Abstract
Objective
HER-MES was the first head-to-head, phase 4 trial to assess the tolerability and effectiveness of erenumab against standard of care treatment (topiramate). This post hoc analysis compared the efficacy of erenumab with topiramate in patients who completed the trial on study medication.
Methods
Post hoc sensitivity analysis was performed using the full analysis set. Outcomes assessed included the proportion of patients with a ≥50% reduction in monthly migraine days (MMD) from baseline (50% responder rate), over the last 3 months (months 4, 5, and 6) of the double-blind treatment phase (DBTP), the 50% responder rate during the first month of the DBTP, and change from baseline in MMD during the DBTP. Multiple imputation was done for efficacy values of patients who discontinued study treatment.
Results
Patients (N = 777) were randomly assigned (1:1) to either 70 or 140 mg/month erenumab (N = 389) or 50–100 mg/day topiramate (N = 388). Of these, 334 patients (85.9%) receiving erenumab, and 231 patients (59.5%) receiving topiramate completed the DBTP on study medication. Patients on study medication until the end of the DBTP received a mean dose of 119 mg/month for erenumab and 92 mg/day for topiramate. At month 1, a significantly greater proportion of patients receiving erenumab (39.2%) reported ≥50% reduction in MMD from baseline compared with those receiving topiramate (24.0%; p < 0.001). In the last 3 months, a significantly larger proportion of patients receiving erenumab (60.3%) achieved ≥50% reduction in MMD from baseline compared with those receiving topiramate (43.3%; p < 0.001). Patients receiving erenumab demonstrated significantly greater reductions in MMD during the last 3 months from baseline versus those receiving topiramate (− 6.13 vs − 4.90; 95% CI: − 1.87 to − 0.61; p < 0.001).
Conclusions
This post hoc analysis demonstrated significantly superior efficacy of erenumab versus topiramate in achieving a ≥50% reduction in MMD with an early onset of efficacy.
Trial registration
ClinicalTrials.gov NCT03828539.
Similar content being viewed by others
Introduction
Globally, migraine is the most burdensome of all neurological diseases and is a leading cause of years lost due to disability [1, 2]. Migraine-induced disability and its impact on patient life is under-recognized and poorly understood, resulting in suboptimal treatment [3,4,5].
Although current prophylactic medications can reduce headache frequency, duration, and severity, most have been repurposed from other disease states and have not been designed to treat the underlying pathophysiology of migraine [6, 7].
Adherence and persistence to prophylactic therapy are poor, with many patients discontinuing due to safety, tolerability and/or efficacy issues [8,9,10,11]. Therefore, patients and physicians are hesitant to try prophylaxis due to the belief that unwanted side effects can occur or based on negative prior experience [12, 13].
Several drugs including beta-blockers, sodium channel modulators (topiramate and valproate) and tricyclic anti-depressants are currently being used for the preventive treatment of migraine [14, 15]. Among the oral prophylactic drugs, topiramate has a proven efficacy and safety profile based on pivotal clinical trials [16,17,18]. According to international guidelines, topiramate is recommended as a first-line medication for the preventive treatment of migraine [14, 15].
Monoclonal antibodies against calcitonin gene-related peptide (CGRP), or its receptor, offer migraine specific preventive treatment for episodic and chronic migraine (EM/CM). Treatment with erenumab, a monoclonal antibody against the CGRP receptor, was demonstrated to be safe and effective in clinical trials in patients with EM and CM and with previous preventive treatment failures [19,20,21,22,23,24,25,26].
The HER-MES (Head-to-head study of Erenumab against topiRamate – Migraine study to assess tolerability and efficacy in a patiEnt-centered Setting) study (ClinicalTrials.gov Identifier: NCT03828539) reached beyond the gold-standard of efficacy analysis in double-blind placebo-controlled trials by conveying the real-world situation into a randomized, controlled, double-blind, double-dummy, head-to-head trial that compared the effectiveness of erenumab versus topiramate [27].
Tolerability of the study medication was the primary endpoint in the HER-MES study, and efficacy endpoints were analyzed in composite populations with patients on therapy and patients who had stopped medication but continued daily reporting. The results showed a superior effectiveness of erenumab over topiramate by means of better tolerability and higher efficacy [27].
