Abstract
Background
The rigors of medical education often take a toll on students' mental well-being, resulting in heightened stress, anxiety, depression, somatization, and thoughts of self-harm. This study aimed to determine the prevalence of mental health problems among Jordanian medical students (Yarmouk University), explore the links between mental state and demographic and lifestyle factors, and compare mental health profiles between pre-clinical/pre-clerkship (years 1–3) and clinical/clerkship (years 4–6) students.
Methods
An online survey was distributed to undergraduate medical students at Yarmouk University. Mental health was measured using validated tools (depression: Patient Health Questionnaire, PHQ-9; eating disorders: SCOFF; Generalized Anxiety Disorder Scale, GAD-7; Somatic Symptoms: Patient Health Questionnaire, PHQ-15; overall stress (single-item measure); ability to handle stress; stressors and coping mechanisms. Data on sociodemographic factors, academic performance, and lifestyle choices, also were collected. Bivariate and multivariable analyses evaluated the associations between academic level and mental health, accounting for sociodemographic and lifestyle factors.
Results
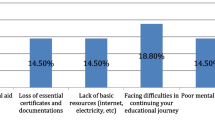
Of the 618 medical students who responded, 48.4% screened positive for depression, 36.7% for anxiety, and 63.6% for high level of stress. Slightly over half experienced somatic symptoms, and 28.6% exhibited signs of eating disorders. Roughly, 26% had suicidal thoughts, as measured by item 9 of the PHQ-9 scale. Low reported rates of healthy behaviors were observed (e.g. balanced diets, 5.7%; vigorous physical activity, 17.0%). Smoking prevalence was 24.6%, notably higher among clinical students. At the multivariable level, stress, insomnia, eating disorders and cigarette smoking were significantly associated with depression, anxiety and somatization. Higher physical activity scores were associated with lower depression risk. Females were significantly more likely than males to fall in more severe somatization categories.
Conclusion
This study highlights the need to address the alarming rates of mental health problems among Jordanian medical students. While few significant differences were observed between pre-clinical and clinical students, the high rates of depression, anxiety, stress, and negative health practices in both groups suggest the need for interventions that begin at enrollment as well as during transitions to clinical settings. Prioritizing mental health support and promoting healthier lifestyles among medical students are vital steps toward nurturing resilient, well-rounded future medical professionals.
Similar content being viewed by others
Background
Mental health problems (MHPs) refer to the existence of symptoms related to mental disorders, such as depression, anxiety, stress, or compulsive behavior [1, 2]. In young people, MHPs tend to be overlooked, and thus need to be identified and addressed in a timely manner [3]. Preventing or managing MHPs is further challenged by the observation of high rates of MHPs in those who can contribute to screening and addressing MHPs (e.g. physicians and medical students) [4, 5].
Specifically with regards to medical students, researchers have documented that medical students are more likely to experience heightened levels of stress, anxiety, depression, burnout, and suicidal thoughts [4, 6,7,8]. Mental health may be detrimentally influenced by fear of failure, academic overload, patient contact, heightened parental expectations, extensive curriculum, examinations, limited leisure time, inadequate recreational facilities, and residing in hostels [9, 10]. Conversely, healthy lifestyles have been recognized to play an important role in positively modifying physical as well as mental health [10,11,12,13].
In low-to-middle income countries in the Arab World, while there are some published studies investigating MHP in medical students [14,15,16,17], most do not examine the potential determinants of psychological morbidity of medical students in a comprehensive approach (i.e. including the various factors such as sociodemographic, academic, lifestyle-related factors as well as the multiple MHPs that may exist). In Jordan in particular, a country that has witnessed a surge in the number of students enrolled in Medical schools (as of the year 2022 19,000 medical students were enrolled in Medical schools) [18], there have been no studies to date that have simultaneously investigated the correlation and impact of sociodemographic, lifestyle, and program/training-related factors on the mental health of Jordanian medical students.
This study aimed to (1) examine the prevalence of depression, anxiety, stress, somatization, eating disorders and lifestyle practices (such as substance abuse, low/no physical activity, stress and coping strategies), and (2) assess the association of academic level (pre-clerkship/pre-clinical versus clerkship/clinical years of medical school) with MHPs (depression, anxiety, and somatization) while adjusting for lifestyle-related and sociodemographic factors. Our findings are of value to clinicians, educational experts, student advisors, and counselors seeking to improve Medical schooling in Jordan and similar countries in the Middle East. By gaining insights into the prevalence of depression, anxiety, somatic symptoms, and eating disorders as well as understanding what factors shape MHPs in medical students, appropriate interventions can be designed to prevent and effectively address mental health concerns within this student population.
Methods
Ethical review
The study was reviewed and approved by the Institutional Review Board of the King Hussein Cancer Center (study number 22 KHCC 69), an accredited body of the Association for the Accreditation of Human Research Protection Programs, Inc (AAHRPP).
Study design and setting
Our study was designed to examine differences between two naturalistic groups: medical students in basic years (pre-clerkship stage) and those in senior years (clerkship stage). Specifically, a cross-sectional study was conducted among undergraduate medical students at Yarmouk University School of Medicine in Irbid, Jordan. Yarmouk University's School of Medicine, founded in 2013, is among the six medical schools in the country. During the 2021/2022 academic year when the data collection for the study took place, Yarmouk University had an estimated total of 2,540 medical students enrolled (1,820 students in the pre-clerkship/pre-clinical stage and 720 students in the clerkship/clinical stage).
