Abstract
Purpose
To evaluate the cost-effectiveness of a multifaceted workplace intervention to reduce musculoskeletal pain (MSP) in nursing staff.
Methods
The study was a 1-year cluster-randomized controlled trial. The intervention combined participatory ergonomics, health promotion, and case management. The control group received usual care. Societal and health system perspectives were used. Costs included direct health and indirect costs. The effects were MSP and quality-adjusted life years (QALYs). MSP was measured using the Standardized Nordic Questionnaire at baseline and 6- and 12-month follow-up. QALYs were measured using the EuroQol-5D-3L at 6- and 12-month follow-up. Incremental costs and QALYs were modelled using generalized linear models. MSP was analysed through generalized logistic models. Incremental cost-effectiveness ratios (ICERs) were calculated, and cost-effectiveness planes and acceptability curves were constructed.
Results
Total mean costs per person were €614 and €216 for the intervention and control group, respectively, with a societal perspective. The intervention mean cost was €38/person. From the societal perspective, the ICER showed that overall additional €68 (€9 from a health system perspective) were required to achieve 1-extra-percentage-point reduction of MSP. ICERs were €34 from the societal and €4 from the health system perspectives for neck, shoulders and upper back pain; €53 and €7 for low back; €179 and €23 for hands; €39 and €5 for legs; €115 and €14 for the knees; €36 and €5 for feet For MSP in the elbows. For participants with pain in the elbow, and for QALYs, the ICER showed that the intervention group was dominated by the control group.
Conclusion
This intervention was not cost-effective in terms of QALYs. However, in terms of MSP, with a willingness to pay of €100, the probability of the intervention being cost-effective was around 90%. Further studies incorporating our recommendations are needed to confirm these findings.
Study Registration
ISRCTN15780649, retrospectively registered.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Musculoskeletal pain is one of the leading contributors to disability worldwide [1]. Low back pain has been the single leading cause of disability globally since 1990, and musculoskeletal pain global prevalence and incidence are increasing [1]. In Europe, musculoskeletal pain is the most common work-related health condition [2], causing 50% of sick leave episodes and 60% of permanent disabilities, generating an estimated cost between 2.6 and 3.8% of the gross domestic product [3, 4].
The prevalence of musculoskeletal pain in nursing staff (i.e. nurses and aides) is around 70–80% in several European countries [5, 6]. In particular, nursing staff who work in hospitals with daily patient handling have almost twice the risk of developing work-related back pain compared with nurses without daily patient handling [7, 8]. Moreover, musculoskeletal pain has a multi-causal origin and is influenced by other non-occupational, individual (e.g. sex, age, genetic factors), psychological, and cultural factors (e.g. health beliefs, somatization) that play an important role in its incidence and management [9].
Musculoskeletal pain clearly requires the adoption of preventive measures in the workplace and the management of nursing staff who already have some complaint, to allow them to continue working and, if necessary, to reintegrate them into the workplace after related sick leave. Several systematic reviews suggest that multicomponent interventions that combine several specific approaches and those that incorporate participatory elements in the intervention process can obtain better results [10,11,12,13]. Therefore, a combination of interventions including primary prevention (aiming to protect healthy people from the possibility of becoming ill or suffering an injury), secondary prevention (early diagnosis and action once the first symptoms or signs of the disease have appeared), and tertiary prevention (to manage long-term health problems, as chronic pain, functional capacity or sick leave) is needed.
In healthcare settings, adapting to the continuous development of new treatments, interventions, and approaches with limited resources is a crucial challenge [14]. Decision-makers benefit from economic evaluations on the efficiency of interventions [15]. In the last decades, the use of patient-reported outcome measures (PROMs) has been increasing. PROMS are usually questionnaires that capture a person’s perception of their own health, as, for example, musculoskeletal pain or quality of life [16]. Their use is highly recommended not only for effectiveness evaluation, but also for economic evaluations as these measures help to understand the patient-relevant outcomes and can be used to influence healthcare decisions on effective therapies, along with clinical and economic outcomes [17, 18].
This economic evaluation is framed in the “INTEVAL_Spain” intervention [19]. It was an intention-to-treat, cluster-randomized controlled trial that aimed to evaluate a multifaceted, evidence-based, workplace intervention comprising three levels of prevention. The intervention included participatory ergonomics: a healthy lifestyle promotion programme with Nordic Walking, mindfulness, and a healthy diet (primary prevention), and a tailored case management programme (secondary and tertiary prevention). Effectiveness evaluation showed that the intervention was effective to reduce neck, shoulder, and upper back pain [20] and suggested that a multifactorial approach is needed to reduce musculoskeletal pain.
The objective of this study was to evaluate the cost-effectiveness and cost utility of this complex workplace intervention designed to reduce musculoskeletal pain in nursing staff.
Methods
The INTEVAL_Spain Intervention
The study was designed as a two-armed, cluster-randomized, controlled trial with 1-year follow-up. Full details of the INTEVAL_Spain protocol, effectiveness analysis, and process results are available elsewhere [19,20,21].
