Abstract
Background
Image-guidance systems allow accurate interfractional repositioning of IMRT treatments, however, these may require up to 15 minutes. Therefore intrafraction motion might have an impact on treatment precision. 3D geometric data regarding intrafraction prostate motion are rare; we therefore assessed its magnitude with pre- and post-treatment fiducial-based imaging with cone-beam-CT (CBCT).
Methods
39 IMRT fractions in 5 prostate cancer patients after 125I-seed implantation were evaluated. Patient position was corrected based on the 125I-seeds after pre-treatment CBCT. Immediately after treatment delivery, a second CBCT was performed. Differences in bone- and fiducial position were measured by seed-based grey-value matching.
Results
Fraction time was 13.6 ± 1.6 minutes. Median overall displacement vector length of 125I-seeds was 3 mm (M = 3 mm, Σ = 0.9 mm, σ = 1.7 mm; M: group systematic error, Σ: SD of systematic error, σ: SD of random error). Median displacement vector of bony structures was 1.84 mm (M = 2.9 mm, Σ = 1 mm, σ = 3.2 mm). Median displacement vector length of the prostate relative to bony structures was 1.9 mm (M = 3 mm, Σ = 1.3 mm, σ = 2.6 mm).
Conclusion
a) Overall displacement vector length during an IMRT session is < 3 mm.
b) Positioning devices reducing intrafraction bony displacements can further reduce overall intrafraction motion.
c) Intrafraction prostate motion relative to bony structures is < 2 mm and may be further reduced by institutional protocols and reduction of IMRT duration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Accurate interfractional patient repositioning before prostate radiotherapy has become possible in the era of Image-Guided RadioTherapy (IGRT, [1]) with several in-room systems such as stereotactic ultrasound [2, 3], beacon responders [4] and kV/MV cone- or fan-beam CT based methods [5–7]. Correction of interfractional movement improves radiation treatment accuracy if geometrical changes are within certain limits [8, 9].
However, the prostate has to be considered an inter- and intrafractionally moving target due to permanent changes in bladder and rectum filling [10]. Motion of the prostate has been analysed e.g. by MR imaging. Padhani et al. have shown by cine MRI measurements a significant displacement in the antero-posterior direction [11]. Ghilezan et al. have shown a correlation between rectal filling and intrafraction motion [12]. Similar data were provided by Mah et al. and Nichol et al. [13, 14].
Intensity Modulated RadioTherapy (IMRT) allows dose escalation with creation of steep dose gradients [15]. Since a step-and-shoot IMRT treatment fraction requires up to 15 minutes [16–18], intrafraction motion due to changing bowel and bladder filling might be an issue [19]. Intrafraction motion should have an impact on PTV margins [20, 21] and dose distribution [22, 23] and several approaches are currently pursued for real time target tracking for compensation [24]. Such approaches allow measuring intrafraction motion and include sonographic tracking [25], tracking based on implanted fiducials [26, 27] or beacon responders [4, 28] and even linac-mounted MRI [29].
Comprehensive 3D volumetric data are, however, scarce [12, 30–32] and data published so far may overestimate prostate mobility if an appropriate preparatory protocol is used [33].
We therefore set out to broaden the available database for patients undergoing an institutional preparatory protocol designed to reduce inter- and possibly intrafraction prostate motion comparing pre- and post-treatment on-board 3D imaging based on fiducials with a gantry-mounted cone-beam CT (CBCT; Elekta Synergy®).
Methods and patients
Patients, treatment planning and delivery
78 CBCTs of 39 fractions in 5 patients with intermediate risk prostate cancer [34, 35] were evaluated. Patients were treated with a 6 MV linear accelerator (Elekta Synergy®, Elekta Inc., Crawley, U.K.) with step-and-shoot IMRT plans (Corvus®, NAS/Nomos, Cranberry Township, USA; 45 Gy) as part of a combined protocol after 125I-seeds-implantation. Stranded 125I-seeds (Rapid Strand, Oncura, Castrop-Rauxel, Germany) were used with a diameter of 0.5 mm and a length of 3 mm. Median number of 125I-seeds was 50.
Treatment planning CT datasets were acquired and processed by each patient using an institutional policy (moderately full bladder, empty rectum using an enema before planning CT) as published previously [2, 36]. Patients were also instructed to empty their rectum and bladder and drink 500 ml water before each treatment fraction. The procedure was explained and informed consent was obtained. Typical IMRT plans consisted of 7 or 9 incident beams.
