Abstract
Background
Both post-COVID-19 condition (long COVID) and the presence of persisting symptoms that do not meet formal definitions of post-COVID-19-condition may adversely affect quality of life and function. However, their prevalence among children and young people in England is unclear.
Methods
We used data from repeated surveys in a large cohort of English schoolchildren from the COVID-19 Schools Infection Survey (SIS) for the school year 2021/22 to describe the weighted prevalence of post-COVID-19-condition and compare persisting symptoms between individuals with a positive SARS-CoV-2 test and those with neither a positive test history nor suspected infection.
Results
Among 7797 children from 173 schools, 1.8% of primary school pupils (aged 4 to 11 years), 4.5% of secondary school pupils in years 7–11 (aged 11 to 16 years) and 6.9% of those in years 12–13 (aged 16 to 18 years) met a definition of post-COVID-19 condition in March 2022. Specific persisting symptoms such as anxiety or difficulty concentrating were frequently reported regardless of prior infection status and increased with age: 48.0% of primary school pupils, 52.9% of secondary school pupils in years 7–11 and 79.5% in years 12–13 reporting at least one symptom lasting more than 12 weeks. Persisting loss of smell and taste, cardiovascular and some systemic symptoms were more frequently reported by those with a previous positive test.
Conclusions
We showed that ongoing symptoms were frequently reported by English schoolchildren regardless of SARS-CoV-2 test results and some specific symptoms such as loss of smell and taste were more prevalent in those with a positive test history. Our study emphasises the wide-ranging impacts of the COVID-19 pandemic on the health and wellbeing of children and young people.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
While COVID-19, the clinical disease associated with acute SARS-CoV-2 infection, is usually of short duration and low symptom burden in children and young people (CYP) [1], persisting physical and psychological symptoms are frequently reported after infection [2]. Post COVID-19 condition (long COVID) among CYP has been defined through a modified DELPHI process as ‘a history of confirmed SARS-CoV-2 infection, with at least one persisting physical symptom for a minimum duration of 12 weeks after initial testing that cannot be explained by an alternative diagnosis. The symptoms have an impact on everyday functioning, may continue or develop after … infection, and may fluctuate or relapse over time’ [3]. While more detailed, this research definition of long COVID is in accordance with clinical case definitions developed by the National Institute for Health and Care Excellence [4].
During the COVID-19 pandemic, however, many CYP who have tested negative for SARS-CoV-2 also report persisting symptoms such as fatigue as well as feelings of worry or unhappiness [5]. This may partly reflect disruptions to schools and social connectedness during the pandemic [6]. Comparing the prevalence of persisting symptoms among CYP with and without confirmed or probable COVID-19 across studies is challenging due to varying case definitions, study designs, lengths of follow up and symptom groupings [7]. Nevertheless, understanding the burden of persisting symptoms in these groups is essential to guide strategies to mitigate the impact of COVID-19 on CYP.
Here we aimed to (i) describe the prevalence of post-COVID-19 condition (long COVID) [3] and (ii) describe the prevalence and distribution of persisting specific symptoms [8] among CYP reporting a previous positive SARS-CoV-2 test compared to those with neither a positive test nor previous suspected infection using data from a representative sample of English schools collected through the COVID-19 Schools Infection Survey.
Methods
We used data from the COVID-19 Schools Infection Survey (SIS) for the school year 2021/22. The original Schools Infection Survey was set up in the school year 2020/21 to monitor the prevalence of SARS-CoV-2 in schools in England and to investigate risk and protective factors for transmission [9]. In 2021/2, the scope broadened to include a focus on physical and mental health during the pandemic. Our study collected health information through three survey rounds (round one: Nov-Dec 2021; round two: Jan-Feb 2022 and round three: Mar-Apr 2022) in a nationally representative cohort of pupils from a stratified random sample of primary and secondary schools in 42 local authorities (LAs) in England. Sampling procedures are described elsewhere [10]. In brief, we planned to enrol 13 primary and 7 secondary schools in each of England’s nine geographic regions from October 2021 aiming to reach a target of 180 schools. This target was reached through sample size calculations based on a primary outcome of antibody prevalence which are reported elsewhere [11]. All pupils aged 4 years and over were invited to participate.