Study Context and Population
The intervention was conducted from September 2016 to December 2017 in two main tertiary hospitals in Barcelona and Sabadell (Spain), each of which had a workforce of 4000 workers, of whom around 60% were nursing staff, and had an experienced in-house occupational health service (OHS).
Clusters were independent hospital units and participants were the nurses and aides working in these hospital units. A total of eight clusters were selected and randomized, with the respective nursing staffs numbering between 20 and 60 in each cluster. All nursing staff from these units were eligible for the study. Exclusion criteria included temporary nursing staff who had worked less than 3 months, those who worked in several units, and those who were on sabbatical leave.
Information briefings were held in person in each cluster before randomization, to collect informed consent and administer the ERGOPAR baseline questionnaire [22, 23]. The questionnaires were anonymous. Follow-up questionnaires were administered at 6 and 12 months. Moreover, the nursing staff could sign the informed consent and join the study at any time during that year (e.g. a nurse who did not take the baseline questionnaire could fill in the follow-up questionnaires and/or participate in the activities).
Interventions
Intervention Group
This study aimed to reduce musculoskeletal pain through an intention-to-treat intervention comprising three levels of prevention. It consisted of (1) participatory ergonomics (primary prevention), (2) a healthy lifestyle promotion programme composed of Nordic Walking, mindfulness, and a healthy diet (primary prevention), and (3) a tailored case management programme (secondary and tertiary prevention).
Participatory ergonomics training was based on the ERGOPAR method and was led by an expert ergonomist of the OHS of each corresponding hospital [22]. Briefly, an Ergo group was created and included the ergonomist, a volunteer nurse, and/or nursing aide from each shift (morning, afternoon, and two night shifts), the unit supervisor/s, one prevention delegate (i.e. representative of workers in the field of occupational risk prevention), and the project coordinator. They held 1-h weekly meetings for 3 weeks to identify the ergonomic problems in their hospital unit, prioritize them, and propose preventive measures. In between these meetings, the volunteers of the Ergo group held discussions with their co-workers in the work units about the subject discussed in the meetings, to provide feedback for the next meeting. Finally, the OHS led an Operative group composed by the key managers of each hospital (e.g. managers from the economics department, human resources, cleaning/maintenance, etc.). This group held monthly meetings to implement the preventive measures (e.g. purchase of sliding sheets and footrests, repair, and maintenance of the wheels of the medication carts, redistribution of the rooms in order to facilitate mobility, etc.).
The healthy lifestyle promotion programme included three group activities: Nordic Walking training [24], mindfulness course based on Mindfulness-Based Stress Reduction [25], and a 3-h formative session about the Mediterranean diet carried out by an expert chef [26].
The tailored case management programme consisted of a multidisciplinary care system for the early detection of disabling musculoskeletal pain and, if necessary, support for return to work. Nursing staff with musculoskeletal pain self-referred to the case manager or were referred by their supervisor or an occupational health physician. A case manager generated a risk profile (i.e. low, medium, or high risk for persistent musculoskeletal symptoms) through a telephone interview using a questionnaire composed of several scales [9, 27,28,29,30,31,32]. Low-risk cases attended a health-beliefs educational session related to musculoskeletal pain. Medium- and high-risk cases were discussed in the weekly clinical session of the OHS to decide the specific treatment, including medical consultation with an occupational physician, rehabilitation service (physician consultation and physiotherapy), and cognitive behavioural therapy by a psychologist.
The implementation of components was progressive to facilitate participation and logistics [21]. All the interventions were conducted during time off work.
Control Group
The OHS carried out the usual occupational health practices for the intervention and control units. These practices included investigation of occupational injuries, risk assessments, smoking cessation programmes, health surveillance, training, expert assessment in occupational health, recommendations of workplace adaptations, and clinical support and management of permanent disability.
Economic Analysis
An economic evaluation was conducted from both a societal and a health system perspective. The societal perspective included the costs of all types of health services (direct costs) and productivity loss costs (indirect costs). The health system perspective included only direct costs from the Spanish public healthcare services. The time frame of this study was 1 year, and consequently, no discount rate was applied. All costs are expressed in euros (€) for the reference year 2022.
Costs
Cost data were collected for the entire study period and for 1 year before the study from several sources specified below. Costs of 1 year before the study were collected in order to adjust the analyses. Table 1 shows the unit costs.
Direct Health Costs
Direct health costs included hospital costs and primary care use of resources.
Hospital costs were obtained from a detailed analytical accounting system implemented in Hospital del Mar (Barcelona) [33] for the reference year 2017 and updated to 2022 using the Spanish Healthcare Consumer Price Index. Hospital services were classified using homogeneous and functional groups and included traumatology surgery, traumatology hospitalization, hospitalized rehabilitation (i.e. physiotherapy sessions), ambulatory rehabilitation, ambulatory traumatology, traumatology emergencies, and diagnostic tests related to musculoskeletal pain.