Cone-beam volume imaging and patient repositioning
Before delivering a treatment fraction, kV CBCT volume imaging was performed. Approximately 610 projection images were acquired during a 360°-rotation using the presets of Elekta (for a single projection: 120 kV, 25 mA, 40 ms). Projections were processed to 3D volume images by the XVI® (X-Ray Volume Imaging) software of Elekta using "high resolution" [36]. Patient position was corrected on-line based on matching the 125I-seeds [36] in the CBCT to the planning CT images with a small alignment clip box considering the prostate (and the 125I-seeds) only. Matching and translational position correction was performed by an automatic grey value algorithm included in the XVI software and always controlled visually by a physician. The XVI algorithm has been extensively tested by phantom-experiments regarding accuracy in case of matching based on ~50 fiducials also in case of physiologic soft tissue deformations [36, 37]. Rotational errors were not corrected. Bone position was recorded by offline matching regarding the bony structures with an alignment clip box considering the whole bony pelvis [36]. Immediately after IMRT delivery, a second CBCT imaging was performed.
Offline image analysis and data processing
The second CBCT was evaluated offline as follows: Changes in bone position (patient intrafraction movement, considering the whole pelvis; alignment clip box including the whole bony pelvis) and fiducial position (overall fiducial/prostate displacement, alignment clip box considering only the 125I-seeds/prostate) were measured by offline grey-value matching ensuring user-independence. Prostate motion relatively to the pelvic bone structures was calculated on a patient-to-patient basis.
Overall mean value (mv) and overall standard deviation (SD) and median value of all translational displacements in each direction were calculated for the matching results. Group systematic error (M), standard deviation of the systematic error (Σ) and standard deviation of the random error (σ) were calculated [38, 39]. All data were evaluated on a patient-by-patient basis.
The length of the translational displacement vector was calculated with the following formula: v = √(x2 + y2 + z2).
Results
Duration of a step-and-shoot IMRT fraction
Time between the pre- and post-treatment CBCTs was 13.6 ± 1.6 minutes (mv ± SD).
Overall intrafraction prostate displacement
Median overall displacement vector length of 125I-seeds was 3 mm (M = 3 mm, Σ = 0.9 mm, σ = 1.7 mm; M: group systematic error, Σ: SD of systematic error, σ: SD of random error).
mv ± SD of overall displacement of 125I-seeds was 0.4 ± 2 mm, 1.1 ± 3.9 mm and 1.3 ± 4.5 mm in × (left-right), y (cranio-caudal) and z (antero-posterior; AP) directions (mean length of overall displacement vector 5.1 ± 3.9 mm).
Intrafraction displacement of bony structures
Median displacement vector of bony structures was 1.84 mm (M = 2.9 mm, Σ = 1 mm, σ = 3.2 mm).
mv ± SD of displacement of bony structures was 0.2 ± 2.0 mm, -0.3 ± 1.6 mm and -0.2 ± 4.3 mm in x, y and z directions (mean length of overall displacement vector 3.1 ± 3.9 mm).
Intrafraction displacement of prostate relative to pelvic bones
Median intrafraction motion of the prostate due to changes in bladder/bowel filling (relative to bony structures) was 1.9 mm (displacement vector length; M = 3 mm, Σ = 1.3 mm, σ = 2.6 mm).
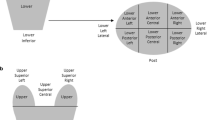
mv ± SD of intrafraction motion of the prostate due to changes in bladder/bowel filling relative to bone structures is -0.2 ± 3.2 mm, -1.5 ± 3.7 mm and -1.5 ± 4.8 mm in x, y and z directions (mean length of overall displacement vector 5.4 ± 4.8 mm). A patient example with a relative large difference in pre- and post-treatment soft tissue position due to a moderately enlarged rectum due to gas that shifted during therapy is shown on Fig. 1. The enlargement in rectal volume seen in this patient was at the limit of what is tolerated at our department. Patients with a larger difference in rectal filling between treatment planning CT are taken off the treatment table and instructed to defecate/pass gas before treatment.