Online consent forms and questionnaires were completed by parents/guardians for children in school years 0–11 (aged 4–16 years) and by pupils in school years 12–13 (aged 16–18 years). Other study procedures are described elsewhere [10]. For this study, data for pupils in school years 7–11 (aged 11–16 years) were taken from parent questionnaires only. Questionnaires captured self-reported information on household composition, socio-demographics, medical and symptom history, SARS-CoV-2 test results, social contacts and mental wellbeing [10]. History of confirmed SARS-CoV-2 infection was defined as self-reporting a positive result on either PCR or lateral flow testing since March 2020. Suspected COVID-19 was based on a positive response to the question ‘Do you know or think that [child’s first name] has had coronavirus (COVID-19) since March 2020?’ We also collected data on the presence, features and impact of symptoms experienced in a persisting or recurring way for more than 12 weeks since March 2020. The wording of the questions used to generate outcome and comparator definitions is shown in the Supplementary methods.
Questionnaire responses were captured in round one (before Omicron) and in round three (during Omicron subvariant waves) when additional participants had been recruited. The dates for round one were 22nd November-15th December for parent questionnaires, with pupils in years 12–13 given five weeks to respond (11th November-15th December) to maximise uptake. For round three, questionnaire delivery was streamlined to a two-week period (15th March-1st April) for both parents and young people in years 12–13 for administrative reasons. Round two did not include questions on long COVID.
Using these data, we first described the weighted prevalence (%) of post-COVID-19-condition (long COVID) meeting a definition based on the DELPHI consensus [3]. This was reporting of a positive SARS-CoV-2 test, the presence of symptoms continuously for 12 weeks or more after the start of their infection, and everyday life being affected by those symptoms. Data were described by school type, age-group, sex, eligibility for free school meals (government-funded school meals for socio-economically disadvantaged children; self-reported at registration) and presence of underlying health conditions. Second, we described the weighted % of all CYP experiencing persisting symptoms lasting more than 12 weeks since March 2020 by age group. We explored persisting symptoms both individually and grouped according to an approach taken by the Patient-Led Research Collaborative [8]. For each symptom and grouping, we calculated differences between those reporting a previous positive SARS-CoV-2 test and those with neither a history of a positive test nor suspected COVID-19 for each age group, generating exact binomial 95% confidence intervals for difference in proportions [12].
Ethical approval was obtained from the UKHSA Research Support and Governance Office (R&D 474) and London School of Hygiene & Tropical Medicine Ethics Review Committee (ref:22,657).
Results
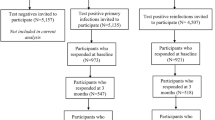
One hundred thirty-four schools participated in round one, with questionnaire data available from 3,375 parents for 4,128 children in school years 0–11 (aged 4–16 years) and from 143 pupils in years 12–13 (aged 16–18 years). In round three, there were 173 registered schools, with questionnaire data available from 6,197 parents for 7,448 children in years 0–11 and from 349 pupils in years 12–13.
In round one, 1% (0.5 to 1.6%) of 2,485 primary school pupils surveyed, 2.5% (1.4 to 4.2%) of 1,902 pupils in years 7–11 and 4.4% (1.1 to 11.6%) of 143 pupils in years 12–13 were reported to have experienced long COVID as a result of their most recent SARS-CoV-2 infection. In round three, the prevalence of long COVID was 1.8% (1.2 to 2.6%) among 3,788 primary school pupils, 4.5% (3.4 to 5.7%) among 2,617 pupils in years 7–11 and 6.9% (3.3 to 12.4%) for 349 pupils in years 12–13, respectively. No clear patterns were seen by gender, the presence of underlying health conditions or eligibility for free school meals, a measure of socio-economic deprivation (Table 1).