Primary care costs were calculated by multiplying the number of health service provided by their unit cost. Primary care services included musculoskeletal pain-related physician visits, diagnostic tests, and medication. Data were obtained from the Shared Clinical History in Catalonia [34]. Unit costs of physician visits and diagnostic tests were obtained from the tariffs corresponding to the services provided by the public provider (Catalan Institute of Health) for the year 2022 [35]. Costs of medication were calculated as the mean price of each medical prescription; that is, when a medication had several formats, we summed up the prices and divided to obtain the mean cost of the medication (Supplementary Table 1). Also, when medication information specified only “Nonsteroidal Anti-Inflammatory Drugs”, the cost was calculated as the mean cost of a full medical prescription of ibuprofen, as it is the most prescribed Nonsteroidal Anti-Inflammatory Drug in Spain [36]. Costs were obtained from the Spanish Pharmaceutical Vademecum (hppt: //www.vademecum.es) for the year 2022.
Indirect Cost: Work Loss
Costs of work loss were calculated, according to the human capital approach of 2022, by multiplying the days on sick by the gross salary of nurses and aides in Spain, obtained from the Catalan Institute of Health tariffs for the reference year 2022 [37]. Sick leave data were available for all workers who signed the informed consent. Data were obtained from the human resources department of each hospital. The episodes were registered by the OHS using the group code of the International Classification of Diseases, 10th revision. Episodes related to musculoskeletal pain were included in the analyses. Red flags, including bone fractures and surgery in the previous 3 months, rheumatic pathologies, pregnancy (e.g. low back pain related to pregnancy), and recurrent episodes of sick leave were excluded from the analyses.
Intervention Costs
Costs of ergonomist, Nordic Walking trainer, mindfulness instructor, and chef were estimated as price per hour for the year 2017 and updated to 2022 using the Consumer Price Index (CPI). For each of these group activities, the costs were summed up and divided by the number of participants, thus assigning the same value to each participant.
Case management was an individual service, so the costs were calculated individually for each user according to the services they attended. Case manager cost was estimated as the cost per case and updated to 2022 using the CPI. Health education beliefs professional cost was calculated as price per hour using the minimum wage in Spain for the reference year 2022. Occupational physician visit, rehabilitation physician, physiotherapy, and cognitive behavioural therapy psychologist visits were obtained from the Catalan tariffs for 2022 [35].
Health Effects
Self-perceived musculoskeletal pain was measured using a validated Spanish version of the Standardized Nordic Questionnaire at baseline and 6- and 12-month follow-up [22, 23, 38]. Data were collected with the question “Do you have pain or discomfort in this anatomical site?”. There were three possible answers (1) yes, pain, (2) yes, discomfort, and (3) no pain. Answers were dichotomized (yes pain or discomfort, no pain). The question was asked at present. The seven anatomical sites were included in the questionnaire (i.e. neck, shoulders and upper back, elbows, hands, legs, knees, and feet). In addition, an overall dichotomous variable was created on whether the nurse/nursing aide reported pain or discomfort in at least one anatomical site.
Quality-adjusted life years were measured using a validated Spanish version the EuroQol 5-dimensional questionnaire [29]. This tool is composed of a self-reported description of health problems according to a 5-dimensional classification (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). For self-reported health with the 5-dimensional classification, workers marked one of three levels of severity in each dimension (1 = no problems, 2 = some/moderate problems, and 3 = severe/extreme problems). Perfect health status is coded as “11,111”. Each health status has a utility based on a country’s median score, where 1 represents perfect health, 0 represents death, and negative numbers symbolize statuses which are considered worse than death. Spanish scores were used to estimate the utility of the health status described by the participants [39]. Quality-adjusted life years were calculated by multiplying the utility by the amount of time a patient spent in a particular health state. EuroQol 5-dimensional questionnaire was not included at baseline, and consequently, quality-adjusted life years’ data were available only at 6- and 12-month follow-ups.
Pairing Data
In our study, effects data could not be paired, as the questionnaires were anonymous and lacked identifiers. This decision was taken to encourage participation and ensure reliability of responses, as the questionnaires were self-administered at the workplace and included personal questions and questions about the respondent’s relationship with their co-workers and supervisors.
Statistical Analysis
Analyses were performed based on the intention-to-treat principle, analysing all participants according to the randomized group to which they belonged, whether or not they were actively participating in the intervention. All the analyses were performed from both the societal and health system perspectives. To evaluate the goodness of fit of the models, we used the Bayesian Information Criterion (BIC) in which a lower value indicates a better fit.
Costs
Primary care and total costs from both perspectives had missing values, which were missing at random and ranged from 23 (11.2%) to 26 (12.7%). Mean costs during the study period by group were calculated using a linear regression adjusted by age and occupation. The incremental cost (difference in cost between the intervention and the control groups) was calculated as the average marginal effects with a generalized linear model (family gamma and link log), adjusted for age, occupation, and the costs for 1 year before the study.
Effects
The effect of the intervention was obtained for the intervention and the control group, as the difference on prevalence data at 12-month follow-up compared to their baseline prevalence. This incremental effect on musculoskeletal pain was calculated as the difference in the effect obtained in the intervention group compared to the effect obtained in the control group. First, we estimated a generalized logistic model (family binomial and link logit) for pain, with an interaction between time and group as independent variables, and adjusted for age. The prevalence of pain for each group and time point was estimated from the GLM as the average marginal effects, i.e. averaging the observations (probability) predictions from the model.