Sample size
To achieve a ± 5% accuracy and a confidence interval of 95%, with a power of 80%, a total sample size of 636 medical students (318 from each study level, i.e., pre-clerkship and clerkship) was required. This calculation was based on the number of students at the pre-clerkship group, which was 1820 students. The chosen 50% prevalence for depression was based on previous reports indicating a high prevalence of depression among medical students, ranging from 30 to 50% [19,20,21].
Recruitment strategy
A self-administered online Arabic questionnaire was created and distributed using the online platform QuestionPro (https://www.questionpro.com/). In order to ensure students completed the survey when they were not experiencing acute stressors (examinations), we distributed the survey during non-examination periods. Each cohort of students [per year of enrollment] was subscribed to a WhatsApp and Facebook group, and the survey link was distributed to students through these groups. Given the variation in examination schedules by cohort, survey links were distributed in a stepwise manner.
Measurement instrument
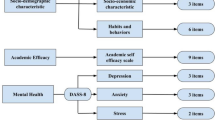
The on-line questionnaire was designed to gauge various conditions (depression, anxiety, somatization, eating disorders) and their association with clerkship status of medical students while also accounting for lifestyle factors (tobacco use, alcohol use, exercise and diet, stress, coping). Before being distributed to participants, the survey was pilot tested on 7 students, and necessary modifications were made based on the feedback received. The final questionnaire specifically measured the following aspects:
Clerkship status
Clerkship status was our main independent variable of interest. Medical students in years 1 to 3 of medical school were categorized in the pre-clinical/pre-clerkship group, while those in years 4 to 6 of medical school were categorized in the clinical/clerkship group.
Mental health
We sought to assess three specific mental health conditions: depression, anxiety and somatization. We employed the Arabic version of the Patient Health Questionnaire (PHQ) [22]. The PHQ is widely recognized as a reliable and valid diagnostic tool used in primary care settings to assesses six disorders (including depression, generalized anxiety, and somatization). Briefly, within each condition, subjects are asked to rate items (symptoms or problems) they experienced over the past few weeks. For example, when measuring depression or anxiety, subjects rate 9 symptoms or 7 symptoms (respectively) on a 4-point scale (ranging from "not at all" to "nearly every day"). When measuring somatization, subjects rate 15 symptoms on a 3-point scale (ranging from "not bothered at all" to "bothered a lot"). Raw scores are then generated for depression (scores range from 0 to 27), anxiety (scores range from 0 to 21) and somatization (scores range from 0 to 30) [23,24,25].
For the purpose of our study, the following specific modules in the Arabic PHQ were used: [22] depression (Patient Health Questionnaire-9 (PHQ9)), generalized anxiety disorder (General Anxiety Disorder-7 (GAD7)), and somatization (Patient Health Questionnaire-15 (PHQ15)). Raw scores of depression, anxiety and somatization were further categorized as follows:
-
✔ Depression (PHQ-9): A cutoff score of 10 or above (out of 27) was used to screen individuals at risk of depression (versus those at low risk). Five categories of severity of PHQ-9 scores were first generated: normal (scores of 0–4), mild depression (5–9), moderate depression (10–14), moderate to severe depression (15–19), and severe depression (20–27) [26]. However, due to limited cell counts in the two highest categories (moderate to severe depression and severe depression) we subsequently opted for a four-category approach similar to that for anxiety and somatization (i.e. normal, mild, moderate, and severe).
-
✔ Anxiety (GAD-7): A cutoff score of 10 or above (out of 21) was used to screen individuals at risk of anxiety (versus those at low risk). Categories of severity of GAD-7 scores also were generated: normal (scores of 0–4), mild anxiety (5–9), moderate anxiety (10–14), and severe anxiety (15–21) [27].
-
✔ Somatization (PHQ-15): A cutoff score of 10 or above (out of 30) was used to screen individuals at risk of experiencing somatic symptoms (versus those at low risk). Categories of severity of PHQ-15 scores also were generated: normal (0–4), mild somatization (5–9), moderate somatization (10–14), and severe somatization (15–30) [25].
Eating disorders
The Arabic version of SCOFF questionnaire, which was previously translated into Arabic and tested for validity and reliability, was used to assess eating disorders [28]. This questionnaire is comprised of five questions that specifically address the fundamental characteristics of anorexia nervosa and bulimia nervosa. Subjects are asked to respond with either "yes" or "no" for each question. Each "yes" response is assigned 1 point, and answering ‘yes’ to two or more questions of the five (i.e. a score of 2) indicates a probable diagnosis of anorexia nervosa or bulimia.
Stress
Perceived stress, the ability to handle stress, and sources of stress (stressors) were measured.
-
✔ Perceived stress and ability to handle stress were assessed using two previously studied single-item measures [29]. One item assesses the perceived amount of stress in a subject’s life on a scale of 1 (no stress) to 6 (extreme stress). The second item asks subjects to rate their ability to handle stress on a scale of 1 (“I can shake off stress”) to 6 ("stress eats away at me"). In our analysis, perceived amount of stress was categorized into three levels: low stress (score 1 or 2), moderate stress (score 3 or 4), and high stress (score 5 or 6). The ability to handle stress was categorized into three levels: Not at all able (scores 5 or 6), moderately able (scores 3 or 4), and extremely able (scores 1 or 2).
