Abstract
Background
Kikuchi-Fujimoto disease (KFD) is typically a benign, self-limiting inflammatory disease. However, some patients may have a prolonged or recurrent disease course, or present with life-threatening complications such as macrophage activation syndrome (MAS). In this study, we aimed to describe the incidence and clinical features of MAS in KFD and to access potential laboratory markers for the diagnosis of KFD-associated MAS.
Methods
Patients with KFD were retrospectively enrolled from January 2015 to November 2021 at Shenzhen Children’s Hospital. Clinical data were collected from inpatient or outpatient medical records. Data collected included clinical manifestations, laboratory and imaging findings, treatment, and clinical outcomes. Data were analyzed using GraphPad Prism 8.0 statistical software (GraphPad Software Inc., La Jolla, CA, USA). A receiver operating characteristic (ROC) curve analysis was further performed to access the potential predictors for the KFD-MAS diagnosis.
Results
Of 58 patients with a histological diagnosis of KFD, 15 (25.9%) patients had MAS. Compared to patients without MAS, patients with KFD-MAS presented with a higher proportion of skin rash (26.7%, p = 0.01), glucocorticoid treatment (80%, p = 0.003), and disease recurrence (33.3%, p = 0.04). KFD-MAS patients had lower absolute peripheral white blood cell (WBC, p = 0.02), platelet (p = 0.002), serum albumin levels (p = 0.01), and lymphocyte count (p < 0.0001), and higher lactate dehydrogenase (LDH) levels (p < 0.0001). ROC curve analysis showed that the cutoff values of absolute lymphocyte count, an absolute platelet count, serum albumin level, and serum LDH level for KFD-MAS diagnosis were < 1235/μL, < 171 × 106/μL, < 35.6 g/L, and > 679 IU/mL, respectively.
Conclusions
The presence of KFD-MAS in children may be more common than previously expected, especially in those with skin rash. KFD-MAS may be associated with a higher recurrence rate. An extremely elevated serum LDH level and moderate to severe lymphopenia may be useful diagnostic markers for MAS in KFD.
Trial registration
Not applicable; this was a retrospective study.
Similar content being viewed by others
Background
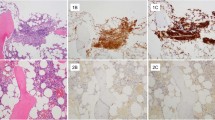
Kikuchi-Fujimoto disease (KFD), also known as histiocytic necrotizing lymphadenitis, is characterized by fever and cervical lymphadenopathy of unknown etiology. Systemic clinical manifestations may include night sweats, weight loss, fatigue, generalized lymphadenopathy, headaches, arthralgia, sore throat, rash, nausea, vomiting, and even neurological involvement [1]. As the symptoms and laboratory findings are non-specific, differential diagnoses include infectious lymphadenitis, malignancies such as lymphoma, and autoimmune diseases such as systemic lupus erythematosus (SLE) and juvenile idiopathic arthritis (JIA). Histopathological diagnosis by a lymph node biopsy is crucial to differentiate KFD from other etiologies.
KFD is typically a benign, self-limiting inflammatory process that resolves with supportive measures within months without any specific treatment. However, some patients may have a prolonged or recurrent disease course, or present with severe complications such as hemophagocytic Lymphohistiocytosis(HLH) [2,3,4]. HLH is a life-threatening syndrome of cytokine storm, characterized by hemophagocytosis, intractable fever, hepatosplenomegaly, cytopenia, hypertriglyceridemia, and hypofibrinogenemia. Serum proinflammatory cytokines, such as interferon-γ(or CXCL9 and CXCL10, chemokines induced by interferon-γ), interleukin-6, interleukin-10, and soluble interleukin-2 receptor alpha, a marker of T-cell activation, are usually excessively produced [5, 6]. Secondary HLH occurs in the setting of a malignant, infectious or autoimmune stimulus. Macrophage activation syndrome (MAS) is the term used to describe HLH that develops secondary to rheumatological diseases such as lupus and juvenile idiopathic arthritis, among others [7, 8]. The presence of MAS in adult KFD patients may be associated with adverse clinical outcomes including higher steroid usage and worse hospitalization outcomes, including a much higher rate of intensive care unit admission or in-hospital mortality [9]. The incidence and clinical features of MAS in KFD are not well understood in children. The potential markers for the diagnosis of MAS in children with KFD are still not well clarified.
Here, we performed a single, retrospective study to describe the incidence and clinical characteristics of MAS in children with KFD and to evaluate potential laboratory markers for the diagnosis of KFD-associated MAS (KFD-MAS).
