Abstract
Background
Traumatic perforation of the distal oesophagus due to blunt trauma is a very rare condition and is still associated with a significant morbidity and mortality. This is further exacerbated by delayed diagnosis and management as symptoms and signs are often masked by or ascribed to more common blunt thoracic injuries.
Case report
We present a case of a distal oesophageal perforation, secondary to a fall from a third storey window, which was masked by concomitant thoracic injuries and missed on both computed tomography imaging and laparotomy. The delay in his diagnosis significantly worsened the patient's recovery by allowing the development of an overwhelming chest sepsis that contributed to his death.
Conclusion
Early identification of an intrathoracic oesophageal perforation requires deliberate consideration and is essential to ensure a favorable outcome. Treatment should be individualised taking into account the nature of the oesophageal defect, time elapsed from injury and the patient's general condition.
Similar content being viewed by others
Background
Oesophageal perforation may result from iatrogenic, penetrating or blunt trauma. Most are secondary to oesophageal instrumentation and occur predominantly in the cervical oesophagus. Penetrating trauma accounts for 20–25%. Blunt trauma accounts for less than 10% of all oesophageal injuries. Perforation of the intrathoracic oesophagus is an extremely rare event [1, 2], with an incidence at less than 0.2% [2–4]. The most recent review by Monzon et al found only sixteen cases in the world literature [5].
Oesophageal perforation is a serious injury to the gastrointestinal tract. Mortality rates of between 5–30% [6–8] are worsened by a delay in diagnosis: treatment after 24 hours can increase mortality to up to 50% [9, 10].
The mechanism of thoracic oesophageal perforation in blunt trauma is unclear. The most commonly accepted theory, similar to the mechanism in Boerhaave syndrome, is an increase in intraluminal pressure against a closed glottis. This results in a tear at the weakest point of the oesophageal wall; usually the distal third of the oesophagus on the left. Other theories include; disruption of the oesophageal blood supply resulting in ischemia and late perforation, or a blast effect caused by a concomitant tracheal injury. Direct injury may also result from thoracic spine fractures or compression between the sternum and thoracic spine, as observed in high-speed road traffic accidents [5, 11–14].
We outline the case of a patient who suffered a distal oesophageal rupture and discuss the pitfalls of management.
Case Report
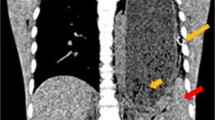
A 28 yr old male jumped from his burning apartment on the third floor. On admission he was resuscitated according to ATLS. On examination he was conscious with chest compression tenderness, a diffusely tender abdomen and bilateral lower limb fractures. Cervical spine, lumbar spine, pelvis and calcaneal films were all normal. A computed tomography (CT) chest and abdomen revealed bilateral pneumothoraces, air and haematoma within the mediastinum but no signs of a thoracic aorta rupture (Figure 1A and 1B). A significant amount of intraperitoneal air was noted. Following resuscitation and bilateral thoracotomy tubes he was taken to theatre for a urgent laparotomy. Despite a thorough search by an experienced surgeon no hollow viscus injury was found. Post operatively in ITU the patients condition continued to deteriorate. A repeat CT scan showed progressive extensive mediastinitis. An upper gastrointestinal endoscopy was performed. This revealed bilateral full thickness tears at the lower end of the oesophagus. The patient was then taken to theatre for thoracotomy and re-laparotomy Extensive lacerations to the distal oesophagus were identified. The degree of mediastinitis and extent of oesophageal injury precluded primary repair. An oesophagectomy and cervical oesophagostomy was performed. A decompressive gastrostomy and feeding jejunostomy were fashioned. A third procedure to washout his mediastinum and re-site chest drains before his condition stabilised. Five days later, he deteriorated suddenly; fresh bleeding was observed via his chest drains and despite an emergency thoracotomy the patient died. The autopsy showed a pericardiac tamponade.
Discussion
Patients with oesophageal perforation may present with a constellation of symptoms including; dysphagia, odynophagia, chest pain, and dyspnoea. Tachycardia, pyrexia, worsening surgical emphysema and progressive sepsis may follow [11, 12]. This case was unusual in that free intraperitonal air was identified in conjunction with a pneumomediastinum and bilateral pneumothoraces. The thoracic findings were attributed to his bilateral rib fractures and/or lung tauma. A laparotomy was performed to identify an intra-abdominal hollow viscus perforation. When no obvious perforation was identified at laparotomy the free intraperitoneal air was attributed to passage of air from the pleural space into the abdomen via anterior and posterior trans-diaphragmatic pathways [15, 16].