-
✔ Stressors among medical students were assessed using 31 items adapted from two sources: the Medical Student Stressors Questionnaire (MSSQ) and a tool employed by Amanya et. Al [30, 31]. The 31 items were translated by our research team and face validity was confirmed by two experts. Participants were asked to rate the level of stress caused by each stressor on a 5-point scale (ranging from "does not cause any stress" to "causes severe stress").
Coping
Coping strategies employed by medical students in response to stress were assessed using the 28-item Arabic Brief Cope scale, which was previously tested for its validity and reliability [32]. Subjects are asked to rate the extent to which they utilize each listed coping strategy on a 4-point scale (ranging from “not at all” to “doing a lot”).
Lifestyle behaviors
-
✔ Diet: dietary habits were assessed using the Simple Lifestyle Indicator Questionnaire (SLIQ) [33]. The SLIQ is a concise measurement scale that evaluates five dimensions of lifestyle, including diet, physical activity, alcohol consumption, smoking, and stress. Each component is scored individually, and an overall lifestyle score is also calculated. The SLIQ/diet component consists of three questions that probe the weekly consumption of fruits, vegetables, and cereals. Subjects assign a value between 0 (less than once a week) and 5 (twice or more daily) to each question, and the scores are then summed to generate a raw score for diet, ranging from 0 to 15. The raw diet scores are then be categorized as follows: 0-5 ("unhealthy"), 6-10 ("average"), and 11-15 ("healthy"). These categories also were used in our study analysis.
-
In addition to the SLIQ, students were asked about their consumption of fish, energy drinks, beverages (including tea and coffee), and unhealthy snacks (sugary snacks, sodas, or chips); how often they had breakfast; and how often they consumed fast food.
-
✔ Physical activity: The physical activity section of the SLIQ was used to measure the weekly frequency of engaging in light, moderate, and vigorous physical activities [33]. In this section, each type of activity is assigned a score based on the weekly frequency reported) ranging from zero times per week to 8 or more times per week). The raw score for physical activity is then obtained by summing the scores for light, moderate, and vigorous activities. The resulting raw score is then categorized into three groups: 0 for individuals engaging in light exercise only, 1 for those participating in any moderate activity, and 2 for individuals involved in any vigorous activity [33]. These categories also were used in our study analysis.
-
✔ Tobacco forms: respondents were asked to report their use of tobacco forms (combustible cigarettes, electronic cigarettes, water pipes, and heated tobacco products). Age of initiation, frequency of use, and time to first use after waking (an item from the Fagerström Test for Nicotine Dependence) also were probed [34].
-
✔ Alcohol use/abuse: the Arabic version of the PHQ was used to measure alcohol use [22]. In the PHQ, subjects are first asked if they drink alcohol. Those who respond with a yes are asked whether or not they experience five events indicative of problematic alcohol use (e.g. missing work or school or had difficulties getting along with people because of alcohol). A yes response to any of these events indicates the likelihood of "probable alcohol abuse or dependence".
-
✔ Insomnia was assessed using the two-question Pittsburgh Insomnia Rating Scale (PIRS-2) [35, 36]. The tool gauges individuals' perceived sleep quality and screens for insomnia risk. The PIRS-2 inquires about overall sleep satisfaction on a scale of 0 (“excellent”) to 3 (“poor”); and how much a person was bothered by lack of energy due perceived poor sleep in the past week on a scale of 0 (“not bothered at all”) to 3 (“severely bothered”). Each question carries a score from 0 to 3, with total scores ranging from 0 to 6. Higher scores correspond to a heightened potential for insomnia.
Other factors
Information was also collected on academic and sociodemographic attributes (age, gender, college year, marital status, place of residence, perceived financial situation of the family), perceived academic performance, perceived health status, weight, height, as well as the presence of any medical conditions.
Statistical analysis
All analyses were conducted using STATA 16 [37, 38], and included:
-
Reliability analyses: Internal consistency estimates (Cronbach's alpha) were calculated for each scale to ensure the instruments used in the study were reliable. The following values were obtained for the instruments tested: PHQ-9: 0.885; GAD-7: 0.905; PHQ-15: 0.851; PHQ alcoholism: 0.702; Brief Cope scale: 0.875; Stressors: 0.936; SCOFF: 0.571; SLIQ-diet: 0.577; SLIQ-physical activity: 0.532.
-
Descriptive analyses: Levels of depression, anxiety, somatization, eating disorders, and lifestyle factors reported across pre-clinical and clinical years were examined through bivariate tests (Chi-square, Independent Samples T-test, One-Way ANOVA, Man-Whitney U, and Kruskal–Wallis).
-
Multivariable analyses: Three multivariable analyses were conducted to determine whether or not being in a pre-clinical (versus clinical) stage of medical school was associated with (1) depression, (2) anxiety, and (3) somatization levels, while adjusting for various sociodemographic and lifestyle factors. Ordinal logistic regressions were used due to the multiple ordered categories of depression, anxiety and somatization (four categories: normal, mild, moderate, and severe). To ensure the appropriateness of our method, the proportional odds assumption was tested in all the models [39,40,41]. In models where variables violated the proportionality assumption, a Partial Proportional Odds Model (PPOM) was used to allow relaxation of this assumption specifically with these variables.
Per outcome (depression, anxiety, or somatization), the PPOM generated three panels. The first panel compared the first level of the outcome variable with all other levels of the outcome (e.g. normal depression versus mild+moderate+severe depression). The second panel compared the first two levels of the outcome variable with the remaining levels of the outcome (e.g. normal+mild depression versus moderate+severe depression). Finally, the third panel compared the three successive levels of the outcome variable with the highest level of the outcome (e.g. normal+mild+moderate depression versus severe depression) [42]. When the proportional odds assumption was met, odds ratios were similar across panels.