Patients and methods
Study population and design
Patients with KFD were retrospectively enrolled from January 2015 to November 2021 at Shenzhen Children’s Hospital. The study was approved by the ethics committee of the hospital. Written informed consent was obtained from all patients’ legal guardians. All patients with KFD were confirmed based on a typical histological diagnosis. Exclusion criteria included patients with a possible alternative diagnosis such as autoimmune diseases (systemic lupus erythematosus, Sjogren's disease, etc.), leukemia, lymphoma, lymphoproliferative diseases, or active infection. Patients with other possible etiologies for HLH were not included either. Recurrence of KFD was defined as a diagnosis of KFD again after complete clinical remission over six months under immune-related drug withdrawal.
MAS was diagnosed according to the 2016 EULAR/ACR/PRINTO classification criteria, including fever, a ferritin level of ≥ 684 ng/mL, and fulfilling more than 2 of the following 4 criteria: platelet count ≤ 181,000/mL, aspartate aminotransferase (AST) level > 48 units/L, triglyceride level > 156 mg/dL, and fibrinogen level ≤ 360 mg/dL. KFD-associated MAS (KFD-MAS) was defined to fulfill the classification criteria for MAS and the diagnosis of KFD. Patients having MAS on admission and those who developed MAS within two weeks after admission were grouped as the KFD-MAS group.
Data collection
Clinical data were collected from inpatient or outpatient medical records. Data collected included clinical manifestations, laboratory and imaging findings, treatment, and clinical outcomes. The clinical symptoms and laboratory data were collected at the onset of KFD. The clinical manifestations were listed in Table 1. Laboratory variables included total leukocyte, neutrophils, lymphocyte and platelet counts, erythrocyte sedimentation rate (ESR), levels of hemoglobulin, C-reactive protein (CRP), aminotransferases, albumin, ferritin, fibrinogen, lactate dehydrogenase (LDH), and auto-antibodies such as anti-nuclear antibodies (ANA). Management included glucocorticoids, intravenous immunoglobulin (IVIG), cyclosporine, etoposide, antibiotics, and other immunosuppressants.
Statistical analysis
Continuous variables were presented as medians with interquartile ranges (IQR), and categorical variables were presented as frequencies and percentages. Unpaired Welch’s t-test for continuous data and Man-Whitney U test for categorical variables were performed. Variables were compared at the onset of KFD in patients who developed MAS within two weeks of KFD versus those who did not develop MAS. We subsequently performed a receiver operating characteristic (ROC) curve analysis for the data with statistical differences between the two groups. Analysis was performed with GraphPad Prism 8.0 statistical software (GraphPad Software Inc., La Jolla, CA, USA). A p-value of < 0.05 was considered statistically significant.
Results
The clinical characteristics of KFD patients
We identified 58 patients with a histological diagnosis of KFD in Shenzhen Children’s Hospital, including 15 patients with KFD-MAS (15/58, 25.9%). Clinical characteristics were summarized and compared between KFD patients without MAS and those with MAS in Table 1 and Additional file 1. The proportion of skin rash was significantly higher in the KFD-MAS group (p = 0.01). Four patients in the KFD-MAS presented with scattered erythematous macules, and only one had plantar erythema in patients without MAS. Most other clinical features were not significantly different between these two groups, including fever, arthralgia/arthritis, hepatosplenomegaly, evidence of acute infection, and other clinical manifestations (Table 1).
Comparison of the laboratory findings between KFD patients without MAS and those with MAS
Compared to KFD patients without MAS, the KFD-MAS group had significantly lower absolute peripheral white blood cell (WBC, p = 0.02), platelet (p = 0.002), serum albumin levels (p = 0.01), and lymphocyte count (p < 0.0001), and higher lactate dehydrogenase (LDH) levels (p < 0.0001). Serum ferritin, aspartate, and aminotransferase (AST) tended to be higher in the KFD-MAS group but were not significantly different between the two groups. There were no significant differences between the two groups in other laboratory data, including C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), triglyceride, fibrinogen, hemophagocytosis by bone marrow smear, and autoantibodies (Table 2).
Treatment and prognosis
Compared to KFD patients without MAS, patients with KFD-MAS had a significantly higher proportion of glucocorticoid treatment (p = 0.003) and KFD recurrence (p = 0.04). There were no significant differences between two the groups in other treatments or outcomes, including intravenous immunoglobulin (IVIG), cyclosporine, etoposide, tofacitinib, and progression to autoimmune diseases (Table 3).