However, when it comes to deciding upon a specific treatment, physicians require data about the actual treatment efficacy in patients who continue on active medication to compare therapies – an unmet need for CGRP pathway inhibitors to date. To address this need, here we describe the post hoc analysis of treatment efficacy of erenumab and topiramate in patients who tolerated the medication and were able to complete the study treatment.
This post hoc efficacy analysis assessed the 50% responder rate and the reduction in monthly migraine days (MMD) based on the results of patients who completed the HER-MES study on the study medications [27].
Methods
Study design
HER-MES (NCT03828539) was a 24-week, randomized, double-blind, double-dummy, active-controlled, parallel-group, phase 4 trial conducted in Germany that compared the tolerability and effectiveness of erenumab (70 mg or 140 mg QM) with topiramate (titrated to 50-100 mg/day). The primary endpoint, the proportion of patients who discontinued erenumab or topiramate due to an adverse event (AE) during the double-blind treatment phase (DBTP), has been reported in an earlier publication [27]. Details of the study design, randomization, and primary analysis have been reported previously [27].
Patients
The eligibility criteria for HER-MES have been previously described [27]. Briefly, HER-MES enrolled adult patients (18–65 years) with a history of EM or CM, as defined by the International Classification of Headache Disorders, 3rd edition [28], for at least 12 months prior to screening.
Patients were eligible if they were either naive to prophylactic migraine treatment or had failed or had not been suitable for up to three of the following treatments: metoprolol/propranolol, amitriptyline, or flunarizine. Eligibility for randomization was assessed based on migraine frequency and electronic diary (eDiary) compliance (≥80% eDiary compliance) during the baseline phase. Patients previously treated with topiramate, any drug targeting the CGRP pathway, valproate, or onabotulinumtoxin A were excluded.
Information about the duration and severity of headache days – migraine and non-migraine – as well as use of rescue medication was recorded in an eDiary by the patients [27].
Outcomes
The post hoc sensitivity analysis was performed on the full analysis set population (FAS) for pre-specified outcomes: i) the proportion of patients with a ≥ 50% reduction in MMD from baseline (50% responder rate), over the last 3 months (months 4,5 and 6) of the DBTP, ii) the 50% responder rate during the first month of the DBTP and iii) the change from baseline in MMD during the DBTP. Additionally, we present the proportion of patients with a ≥ 50% reduction in MMD from baseline over the last 3 months amongst the subgroup of patients completing the DBTP on study medication (true completers).
Statistical analysis
The FAS comprised all randomized patients who received at least one dose of the double-blind study medication.
In this post hoc sensitivity analysis, the efficacy of erenumab versus topiramate in patients who completed treatment with study medication was evaluated (true completers). However, this analysis would impair the randomization due to unequal discontinuation rates between the two treatment groups. To preserve the randomization, multiple imputation was conducted based on the data of patients who stayed on medication during the entire 24 weeks of the treatment phase. For those patients who discontinued the study medication, prospective data were imputed as if they had been able to stay on medication as well. Missing values from patients who discontinued the study were also imputed.
For the proportion of patients who achieved at least a 50% reduction in MMD, the odds ratio (OR) was calculated using a logistic regression model with categorical variables of treatment and stratification factor (MMD at baseline: 4–7 days, 8–14 days, ≥15 days).
The analysis model included the factors treatment, scheduled visit, and the stratification factor (MMD at baseline: 4–7 days, 8–14 days, ≥15 days). An unstructured covariance matrix for the random effects was assumed.
Statistical analyses were performed using SAS (version 9.2). Since both study drugs used are already on the market, no data monitoring committee was required.
Ethics approval
At each trial center, the study protocol and its amendments were approved by an independent local ethics committee. Details of the study protocol and its amendments have been reported previously [27]. This study was conducted in compliance with Good Clinical Practice (GCP). Patients were informed according to GCP guidelines and provided written consent to participate in the trial.
The data were partly presented in abstract form at the International Headache Congress International Headache Society and European Headache Federation joint congress 2021 [29].