A history of symptoms persisting for more than 12 weeks was common regardless of infection history, with 48.0% (45.6 to 50.5%) of primary school pupils, 52.9% (50.5 to 55.3%) of secondary school pupils in years 7–11 and 79.5% (71.9 to 85.8%) of those in years 12–13 reporting at least one persisting symptom in round three. Similar results were reported in round one (Supplementary table 1). For primary school pupils, the most common persisting symptoms in both rounds were cough, sore throat, worry or anxiety and difficulty concentrating. In secondary schools in both rounds, worry or anxiety was the most frequently reported symptom, with low mood and difficulty concentrating both in the commonest four symptoms, as well as sore throat (years 7–11) and weakness or tiredness (years 12–13) (Supplementary table 1).
In round three, 2,027 secondary school pupils in years 7–11 reported a previous positive test, 216 had had suspected COVID while 1,415 had neither a history of a positive test nor suspected COVID-19 (weighted percentages 54.0%, 6.8% and 39.2% respectively). More secondary school-aged pupils reported at least one persisting symptom if they had had a positive SARS-CoV-2 test (55.4% (52.2 to 58.6%)) compared to those with neither a history of a positive test nor suspected COVID-19 (47.8% (43.9 to 51.6%)). However, among primary school pupils, of whom 2,130 reported a previous positive test, 319 had had suspected COVID-19 and 1,334 had no positive test or suspected COVID-19 (weighted percentages 53.0%, 8.9%, 38.1%), there were no differences in those reporting at least one persisting symptom by COVID-19 history (Fig. 1; Supplementary table 2).
Difference in weighted1 prevalence of grouped symptoms2 reported between individuals with a history of a positive test and those with neither a positive test nor suspected COVID-19 in rounds one* and three±, by age group (A: primary school years 0–6; B: secondary school years 7–11; C: secondary school years 12–13). 1 Estimates are weighted for sampling design, school-level response rate, school years, sex, ethnicity and free school meal eligibility (a measure of socio-economic deprivation). 2 Grouped symptoms comprised the following: cardiovascular (chest pain or tightness; palpitations), cognitive disturbance (feeling lightheaded or disorientated; feeling dizzy; trouble sleeping; headache; memory loss or confusion; difficulty concentrating), dermatologic (raised, red, itchy bumps on skin or swelling of face or lips; red or purple blisters on feet or toes; prickling, tingling or burning sensations in skin), gastrointestinal (diarrhoea; not feeling hungry or wanting to eat; feeing or being sick; stomach pain), HEENT (lost or husky voice; sore throat; sore or uncomfortable eyes; earache or ringing in ears), loss of smell or taste, mood (worry or anxiety; low mood or not enjoying anything), musculoskeletal (strong aches or pains in joints or muscles), pulmonary (cough; feeling short of breath), systemic (fever or high temperature; chills or shivers; weakness or tiredness). * In round one, 532 primary school pupils had a history of a positive test compared to 1,791 with no reported COVID. For years 7-11, 515 pupils reported a positive test history compared to 1,037 with no reported COVID. The corresponding figures for years 12-13 were 39 and 90. ± In round three, 2,130 primary school pupils had a history of a positive test compared to 1,334 with no reported COVID. The corresponding figures were 2,027 and 1,415 for pupils in years 7-11 and 161 and 159 for pupils in years 12-13. Note that in round one, figures for loss of smell and taste for primary school years 0-6 and secondary school years 12-13 were suppressed due to small numbers
For individual symptoms, the most striking difference was for loss of smell or taste, which was consistently reported more frequently by pupils with a positive test compared to those with neither a positive test nor suspected COVID-19 in all age groups in round three (3.1% versus 0.1% in years 0–6, 10.3% versus 1.5% in years 7–11, 18.4% versus 1.3% in years 12–13). Cardiovascular symptoms (chest pain or tightness, palpitations) were also more commonly reported among children in school years 0–11 with a positive test than those with neither a positive test nor suspected COVID-19: 4.8% v. 1.2% in primary school and 8.5% v. 4.5% for pupils in years 7–11. For those in years 7–11, systemic symptoms (fever, chills, weakness or tiredness) were more frequently reported among those with a positive test: 22.1% v. 14.4%. For years 12–13, while numbers were small, pulmonary symptoms and symptoms affecting the head, eyes, ears, nose and throat were also more prevalent among those with a positive test (Fig. 1; Supplementary table 2).