Results
Overall descriptive statistics and bivariate associations
A total of 618 students (representing approximately a quarter of all enrolled students) responded to the survey. Sociodemographic characteristics of the sample by clerkship group are included in Table 1. Among students participating in the study, 312 (50.5%) were in their pre-clinical years (and 49.5% in their clinical years). The median age of the sample was 22. The majority of the sample of students were Jordanian, unmarried, and resided with their families. In terms of perceived financial situation at home, 84% of the students reported this as “average” (with a greater proportion of students in the pre-clinical years reporting “low” than those in the clinical years). With regards to academic performance, a greater proportion of students in pre-clinical years reported “poor to fair” academic performance than those in clinical years while a greater proportion in the latter group reported “very good” performance.
The association of health and lifestyle-related factors with clerkship status are displayed in Table 2. Approximately 57% of students had a healthy body weight with a BMI (18.5 to < 25). The median raw score for dietary habits was 5 (interquartile range 3–7), placing 60.2% of students in the “unhealthy diet” category. Overall, 28.6% of students were identified as being at high risk for eating disorders, but a significantly greater proportion was observed in the pre-clerkship group (33.7% versus 23.5% in the clerkship group). In terms of physical activity, the median raw score was 6 (interquartile range 3–10), and only 17% of students engaged in vigorous activities. Only 1% of the sample screened positive for alcohol abuse or dependence. Finally with regards to health and lifestyle, roughly a quarter of the sample reported any tobacco use, with significantly higher rates of any tobacco use (29.1%) in the clerkship group. The most frequently used form of tobacco was the waterpipe (19.1% of students) while the least used form was heat-not-burn tobacco (used by 1.3%). Notable results not presented in the Tables was the dual use of combustible cigarettes and vapes – more than half of the students who smoked conventional cigarettes also used electronic cigarettes; and the higher rates of smoking in males for all tobacco products except for waterpipe.
With regards to MHPs (Table 2), 4.7% of students reported having a mental illness prior to joining medical school, with the proportion being significantly higher among students in the pre-clerkship group (6.7% versus 2.6% in the clerkship group). The percentage of students reporting a diagnosis of a mental illness post-enrollment at University was 10%. In terms of perceived stress, 63.6%, 30.6% and 5.8% of students reported high levels, moderate levels, and normal to low levels of stress, respectively. Approximately 24% stated that they were not at all able to handle the amount of stress they faced. Furthermore, 48.4%, 36.7%, and 55% of students screened positive for depression, anxiety and somatization, respectively. Specifically, 25.4% had severe depression and 15.4% had severe anxiety. Just over a quarter of the sample experienced severe somatic symptoms, with the most frequently reported symptoms being feeling tired, headaches, trouble sleeping, back pain, and pain in the arms and legs. In terms of significant differences when comparing pre-clerkship and clerkship groups, distributional differences were observed between “normal” and severe somatization levels and depression levels: significantly greater proportions of pre-clerkship students reported severe somatization and severe depression (and lower proportions reported no somatization or no depression). Finally with regards to MHPs prevalence, roughly 26% of students experienced suicidal ideation, with 36 students (5.8%) having such thoughts almost daily.
For further insight, supplemental Tables 1, 2 and 3 (online supplement 1) provide the bivariate associations of the sociodemographic, lifestyle and academic factors measured in the study by reported levels of depression, anxiety and somatization, respectively.
Multivariable analyses
The results of the final multivariable analyses for each outcome (depression, anxiety, and somatization) are displayed in Table 3.
Depression-related findings
With regards to depression, students in the clinical/clerkship group were 0.49 times less likely to experience any form of depression (mild, moderate, or severe) compared to their counterparts in the pre-clerkship status (p < 0.05). Any [moderate or extreme] ability to handle stress was significantly associated with lower odds of being in moderate to severe levels of depression (odds ratios ranged between 0.32 and 0.65 across panels). Our analysis also revealed a statistically significant association between physical activity and depression, indicating that for each unit increase in physical activity raw score, there was a 4% decrease in the odds of falling into higher depression categories (odds ratio 0.96, 95% confidence interval: 0.93-0.99, p value 0.011). Conversely, having a higher insomnia score, reporting an eating disorder, and being a cigarette smoker were associated with a 1.34, 1.93 and 1.8 times (respectively) greater odds of being in higher categories of depression.
Anxiety-related findings
Students who reported their academic performance as “very good” or “excellent” were 0.55 and 0.57 times less likely [than those reporting poor/fair performance] to fall in higher anxiety categories (respectively). Furthermore, ability to handle stress (i.e. moderate ability or extreme ability) was significantly associated with lower odds of being in moderate to severe levels of anxiety across most panels (odds ratios ranged between 0.37 and 0.59). Conversely, having a higher insomnia score, reporting an eating disorder, and being a cigarette smoker were significantly associated with a 1.37, 1.67 and 2.51 times (respectively) greater odds of being in higher categories of anxiety.