Planning CT (A-C) and CBCT images of a patient immediately before (D-F) and after (G-I) an IMRT fraction. Prostate position differs due to differences in rectal filling during therapy caused by rectal gas not present on treatment planning (in this case -7.4 mm in AP, 1.1 mm in left-right and -1.0 mm in cranio-caudal directions). Planning CT was acquired due to the intitutional policy using enema. This patient marks the maximum unidirectional displacement observed. In general patients with larger differences in rectal filling between treatment planning CT and daily online cone beam CT are asked to empty their rectum and drink water before another treatment attempt.
All results are summarised in Table 1 and displacements on a patient-to-patient basis are shown on Fig 2.
Overall intrafraction motion vs bony displacement only vs soft tissue displacement. Overall intrafraction motion (blue); bony displacement only (pink) and displacement of the sof tissue structures relative to the bony anatomy (yellow) on a patient-to-patient basis in × (left-right; abscissa) and z (AP; ordinate) directions.
Discussion
Modern IGRT technologies allow precise repositioning, target-volume-visualization and even daily re-planning [40–42] before treatment delivery so that interfraction motion of various target sites in the body can be considered a solved problem [43, 44]. Patient- and organ motion, however, also has an intrafractional component which has to be considered, too. In some anatomic sites (lung- and liver tumors, upper abdominal targets), intrafraction motion can be extreme due to e.g. respiratory or cardiac motion if not addressed properly. In case of the prostate, continuous changes in bladder and bowel filling may cause a significant intrafraction motion component that is currently still accounted for by PTV margins and dose distribution. Based on measurements with the Calypso™ system, the prostate may, in some cases, move as much as > 3–5 mm already in the first 5–10 minutes of the treatment [28], however with a significant individual variation among patients [10, 28]. The percentage of patients with these extreme movements, however, is small (3D-offset exceeding 5 mm was observed in 15% of 1157 fractions in 35 observed patients, [28]) in a patient cohort that apparently underwent no specific preparatory protocol. Other groups have also published data without specifying if a preparatory protocol was used. Using 2D kV projections and 3 implanted fiducials, Letourneau et al. have shown a small intrafraction motion with a SD of 0.9 mm [31]. Wu et al. calculated the effect of intrafraction motion on dose distribution and showed that intrafraction motion worsens target coverage, its effect of course being larger for small margins than for larger margins [32]. MRI based data already suggest that intrafraction motion is smaller in comparison to interfraction motion, with an expected displacement of the prostate of < 3 mm for 20 minutes in case of patients with an empty rectum [12, 30]. However, this was not the case in patiens with a full rectum [12, 30], which underlines the importance of using institutional protocols before planning CT and each therapy fraction. We therefore set out to further evaluate this parameter in the actual treatment setting in exactly such a patient cohort that was appropriately prepared before treatment planning CT and each treatment fraction.
In this work, we analysed 3D geometric data about intrafraction motion of the prostate with pre- and post-treatment on-board imaging based on fiducials with a gantry-mounted cone-beam CT for the first time. The novelty of our data lie in the 3D online volumetric assessment of inrafraction prostate motion. We have shown that during a single step-and-shoot IMRT fraction of about 15 minutes, the overall motion of the prostate is relatively small (median displacement vector length 3 mm with a group systematic error of 3 mm). While we could not assess spurious, reversible movements of the prostate during beam-on-time, this seems to be a less relevant event based on on-line beacon data [10, 28]. To analyse the deformational component of the motion, fiducial to fiducial mapping would be very interesting, however it is not possible with the current vendor-provided XVI™ matching algorithm and was therefore not addressed because it would have comprised a large extent of manual matching. Qualitative evaluation, however, showed that the deformational component was minor in comparison to translation and tilt and the evaluation of the matching algorithm showed, that minor deformations do not affect evaluation of translation and tilt [37]. However, actually deformable matching algoritms which are able to perform a fiducial-to-fiducial based matching are being developed in our department and are planned to be subject of further work. The intrafraction motion of the prostate consists of two components: motion of the bony structures caused by e.g. relaxation of the patient, coughing, non-compliance etc., and motion of the soft tissue structures relative to the bone due to e.g. changing bowel or bladder filling. The bony motion component can be minimized by patient education and improved immobilisation techniques with devices such as stereotactic body frames [45], leg holder immobilisation devices [46] or customized body pillows formed by vacuum suction [47]. The soft tissue motion relative to bony structures due to changing bowel and bladder filling can be reduced by institutional policies such as training of the patients to have an empty rectum and a relatively full bladder before each radiation session as suggested by other groups and used for our patients [33]. If pre-delivery image guidance shows that, e.g., the rectum is filled (as opposed to the planning CT), patients can be repositioned after emptying the rectum.
