Abstract
Background
To investigate whether cumulus cell removal after a 3 h co-incubation of gametes can affect the outcomes of in vitro fertilization.
Methods
A prospective randomized sibling-oocyte study was performed in which sibling oocytes obtained from each patient were randomly assigned to either a 3 h or 20 h group (cumulus cells removed at 3 h or 20 h after insemination, respectively). Same origin embryos (either 3 h or 20 h) were transferred. The study participants were patients < 38 years old and with infertility due to tubal factors. The study outcomes included fertilization, embryo quality, and birth status.
Results
The study enrolled 172 patients, from whom 2275 oocytes were retrieved (1139 oocytes for the 3 h group and 1136 oocytes for the 20 h group). A total of 134 patients received embryo transfers (74 patients in the 3 h group and 60 patients in the 20 h group), and there were 54 live births (32 in the 3 h group and 22 in the 20 h group). When compared with patients in the 20 h group, patients in the 3 h group produced a larger number of optimal quality embryos, but had higher rates of polyspermy and low birth weight newborns. The two groups showed no differences in their rates of normal fertilization, pregnancy, and live birth.
Conclusions
When compared with results obtained using a traditional cumulus cell removal protocol, early cumulus cell removal has both advantages and disadvantages. Further studies, and especially long-term outcome studies on newborns, need to be performed.
Trial registration
Current controlled trial ChiCTR-OOC-15006878
Similar content being viewed by others
Background
Infertility can produce high levels of stress and have a negative impact on both individuals and society. Assisted reproductive technology, which includes several types of medical treatments, can improve the chance of pregnancy and a live birth. However, even with in vitro fertilization (IVF), which has the highest success rate among all types of assisted reproductive technology, only ~ 50 % of women achieve pregnancy [1]. Therefore, research on methods to improve the IVF process and its pregnancy outcomes is of great importance.
One major cause for failed IVF is failure of the sperm to fertilize the oocyte [2]. A rescue procedure, such as intracytoplasmic sperm injection (ICSI), can help improve the oocyte fertilization rate. Additionally, it was previously shown that early ICSI can increase pregnancy rates and lead to better clinical outcomes [3]. In order to recognize unfertilized oocytes and perform ICSI early on, oocytes have to be examined for the absence of a second polar body, and early cumulus cell removal can facilitate this examination [4]. Furthermore, early cumulus cell removal can also reduce the required co-incubation time between sperm and oocytes, and help eliminate degradation products from granulosa cells. These effects of early cumulus cell removal can reduce the potential for oocytes to be damaged by reactive oxygen species [5, 6]. However, previous studies which investigated the outcomes of early cumulus cell removal have shown conflicting results, with some studies reporting no change in pregnancy rates, and other studies reporting a decreased number of available embryos [7–9]. Such results suggest that further studies are needed to understand the effects of early cumulus cell removal during IVF on pregnancy outcomes.
We performed a prospective randomized sibling-oocytes study comparing the effects of cumulus cell removal performed at different time points on pregnancy outcomes.
Methods
Study design and patient selection
This prospective randomized clinical study was performed at the Reproductive Medicine Center of Tongji Hospital, Huazhong University of Science and Technology in China, between May 2012 and August 2013. The study protocol was approved by the hospital’s Institutional Review Board, and registered with the Chinese Clinical Trial Registry (registration number ChiCTR-OOC-15006878). Patients undergoing conventional IVF treatment were invited to participate in this study, and those who enrolled provided their signed written informed consent. The study inclusion criteria were an age < 38 years old and infertility due to tubal factors.
Ovarian stimulation
All patients received a long protocol treatment of down-regulation with a gonadotrophin releasing hormone (GnRH) agonist (Decapeptyl, Ferring, Kiel, Germany; Diphereline, Ipsen, Paris, France) which was administrated daily starting on day 21 of the previous menstrual cycle. Individually adapted doses of follicle-stimulating hormone and/or human menopausal gonadotropins were injected after pituitary desensitization was confirmed. A single 10,000 unit dose of human chorionic gonadotropin was administrated when at least three ovary follicles reached a mean diameter of 17–18 mm; at which point, follicular aspiration was performed 36 h later.
Sperm preparation
All semen samples were collected via masturbation following 3–7 days of sexual abstinence, and were allowed to liquefy for at least 30 min at 37 °C prior to the swim-up purification process. Sperm concentration, motility, and morphology were evaluated under a light microscope based on criteria established by the World Health Organization (WHO, 1992).