The incremental effect on quality-adjusted life years was calculated by comparing 12-month follow-up data with 6-month follow-up data, since baseline data were not available, and the average marginal effects were estimated through a generalized linear model with family gamma and link log, adjusted for age.
Incremental Cost-Effectiveness Ratios (ICERs)
Multiple imputation by chained equations using predictive mean matching and 40 imputed databases was used to deal with the missing data. ICERs were calculated as the difference in the cost between the intervention and the control group, divided by the difference in the effect of each outcome (musculoskeletal pain and quality-adjusted life years). A probabilistic cost-effectiveness analysis was performed based on 5000 bootstrap replications and cost-effectiveness planes and acceptability curves were constructed for the ICERs from societal and health system perspectives to assess the uncertainty around the estimates [40, 41]. The proportions of (bootstrapped) ICERs in each quadrant were calculated.
The analyses were performed using STATA 17 (Stata Statistical Software Release 17; StataCorp, College Station, TX).
Results
Participants
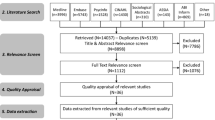
The eight clusters included 473 nurses and aides. Eighteen workers were excluded because they were on a sabbatical leave. At baseline, 293 nurses and aides signed the informed consent to participate and 257 answered the baseline questionnaire, 138 in the intervention group, and 119 in the control group. Costs data were collected for 134 participants in the intervention group and 71 in the control group. During the fieldwork, one of the control clusters (n = 105; informed consent n = 53) started a period of reorganization and left the study (Fig. 1). No adverse effects were reported to the OHS.
Table 2 shows that, at baseline, the participants in both groups were similar with regard to sex (84% women), age (53% between 31 and 49 years), occupation (63% nurses and 37% nursing aides), and self-perceived musculoskeletal pain (ranged from 95% overall to 10% in elbows). Quality-adjusted life years were 0.757 and 0.751 in the intervention and control group, respectively, at 6 months’ follow-up (baseline data not available). Baseline characteristics of workers by cluster are described in Supplementary Table 2.
Costs
During the study period, the total mean cost per person in the intervention group was €614 and €216 in the control group with a societal perspective. Total mean direct health costs during the study period were also slightly higher in the intervention group (€95/person) than in the control group (€90/person). Work loss mean cost had a cost of €408/person for the intervention group and €115/person for the control group. The mean cost of the workplace intervention was €38/person.
Cost-Effectiveness Analysis
Table 3 shows the incremental costs, the incremental effects (i.e. the difference between the effect in the intervention group and the control group) and the ICERs. The ICERs showed that an additional €68 (from a societal perspective) and €8 (from a health system perfective) were required to achieve 1-extra-percentage-point reduction in overall musculoskeletal pain in the intervention group compared to the control group. The ICERs from the societal and health system perspectives were, respectively, €34 and €4 for musculoskeletal pain in neck, shoulders, and upper back; €53 and €7 in the low back; €179 and €23 in the hands; €39 and €5 in the legs; €115 and €14 in the knees; and €36 and €5 in the feet. Musculoskeletal pain in elbows and quality-adjusted life years worsened in the intervention group compared with the control group, and the costs were higher. The ICER for elbows and QALYs showed that the intervention group was dominated by the control group. The ICER for elbows and QALYs showed that the intervention group was dominated by the control group.
Figure 2a shows the cost-effectiveness plane for the analysis of overall musculoskeletal pain with both societal and health system perspectives. In both perspectives, around 90% of the ICERs were distributed in the North-East quadrant (most effective and costly intervention) and 0 to 4% in the South-East quadrant (most effective and less expensive intervention). Figure 2b shows the cost-effectiveness plane for quality-adjusted life years. In both societal and health system perspectives, 60 to 70% of ICERS were distributed in the North-East quadrant and 0 to 3% for societal and for health system in the South-East quadrant. Acceptability curves (Supplementary Fig. 1) shows that for a willingness to pay of €100, the probability of the intervention being cost-effective for musculoskeletal pain was around 90% in both perspectives. For QALY, acceptability curves showed that with a willingness to pay of €25,000, the probability of the intervention being cost-effective was around 67% in both perspectives. Cost-effectiveness planes of musculoskeletal pain for each anatomical site (i.e. neck, shoulders, and upper back, low back, elbows, hands, legs, knees, and feet) from both societal and health system perspectives are shown in Supplementary Fig. 2.
Cost-effectiveness plane of a musculoskeletal pain in overall and b quality-adjusted life years of the intervention group compared to the control group at 12 months’ follow-up with societal and health system perspective. MSP Musculoskeletal pain. QALYs Quality-adjusted life years. % shows the percentages of dots in each quadrant. Blue dot shows the cost-effectiveness data of the original database
Discussion
The intervention showed that to achieve a 1-extra-percentage-point reduction in musculoskeletal pain overall in the intervention group compared with the control group, an additional €12 was needed from a societal perspective and €6 from a health system perspective. For quality-adjusted life years, the usual care dominated.
Comparison with the Existing Literature
Economic evaluations of multifaceted interventions in the workplace to reduce and manage musculoskeletal pain in nursing staff are scarce, and we did not find any study that used musculoskeletal pain as outcome for a cost-effectiveness analysis.