The extent of prostate motion is correlated to treatment delivery time [11]. Further reduction of IMRT delivery time to ~3 minutes with novel methods such as IMAT (Intensity Modulated Arc Therapy)/VMAT (Volumetric Modulated Arc Therapy) will reduce overall target motion [48–50]. Given the small magnitude of intrafractional motion and the prospect for further dramatic reduction of treatment times in the near future, the impact of this component on the compound positioning error will likely lose relative importance.
Intrafraction motion has, in addition to the translational displacement, which was analysed in this report, also rotational and deformational components [51]. Intrafraction rotation [36, 52] could possibly be compensated (if necessary) in the future with real time target tracking and treatment tables with 6 degrees of freedom (HexaPOD™). In this work, we did not analyse the interfraction motion of each individual fiducial, however, studies about inter- and intrafraction prostate deformation are currently being performed with a self-developed deformable matching algorithm at our department. While the translational intrafractional motion is small in our series and is accounted for with PTV margins of 5 mm, an additional deformational component may well be negligible. Faster treatment paradigms such as IMAT/VMAT may aid further in the reduction of PTV margins.
Conclusion
a) The median length of the displacement vector of the prostate during a ~13 min IMRT session is < 3 mm. This amount of intrafraction motion has to be considered in choosing PTV margins even in patient cohorts that undergo daily online image guidance.
b) Positioning devices reducing intrafraction bony displacements can further reduce overall intrafraction prostate motion.
c) Intrafraction motion of the prostate represented by 125I-seeds relative to bony structures is < 2 mm in patients appropriately prepared according to institutional protocols (full bladder, empty rectum). It may be further reduced by reduction of IMRT duration (e.g. by IMAT; Intensity Modulated Arc Therapy, ~ fraction time 3 minutes).
Abbreviations
- CBCT:
-
Cone-beam CT
- IMRT:
-
Intensity Modulated RadioTherapy
- IGRT:
-
Image-Guided RadioTherapy
- XVI:
-
X-ray Volume Imaging
- kV:
-
kilovoltage
- MV:
-
megavoltage
- PTV:
-
Planning Target Volume
- EPID:
-
Electronic Portal Imaging Device
- EBRT:
-
External Beam Radiation Therapy
- 3D:
-
3-dimensional
- IMAT:
-
Intensity Modulated Arc Therapy
- VMAT:
-
Volumetric Modulated Arc Therapy
- mv:
-
mean value
- SD:
-
standard deviation.
References
Fuss M, Boda-Heggemann J, Papanikolau N, Salter BJ: Image-guidance for stereotactic body radiation therapy. Med Dosim 2007, 32: 102-110.
Boda-Heggemann J, Kohler FM, Kupper B, Wolff D, Wertz H, Mai S, Hesser J, Lohr F, Wenz F: Accuracy of ultrasound-based (BAT) prostate-repositioning: a three-dimensional on-line fiducial-based assessment with cone-beam computed tomography. Int J Radiat Oncol Biol Phys 2008, 70: 1247-1255.
Fuss M, Cavanaugh SX, Fuss C, Cheek DA, Salter BJ: Daily stereotactic ultrasound prostate targeting: inter-user variability. Technol Cancer Res Treat 2003, 2: 161-170.
Willoughby TR, Kupelian PA, Pouliot J, Shinohara K, Aubin M, Roach M 3rd, Skrumeda LL, Balter JM, Litzenberg DW, Hadley SW, et al.: Target localization and real-time tracking using the Calypso 4D localization system in patients with localized prostate cancer. Int J Radiat Oncol Biol Phys 2006, 65: 528-534.
de Crevoisier R, Kuban D, Lefkopoulos D: [Image-guided radiotherapy by in-room CT-linear accelerator combination]. Cancer Radiother 2006, 10: 245-251.
Jaffray DA: Kilovoltage volumetric imaging in the treatment room. Front Radiat Ther Oncol 2007, 40: 116-131.