Somatization-related findings
Females had significantly higher odds of falling into the severe somatization category compared to males (odds ratios ranged between 2.54 and 6.07 across panels). High-perceived stress was significantly associated with moderate to severe somatization. Specifically, those perceiving moderate to high stress were 2.44 to 3.17 times (respectively) more likely to fall in categories indicative of greater somatization. Having a higher insomnia score, reporting an eating disorder, being a cigarette smoker, and being a waterpipe (or other forms of tobacco) smoker were significantly associated with a 1.31, 1.55, 2.78 and 1.65 times (respectively) greater odds of being in higher categories of somatization.
Discussion
In our study, we examined the association of academic, sociodemographic and lifestyle-related factors with key MHPs, namely depression, anxiety and somatization, in medical students at Yarmouk University in Jordan. Our findings revealed few significant differences between pre-clinical and clinical years of study. Rather, across both groups of study, our findings revealed a high prevalence of depression, anxiety, somatic symptoms, eating disorders, and stress. Moreover, a considerable proportion of students experienced severe symptoms of MHPs.
Limited studies in Jordan have explicitly evaluated depression in medical students. The prevalence of depression in our study (48.4%) aligns with previous research conducted in the Arab world [10, 14, 20, 43], but is significantly higher than the global rates [8, 44]. This could be attributed to various factors: high-pressure academic environments and a conventional non-student-centered program and curriculum elements; limited access to mental health services and support; cultural norms that deter from healthy discussions about mental health; increasingly competitive opportunities to train abroad; and challenging employment prospects for physicians.
With regards to factors that influenced depression, we found that being in the pre-clerkship years of study negatively influenced depression. Findings in the literature have varied (some have found a similar association [16, 19, 45, 46], some have found the converse [47, 48], and some have found no association between depression and clerkship status [8]). Given the high prevalence of depression in our study, it is important to avail efforts to enhance mental well-being to all medical students, rather than assuming only in-coming students (or only students experiencing clinical work) require this.
Several studies have demonstrated that females are more likely than males to suffer from depression [14, 20, 44, 49]. However, our results did not reveal an association between gender and the severity of depressive symptoms, a finding consistent with a systematic review of studies on depression in medical students [8]. Such inconsistencies also were observed with obesity: our findings, like others [50, 51], indicated no association between obesity and depression, but some studies have reported greater psychological morbidity with obesity [52]. More importantly, we were able to confirm the protective potential of physical activity against depression, a finding which aligns with previous studies [10, 53], and which can be used to encourage students to engage in active lifestyles.
We also observed a relatively high prevalence of eating disorders when compared to international studies [15, 54,55,56]. There is a noticeable lack in the number and quality of research studies on eating disorders in Arab communities (let alone Jordanian medical students in particular). One review of studies in the Arab world revealed a wide variability in estimates of eating disorders (2% to 54.8%), and further emphasized the scarcity of and need for better-designed studies [57]. Nevertheless, we speculate that our finding is not unusual. In our view, eating disorders in Arab cultures may well be on the rise due to the clash of older sociocultural norms with the relatively rapid exposure to global Westernized norms that are now much more pervasive in Arab communities and tend to focus on being thin (in the case of females) or being more toned or muscular (in the case of males). There is a pressing need for national and epidemiological studies to examine the prevalence of eating disorders in Arab countries, particularly in Jordan, and to investigate why these rates are higher than in other countries worldwide.
Our findings (supplementary tables) suggest an association between the presence of eating disorders and the degree of depression among our sample of students.
With regards to the prevalence of anxiety observed in our study, it was comparable to the global prevalence of 33.8% reported in a meta-analysis [6], although individual studies have reported both higher, [20, 45, 47, 58, 59], and lower rates than ours [60,61,62,63]. Combustible cigarette smoking, insomnia, and the presence of indications of an eating disorder all were associated with higher anxiety; while ability to manage stress was protective. This finding aligns with similar findings in other studies [64].
The prevalence of somatization in our study was higher than rates reported in the literature [26, 65,66,67]. Notably, amongst other factors, females were significantly more likely than males to experience somatization, suggesting that female students may process MHPs in a different manner than males.
Our study has certain limitations: our survey was a cross-sectional and we were therefore unable to capture any fluctuations in MHPs across time to better understand how MHPs developed. Our study also was solely quantitative, and did not probe in-depth experiences of students with regards to their MHPs. Furthermore, due to its cross-sectional nature, we were unable to conclude a temporal relation between the variables examined. In addition, our measurement tool was relatively long. We sought to gauge several important constructs that no single available pre-existing questionnaire could cover, and multiple items and tools were therefore included in the study questionnaire. While the briefest valid versions of measurements were used [per construct], and piloting of the questionnaire was conducted to ensure that the questionnaire was well-understood and was not burdensome, it arguable that some respondents may still have perceived it to be complex or long (of the 1,208 who began the survey, and 618 complete results were obtained). Non-responders may have had different experiences, and we could not assess their characteristics. Thus, while our sample represented approximately a quarter of students enrolled, nonresponse bias cannot be ruled out. Finally, our study was conducted in one Medical College, and arguably may not be generalizable to other colleges. To address these limitations, conducting longitudinal studies would be of value to chart the trajectory of MHPs throughout medical training, and identify both risk and protective factors over time. Moreover, harmonizing how these studies are conducted across all colleges (for example, by incorporating metrics of mental health and lifestyle in college-wide surveys) would allow for comparisons across campuses and specialties to provide generalizable insight with regards to how MHPs, lifestyle factors and academic environments interact during these formative years of professional and overall development. Qualitative research studies would also add a wealth of information regarding how MHPs develop in young medical professionals, and what interventions would resonate with this important subgroup of the community.