Results
Results from the HER-MES trial
Overall, of the 777 patients who were randomized (1:1) between February 2019 and July 2020, 389 patients were allocated to the erenumab group and 388 to the topiramate group. One patient in the erenumab group did not receive study medication and was therefore excluded from the analysis.
The treatment groups, reasons for treatment or study discontinuation and patients included in the post hoc analysis are presented in Fig. 1.
HER-MES demonstrated a favorable tolerability of erenumab over topiramate, as significantly less patients discontinued medication due to AEs in the erenumab group (10.6%) than in the topiramate group (38.9%) during the DBTP of the trial (OR: 0.19; 95% confidence interval [CI]: 0.13; 0.27; p < 0.001).
The primary analysis of the HER-MES results also showed that significantly more patients in the erenumab group achieved a ≥ 50% reduction in MMD from baseline (over the last 3 months of DBTP), demonstrating better efficacy of erenumab (55.4% vs 31.2%; OR: 2.76; 95% CI: 2.06; 3.71; p < 0.001) [27].
Post hoc efficacy analysis
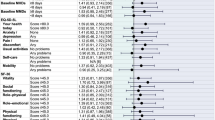
Patients on study medication until the end of the DBTP received a mean dose of 92 mg/day of topiramate (n = 231) and 119 mg/month of erenumab (n = 334). In the erenumab group, 60.3% (234/388) of patients achieved at least a 50% reduction in MMD during the last 3 months of the DBTP versus 43.3% (168/388) in the topiramate group (95% CI: 1.48; 2.76; p < 0.001). A significant difference was observed from month 1 of the DBTP with 39.2% (152/388) of patients in the erenumab group versus 24.0% (93/388) in the topiramate group (95% CI: 1.49; 2.84; p < 0.001) achieving at least a 50% reduction in MMD. Throughout the course of the DBTP, the odds of achieving at least a 50% reduction in MMD was about two times higher in the erenumab group compared to the topiramate group (Fig. 2).
The result of this post hoc efficacy analysis using the multiple imputation approach is similar to the 50% responder rate in true completers of the DBTP. In this subgroup of patients who stayed on treatment until study completion without multiple imputation (true completers), and thus breaking the randomization, 60.8% (203/334) of patients in the erenumab group and 45.9% (106/231) in the topiramate group achieved at least a 50% reduction in MMD during the last 3 months (months 4-6) of the DBTP (OR: 1.81; 95% CI: 1.29; 2.56).
Effects of erenumab and topiramate on MMD
The mean number of MMD at baseline was 10.34 (4.05) days for erenumab and 10.46 (3.78) for the topiramate group. The mean change from baseline in MMD over the last 3 months (month 4, 5 and 6) of the DBTP was significantly higher in the erenumab group (− 6.13 days) compared to the topiramate group (− 4.90 days), with a mean difference of − 1.24 days (95% CI: − 1.87; − 0.61 days; p < 0.001; Table 1).
During the first month of the DBTP, a significant difference in the MMD could be observed between erenumab (− 4.09 days) and topiramate (− 2.77 days: mean difference: − 1.32; 95% CI: − 1.96; − 0.68 days; p < 0.001). This analysis confirms the early onset of efficacy of erenumab as reported in several previous studies [30, 31] and the difference was maintained over the entire DBTP (Fig. 3).
Discussion
The HER-MES post hoc analysis is the first direct head-to-head comparison in patients with migraine who completed 6 months of study treatment with either erenumab, a monoclonal antibody against the CGRP receptor, or topiramate, an oral medication for migraine prophylaxis. Erenumab led to a greater reduction in MMD from the first month onwards and demonstrated superiority in the proportion of patients who achieved a ≥ 50% reduction in MMD.
HER-MES was designed to assess the effectiveness of erenumab compared with topiramate [27]. Effectiveness is the combination of tolerability and efficacy, and it currently represents the best approximation of clinical reality under a controlled, randomized, double-blind study setting [32].