Musculoskeletal pain, as well as the EQ-5D, is a patient-reported outcome measure (PROM). Hospitals and healthcare services can better meet the needs and preferences of their patients by responding to PROM’s questionnaires. These measurements are intended to close a critical gap in our understanding of patient-relevant outcomes by providing useful source of data to influence healthcare decisions on effective therapies, along with clinical and economic outcomes [16,17,18, 42]. Despite the recommendations of using PROMs in effectiveness and cost-effectiveness studies, musculoskeletal pain has not been used previously in cost-effectiveness analysis. Thus, there is no established threshold in the literature for the maximum amount of money that may be required for an intervention to reduce musculoskeletal pain and still be considered cost-effective, which can be a barrier to stablish recommendations.
We found two previous cost-effectiveness evaluations of a multicomponent intervention for musculoskeletal pain in workers. Suni et al. (2018) study consisted of neuromuscular exercise and back-care counselling in female healthcare workers with non-specific low back pain and lasted 12 months. The authors concluded that the combined arm (i.e. the study arm combining neuromuscular exercise and back-care counselling) was effective in reducing pain, but was not cost-effective on sick leave and quality-adjusted life years [43]. Otherwise, Tingulstad et al. (2023) concluded that their multicomponent intervention for workers on sick leave due to musculoskeletal disorders was cost-effective in terms of quality-adjusted life years [44]. In our study, the intervention was also effective to reduce pain, especially in those anatomical sites with a higher prevalence of pain (e.g. neck, shoulders, and upper back), but it entailed a higher cost than the usual care. However, acceptability curves showed that by increasing the willingness to pay, the probability of being efficient could reach 90% with a 100€/1-percentual-point reduction of musculoskeletal pain. In terms of quality-adjusted life years, our intervention was neither efficient as the mean quality-adjusted life years was lower in the intervention group compared with the control group. Despite this, this result should be interpreted carefully, as we did not have the baseline measure for quality-adjusted life years.
In relation to sick leave, the intervention evaluated by Suni et al. was not efficient [43]. In contrast, the intervention evaluated by Steenstra et al., [45] consisting in a multi-stage return-to-work programme for workers on sick leave due to low back pain, found that an additional expenditure of €19 was required in the workplace intervention to reduce sick leave due to musculoskeletal pain by 1 day compared with usual care [45]. In our study, sick leave was included in the societal perspective analysis, showing higher mean costs in the intervention group (€408) compared to the control group (€155). A longer follow-up is recommended to detect differences in sick leave [46]. Also, in our intervention, the case management programme was the component focused on return to work, but only 13 workers participated and only 5 finished it (data not shown) [21]. Perhaps, a higher implementation of this component could have decreased sick leave duration and improved the efficiency of our intervention.
Limitations
This study has some limitations. The main limitation is that the questionnaires were anonymous, and an identifier was not created to guarantee confidentiality, so effects data could not be paired. Second, the baseline questionnaire did not include the EuroQol 5-dimensional questionnaire, and therefore quality-adjusted life years’ data were only available for the 6- and 12-months follow-ups. Perhaps we would have found an effect on quality-adjusted life years by comparing baseline data with the 12-month follow-up. Third, effectiveness results could have been limited by the process implementation, as the intervention had a slightly lower implementation than expected [47]. Recommendations to improve the implementation have been published elsewhere [47]. Finally, other information regarding costs and effectiveness might be missing, as no information was available on whether nursing staff consumed over-the-counter medication, or whether they went to private hospitals or services (e.g. physiotherapy consultations, etc.).
Study Implications and Future Research
This intervention could be a first approach to develop efficient interventions to reduce and manage musculoskeletal pain in nursing staff at work. Given that this study shows that the willingness to increase the spending needed to improve musculoskeletal pain is currently low, health policy makers should consider these types of evidence-based, multifaceted workplace interventions to improve musculoskeletal pain in nursing staff.
Studies in the economic evaluation of multifaceted interventions with paired data are needed to reinforce the quality of the analyses and confirm the findings of this study. Quality-adjusted life years should be measured from the baseline, and a longer follow-up is recommended [46]. Also, as suggested by other authors, we recommend adding an economic evaluation to any future randomized controlled trial, and collaboration with health economists or researchers with expertise in this area. Finally, to establish a threshold for musculoskeletal pain PROM could be a useful basis to promote recommendations.
Conclusion
This intervention reduced musculoskeletal pain, but was not cost-effective in terms of quality-adjusted life years. ICERs, in terms of musculoskeletal pain, showed that an additional €68 from a societal perspective and €9 from a health system perspective were needed to achieve an additional 1 percentage point reduction overall in musculoskeletal pain in the intervention group compared to the control group. With a willingness to pay of €100, the probability of the intervention being cost-effective for musculoskeletal pain was around 90%. For quality-adjusted life years, the usual care dominated the intervention. Further studies incorporating our recommendations are needed to confirm these findings.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- OHS:
-
Occupational Health Service
- ICERS:
-
Incremental Cost-Effectiveness Ratios
- PROM:
-
Patient-Reported Outcome Measure
References
World Health Organization. Occupational health. Workplace health promotion. [Internet]. 2022 [cited 25 May 2023]. Available in: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions
Kok de J, Vroonhof P, Snijders J, Roullis G, Clarke M, Peereboom K, van DP, Isusi I. Work-related musculoskeletal disorders: prevalence, costs and demographics in the EU. European Agency for Safety and Health at work. 2019.
