre AM, Forzy G, Filoche B: Routine practice HCV infection screening with saliva samples: multicentric study in an intravenous drug user population. Gastroenterology and Clinical Biology 2007, 31: 480-484. 10.1016/S0399-8320(07)89415-2
Micalessi M, Gerard C, Ameye L, Plasschaert S, Brochier B, Vranckx R: Distribution of hepatitis C virus genotypes among injecting drug users in contract with treatment centers in Belgium 2004-2005. Journal of Medical Virology 2008, 80: 640-645. 10.1002/jmv.21145
Pybus O, Cochrane A, Holmes E, Simmonds P: The hepatitis C virus epidemic among injecting drug users, Infection. Genetics and Evolution 2005, 5: 131-139. 10.1016/j.meegid.2004.08.001
Taylor A, Goldberg D, Hutchinson S, Cameron S, Gore SM, McMenamin J, Green S, Pithie A, Fox R: Prevalence of hepatitis C virus infection among injecting drug users in Glasgow 1990-1996: are current harm reduction strategies working? Journal of Infection 2000, 40: 176-183. 10.1053/jinf.2000.0647
Goldberg D, Burns S, Taylor A, Cameron S, Hargreavas D, Hutchison S: Trends in HCV prevalence among injecting drug users in Glasgow and Edinburgh during the era of needle exchange. Scandinavian Journal Infectious Diseases 2001, 33: 457-461. 10.1080/00365540152029936
de Lamballerie X, Charrel RN, Attoui H, De Miccop: Classification of hepatitis C virus variants in six major types based on analysis of the envelop 1 and non-structural 5B genome regions and complete polyprotein sequences. Journal of General Virology 1997, 78: 45-51.
Tokita H, Okamoto H, Luengrojanakul P, Vareesangthip K, Chainuvati T, Iizuka H, Tsuda F, Miyakawa Y, Mayumi M: Hepatitis C virus variants from Thailand classifiable into five novel genotypes in the sixth (6b), seventh (7c, 7d) and ninth (9b, 9c) major genetic groups. Journal of General Virology 1995, 76: 2329-2335. 10.1099/0022-1317-76-9-2329
Tokita H, Okamoto H, Iizuka H, Kishimoto J, Tsuda F, Lesmana LA, Miyakawa Y, Mayumi M: Hepatitis C virus variants from Jakarta, Indonesia, classifiable into novel genotypes in the second (2e and 2f), tenth (10a) and eleventh (11a) genetic groups. Journal of General Virology 1996, 77: 293-301. 10.1099/0022-1317-77-2-293
Simmonds P: Variability of the hepatitis C genome. In Hepatitis C virus. Edited by: Reesink HW. Karger, Basel; 1998.
Sharara A, Ramia S, Ramlawi F, Eid-Fares J, Klayme S, Naman R: Genotypes of hepatitis C virus (HCV) among positive Lebanese patients: comparison of data with that from other Middle Eastern countries. Epidemiology and Infection 2007, 135: 427-432. 10.1017/S0950268806006911
Kurbanov F, Tanaka Y, Sugauchi F, Kato H, Ruzibakiev R, Zalyalieva M, Yunusova Z, Mizokami M: Hepatitis C virus molecular epidemiology in Uzbekistan. Journal of Medical Virology 2003, 69: 367-375. 10.1002/jmv.10298
Poynard T, Yuen MF, Ratziu V, Lai CL: Viral hepatitis C. Lancet 2004, 362: 2095-2100. 10.1016/S0140-6736(03)15109-4
Pawlotsky JM, Tsakiris L, Roudot-Thoraval F, Pellet C, Stuyver L, Duval J, Dhumeaux D: Relationship between hepatitis C virus genotypes and sources of infection in patients with chronic hepatitis C. Journal of Infectious Diseases 1995, 171: 1607-1610.