Pouliot J: Megavoltage imaging, megavoltage cone beam CT and dose-guided radiation therapy. Front Radiat Ther Oncol 2007, 40: 132-142.
Wertz H, Lohr F, Dobler B, Mai S, Welzel G, Boda-Heggemann J, Wenz F: Dosimetric consequences of a translational isocenter correction based on image guidance for intensity modulated radiotherapy (IMRT) of the prostate. Phys Med Biol 2007, 52: 5655-5665.
Wertz H, Lohr F, Dobler B, Mai S, Wenz F: [Dosimetric impact of image-guided translational isocenter correction for 3-D conformal radiotherapy of the prostate]. Strahlenther Onkol 2007, 183: 203-210.
Kupelian PA, Langen KM, Willoughby TR, Zeidan OA, Meeks SL: Image-guided radiotherapy for localized prostate cancer: treating a moving target. Semin Radiat Oncol 2008, 18: 58-66.
Padhani AR, Gapinski CJ, Macvicar DA, Parker GJ, Suckling J, Revell PB, Leach MO, Dearnaley DP, Husband JE: Dynamic contrast enhanced MRI of prostate cancer: correlation with morphology and tumour stage, histological grade and PSA. Clin Radiol 2000, 55: 99-109.
Ghilezan MJ, Jaffray DA, Siewerdsen JH, van Herk M, Shetty A, Sharpe MB, Zafar Jafri S, Vicini FA, Matter RC, Brabbins DS, Martinez AA: Prostate gland motion assessed with cine-magnetic resonance imaging (cine-MRI). Int J Radiat Oncol Biol Phys 2005, 62: 406-417.
Mah D, Freedman G, Milestone B, Hanlon A, Palacio E, Richardson T, Movsas B, Mitra R, Horwitz E, Hanks GE: Measurement of intrafractional prostate motion using magnetic resonance imaging. Int J Radiat Oncol Biol Phys 2002, 54: 568-575.
Nichol AM, Brock KK, Lockwood GA, Moseley DJ, Rosewall T, Warde PR, Catton CN, Jaffray DA: A magnetic resonance imaging study of prostate deformation relative to implanted gold fiducial markers. Int J Radiat Oncol Biol Phys 2007, 67: 48-56.
Cahlon O, Hunt M, Zelefsky MJ: Intensity-modulated radiation therapy: supportive data for prostate cancer. Semin Radiat Oncol 2008, 18: 48-57.
Munter MW, Debus J, Hof H, Nill S, Haring P, Bortfeld T, Wannenmacher M: Inverse treatment planning and stereotactic intensity-modulated radiation therapy (IMRT) of the tumor and lymph node levels for nasopharyngeal carcinomas. Description of treatment technique, plan comparison, and case study. Strahlenther Onkol 2002, 178: 517-523.
Schafer M, Munter M, Sterzing F, Haring P, Rhein B, Debus J: Measurements of characteristics of time pattern in dose delivery in step-and-shoot IMRT. Strahlenther Onkol 2005, 181: 587-594.
Thilmann C, Zabel A, Milker-Zabel S, Schlegel W, Wannenmacher M, Debus J: Number and orientation of beams in inversely planned intensity-modulated radiotherapy of the female breast and the parasternal lymph nodes. Am J Clin Oncol 2003, 26: e136-143.
Huang E, Dong L, Chandra A, Kuban DA, Rosen II, Evans A, Pollack A: Intrafraction prostate motion during IMRT for prostate cancer. Int J Radiat Oncol Biol Phys 2002, 53: 261-268.
Beltran C, Herman MG, Davis JB: Planning target margin calculations for prostate radiotherapy based on intrafraction and interfraction motion using four localization methods. Int J Radiat Oncol Biol Phys 2008, 70: 289-295.
Litzenberg DW, Balter JM, Hadley SW, Sandler HM, Willoughby TR, Kupelian PA, Levine L: Influence of intrafraction motion on margins for prostate radiotherapy. Int J Radiat Oncol Biol Phys 2006, 65: 548-553.
Keall PJ, Lauve AD, Hagan MP, Siebers JV: A strategy to correct for intrafraction target translation in conformal prostate radiotherapy: simulation results. Med Phys 2007, 34: 1944-1951.
Li HS, Chetty IJ, Enke CA, Foster RD, Willoughby TR, Kupellian PA, Solberg TD: Dosimetric consequences of intrafraction prostate motion. Int J Radiat Oncol Biol Phys 2008, 71: 801-812.