Most clinical trials focus on treatment efficacy as this is a requirement by regulatory authorities, imputing missing values due to tolerability issues via statistical methods like last observation carried forward (LOCF) or, more accurately, using multiple imputation. Consequently, for the HER-MES trial, describing for the first-time superior effectiveness of an anti-CGRP pathway inhibitor in a head-to-head trial approach, the question was raised as to whether the efficacy in patients who tolerated the study drug is also superior for erenumab. Therefore, we focused this analysis on the efficacy of erenumab versus topiramate in patients who completed 24 weeks on the study medication.
In this post hoc analysis of the HER-MES study, erenumab has shown superior efficacy over topiramate. Superiority was achieved from month 1 until the end of the DBTP, with an OR of 2.02 for the proportion of patients achieving a ≥ 50% reduction in MMD during the last 3 months from baseline. The early onset of superior efficacy from month 1 onwards can be explained by different aspects. Based on the s.c. mode of application the maximal plasma concentration of erenumab is much earlier reached as compared to topiramate, which needs to be up-titrated in order to reach a sufficient Cmax. In addition, monoclonal antibodies typically have a high affinity to their binding site which may also contribute to rapid onset of activity. Finally, due to the specificity of erenumab and very little unwanted effects, this monoclonal antibody can be administered in an efficacious dose from the start of therapy.
The average dose of topiramate in this post hoc analysis was 92 mg, which is rarely achieved in clinical practice due to tolerability issues.
Hence, presented data comprised patients who showed efficacy in a dose of 92 mg of topiramate, which is within the recommended range of topiramate for migraine prevention [16,17,18]. In addition, the results demonstrated that topiramate was an effective therapy for migraine patients tolerating the drug despite not as efficacious as erenumab.
In order to perform this analysis, only the values of patients on study medication were included. Data collected from patients after drug discontinuation were not incorporated. All missing efficacy values were replaced by multiple imputations based on efficacy results from patients on study drug to maintain randomization. Efficacy values were imputed for 40% of the patients on topiramate and 10% on erenumab. The result of this analysis using multiple imputation is similar to the 50% responder rate in true completers, while having the advantage of preserving the randomization of the study population.
Prior to this study, only a few direct comparisons of oral migraine prophylactics had been conducted [33]. The benefits of anti-CGRP pathway therapies were known from placebo-controlled trials [19,20,21,22,23,24,25,26]. The assumptions for the superior effects of anti-CGRP pathway monoclonal antibodies over oral migraine preventive therapies were derived from indirect comparisons only [34,35,36]. Here, we demonstrate the superior efficacy of an anti-CGRP pathway monoclonal antibody compared to an oral migraine prophylactic based on clinical head-to-head trial data for the first time.
Conclusions
The HER-MES post hoc analysis confirmed the superior efficacy of erenumab over topiramate for patients on study medication, with a higher proportion of patients achieving a ≥ 50% reduction in MMD, reduction of MMD from baseline, and an early onset of action (significant superiority starting from month 1). The post hoc analysis of the HER-MES study further supports the initially published superior effectiveness results of erenumab compared with topiramate in the prevention of migraine across a broad patient population.
Availability of data and materials
The study data for the analysis described in this report may be made available on request by the author investigators or Novartis Pharma GmbH, sponsor of this clinical research.