Gauthy R. Musculoskeletal disorders. An ill-understood “pandemic”. European Trade Union Institute, 2007 ISBN: 978-2-87452-100-3.
Okunribido O, Wynn T. Aging and work-related musculoskeletal disorders: a review of the recent literature. Norwich, UK: Health and Safety Executive. 2010;RR799.
Pinilla García J, Almodóvar Molina A, Galiana Blanco ML, Hervás Rivero P, Zimmermann Verdejo M. National Survey of Working Conditions. 2015 6th EWCS—Spain. Madrid (Spain): National Institute of Safety and Hygiene at Work, 2017.
Bernal D, Campos-Serna J, Tobias A, Vargas-Prada S, Benavides FG, Serra C. Work-related psychosocial risk factors and musculoskeletal disorders in hospital nurses and nursing aides: a systematic review and meta-analysis. Int J Nurs Stud. 2015;52:635–648.
Holtermann A, Clausen T, Aust B, Mortensen OS, Andersen LL. Risk for low back pain from different frequencies, load mass and trunk postures of lifting and carrying among female healthcare workers. Int Arch Occup Environ Health. 2013;86(4):463–470.
Andersen LL, Burdorf A, Fallentin N, Persson R, Jakobsen MD, Mortensen OS. Patient transfers and assistive devices: prospective cohort study on the risk for occupational back injury among healthcare workers. Scand J work Environ Health. 2014;40:74–81.
Vargas-Prada S, Serra C, Martínez JM, Ntani G, Delclos G, Palmer KT, Coggon D, Benavides FG. Psychological and culturally-influenced risk factors for the incidence and persistence of low back pain and associated disability in Spanish workers: findings from the CUPID study. Occup Environ Med. 2013;70(1):57–62.
Cullen KL, Irvin E, Collie A, Clay F, Gensby U, Jennings PA. Effectiveness of workplace interventions in return-to-work for musculoskeletal, pain-related and mental health conditions: an update of the evidence and messages for practitioners. J Occup Rehabil. 2018;28(1):1–15.
Hoefsmit N, Houkes I, Nijhuis F. Intervention characteristics that facilitate return to work after sickness absence: a systematic literature review. J Occup Rehabil. 2012;22:462–477.
Hignett S. Intervention strategies to reduce musculoskeletal injuries associated with handling patients: a systematic review. Occup Environ Med. 2003;60(9):E6.
Tullar JM, Brewer S, Amick BC 3rd, Irvin E, Mahood Q, Pompeii LA, Wang A, Van Eerd D, Gimeno D, Evanoff B. Occupational safety and health interventions to reduce musculoskeletal symptoms in the health care sector. J Occup Rehabil. 2010;20(2):199–219.
Chandra A, Skinner J. Technology growth and expenditure growth in health care. J Econ Lit. 2012;50:645–680.
Steel J, Godderis L, Luyten J. Methodological challenges in the economic evaluation of occupational health and safety programmes. Int J Environ Res Public Health. 2018;15:2606.
Kluzek S, Dean B, Wartolowska KA. Patient-reported outcome measures (PROMs) as proof of treatment efficacy. BMJ Evid Based Med. 2022;27:153–155.
Williams K, Sansoni J, Morris D, Grootemaat P and Thompson C. Patient-reported outcome measures: literature review. Sydney: ACSQHC; 2016. [cited 25 May 2023]. Available in: https://www.safetyandquality.gov.au/sites/default/files/migrated/PROMs-Literature-Review-December-2016.pdf
Gibbons C, Porter I, Gonçalves-Bradley DC, Stoilov S, Ricci-Cabello I, Tsangaris E, Gangannagaripalli J, Davey A, Gibbons EJ, Kotzeva A, Evans J, van der Wees PJ, Kontopantelis E, Greenhalgh J, Bower P, Alonso J, Valderas JM. Routine provision of feedback from patient-reported outcome measurements to healthcare providers and patients in clinical practice. Cochrane Database Syst Rev. 2021;10(10):CD011589.
Serra C, Soler-Font M, García AM, Vargas-Prada S, Peña P, Ramada JM. Prevention and management of musculoskeletal pain in nursing staff by a multifaceted intervention in the workplace: design of a cluster randomized controlled trial with effectiveness, process and economic evaluation (INTEVAL_Spain). BMC Public Health. 2019;19:348.
Soler-Font M, Ramada JM, van Zon SKR, Almansa J, Bültmann U, Serra C. Multifaceted intervention for the prevention and management of musculoskeletal pain in nursing staff: results of a cluster randomized controlled trial. PLoS ONE. 2019;14(11):e0225198.