Li G, Citrin D, Camphausen K, Mueller B, Burman C, Mychalczak B, Miller RW, Song Y: Advances in 4D Medical Imaging and 4D Radiation Therapy. Technol Cancer Res Treat 2008, 7: 67-82.
Krupa A, Fichtinger G, Hager GD: Real-time tissue tracking with B-mode ultrasound using speckle and visual servoing. Med Image Comput Comput Assist Interv Int Conf Med Image Comput Comput Assist Interv 2007, 10: 1-8.
Kotte AN, Hofman P, Lagendijk JJ, van Vulpen M, Heide UA: Intrafraction motion of the prostate during external-beam radiation therapy: analysis of 427 patients with implanted fiducial markers. Int J Radiat Oncol Biol Phys 2007, 69: 419-425.
Madsen BL, Hsi RA, Pham HT, Presser J, Esagui L, Corman J, Myers L, Jones D: Intrafractional stability of the prostate using a stereotactic radiotherapy technique. Int J Radiat Oncol Biol Phys 2003, 57: 1285-1291.
Langen KM, Willoughby TR, Meeks SL, Santhanam A, Cunningham A, Levine L, Kupelian PA: Observations on Real-Time Prostate Gland Motion Using Electromagnetic Tracking. Int J Radiat Oncol Biol Phys 2008,71(4):1084-1090.
Lagendijk JJ, Raaymakers BW, Raaijmakers AJ, Overweg J, Brown KJ, Kerkhof EM, Put RW, Hardemark B, van Vulpen M, Heide UA: MRI/linac integration. Radiother Oncol 2008, 86: 25-29.
Ghilezan M, Yan D, Liang J, Jaffray D, Wong J, Martinez A: Online image-guided intensity-modulated radiotherapy for prostate cancer: How much improvement can we expect? A theoretical assessment of clinical benefits and potential dose escalation by improving precision and accuracy of radiation delivery. Int J Radiat Oncol Biol Phys 2004, 60: 1602-1610.
Letourneau D, Martinez AA, Lockman D, Yan D, Vargas C, Ivaldi G, Wong J: Assessment of residual error for online cone-beam CT-guided treatment of prostate cancer patients. Int J Radiat Oncol Biol Phys 2005, 62: 1239-1246.
Wu Q, Ivaldi G, Liang J, Lockman D, Yan D, Martinez A: Geometric and dosimetric evaluations of an online image-guidance strategy for 3D-CRT of prostate cancer. Int J Radiat Oncol Biol Phys 2006, 64: 1596-1609.
Nuver TT, Hoogeman MS, Remeijer P, van Herk M, Lebesque JV: An adaptive off-line procedure for radiotherapy of prostate cancer. Int J Radiat Oncol Biol Phys 2007, 67: 1559-1567.
Frank SJ, Grimm PD, Sylvester JE, Merrick GS, Davis BJ, Zietman A, Moran BJ, Beyer DC, Roach M 3rd, Clarke DH, et al.: Interstitial implant alone or in combination with external beam radiation therapy for intermediate-risk prostate cancer: a survey of practice patterns in the United States. Brachytherapy 2007, 6: 2-8.
Sylvester JE, Blasko JC, Grimm PD, Meier R, Malmgren JA: Ten-year biochemical relapse-free survival after external beam radiation and brachytherapy for localized prostate cancer: the Seattle experience. Int J Radiat Oncol Biol Phys 2003, 57: 944-952.
Boda-Heggemann J, Kohler F, Wertz H, Welzel G, Riesenacker N, Schafer J, Lohr F, Wenz F: Fiducial-based quantification of prostate tilt using cone beam computer tomography (CBCT). Radiother Oncol 2007, 85: 247-250.
Kohler FM, Boda-Heggemann J, Kupper B, Wolff D, Frommrich-Ross D, Lohr F, Wenz F: Accuracy of a commercially available algorithm for multiple fiducial-based grey value matching by cone-beam CT. Strahlenther Onkol 2008, 184: 96.
Bijhold J, Lebesque JV, Hart AA, Vijlbrief RE: Maximizing setup accuracy using portal images as applied to a conformal boost technique for prostatic cancer. Radiother Oncol 1992, 24: 261-271.
van Herk M: Errors and margins in radiotherapy. Semin Radiat Oncol 2004, 14: 52-64.