In vitro insemination
Follicles were punctured using a double lumen oocyte harvesting needle. Each follicle was individually punctured, and each oocyte was cultured in one droplet. The first oocyte obtained from each patient was randomly assigned to either a cumulus cell 3 h removal group (3 h) or a standard 20 h removal group (20 h) on retrieval day (day 0). Subsequent oocytes obtained from the same patient were also assigned to either a 3 h or 20 h group. Following retrieval, the oocytes were incubated for 3 h in a single droplet containing 20,000-30,000 motile sperm.
Cumulus cell removal
The cumulus cells and oocytes in the 3 h group were incubated with sperm for 3 h. Following incubation, the oocytes were rinsed and gently washed; after which, the cumulus cells were mechanically removed using a pipette with an inner diameter slightly smaller than that of the oocytes. After most of the cumulus cells were removed, the oocytes were transferred and cultured in a fresh medium. Fertilized oocytes were checked for the presence of a second polar body, and those without a second polar body were subjected to rescue ICSI. Oocytes in the 20 h group were inseminated for 3 h, and then transferred from the insemination medium to fresh medium with their surrounding cumulus cells left intact during transfer. On day 1, which was ~ 20 h after the oocyte retrievals, the cumulus cells were removed to allow an assessment of fertilization. Because early rescue ICSI is usually performed at 3 h after insemination, and cumulus cell removal is usually performed at 20 h [4, 8, 9], we chose 3 h and 20 h, respectively, as our early and late time points for cumulus cell removal.
Embryo transfer
Embryos were transferred on day 3 after oocyte retrieval. Each patient received two transferred embryos, and patients received only same origin embryos (either 3 h or 20 h). Progesterone injections were initiated according to the conventional IVF treatment protocol. All patients were closely monitored for clinical pregnancy and birth.
Outcome measurements
Normal fertilization was defined as the presence of two clearly visible pronuclei, together with two individualized or fragmented polar bodies at 20 h after IVF. An optimal embryo on day 3 contained ≥ 6 equal sized blastomeres, and showed a ≤ 10 % degree of fragmentation rate [10, 11]. Gardner’s scoring system was used to evaluate blastocysts. An optimal blastocyst was defined as a blastocoel fully filled embryo which displayed a tightly packed inner cell mass, and a trophectoderm with numerous cells which formed a cohesive epithelium on day 5 or 6. Embryos which reached the blastocyst stage (minimum expansion: early blastocyst; inner cell mass and trophectoderm layer: score A or B) were cryopreserved on day 5 or day 6. Clinical pregnancy was defined as the presence of a gestational sac that displayed a fetal heartbeat during ultrasound screening. Implantation rate was defined as the number of gestational sacs observed, divided by the number of embryos transferred. Premature delivery was defined as the baby being born at a gestational age of < 37 weeks. Birth weight was recorded in kilograms, and low birth weight was defined as < 2500 g.
Statistical analysis
Continuous data are presented as the mean ± standard deviation, and ordinal data are presented as proportions. The data were analyzed by either the student’s t-test or chi-squared test using IBM SPSS Statistics for Windows Version 19.0 (IBM Corp., Armonk, NY). A P-value < 0.05 was considered statistically significant.
Results
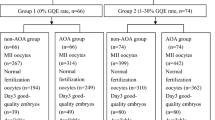
The study recruited 172 patients; among whom, 134 patients were analyzed (Fig. 1, 74 patients in the 3 h group and 60 patients in the 20 h group). The mean age of the patients was 29.7 years (30.3 ± 3.7 years in the 3 h group and 29.3 ± 2.7 years in the 20 h group). The numbers of treatment cycles in the 3 h and 20 h groups were 1.0 ± 0.2 and 1.1 ± 0.4, respectively. Thirty patients were excluded due to either cancelled cycles (3 patients) or mixed embryo transfers (27 patients). Eight patients were not included in the statistical analysis because they received early rescue ICSI.
The fertilization, embryo, and pregnancy outcomes are shown in Tables 1, 2, and 3. When compared with the 20 h group, the 3 h group had a significantly higher polyspermy rate and percentage of optimal embryos. An analysis on obstetric outcomes showed that low birth weight infants were more common in the 3 h group (Table 4).
Discussion
While early cumulus cell removal can facilitate early rescue ICSI and might improve pregnancy outcomes [3, 12], several previous studies have reported inconsistent results regarding outcomes after early cumulus cell removal. Some studies reported that early cumulus cell removal resulted in fertilization and clinical pregnancy rates similar to those obtained when performing a standard removal at 20 h post-insemination [8]. Another study showed that early cumulus removal after 4 h of insemination was associated with low numbers of available embryos [7]. Our current prospective randomized sibling-oocyte study demonstrated that early cumulus cell removal resulted in larger numbers of optimal embryos, but also a higher rate of polyspermy and a larger percentage of low birth weight infants. These types of results have not been previously reported.