Abbreviations
- AE:
-
Adverse event
- CGRP:
-
Calcitonin gene-related peptide
- CI:
-
Confidence interval
- CM:
-
Chronic migraine
- DBTP:
-
Double-blind treatment phase
- IHC:
-
International Headache Congress
- EHF:
-
European Headache Federation
- EM:
-
Episodic migraine
- FAS:
-
Full analysis set
- GCP:
-
Good Clinical Practice
- MMD:
-
monthly migraine days
- N:
-
Total number of patients
- N′:
-
Number of patients in the analysis
- OR:
-
Odds ratio
- RR:
-
Relative risk
- SD:
-
Standard deviation
- SE:
-
Standard error
References
Vos T, Abajobir AA, Annafati C, Abbas KM, Abate KH et al (2017) Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet 390(10100):1211–1259. https://doi.org/10.1016/S0140-6736(17)32154-2
Steiner TJ, Stovner LJ, Jensen R, Uluduz D, Katsarava Z (2020) Migraine remains second among the world’s causes of disability, and first among young women: findings from GBD2019. J Headache Pain 21(1):137. https://doi.org/10.1186/s10194-020-01208-0
Buse DC, Rupnow MF, Lipton RB (2009) Assessing and managing all aspects of migraine: migraine attacks, migraine-related functional impairment, common comorbidities, and quality of life. Mayo Clin Proc 84(5):422–435. https://doi.org/10.1016/S0025-6196(11)60561-2
Holmes WF, MacGregor EA, Sawyer JP, Lipton RB (2001) Information about migraine disability influences physicians’ perceptions of illness severity and treatment needs. Headache 41(4):343–350. https://doi.org/10.1046/j.1526-4610.2001.111006343.x
Lipton RB, Hahn SR, Cady RK, Brandes JL, Simons SE, Bain PA et al (2008) In-office discussions of migraine: results from the American Migraine Communication Study. J Gen Intern Med 23(8):1145–1151. https://doi.org/10.1007/s11606-008-0591-3
Silberstein SD, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E et al (2017) Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology 78(17):1337–1345. https://doi.org/10.1212/WNL.0b013e3182535d20
Shapiro RE (2012) Preventive treatment of migraine. Headache 52(Suppl 2):65–69. https://doi.org/10.1111/j.1526-4610.2012.02242.x
Hepp Z, Dodick DW, Varon SF, Chia J, Matthew N, Gillard P et al (2017) Persistence and switching patterns of oral migraine prophylactic medications among patients with chronic migraine: a retrospective claims analysis. Cephalagia 37(5):470–485. https://doi.org/10.1177/0333102416678382
Blumenfeld AM, Bloudek LM, Becker WJ, Buse DC, Varon SF, Maglinte GA et al (2013) Patterns of use and reasons for discontinuation of prophylactic medications for episodic migraine and chronic migraine: results from the second international burden of migraine study (IBMS-II). Headache 53(4):644–655. https://doi.org/10.1111/head.12055
Yaldo AZ, Wertz DA, Rupnow MF, Quimbo RM (2008) Persistence with migraine prophylactic treatment and acute migraine medication utilization in the managed care setting. Clin Ther 30(12):2452–2460. https://doi.org/10.1016/j.clinthera.2008.12.010
Berger A, Bloudek LM, Varon SF, Oster G (2012) Adherence with migraine prophylaxis in clinical practice. Pain Pract 12(7):541–549. https://doi.org/10.1111/j.1533-2500.2012.00530.x
Dekker F, Neven AK, Andriesse B, Kernick D, Reis R, Ferrari MD et al (2012) Prophylactic treatment of migraine; the patient’s view, a qualitative study. BMC Fam Pract 13:13. https://doi.org/10.1186/1471-2296-13-13
Dekker F, Neven AK, Andriesse B, Kernick D, Ferrari MD, Assendelft WJ (2012) Prophylactic treatment of migraine by GPs: a qualitative study. Br J Gen Pract 62(597):e268–e274. https://doi.org/10.3399/bjgp12X636100
The American Headache Society position statement on integrating new migraine treatments into clinical practice. Headache. 2019;59(1):1–18. https://doi.org/10.1111/head.13456
Steiner TJ, Jensen R, Katsarava Z, Linde M, MacGregor EA, Osipova V et al (2019) Aids to management of headache disorders in primary care (2nd edition): on behalf of the European Headache Federation and Lifting The Burden: the Global Campaign against Headache. J Headache Pain 20(1):57. https://doi.org/10.1186/s10194-018-0899-2
Silberstein SD, Neto W, Schmitt J, Jacobs D, MIGR-001 Study Group (2004) Topiramate in migraine prevention: results of a large controlled trial. Arch Neurol 61(4):490–495. https://doi.org/10.1001/archneur.61.4.490