Boggula R, Wertz H, Lorenz F, Abo Madyan Y, Boda-Heggemann J, Schneider F, Polednik M, Hesser J, Lohr F, Wenz F: A Proposed Strategy To Implement CBCT Images For Replanning and Dose Calculations. Int J Radiat Oncol Biol Phys 2007, 69: S655-S656.
Nijkamp J, Pos FJ, Nuver TT, de Jong R, Remeijer P, Sonke JJ, Lebesque JV: Adaptive radiotherapy for prostate cancer using kilovoltage cone-beam computed tomography: first clinical results. Int J Radiat Oncol Biol Phys 2008, 70: 75-82.
Yang Y, Schreibmann E, Li T, Wang C, Xing L: Evaluation of on-board kV cone beam CT (CBCT)-based dose calculation. Phys Med Biol 2007, 52: 685-705.
Verellen D, De Ridder M, Storme G: A (short) history of image-guided radiotherapy. Radiother Oncol 2008, 86: 4-13.
Verellen D, Ridder MD, Linthout N, Tournel K, Soete G, Storme G: Innovations in image-guided radiotherapy. Nat Rev Cancer 2007, 7: 949-960.
Herfarth KK, Pirzkall A, Lohr F, Schulz-Ertner D, Spoo J, Frank C, Bahner ML, Pastyr O, Debus J: [First experiences with a noninvasive patient set-up system for radiotherapy of the prostate]. Strahlenther Onkol 2000, 176: 217-222.
Baumert BG, Zagralioglu O, Davis JB, Reiner B, Luetolf UM, Ciernik IF: The use of a leg holder immobilisation device in 3D-conformal radiation therapy of prostate cancer. Radiother Oncol 2002, 65: 47-52.
Wang L, Jacob R, Chen L, Ma C, Movsas B, Feigenberg S, Konski A: Stereotactic IMRT for prostate cancer: setup accuracy of a new stereotactic body localization system. J Appl Clin Med Phys 2004, 5: 18-28.
Otto K: Volumetric modulated arc therapy: IMRT in a single gantry arc. Med Phys 2008, 35: 310-317.
Stieler F, Lohr F, Wolff D, Steil V, Abo-Madyan Y, Wenz F, Mai S: Imat vs Step-and-shoot Imrt vs. 3D-Rt for integral treatment of pelvis and inguinal lymph nodes in anal cancer. Strahlenther Onkol 2008, 184: 77.
Wolff D, Stieler F, Lohr F, Polednik M, Steil V, Abo-Madyan Y, Wenz F: Vergleich der Intensitätsmodulierten Arc Therapie (IMAT) mit der seriellen Tomotherapie und Step-and-Shoot IMRT für die Bestrahlung des Prostatakarzinoms hinsichtlich Effizienz und Planqualität. Strahlenther Onkol 2008, 184: 56.
Deurloo KE, Steenbakkers RJ, Zijp LJ, de Bois JA, Nowak PJ, Rasch CR, van Herk M: Quantification of shape variation of prostate and seminal vesicles during external beam radiotherapy. Int J Radiat Oncol Biol Phys 2005, 61: 228-238.
Rijkhorst EJ, van Herk M, Lebesque JV, Sonke JJ: Strategy for online correction of rotational organ motion for intensity-modulated radiotherapy of prostate cancer. Int J Radiat Oncol Biol Phys 2007, 69: 1608-1617.
Acknowledgements
Parts of these studies were supported by research grants from Elekta Inc. We thank Ulrike Danter for excellent technical assistance with XVI®.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
This work was partially supported by grants from Elekta GmbH, Hamburg, Germany.
Authors' contributions
JBH conceived the study, drafted the manuscript the supervised data acquisition. NR and BK acquired data, FMK evaluated the CBCTs offline. HW, ME and BH acquired data and were involved in data analysis. FL and FW supervised the project and finalized the manuscript together with JBH.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Boda-Heggemann, J., Köhler, F.M., Wertz, H. et al. Intrafraction motion of the prostate during an IMRT session: a fiducial-based 3D measurement with Cone-beam CT. Radiat Oncol 3, 37 (2008). https://doi.org/10.1186/1748-717X-3-37
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1748-717X-3-37