Discussion
In this large cohort of schoolchildren in England, the prevalence of post-COVID-19 condition (long COVID) in March 2022 was low, ranging from 1.8% in primary school pupils to 6.9% among those in school years 12–13. Specific persisting symptoms such as worry or anxiety and difficulty concentrating were frequently reported regardless of prior infection status and increased with age. Persisting loss of smell and taste along with cardiovascular and some systemic symptoms showed the most marked difference in prevalence by infection history.
The low prevalence of cases meeting a definition of post-COVID-19 condition (long COVID) based on the DELPHI consensus definition is compatible with estimates from other studies of community cases in CYP [13] and lower than estimates from studies of hospitalised cases [14]. Similarly, the high prevalence of reported specific persisting symptoms is also consistent with other studies. A systematic review and meta-analysis of 17 studies of children with confirmed or probable COVID-19 with a median follow up of 125 days, showed pooled prevalence estimates for persisting symptoms ranging from 15% (diarrhoea) to 47% (fatigue) [2]. As in our study, others have shown relatively small differences in symptom reporting when comparing infected and uninfected groups: among 6 studies comparing persisting symptoms between children with and without a history of COVID-19, the difference in the proportion reporting persisting specific symptoms varied from -0.5% to 13.2% between groups (median difference 3.0%, IQR 1.4 to 3.6%) [7]. Nevertheless, these differences may increase with age: as in our study, a Danish community-based study of adolescents aged 15 to 18 years showed that those with a positive test history were more likely to report at least one persisting symptom than a matched control group [15].
These results highlight the high proportion of CYP reporting persisting symptoms during the pandemic, despite not meeting definitions of post-COVID-19 condition (long COVID). Repeated representative longitudinal surveys conducted in the UK also show that rates of probable mental disorders among CYP have increased steeply from 2017 to 2020–21 [16]. Reasons for this, including any impacts of the seasonality of survey administration on symptom reporting, are unclear. However, COVID-19 mitigation measures to reduce risk of infection by limiting physical access to schools, childcare, social activities, as well as health and social care services may have contributed to negative outcomes for the health and wellbeing of CYP. Measures to support the mental health and wellbeing of CYP regardless of prior infection status, including recognising the importance of school and family connectedness [6], should be a priority.
Strengths of our study include its large size, broad geographic representation across England and the use of repeated measures of persisting symptoms over time among CYP with and without a reported history of COVID-19. Nevertheless, the self-reported nature of symptoms lasting for more than 12 weeks and proxy reporting used for younger children may have led to some misclassification of persisting symptoms. In addition, the time period between initial infection and survey completion was variable with a maximum gap of two years for any child infected in March 2020 completing surveys in round three, which could lead to symptom misclassification. The limited data on timing of initial infection did not allow us to assess the impact of any time lag on symptom reporting. We also did not have data on repeated infections or information about whether an infection led to hospitalisation, which might have affected reporting of persisting symptoms. This could be an area for future research.
Our comparison group of those with neither a history of positive test nor suspected infection might include pupils infected but not diagnosed before the introduction of mass community testing around June 2020, though we tried to minimise the bias by excluding those with suspected (likely symptomatic) infection. We also cannot exclude selection bias among those who both agree to participate and chose to complete questionnaires. Another limitation is that the study only covers state-funded primary and secondary schools and excludes others such as independent and special schools, although it is estimated that 93% of pupils attend state funded schools [17]. Finally, numbers for some stratified analyses, particularly in the oldest age group were small.