For the diagnosis of oesophageal rupture the investigation of choice is a water-soluble contrast swallow. This requires a cooperative patient. Combative patients or those requiring intensive support and ventilation are ill-suited. Moreover under these conditions 10–40% of contrast swallows give a false-negative result [8, 17, 18]. Thoracic CT can identify the sequelae of oesophageal perforation, identified by an area of oesophageal wall thickening and or mediastinal air, but this is often obscured by oedema or haemorrhage [12] Mediastinal air is not uncommon in the polytrauma patient. CT is the most accurate method for illustrating para-oesophageal manifestations of rupture such as mediastinal collections, abscesses and effusions [17, 19, 20]. CT is a poor investigation to detect the presence or site of an oesophageal rupture. When a swallow is technically impossible or where a high index of suspicion remains despite a negative oesophagogram, flexible oesophagoscopy should be used. This is a widely available investigation allowing direct visualisation of the oesophageal mucosa. A sensitivity of 70–100% and a specificity of 96% [17] with a morbidity rate of only 0.2% [21, 22]. It is thus a safe and effective method for both detection and exclusion of suspected oesophageal trauma.
Management options for oesophageal injuries are conservative or surgical and are summarised in Table 1.
In this case the degree of mediastinal sepsis and extent of oesophageal injury precluded primary repair. Resection of the severely damaged oesophagus and cervical oesophagostomy was deemed the most appropriate treatment. However, the patient died from multi-organ failure secondary to overwhelming sepsis, of which a contributing factor must have been the delay in diagnosis of his oesophageal injury.
Conclusion
Rupture of the oesophagus due to blunt trauma is rare. Intraperitoneal air following blunt trauma cannot be ignored. On table endoscopy at the first operation would have been diagnostic. It is vital to achieve an early diagnosis to limit thoracic contamination and improve survival.
References
Glatterer MS, Toon RS, Ellestad C, McFee AS, Rogers W, Macj JW, Trinkle KJ, Grover FL: Management of blunt and penetrating external esophageal trauma. J Trauma. 1985, 25: 784-791.
Beal SL, Pottmeyer EW, Spisso JM: Esophageal perforation following blunt trauma. J Trauma. 1988, 28: 1425-1432.
Kemmerer WT, Eckert WG, Gaithright JB, Reemtsma K, Creech O: Patterns of thoracic injuries in fatal traffic accidents. J Trauma. 1961, 1: 595-599.
Wilson RF, Gibson DB, Antonenko D: Shock and acute respiratory failure after chest trauma. J Trauma. 1977, 17: 697-705.
Monzon JR, Ryan B: Thoracic esophageal perforation secondary to blunt trauma. J Trauma. 2000, 49: 1129-1131.
Whyte RI, Iannettoni MD, Orringer MB: Intrathoracic esophageal perforation. The merit of primary repair. J Thorac Cardiovasc Surg. 1995, 109 (1): 140-144. 10.1016/S0022-5223(95)70429-9. discussion 144–146
Cohn HE, Hubbard A, Patton G: Management of esophageal injuries. Ann Thorac Surg. 1989, 48 (2): 309-314.
Pate JW: Tracheobronchial and esophageal injuries. Surg Clin North Am. 1989, 69 (1): 111-123.
Brewer LA, Carter R, Mulder GA, Stiles QRl: Options in the management of perforations of the esophagus. Am J Surg. 1986, 152 (1): 62-69. 10.1016/0002-9610(86)90144-3.
Bladergroen MR, Lowe JE, Postlethwait RW: Diagnosis and recommended management of esophageal perforation and rupture. Ann Thorac Surg. 1986, 42 (3): 235-239.
Sartorelli KH, McBride WJ, Vane DW: Perforation of the intrathoracic esophagus from blunt trauma in a child: case report and review of the literature. J Pediatr Surg. 1999, 34 (3): 495-7. 10.1016/S0022-3468(99)90511-0.