Heckathorn DD: Respondent-driven sampling: A new approach to the study of hidden populations. Social Problems 1997, 44: 174-199. 10.1525/sp.1997.44.2.03x0221m
Parker SP, Gubilt WD: The use of the dried blood spot sample in epidemiological studies. J Clinical Pathology 1999, 52: 633-639. 10.1136/jcp.52.9.633
Mathei C, Wollants E, Verbeeck J, Van Ranst M, Robaeys G, Van Damme P, Buntinx F: Molecular epidemiology of hepatitis C among drug users in Flanders, Belgium: association of genotypes with clinical parameters with sex and drug- related risk behaviors. European Journal Clinical Microbiology and Infectious Diseases 2005, 24: 514-522. 10.1007/s10096-005-1376-9
Lauer GM, Walker BD: Hepatitis C virus infection. New England Journal of Medicine 2001, 345: 41-52. 10.1056/NEJM200107053450107
Freeman AJ, Zekry A, Whybin LR, Harvey CE, van Beek IA, de Kantzow SL, Rawlinson WD, Boughton CR, Robertson PW, Marinos G, Lloyd AR: Hepatitis C prevalence among Australian injecting drug users in the 1970s and profiles of virus genotypes in the 1970s and 1990s. Medical Journal of Australia 2000, 172: 588-591.
Mathei C, Buntinx F, Van Damme P: Is the prevalence of hepatitis C virus (HCV) RNA in an anti-HCV-positive injection drug users positively correlated with age? Journal of Infectious Diseases 2001, 184: 659-660. 10.1086/322795
Silini E, Bono F, Cividini A, Cerino A, Maccabruni A, Tinelli C, Bruno S, Bellobuono A, Mondelli M: Molecular epidemiology of hepatitis C virus infection among intravenous drug users. Journal of Hepatology 1995, 22: 691-695. 10.1016/0168-8278(95)80225-8
Zamani S, Ichikawa S, Nassirimanesh B, Vazirian M, Ichikawa K, Gouya MM, Afshar P, Ono-Kihara M, Ravari SM, Kihara M: Prevalence and correlates of hepatitis C virus infection among injecting drug users in Tehran. International Journal of Drug Policy 2007, 18: 359-563. 10.1016/j.drugpo.2007.02.007
Alzahrani AJ: Simultaneous detection of hepatitis C virus core antigen and antibodies in Saudi drug users using a novel assay. Journal of Medical Virology 2008, 80: 603-606. 10.1002/jmv.21075
Acknowledgements
We would like to thank the National AIDS Control Programme, Ministry of Public Health, Lebanon, who supported the study, and who through the World Bank Group, provided funds under the IDF Grant for Strengthening the National HIV/AIDS Monitoring and Evaluation and Surveillance Systems in Lebanon. We specifically thank Dr. Mostafa El Nakib, Program Manager NAP-MOPH, for his continuous input and support.
We gratefully acknowledge Dr. David Wilson, Lead Health Specialist-World Bank and Dr. Francisca Ayo Akala, Senior Public Health Specialist-World Bank for substantive comments and support.
The study would not have been possible without the cooperation of the Lebanese NGOs involved as members of the research team Oum El Nour (Mother of Light) and Skoun (Stillness). We thank all team members at these NGOs and other team members at the American University of Beirut.
We would like to thank all those who participated in the study for their time, efforts and willingness to address sensitive topics. The authors would like to acknowledge Roche Diagnostics and all those who helped in supporting the implementation of the study: Miss Danielle El-Khoury (Study Coordinator), Miss Farah El-Barbir and Miss Maguy Ghanem (Research Assistants), and Ms. Maha Abul Naja (Secretary).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
ZM have made contributions to acquisition, analysis and interpretation of data. KK2 designed the study. KK3 carried out the laboratory tests and have been involved in drafting the manuscript and revising its content. SS performed the laboratory tests. SR was responsible for drafting and finalizing the manuscript and has given final approval of the version to be published. All authors read and approved the final version.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Mahfoud, Z., Kassak, K., Kreidieh, K. et al. Distribution of hepatitis C virus genotypes among injecting drug users in Lebanon. Virol J 7, 96 (2010). https://doi.org/10.1186/1743-422X-7-96
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1743-422X-7-96