Soler-Font M, Ramada JM, Merelles A, Amat A, de la Flor C, Martínez O, Palma-Vasquez C, Sancho C, Peña P, Bültmann U, van Zon SKR, Serra C. Process evaluation of a complex workplace intervention to prevent musculoskeletal pain in nursing staff: results from INTEVAL_Spain. BMC Nurs. 2021;20(1):189.
Gadea R, Sevilla M, García A. ERGOPAR 2.0. A participatory ergonomics procedure for the prevention of musculoskeletal disorders of occupational origin. Madrid: Trade Union Institute of Work, Environment and Health (ISTAS); 2014.
García AM, Gadea R, Sevilla MJ, Ronda E. Validation of a questionnaire to identify damage and exposure to ergonomic risks at work. Rev Esp Salud Pública. 2011;85:331–340.
Tschentscher M, Niederseer D, Niebauer J. Health benefits of Nordic walking: a systematic review. Am J Prev Med. 2013;44(1):76–84.
Zeller JM, Levin PF. Mindfulness interventions to reduce stress among nursing personnel: an occupational health perspective. Workplace Health Saf. 2013;61(2):85–89.
World Health Organization (WHO). Diet, nutrition and the prevention of chronic diseases: report of a Joint WHO/FAO Expert Consultation WHO Technical Report Series. Geneva. 2003;916.
Hill JC, Whitehurst DG, Lewis M, Bryan S, Dunn KM, Foster NE, Konstantinou K, Main CJ, Mason E, Somerville S, Sowden G, Vohora K, Hay EM. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomized controlled trial. Lancet. 2011;378:1560–1571.
Sánchez-López P, Dresch V. The 12-item general health questionnaire (GHQ-12): reliability, external validity and factor structure in the Spanish population. Psicothema. 2008;20(4):839–843.
Williams A. In: Kind P, Brooks R, Rabin R, editors. EQ-5D concepts and methods. Dordrecht: Springer; 2005. p. 1–17.
Schwarzer R, Jerusalem M. Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in health psychology: a user’s portfolio. Causal and control beliefs. Windsor: NFER-NELSON; 1995. p. 35–37.
Bayliss EA, Ellis JL, Steiner JF. Seniors’ self-reported multimorbidity captured biopsychosocial factors not incorporated into two other data-based morbidity measures. J Clin Epidemiol. 2009;62(5):550–557.
Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52–2:157–168.
Corral J, Espinàs JA, Cots F, Pareja L, Solà J, Font R, Borràs JM. Estimation of lung cancer diagnosis and treatment costs based on a patient-level analysis in Catalonia (Spain). BMC Health Serv Res. 2015;15:70.
Department of Health. Shared clinical history in Catalonia (HC3). [Internet]. 2021 [cited 25 May 2023]. Available in: https://salutweb.gencat.cat/ca/ambits_actuacio/linies_dactuacio/tic/sistemes-informacio/gestio-assistencial/hc3/index.html
Official Gazette of the Generalitat of Catalonia (DOGC). Provisions. Health Department. [Internet] 2022. Núm. 8816 - 20.12.2022 [cited 11 Nov 2023]. Available in: https://portaldogc.gencat.cat/utilsEADOP/PDF/8816/1943112.pdf
Spanish Agency for Medicines and Health Products (AEMPS). Use of nonsteroidal anti-inflammatory drugs (NSAIDs) in Spain during the period 2000–2012. Medication utilization report U/AIN/V1/15012014. [Internet] 2014. [cited 25 May 2023]. Available in: https://www.aemps.gob.es/medicamentosUsoHumano/observatorio/docs/AINE.pdf
Catalan Institute of Health. Remuneration book 2022. ICS statutory staff. [Internet] 2022. [Cited 09 May 2024]. Available in: https://ics.gencat.cat/web/.content/Documents/transparencia/personal/Llibre-de-retribucions-gener-2023.pdf
Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sorensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–237.
Herdman M, Badia X, Berra S. EuroQol-5D: a simple alternative for measuring health-related quality of life in primary care. AtenPrimaria. 2001;28:425–430.
Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry. 2005;187(2):106–108.
Fenwick E, Marshall DA, Levy AR, Nichol G. Using and interpreting cost-effectiveness acceptability curves: an example using data from a trial of management strategies for atrial fibrillation. BMC Health Serv Res. 2006;6:52.
Williams K and Thompson C. Patient-reported outcome measures: stakeholder interviews. Sydney: ACSQHC; 2018. [cited 25 May 2023]. Available in: https://www.safetyandquality.gov.au/sites/default/files/migrated/PROMs-stakeholder-interviews-report-2018.pdf
Suni JH, Kolu P, Tokola K, Raitanen J, Rinne M, Taulaniemi A, Parkkari J, Kankaanpää M. Effectiveness and cost-effectiveness of neuromuscular exercise and back care counseling in female healthcare workers with recurrent non-specific low back pain: a blinded four-arm randomized controlled trial. BMC Public Health. 2018;18(1):1376.
Tingulstad A, Maas ET, Rysstad T, Øiestad BE, Aanesen F, Pripp AH, Van Tulder MW, Grotle M. Six-month cost-effectiveness of adding motivational interviewing or a stratified vocational advice intervention to usual case management for workers with musculoskeletal disorders: the MI-NAV economic evaluation. J Occup Med Toxicol. 2023;18(1):25.