Potential predictors for the KFD-MAS diagnosis
A ROC curve analysis was performed to access the potential laboratory markers for the KFD-MAS diagnosis. The results showed that an absolute lymphocyte count < 1235/μL (0.84, 95%CI: 0.74–0.95, p < 0.0001) distinguished the KFD-MAS group from the KFD without MAS group with 80.0% sensitivity and 79.1% specificity (Fig. 1 A). The cutoff values of an absolute platelet count, serum albumin level, and serum LDH level for KFD-MAS diagnosis were < 171 × 106/μL (ROC-AUC 0.76, 95%CI: 0.61–0.90, p = 0.003) (Fig. 1 B), < 35.6 g/L (ROC-AUC 0.76, 95%CI: 0.59–0.92, p = 0.01) (Fig. 1 C), and > 679 IU/mL (ROC-AUC 0.99, 95%CI: 0.97–1.0, p < 0.0001) (Fig. 1 D), respectively. From ROC curve analysis, the most useful candidate markers for predicting KFD-MAS were absolute lymphocyte count and serum LDH level (Table 4).
Discussion
In this study, as the previously reported incidence (30.8%) of MAS in KFD adults, a total of 25.9% of our patients presented with KFD-MAS [9]. The occurrence may be a bit overestimated since some mild cases without referral to our hospital might be missed. KFD tends to have female predominance with a female-to-male ratio of 1:3 in young patients of ages 15–18 years [10]. However, as some reported pediatric series [10,11,12], we found a greater proportion of males with KFD, especially in KFD-MAS patients with a female-to-male ratio of 1:2.75.
Most clinical manifestations between patients with KFD with and without MAS were not significantly different but there was a greater proportion of skin rash in our KFD-MAS patients. Similarly, despite no statistical significance, a previous report has found that a higher ratio of KFD-MAS patients tended to present with skin rash [9]. Therefore, there might be an association between skin rash and MAS in KFD, and future studies are required to confirm this interesting finding.
Compared to KFD patients without MAS, more KFD-MAS patients required glucocorticoid treatment. Corticosteroids and IVIG can be considered effective treatment options for KFD with and without MAS; etoposide could be an alternative regimen for severe KFD-MAS. Unlike the reported adult patients with KFD-MAS, our series showed no deaths. Compared to patients aged < 50 years, those aged 50 years and older had significantly higher mortality in KFD with MAS [9]. These findings suggest a possible better prognosis in younger patients, especially in the pediatric population with KFD-MAS.
Similar to most previous studies, our series had a noted higher recurrence rate of 15.5% than the reported recurrence rate of 3–4% in adults [11, 13, 14]. The higher recurrence rates in the pediatric population may be related to the difference in the immune status due to age and a possible higher diagnosis rate in those patients. Compared to KFD patients without MAS, our series showed a significantly higher recurrence rate in KFD-MAS patients. Previous studies have reported that leukopenia and lymphopenia were significantly associated with KFD recurrence [15, 16]. Thus, more severe leukopenia and lymphopenia may partially account for the higher recurrence rate in KFD-MAS patients.
A comparison of the laboratory findings showed a lower absolute peripheral white blood cell, platelet, serum albumin levels, lymphocyte count, and higher LDH levels in KFD-MAS patients. Further ROC curve analysis for the KFD-MAS diagnosis revealed that serum LDH level > 679 IU/mL had the highest areas under the ROC curve, and an absolute lymphocyte count < 1235/μL was the second. The diagnostic criteria for MAS in SJIA used in this study have not been validated for KFD. Clinical and laboratory characteristics of the patients, particularly the trend observed in the platelet count, levels of ferritin, transaminases, and fibrinogen, should still be the main elements in the early diagnosis of HLH in children. From these findings in this study, an extremely elevated serum LDH level and moderate to severe lymphopenia could help to find more patients with KFD-MAS.
The limitations of this study are the small sample size in a single center and the that it is retrospective. More than half of recurrences were diagnosed clinically without repeat lymph node biopsies. Bone marrow evaluation and serum TG levels were not detected in all patients. Future prospective studies with large sample sizes may help to further explore laboratory markers for the KFD-MAS diagnosis.
Conclusions
The presence of KFD-MAS in children may be more common than previously expected, especially in those with skin rash. It may be associated with a higher recurrence rate. Severe lymphopenia may be a helpful predictor for KFD recurrence. An extremely elevated serum LDH level and moderate to severe lymphopenia might be useful diagnostic markers for MAS in KFD.
Availability of data and materials
The datasets were collected from the medical records of participating patients at Shenzhen Children’s Hospital.
Abbreviations
- KFD:
-
Kikuchi-Fujimoto disease
- SLE:
-
Systemic lupus erythematosus
- JIA:
-
Juvenile idiopathic arthritis
- MAS:
-
Macrophage activation syndrome
- AST:
-
Aspartate aminotransferase
- ESR:
-
Erythrocyte sedimentation rate
- CRP:
-
C-reactive protein
- LDH:
-
Lactate dehydrogenase
- IVIG:
-
Intravenous immunoglobulin
- IQR:
-
Interquartile ranges
- ROC:
-
Receiver operating characteristic curve
References
Masab M, Surmachevska N, Farooq H. Kikuchi Disease. 2022.