Previous studies have demonstrated that co-culture of human oocytes and cumulus cells can improve embryo morphology and blastocyst formation [13, 14]. This might be due to bi-directional communications between oocytes and cumulus cells [15]. Cumulus cells provide oocytes with a local source of glycosaminoglycans, steroid hormones, nutrients, and other factors during stages of oocyte nuclear and cytoplasmic maturation, fertilization, and development [16]. However, our study showed that early cumulus cell removal can increase the quality of embryos. This is probably because cumulus cell removal reduces the levels of toxic metabolic products (e.g., active oxygen species, E2, and progesterone) produced by sperm and cumulus cells, and thus the adverse effects of these products on the vitality and quality of embryos [5, 6]. Some researchers have demonstrated a significant negative relationship between the incidence of cumulus cell apoptosis and the “good-embryo” rate [6]. Cumulus cells may have both beneficial and adverse effects on oocytes, and the exact nature of these effects require further investigation.
Our study showed a higher polyspermy rate among patients in the 3 h group. Cumulus cells are more difficult to remove at 2–4 h after insemination when compared with their removal at 20 h. However, at early times after insemination, the oocytes are also more vulnerable, due to their active spindles and microtubules [7, 8]. This can result in their greater susceptibility to being damaged by the additional mechanical stress created when a denuding pipette is used remove cumulus cells. Moreover, repeated mechanical stimulation can also have detrimental effects on the integrity of an oocyte’s zona pellucid, and thus reduce its defense against polyspermy. Polyspermy might also be caused by unstable culture conditions or an excessive number of sperm in the culture medium, which may be directly or indirectly related to early cumulus cell removal. All of these factors may have contributed to the increased polyspermy rate found in the current study’s 3 h group. However, our study did not find a significant difference between the rates of normal fertilization in the 3 h and 20 h groups, suggesting that normal fertilization was not affected by early cumulus cell removal. We also observed a high rate of low birth weight newborns in the 3 h group. Whether these low birth weight newborns were a result of mechanical stimulation during cumulus cell removal remains unknown, and requires further study.
Our current study showed that when compared with the 20 h group, the 3 h group had poorer obstetric and prenatal outcomes. Also, while the differences were not statistically significant, patients in the 3 h group had higher premature deliver and twin delivery rates, as well as a higher chance of having a low birth weight newborn. One possible explanation for these findings might be injuries that occurred due to mechanical stimulation during the stripping of cumulus cells from oocytes. Also, inappropriate repeated mechanical stimulation can cause epigenetic-based changes resulting from DNA methylation and gene differential expression; both of which are related to the incidence of low birth weight newborns [17, 18]. Additionally, it has been shown that removal of cumulus cells by high-speed vortexing can affect the relative locations of chromosome spindles and the first polar body [19]. Such changes might result in poor fetal development, twin pregnancy or early delivery. Other alterations created by cumulus cell retrieval, such as imprinted genes, subtle epigenetic alterations, and epigenetic reprogramming, might also contribute to a higher incidence of low birth weight newborns [20].
Our study has some limitations that should be mentioned. First, the study was conducted at a single hospital. Therefore, our results may not be applicable to other hospitals, because different hospitals may use different ovarian stimulation and IVF protocols. Second, our study population only included patients with infertility due to tubal factors, and not other causes. Similar studies should be performed at other hospitals, and with patients having other causes for infertility.
Conclusions
In conclusion, our prospective randomized sibling-oocyte study showed that early cumulus cell removal at 3 h after insemination resulted in embryos of greater quality, but also higher rates of polyspermy and low birth weight infants. These findings have never been previously reported. Further studies are required to investigate the advantages and disadvantages of early cumulus cell removal. A study which includes the long-term follow-up of newborns as a means to evaluate the effects of cumulus cell removal should also be performed.
Consent to publish
The study participants provided their consent to publish this article.
Ethical approval
All procedures involving human participants were performed in accordance with ethical standards developed by an institutional and/or national research committee, and were in compliance with the 1964 Helsinki declaration and its later amendments, or comparable ethical standards.
References
Centers for Disease Control and Prevention. 2013 Assisted reproductive technology fertility clinic succes rates report http://www.cdc.gov/art/pdf/2013-report/art-2013-fertility-clinic-report.pdf. Accessed on October 18th, 2015.
Bhattacharya S, Maheshwari A, Mollison J. Factors associated with failed treatment: an analysis of 121,744 women embarking on their first IVF cycles. PLoS One. 2013;8, e82249.
Chen C, Kattera S. Rescue ICSI of oocytes that failed to extrude the second polar body 6 h post-insemination in conventional IVF. Hum Reprod. 2003;18:2118–21.