Steenstra IA, Anema JR, van Tulder MW, Bongers PM, de Vet HC, van Mechelen W. Economic evaluation of a multi-stage return to work program for workers on sick-leave due to low back pain. J Occup Rehabil. 2006;16(4):557–578.
Lindholdt L, Labriola M, Nielsen CV, Horsbøl TA, Lund T. Sequence analysis to assess labour market participation following vocational rehabilitation: an observational study among patients sick-listed with low back pain from a randomised clinical trial in Denmark. BMJ Open. 2017;7(7): e015661.
Miyamoto GC, Lin CC, Cabral CMN, van Dongen JM, van Tulder MW. Cost-effectiveness of exercise therapy in the treatment of non-specific neck pain and low back pain: a systematic review with meta-analysis. Br J Sports Med. 2019;53(3):172–181.
Acknowledgements
We want to thank all healthcare workers and their representatives, referents, managers, and supervisors from the hospital clusters of Hospital del Mar (HMAR) and Corporació Sanitaria Parc Taulí (CSPT) who agreed to participate in the trial. Especially, HMAR: Pilar Pastor (Ward manager), Isabel Aranega, Noemí Cajete, Raúl Martín, Dolores Rincón, Nuria Saavedra (UH30); Rosa Balaguer (ward manager), Sonia Advíncula, Nuria Esteban, Montse Regordosa, Cristina Salvat, Ana Uribe (Intensive Care Unit); Isabel Egea (ward manager), Ana Delgado, M Ángeles Fernández, Josefa García, Susana Margalef, Alexandra Morales, Ana M Rodríguez, Isabel Rodríguez (Llevants 3,4); Montse Sitges, Txell Gumà (ward managers), Rosa Elias, Lucía Fernández, Ana M Luque, Nuria Morillas, Carlos Perez, Sandra Vives (Surgical area); Elena Maull, Desirée Ruiz (ward manager), Alberto Gonzalez, Antonia Rincón, Bernat Sarrió, Gina Shakya (UH04); Beatriz Fernández (ward manager), Mª Encarnación Avilés, Miriam Hernández, Naza Martinez, Carme Pellín, Nenita de los Santos, Sergio Taibo, Chari Villanueva (Acute geriatrics unit). Rosa Aceña, Cuca Esperanza and Núria Pujolar (Nursing Coordinators); Mercedes Calvo, Miguel Celada, Lluisa Cosp, Eugenio Gurrea, Montse Sallés, Pilar Serrano (Nurse Supervisors); and Vicky Abad, Pilar González, Francisco Martos (Prevention Delegates). CSPT: Isabel Simó (ward manager), Mª Goretti Gelonch, Elisabeth Mérida, Sara Purcalla, Mónica Sianes (UH06); José Mª Barradas (ward manager), Judith Camps, M José González, Verònica Gómez, Victoria Plaza, Estefanía del Pino (UH08); and Elena Polo (Prevention Delegate). We also want to thank the contribution of Rocío Villar (occupational physician, HMAR); Cristina Cervantes, Ferran Escalada and the physiotherapists team (Rehabilitation Service, HMAR); Fernanda Caballero and physiotherapists team (Rehabilitation Service, CSPT); Gemma Salvador (Agència de Salut Pública de Catalunya) and Ada Parellada (Chef); Montserrat Fernandez (CiSAL, UPF); Cristina Giménez (Psychologist); Antonio Brieba (Nordic walking instructor); Georgina Badosa and Mónica Astals (Mindfulness instructors).
Funding
The study is funded by the Instituto de Salud Carlos III-FEDER (reference number PI14/01959, PI17/00779 and PI20/00101). The funders had no role in the study design, data collection, analysis, decision to publish, or preparation of the manuscript. Ignacio Aznar-Lou had a Miguel Servet research contract (CP22/00029) during the analysis and manuscript preparation.
Author information
Authors and Affiliations
Contributions
CS, PP, and JMR contributed to the study conception. MSF, CS, PP, and JMR performed material preparation and data collection. MSF, IAL, and JA performed analysis. MSF wrote the first draft of the manuscript and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors Mercè Soler-Font, Ignacio Aznar-Lou, Josué Almansa, Pilar Peña, Michael Silva-Peñaherrera, Consol Serra, and José Maria Ramada declare that they have no conflict of interest.
Ethical Approval
The Clinical Research Ethical Committee of Parc de Salut Mar approved the study (reference number: 2014/5714/1), and the study was retrospectively registered to ISRCTN (ISRCTN15780649).
Informed Consent
Written informed consent was obtained from all individual participants included in the study.
Consent to Participate
Written informed consent was obtained from all individual participants included in the study.
Consent to Publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Soler-Font, M., Aznar-Lou, I., Almansa, J. et al. Cost-Effectiveness of a Multi-faceted Workplace Intervention to Reduce Musculoskeletal Pain in Nursing Staff: A Cluster-Randomized Controlled Trial (INTEVAL_Spain). J Occup Rehabil (2024). https://doi.org/10.1007/s10926-024-10227-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s10926-024-10227-6