Yang Y, Lian H, Ma H, Zhao Y, Zhang Q, Zhang L, et al. Hemophagocytic Lymphohistiocytosis Associated with Histiocytic Necrotizing Lymphadenitis: A Clinical Study of 13 Children and Literature Review. J Pediatr. 2021;229:267-274.e3.
Lim GY, Cho B, Chung NG. Hemophagocytic lymphohistiocytosis preceded by Kikuchi disease in children. Pediatr Radiol. 2008;38(7):756–61.
Sykes JA, Badizadegan K, Gordon P, Sokol D, Escoto M, Ten I, et al. Simultaneous Acquired Self-limited Hemophagocytic Lymphohistiocytosis and Kikuchi Necrotizing Lymphadenitis in a 16-Year-Old Teenage Girl: A Case Report and Review of the Literature. Pediatr Emerg Care. 2016;32(11):792–8.
Fajgenbaum DC, June CH. Cytokine Storm. N Engl J Med. 2020;383(23):2255–73.
Henderson LA, Canna SW, Schulert GS, Volpi S, Lee PY, Kernan KF, et al. On the Alert for Cytokine Storm: Immunopathology in COVID-19. Arthritis Rheumatol. 2020;72(7):1059–63.
Henderson LA, Cron RQ. Macrophage Activation Syndrome and Secondary Hemophagocytic Lymphohistiocytosis in Childhood Inflammatory Disorders: Diagnosis and Management. Paediatr Drugs. 2020;22(1):29–44.
De Matteis A, Colucci M, Rossi MN, Caiello I, Merli P, Tumino N, et al. Expansion of CD4dimCD8+ T cells characterizes macrophage activation syndrome and other secondary HLH. Blood. 2022;140(3):262–73.
Ahn SS, Lee B, Kim D, Jung SM, Lee SW, Park MC, et al. Evaluation of macrophage activation syndrome in hospitalised patients with Kikuchi-Fujimoto disease based on the 2016 EULAR/ACR/PRINTO classification criteria. PLoS ONE. 2019;14(7): e0219970.
Kim TY, Ha KS, Kim Y, Lee J, Lee K, Lee J. Characteristics of Kikuchi-Fujimoto disease in children compared with adults. Eur J Pediatr. 2014;173(1):111–6.
Selvanathan SN, Suhumaran S, Sahu VK, Chong CY, Tan N, Thoon KC. Kikuchi-Fujimoto disease in children. J Paediatr Child Health. 2020;56(3):389–93.
Lin HC, Su CY, Huang SC. Kikuchi’s disease in Asian children. Pediatrics. 2005;115(1):e92–6.
Hutchinson CB, Wang E. Kikuchi-Fujimoto disease. Arch Pathol Lab Med. 2010;134(2):289–93.
Kang HM, Kim JY, Choi EH, Lee HJ, Yun KW, Lee H. Clinical Characteristics of Severe Histiocytic Necrotizing Lymphadenitis (Kikuchi-Fujimoto Disease) in Children. J Pediatr. 2016;171:208-12.e1.
Jung HJ, Lee IJ, Yoon SH. Risk Assessment of Recurrence and Autoimmune Disorders in Kikuchi Disease. Risk Manag Healthc Policy. 2020;13:1687–93.
Song JY, Lee J, Park DW, Sohn JW, Suh SI, Kim IS, et al. Clinical outcome and predictive factors of recurrence among patients with Kikuchi’s disease. Int J Infect Dis. 2009;13(3):322–6.
Acknowledgements
We thank all the patients and their families for their participation.
Funding
This work was supported by the Sanming Project of Medicine in Shenzhen (SZSM201812002) and the Shenzhen Key Medical Discipline Construction Fund (SZGSP012).
the Sanming Project of Medicine in Shenzhen,SZSM201812002,Jun Yang,the Shenzhen Key Medical Discipline Construction Fund,SZGSP012
Author information
Authors and Affiliations
Contributions
Zixuan Shen designed the work, collected and analyzed the data. Jiayun Ling and Xiaona Zhu helped to collect the data. Jun Yang supervised the work and reviewed the manuscript. Tingyan He supervised the work, drafted and reviewed the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participating members were enrolled with the approval of the ethics committee of Shenzhen Children’s Hospital and provided written consent from legal guardians.
Consent for publication
Written consent for publication of this anonymous information was obtained from patients’ legal guardians.
Competing interests
All authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shen, Z., Ling, J., Zhu, X. et al. Macrophage activation syndrome in children with Kikuchi-Fujimoto disease. Pediatr Rheumatol 21, 10 (2023). https://doi.org/10.1186/s12969-023-00788-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12969-023-00788-w