Brandes JL, Saper JR, Diamond M, Couch JR, Lewis DW, Schmitt J et al (2004) Topiramate for migraine prevention: a randomized controlled trial. JAMA 291(8):965–973. https://doi.org/10.1001/jama.291.8.965
Diener HC, Tfelt-Hansen P, Dahlof C, Láinez MJ, Sandrini G, Wang SJ et al (2004) Topiramate in migraine prophylaxis–results from a placebo-controlled trial with propranolol as an active control. J Neurol 251(8):943–950. https://doi.org/10.1007/s00415-004-0464-6
Sun H, Dodick DW, Silberstein S, Goadsby PJ, Reuter U, Ashina M et al (2016) Safety and efficacy of AMG 334 for prevention of episodic migraine: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Neurol 15(4):382–390. https://doi.org/10.1016/S1474-4422(16)00019-3
Goadsby PJ, Reuter U, Hallstrom Y, Broessner G, Bonner JH, Zhang F et al (2017) A controlled trial of erenumab for episodic migraine. N Engl J Med 377(22):2123–2132. https://doi.org/10.1056/NEJMoa1705848
Tepper S, Ashina M, Reuter U, Brandes JL, Doležil D, Silberstein S et al (2017) Safety and efficacy of erenumab for preventive treatment of chronic migraine: a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Neurol 16(6):425–434. https://doi.org/10.1016/S1474-4422(17)30083-2
Goadsby PJ, Paemeleire K, Broessner G, Brandes J, Klatt J, Zhang F et al (2019) Efficacy and safety of erenumab (AMG334) in episodic migraine patients with prior preventive treatment failure: a subgroup analysis of a randomized, double-blind, placebo-controlled study. Cephalalgia 39(7):817–826. https://doi.org/10.1177/0333102419835459
Dodick DW, Ashina M, Brandes JL, Kudrow D, Lanteri-Minet M, Osipova V et al (2018) ARISE: a phase 3 randomized trial of erenumab for episodic migraine. Cephalalgia 38(6):1026–1037. https://doi.org/10.1177/0333102418759786
Reuter U, Goadsby PJ, Lanteri-Minet M, Wen S, Hours-Zesiger P, Ferrari MD et al (2018) Efficacy and tolerability of erenumab in patients with episodic migraine in whom two-to-four previous preventive treatments were unsuccessful: a randomised, double-blind, placebo-controlled, phase 3b study. Lancet 392(10161):2280–2287. https://doi.org/10.1016/S0140-6736(18)32534-0
Ashina M, Tepper S, Brandes JL, Reuter U, Boudreau G, Dolezil D et al (2018) Efficacy and safety of erenumab (AMG334) in chronic migraine patients with prior preventive treatment failure: a subgroup analysis of a randomized, double-blind, placebo-controlled study. Cephalgia 38(10):1611–1621. https://doi.org/10.1177/0333102418788347
Wang SJ, Roxas AA Jr, Saravia B, Kim BK, Chowdhury D, Riachi N et al (2021) Randomised, controlled trial of erenumab for the prevention of episodic migraine in patients from Asia, the Middle East, and Latin America: the EMPOwER study. Cephalalgia 41(13):1285–1297. https://doi.org/10.1177/03331024211024160
Reuter U, Ehrlich M, Gendolla A, Heinze A, Klatt J, Wen S et al (2022) Erenumab versus topiramate for the prevention of migraine - a randomised, double-blind, active-controlled phase 4 trial. Cephalalgia 42(2):108–118. https://doi.org/10.1177/03331024211053571
Headache Classification Committee of the International Headache Society (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38(1):1–211. https://doi.org/10.1177/0333102417738202
Ehrlich M, Maier-Peuschel M, Sieder C, Hentschke C, Reuter U (2021) Erenumab versus topiramate for the prevention of migraine: results of a post hoc efficacy analysis. IHS and EHF joint congress. J Headache Pain 22:103. https://doi.org/10.1186/s10194-021-01293-9
Schwedt T, Reuter U, Tepper S, Ashina M, Kudrow D, Broessner G et al (2018) Early onset of efficacy with erenumab in patients with episodic and chronic migraine. J Headache Pain 19(1):92. https://doi.org/10.1186/s10194-018-0923-6
Hirata K, Takeshima T, Sakai F, Imai N, Matsumori Y, Tatsuoka Y et al (2022) Early onset of efficacy with erenumab for migraine prevention in Japanese patients: analysis of two randomized, double-blind, placebo-controlled studies. Brain Behav 12(3):e2526. https://doi.org/10.1002/brb3.2526
Singal AG, Higgins PD, Waljee AK (2014) A primer on effectiveness and efficacy trials. Clinc Transl Gastroenterol 5(1):e45. https://doi.org/10.1038/ctg.2013.13