In summary with regards to our findings, MHPs were observed in considerable percentages of medical students. Ability to handle stress, a skill that can be taught to students, played a protective role across all MHPs, and physical activity appeared to have a positive effect on depression. Contrary to the common misconception that smoking may help manage MHPs, combustible cigarette smokers had a higher risk of falling in more severe categories of anxiety, a useful finding when educating young adults. Insomnia also was associated with higher levels of anxiety. Collectively, our results paint a compelling picture that can provide the rational to engage with medical students and empower them with skills to manage their well-being holistically (for example, incorporating sleep hygiene practices, being physically active, and learning stress management techniques).
Conclusion
Our study revealed concerning prevalence rates of depression, anxiety, somatic symptoms, stress, and eating disorders among undergraduate medical students at Yarmouk University. Key findings include the protective effects of ability to handle stress and having healthy lifestyles. However, only a small percentage of the participating students demonstrated healthy lifestyle practices relative to the higher proportion of students reporting tobacco use. Medical students need to be better educated about the interconnections between mental health, lifestyle, and stress; and more interventions need to be availed to build students’ skills in resilience and stress management.
Data availability
Data cannot be shared publicly because of institutional regulations. Data requests are reviewed and approved by the Institutional Review Board at King Hussein Cancer Center (contact Linda Kateb, at IRBOffice@KHCC.JO). For researchers who meet the criteria for access to confidential data, data can then be shared.
Abbreviations
- MHPs:
-
Mental health problems
- AAHRPP:
-
Association for the Accreditation of Human Research Protection Programs
- PHQ:
-
Patient Health Questionnaire
- PHQ9:
-
Patient Health Questionnaire-9
- GAD7:
-
General Anxiety Disorder-7
- PHQ15:
-
Patient Health Questionnaire-15
- MSSQ:
-
Medical Student Stressors Questionnaire
- SLIQ:
-
Simple Lifestyle Indicator Questionnaire
- PIRS-2:
-
The two-question Pittsburgh Insomnia Rating Scale
- PPOM:
-
Partial Proportional Odds Model
References
Anxiety disorders. In Diagnostic and statistical manual of mental disorders (5th ed.) https://doi.org/10.1176/appi.books.9780890425596.dsm05
Organization WH. The ICD-10 Classification of Mental and Behavioural Disorders. Clinical descriptions and diagnostic guidelines. Geneval: World Health Organization; 1993.
Fusar-Poli P, Correll CU, Arango C, Berk M, Patel V, Ioannidis JPA. Preventive psychiatry: a blueprint for improving the mental health of young people. World Psychiatry. 2021;20(2):200–21.
Aljuwaiser S, Brazzelli M, Arain I, Poobalan A. Common mental health problems in medical students and junior doctors - an overview of systematic reviews. J Ment Health. 2023:1–37.
Braquehais MD, Vargas-Caceres S. Psychiatric issues among health professionals. Med Clin North Am. 2023;107(1):131–42.
Quek TT, Tam WW, Tran BX, Zhang M, Zhang Z, Ho CS, Ho RC. The Global Prevalence of Anxiety Among Medical Students: A Meta-Analysis. Int J Environ Res Public Health. 2019;16(15):2735.
Varshney K, Patel H, Panhwar MA: Risks and Warning Signs for Medical Student Suicide Mortality: A Systematic Review. Arch Suicide Res 2024:1–19.
Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, Sen S, Mata DA. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316(21):2214–36.
Sreeramareddy CT, Shankar PR, Binu VS, Mukhopadhyay C, Ray B, Menezes RG. Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Med Educ. 2007;7:26.
Ben Ayed H, Yaich S, Ben Jemaa M, Ben Hmida M, Trigui M, Jedidi J, et al. Lifestyle behaviors and mental health in medical students. J Public Ment Health. 2018;17(4):210–7.
Terebessy A, Czegledi E, Balla BC, Horvath F, Balazs P. Medical students’ health behaviour and self-reported mental health status by their country of origin: a cross-sectional study. BMC Psychiatry. 2016;16:171.
Zaman R, Hankir A, Jemni M. Lifestyle factors and mental health. Psychiatr Danub. 2019;31(Suppl 3):217–20.
Fargen KM, Spiotta AM, Turner RD, Patel S. The importance of exercise in the well-rounded physician: dialogue for the inclusion of a physical fitness program in neurosurgery resident training. World Neurosurg. 2016;90:380–4.
Mohammed HM, Soliman SM, Abdelrahman AA, Ibrahim AK. Depressive symptoms and its correlates among medical students in Upper Egypt. Middle East Current Psychiatry. 2022;29(1):66.
Bizri M, Geagea L, Kobeissy F, Talih F. Prevalence of eating disorders among medical students in a Lebanese medical school: a cross-sectional study. Neuropsychiatr Dis Treat. 2020;16:1879–87.
Shawahna R, Hattab S, Al-Shafei R, Tab’ouni M. Prevalence and factors associated with depressive and anxiety symptoms among Palestinian medical students. BMC Psychiatry. 2020;20(1):244.
Masri R, Kadhum M, Farrell SM, Khamees A, Al-Taiar H, Molodynski A. Wellbeing and mental health amongst medical students in Jordan: a descriptive study. Int Rev Psychiatry. 2019;31(7–8):619–25.