Moreno-Ramos MD, Serrano BV: Distal esophageal perforation secondary to blunt trauma diagnosed by computed tomography. European Journal of Radiology Extra. 2004, 51 (3): 91-127. 10.1016/j.ejrex.2004.06.006.
Ketai L, Brandt MM, Schermer C: Nonaortic mediastinal injuries from blunt chest trauma. J Thorac Imaging. 2000, 15 (2): 120-127. 10.1097/00005382-200004000-00007.
Stothert JC, Buttorff J, Kaminski DL: Thoracic esophageal and tracheal injury following blunt trauma. J Trauma. 1980, 20 (11): 992-995.
Koh ES, Chapeikin G: Anterior infradiaphragmatic free gas following bronchial rupture: case report and literature review. Australas Radiol. 2004, 48 (1): 58-60. 10.1111/j.1440-1673.2004.01244.x.
Balthazar EJ, Moore SL: CT evaluation of infradiaphragmatic air in patients treated with mechanically assisted ventilation: a potential source of error. AJR Am J Roentgenol. 1996, 167 (3): 731-734.
Flowers JL, Graham SM, Ugarte MA, Sartor WM, Rodriquez A, Gens DR, Imbembo AL, Gann DS: Flexible endoscopy for the diagnosis of esophageal trauma. J Trauma. 1996, 40 (2): 261-265. discussion 265–6
Wood J, Fabian TC, Mangiante EC: Penetrating neckinjuries: recommendations for selective management. J Trauma. 1989, 29 (5): 602-605.
Rubesin SE, Levine MS: Radiological diagnosis of gastrointestinal perforation. Radiol Clin North Am. 2003, 41 (6): 1095-115. 10.1016/S0033-8389(03)00100-3.
Ghahremani GG: Radiologic evaluation of suspected gastrointestinal perforations. Radiol Clin North Am. 1993, 31 (6): 1219-1234.
Habr-Gama A, Waye JD: Complications and hazards of gastrointestinal endoscopy. World J Surg. 1989, 13 (2): 193-201. 10.1007/BF01658399.
Mellinger JD: Upper gastrointestinal endoscopy: current status. Semin Laparosc Surg. 2003, 10 (1): 3-12.
Cameron JL, Kieffer RF, Hendrix TR, Mehigan DG, Baker RR: Selective nonoperative management of contained intrathoracic esophageal disruptions. Ann Thorac Surg. 1979, 27 (5): 404-408.
Bufkin BL, Miller JI, Mansour KA: Esophageal perforation: emphasis on management. Ann Thorac Surg. 1996, 61 (5): 1447-1451. 10.1016/0003-4975(96)00053-7. discussion 1451–1452
Vogel SB, Rout WR, Martin TD, Abbitt PL: Esophageal perforation in adults: aggressive, conservative treatment lowers morbidity and mortality. Ann Surg. 2005, 241 (6): 1016-1021. 10.1097/01.sla.0000164183.91898.74. discussion 1021–1023
Gupta NM, Kaman L: Personal management of 57 consecutive patients with esophageal perforation. Am J Surg. 2004, 187 (1): 58-63. 10.1016/j.amjsurg.2002.11.004.
Wang N, Razzouk AJ, Safavi A, Gan K, Van Arsdell GS, Burton PM, Fandrich BL, Wood MJ, Hill AC, Vyhmeister EE, Miranda R, Ahn C, Gundry SR: Delayed primary repair of intrathoracic esophageal perforation: is it safe?. J Thorac Cardiovasc Surg. 1996, 111 (1): 114-121. 10.1016/S0022-5223(96)70407-5. discussion 121–122
Orringer MB, Stirling MC: Esophagectomy for esophageal disruption. Ann Thorac Surg. 1990, 49 (1): 35-42. discussion 42–43
Acknowledgements
Written consent was obtained from the patient's relatives in order to publish this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
DCS Collected data, literature review and drafted the original manuscript
RT Collected data and drafted the original manuscript
RCM Conceived idea for manuscript and acts as guarantor of manuscript
All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Strauss, D.C., Tandon, R. & Mason, R.C. Distal thoracic oesophageal perforation secondary to blunt trauma: Case report. World J Emerg Surg 2, 8 (2007). https://doi.org/10.1186/1749-7922-2-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1749-7922-2-8