Nagy ZP, Rienzi LF, Ubaldi FM, Greco E, Massey JB, Kort HI. Effect of reduced oocyte aging on the outcome of rescue intracytoplasmic sperm injection. Fertil Steril. 2006;85:901–6.
Enkhmaa D, Kasai T, Hoshi K. Long-time exposure of mouse embryos to the sperm produces high levels of reactive oxygen species in culture medium and relates to poor embryo development. Reprod Domest Anim. 2009;44:634–7.
Diaz-Fontdevila M, Pommer R, Smith R. Cumulus cell apoptosis changes with exposure to spermatozoa and pathologies involved in infertility. Fertil Steril. 2009;91:2061–8.
Wei D, Zhang C, Yin B, Wang P, Xie J, Song X, et al. Early cumulus cell removal could reduce the available embryo rate in human IVF. J Assist Reprod Genet. 2011;28:1213–6.
Xiong S, Han W, Liu JX, Zhang XD, Liu WW, Liu H, et al. Effects of cumulus cells removal after 6 h co-incubation of gametes on the outcomes of human IVF. J Assist Reprod Genet. 2011;28:1205–11.
Xue Y, Tong X, Jiang L, Zhu H, Yang L, Zhang S. Effect of cumulus cell removal 4 h post-insemination on fertilization and embryo quality: a prospective randomized sibling-oocyte study. J Assist Reprod Genet. 2013;30:1049–53.
Nagy ZP, Dozortsev D, Diamond M, Rienzi L, Ubaldi F, Abdelmassih R, Greco E. Pronuclear morphology evaluation with subsequent evaluation of embryo morphology significantly increases implantation rates. Fertil Steril. 2003;80:67–74.
Berger DS, Zapantis A, Merhi Z, Younger J, Polotsky AJ, Jindal SK. Embryo quality but not pronuclear score is associated with clinical pregnancy following IVF. J Assist Reprod Genet. 2014;31:279–83.
Morton PC, Yoder CS, Tucker MJ, Wright G, Brockman WD, Kort HI. Reinsemination by intracytoplasmic sperm injection of 1-day-old oocytes after complete conventional fertilization failure. Fertil Steril. 1997;68:488–91.
Parikh FR, Nadkarni SG, Naik NJ, Naik DJ, Uttamchandani SA. Cumulus coculture and cumulus-aided embryo transfer increases pregnancy rates in patients undergoing in vitro fertilization. Fertil Steril. 2006;86:839–47.
Cihangir N, Gorkemli H, Ozdemir S, Aktan M, Duman S. Influence of cumulus cell coculture and cumulusaided embryo transfer on embryonic development and pregnancy rates. J Turk Ger Gynecol Assoc. 2010;11:121–6.
Huang Z, Wells D. The human oocyte and cumulus cells relationship: new insights from the cumulus cell transcriptome. Mol Hum Reprod. 2010;16:715–25.
Wongsrikeao P, Kaneshige Y, Ooki R, Taniguchi M, Agung B, Nii M. Effect of the removal of cumulus cells on the nuclear maturation, fertilization and development of porcine oocytes. Reprod Domest Anim. 2005;40:166–70.
Gordon L, Joo JE, Powell JE, Ollikainen M, Novakovic B, Li X. Neonatal DNA methylation profile in human twins is specified by a complex interplay between intrauterine environmental and genetic factors, subject to tissue-specific influence. Genome Res. 2012;22:1395–406.
Kondapalli LA, Perales-Puchalt A. Low birth weight: is it related to assisted reproductive technology or underlying infertility? Fertil Steril. 2013;99:303–10.
Li GP, Bunch TD, White KL, Rickords L, Liu Y, Sessions BR. Denuding and centrifugation of maturing bovine oocytes alters oocyte spindle integrity and the ability of cytoplasm to support parthenogenetic and nuclear transfer embryo development. Mol Reprod Dev. 2006;73:446–51.
Niemitz EL, Feinberg AP. Epigenetics and assisted reproductive technology: a call for investigation. Am J Hum Genet. 2004;74:599–609.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
NG conducted the studies, participated in the sequence alignment, and drafted the manuscript. FY prepared and analyzed the data. QL & XR helped to design the study, and performed the statistical analyses. HZ & YL conceived of the study, participated in its design and coordination, and helped to draft the manuscript. JA gave final approval of the version to be published. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Guo, N., Yang, F., Liu, Q. et al. Effects of cumulus cell removal time during in vitro fertilization on embryo quality and pregnancy outcomes: a prospective randomized sibling-oocyte study. Reprod Biol Endocrinol 14, 18 (2016). https://doi.org/10.1186/s12958-016-0151-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12958-016-0151-3