(Petra). JNA: عويس_ 19 ألف طالب طب في الجامعات الوطنية ومثلهم في الخارج. Available from https://petra.gov.jo/Include/InnerPage.jsp?ID=205009&lang=ar&name=news. Accessed 02 Aug 2023. In.; 2022.
Elsawy WIH, Sherif AAR, Attia M, El-Nimr NA. Depression among medical students in Alexandria. Egypt Afr Health Sci. 2020;20(3):1416–25.
Ibrahim MB, Abdelreheem MH. Prevalence of anxiety and depression among medical and pharmaceutical students in Alexandria University. Alexandria Journal of Medicine. 2019;51(2):167–73.
Midtgaard M, Ekeberg O, Vaglum P, Tyssen R. Mental health treatment needs for medical students: a national longitudinal study. Eur Psychiatry. 2008;23(7):505–11.
AlHadi AN, AlAteeq DA, Al-Sharif E, Bawazeer HM, Alanazi H, AlShomrani AT, Shuqdar RM, AlOwaybil R. An arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. Ann Gen Psychiatry. 2017;16:32.
Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–66.
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–44.
Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345–59.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Spitzer RLKK, Williams JBW, Lo B. A brief measure for assessing generalized anxiety disorder. Arch Intern Med. 2006;166:1092–7. https://doi.org/10.1001/archinte.166.10.1092. PMID: 16717171.
Aoun AAJ, Jabbour FE, et al. Validation of the Arabic version of the SCOFF questionnaire for the screening of eating disorders. East Mediterr Health J. 2015;21(5):326–31. https://doi.org/10.26719/2015.21.5.326. Published 2015 Aug 27.
Littman AJ, White E, Satia JA, Bowen DJ, Kristal AR. Reliability and validity of 2 single-item measures of psychosocial stress. Epidemiology. 2006;17(4):398–403.
Yusoff MSB, Rahim AFA, Yaacob MJ . The development and validity of the Medical Student Stressor Questionnaire (MSSQ), ASEAN J Psychiatry. 2010;11(1). Available online at http://www.aseanjournalofpsychiatry.org/oe11105.htm.
Amanya SB, Nakitende J, Ngabirano TD. A cross-sectional study of stress and its sources among health professional students at Makerere University Uganda. Nurs Open. 2018;5(1):70–6.
Hamdan- Mansour ABT, Haourani E, Marmash L. Depression, psychological distress and coping skills among patients diagnosed with type-II Diabetes Mellitus. Life Sci J. 2013;10:3044–8.
Godwin M, Streight S, Dyachuk E, van den Hooven EC, Ploemacher J, Seguin R, Cuthbertson S. Testing the simple lifestyle indicator questionnaire: initial psychometric study. Canadian family physician Medecin de famille canadien. 2008;54(1):76–7.
Fagerström KO. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict Behav. 1978;3(3–4):235–41. https://doi.org/10.1016/0306-4603(78)90024-2. PMID: 735910.
Moul DE ME, Shablesky M et al. The 2-item and 20-item versions of the Pittsburgh Insomnia Rating Scale (PIRS): design, methods and initial modeling. Presented at: the Annual Meeting of the World Psychiatric Association; November 29, 2009; Melbourne. 2009.
Moul DE, Pilkonis PA, Miewald JM, Carey TJ, Buysse DJ. Preliminary study of the test-retest reliability and concurrent validities of the Pittsburgh Insomnia Rating Scale (PIRS). Sleep. 2002;25:A246–7.
Jann B. ESTOUT: Stata module to export estimation results from estimates table. 2004. Available from http://ideas.repec.org/c/boc/bocode/s439301.html.
StataCorp. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC; 2019.
Williams R. Generalized ordered logit/partial proportional odds models for ordinal dependent variables. Stata J. 2006;6(1):58–82 A pre-publication version is available at http://www.nd.edu/~rwilliam/gologit2/gologit2.pdf.
Peterson BFEHJ. Partial proportional odds models for ordinal response variables. J Roy Stat Soc: Ser C (Appl Stat). 1990;39(2):205–17.
Williams R. Understanding and interpreting generalized ordered logit models. The Journal of Mathematical Sociology. 2016;40(1):7–20.
Fu V. Estimating generalized ordered logit models. Stata Tech Bull. 1999;8(44):27–30.
Mahroon ZA, Borgan SM, Kamel C, Maddison W, Royston M, Donnellan C. Factors associated with depression and anxiety symptoms among medical students in Bahrain. Acad Psychiatry. 2018;42(1):31–40.
Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50(4):456–68.
Fawzy M, Hamed SA. Prevalence of psychological stress, depression and anxiety among medical students in Egypt. Psychiatry Res. 2017;255:186–94.
Olum R, Nakwagala FN, Odokonyero R. Prevalence and factors associated with depression among medical students at Makerere university. Uganda Adv Med Educ Pract. 2020;11:853–60.
Iqbal S, Gupta S, Venkatarao E. Stress, anxiety and depression among medical undergraduate students and their socio-demographic correlates. Indian J Med Res. 2015;141(3):354–7. https://doi.org/10.4103/0971-5916.156571. PMID: 25963497; PMCID: PMC4442334.
Baldassin S, Alves TC, de Andrade AG, Nogueira Martins LA. The characteristics of depressive symptoms in medical students during medical education and training: a cross-sectional study. BMC Med Educ. 2008;8:60.
Ngasa SN, Sama CB, Dzekem BS, Nforchu KN, Tindong M, Aroke D, Dimala CA. Prevalence and factors associated with depression among medical students in Cameroon: a cross-sectional study. BMC Psychiatry. 2017;17(1):216.