Kawata AK, Shah N, Poon JL, Shaffer S, Sapra S, Wilcox TK et al (2021) Understanding the migraine treatment landscape prior to the introduction of calcitonin gene-related peptide inhibitors: results from the Assessment of Tolerability and Effectiveness in MigrAINe Patients using Preventive Treatment (ATTAIN) study. Headache 61(3):438–454. https://doi.org/10.1111/head.14053
Yang CP, Zeng BY, Chang CM, Shih PH, Yang CC, Tseng PT et al Comparative effectiveness and tolerability of the pharmacology of monoclonal antibodies targeting the calcitonin gene-related peptide and its receptor for the prevention of chronic migraine: a network meta-analysis of randomized controlled trials. Neurotherapeutics 18(4):2639–2650. https://doi.org/10.1007/s13311-021-01128-0
Vandervorst F, Van Deun L, Van Dycke A, Paemeleire K, Reuter U, Schoenen J et al (2021) CGRP monoclonal antibodies in migraine: an efficacy and tolerability comparison with standard prophylactic drugs. J Headache Pain 22(1):128. https://doi.org/10.1186/s10194-021-01335-2
Overeem LH, Raffaelli B, Mecklenburg J, Kelderman T, Neeb L, Reuter U (2021) Indirect comparison of topiramate and monoclonal antibodies against CGRP or its receptor for the prophylaxis of episodic migraine: a systematic review with meta-analysis. CNS Drugs 35(8):805–820. https://doi.org/10.1007/s40263-021-00834-9
Acknowledgements
The authors would like to thank all participants, their families, and the investigators who participated in the HER-MES study for their commitment to this study. The authors would like to thank Rachna Shukla and Fatima Hasan, Novartis Healthcare Pvt. Ltd., Hyderabad, India for the medical writing and editorial assistance in accordance with the Good Publication Practice guidelines.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by Novartis Pharma GmbH, Nuremberg, Germany, who designed the study in collaboration with the investigators and provided the investigational medicinal products in a double-dummy setting, funded data analysis by Winicker Norimed GmbH and medical writing support of the methods and results sections which was done under the directions of the authors. Novartis had no role in the data collection. Employees of Novartis contributed to data interpretation and writing of the report in their role as authors. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
UR, ME, MMP, CS, and CH participated in the conceptualization of the study and were involved in the development or design of methodology. The chief investigators were UR, ME and MMP. CS, and CH were the study biostatisticians responsible for the statistical analyses. ME was the medical lead for the study. All authors were involved in the preparation, creation and/or presentation of the published work, specifically visualization/ data presentation. All authors agreed on the content of the manuscript, reviewed drafts and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol, protocol amendments, informed consent forms, and accompanying materials were reviewed and approved by the Institutional Review Board /Independent Ethics Committee and Health Authorities at each study center.
All participants provided written informed consent before undergoing any study-specific procedures.
Consent for publication
Consent for publication was received.
Competing interests
Uwe Reuter reports grants, personal fees and other from Novartis, and personal fees and other from Amgen during the conduct of the study. He reports personal fees and other from AbbVie; grants, personal fees and other from Allergan; other from Alder; personal fees and other from Eli Lilly; personal fees from Lundbeck; personal fees from Pfizer; personal fees from Medscape and StreaMedUP; grants, personal fees and other from Novartis; and personal fees from Teva Pharmaceuticals outside the submitted work.
Marc Ehrlich, Monika Maier-Peuschel, Christian Sieder, and Christian Hentschke are employees of, and hold stocks in Novartis.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ehrlich, M., Hentschke, C., Sieder, C. et al. Erenumab versus topiramate: post hoc efficacy analysis from the HER-MES study. J Headache Pain 23, 141 (2022). https://doi.org/10.1186/s10194-022-01511-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-022-01511-y