Arslan M, AydemİR İs, Yabanci Ayhan N. Examining The Level Of Depression Among University Students And Evaluating Its Relationship With Body Mass Index (BMI). Clin Exp Health Sci. 2021;11:175–81.
Al-Khlaiwi T, Habib S. Depression, anxiety, stress, and satisfaction of medical students in relation to income and body mass index. King Khalid University J Health Sci. 2022;7(2):104–10.
Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90(2):251–7. https://doi.org/10.2105/ajph.90.2.251. PMID: 10667187; PMCID: PMC1446144.
Gabal HA, Wahdan MM, Gamal Eldin DA. Prevalence of anxiety, depression and stress among medical students, and associated factors. Egypt J Occup Med. 2022;46(1):55–74.
Memon AA, Adil SE, Siddiqui EU, Naeem SS, Ali SA, Mehmood K. Eating disorders in medical students of Karachi, Pakistan-a cross-sectional study. BMC Res Notes. 2012;5:84.
Fekih-Romdhane F, Daher-Nashif S, Alhuwailah AH, Al Gahtani HMS, Hubail SA, Shuwiekh HAM, Khudhair MF, Alhaj OA, Bragazzi NL, Jahrami H. The prevalence of feeding and eating disorders symptomology in medical students: an updated systematic review, meta-analysis, and meta-regression. Eat Weight Disord. 2022;27(6):1991–2010.
Jahrami H, Sater M, Abdulla A, Faris MA, AlAnsari A. Eating disorders risk among medical students: a global systematic review and meta-analysis. Eat Weight Disord. 2019;24(3):397–410.
Melisse B, de Beurs E, van Furth EF. Eating disorders in the Arab world: a literature review. J Eat Disord. 2020;8(1):59.
Abdel Wahed WY, Hassan SK. Prevalence and associated factors of stress, anxiety and depression among medical Fayoum University students. Alexandria Journal of Medicine. 2019;53(1):77–84.
KhanMS MS, Badshah A, Ali SU, Jamal Y. Prevalence of depression, anxiety and their associated factors among medical students in Karachi, Pakistan. J PakMed Assoc. 2006;56:583–6.
Ahmed I, Banu H, Al-Fageer R, Al-Suwaidi R. Cognitive emotions: depression and anxiety in medical students and staff. J Crit Care. 2009;24(3):e1-7.
Said D, Kypri K, Bowman J. Risk factors for mental disorder among university students in Australia: findings from a web-based cross-sectional survey. Soc Psychiatry Psychiatr Epidemiol. 2013;48(6):935–44.
El-Gilany AHAM, Hammad S. Perceived stress among male medical students in Egypt and Saudi Arabia: effect of sociodemographic factors. Ann Saudi Med. 2008;28(6):442–8. https://doi.org/10.5144/0256-4947.2008.442. PMID: 19011321; PMCID: PMC6074256.
Tabalipa FD, Souza M, Pfützenreuter G, Lima VC, Traebert E, Traebert J. Prevalence of anxiety and depression among medical students. Revista Brasileira de Educação Médica. 2015;39(3):388–94.
Alkhalaf AM. Positive and negative affect, anxiety, and academic achievement among medical students in Saudi Arabia. International Journal of Emergency Mental Health and Human Resilience. 2018;20(2):397.
Chinawa JM, Nwokocha AR, Manyike PC, Chinawa AT, Aniwada EC, Ndukuba AC. Psychosomatic problems among medical students: a myth or reality? Int J Ment Health Syst. 2016;10:72.
Goweda R, Alshinawi MA, Janbi BM, Idrees UY, Babukur RM, Alhazmi HA, Aiash H. Somatic Symptom Disorder among medical students in Umm Al-Qura University, Makkah Al-Mukarramah, Kingdom of Saudi Arabia. Middle East J Fam Med. 2022;20(5):6–11.
Abdelaziz AMYAK, Alhurayyis JH, Alqahtani TA, Alghamlas AM, Algahtani HM, Jahrami HA. The association between physical symptoms and depression among medical students in Bahrain. Int J Med Educ. 2017;15(8):423–7. https://doi.org/10.5116/ijme.5a2d.16a3.PMID:29252203;PMCID:PMC5768439.
Acknowledgements
Declared none.
Funding
None.
Author information
Authors and Affiliations
Contributions
YD and NO contributed to the conceptualization and design of the study, literature review, questionnaire development, formal data analysis, results interpretation, and manuscript development. RD and KS contributed to the conceptualization and design of the study, project supervision, results interpretation, and manuscript revision. SA, MA, MI, AA, AA, AA and GS contributed to the pilot testing, data collection, and manuscript revision. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was reviewed and approved by the Institutional Review Board of the King Hussein Cancer Center (study number 22 KHCC 69), an accredited body of the Association for the Accreditation of Human Research Protection Programs, Inc (AAHRPP). The formal informed consent was waived by the King Hussein Cancer Center Institutional Review Board and the participants were considered to have an agreement on the study if they proceeded with the survey. The data were kept confidential and no personally identifiable information was reported.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dodin, Y., Obeidat, N., Dodein, R. et al. Mental health and lifestyle-related behaviors in medical students in a Jordanian University, and variations by clerkship status. BMC Med Educ 24, 1283 (2024). https://doi.org/10.1186/s12909-024-06273-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1186/s12909-024-06273-6