Conclusions
The increasing, albeit low, prevalence of post-COVID-19-condition (long COVID) among CYP and the high proportion reporting persisting symptoms regardless of COVID-19 test results, emphasise the wide-ranging impacts that the COVID-19 pandemic has had on CYP. Further work is needed to understand how persisting symptoms affect educational outcomes and quality of life longer-term. Emerging from the pandemic, child health and wellbeing must be prioritised to avoid embedding long-term disadvantage for a generation of CYP.
Availability of data and materials
The datasets supporting the conclusions of this article are available on the Office for National Statistics website at the following URLs: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/datasets/covid19schoolsinfectionsurveyquestionnairedataengland and https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/adhocs/14808covid19schoolsinfectionsurveyenglandsymptomprevalencebycovid19statusnovembertodecember2021
References
Molteni E, Sudre CH, Canas LS, Bhopal SS, Hughes RC, Antonelli M, et al. Illness duration and symptom profile in symptomatic UK school-aged children tested for SARS-CoV-2. Lancet Child Adolesc Health. 2021;5(10):708–18.
Behnood SA, Shafran R, Bennett SD, Zhang AXD, O’Mahoney LL, Stephenson TJ, et al. Persistent symptoms following SARS-CoV-2 infection amongst children and young people: A meta-analysis of controlled and uncontrolled studies. J Infect. 2022;84(2):158–70.
Stephenson T, Allin B, Nugawela MD, Rojas N, Dalrymple E, Pereira SP, et al. Long COVID (post-COVID-19 condition) in children: a modified Delphi process. Arch Dis Child. 2022;107(7):674–80.
National Institute for Health and Care Excellence. COVID-19 rapid guideline: managing the long-term effects of COVID-19. 2022 Jan [cited 2022 Sep 9]. Report No.: 188. Available from: https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-effects-of-covid19-pdf-51035515742
Stephenson T, Pinto Pereira SM, Shafran R, de Stavola BL, Rojas N, McOwat K, et al. Physical and mental health 3 months after SARS-CoV-2 infection (long COVID) among adolescents in England (CLoCk): a national matched cohort study. Lancet Child Adolesc Health. 2022;6(4):230–9.
Hertz MF, Kilmer G, Verlenden J, Liddon N, Rasberry CN, Barrios LC, et al. Adolescent Mental Health, Connectedness, and Mode of School Instruction During COVID-19. J Adolesc Health Off Publ Soc Adolesc Med. 2022;70(1):57–63.
Zimmermann P, Pittet LF, Curtis N. The Challenge of Studying Long COVID: An Updated Review. Pediatr Infect Dis J. 2022;41(5):424–6.
Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re’em Y, et al. Characterizing long COVID in an international cohort: months of symptoms and their impact. eClinicalMedicine. 2021;38:101019.
Halliday KE, Nguipdop-Djomo P, Oswald WE, Sturgess J, Allen E, Sundaram N, et al. The COVID-19 Schools Infection Survey in England: protocol and participation profile for a prospective observational cohort study. JMIR Res Protoc. 2022;11(11): e34075.
Office for National Statistics. COVID-19 Schools Infection Survey, 2021 to 2022: methods and further information. 2022. Last accessed 06/10/2022. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/methodologies/covid19schoolsinfectionsurvey2021to2022methodsandfurtherinformation
Powell AA, Ireland G, Leeson R, Lacey A, Ford B, Poh J, Ijaz S, et al. National and regional prevalence of SARS-CoV-2 antibodies in primary and secondary school children in England: the School Infection Survey, a national open cohort study, November 2021. J Infect. 2023;S0163–4453(23):00085–93.
Armitage P, Berry G, Matthews J. Statistical methods in medical research. 4th ed. Oxford: Blackwell Science; 2002.
Radtke T, Ulyte A, Puhan MA, Kriemler S. Long-term Symptoms After SARS-CoV-2 Infection in Children and Adolescents. JAMA. 2021;326(9):869–71.
Bergia M, Sanchez-Marcos E, Gonzalez-Haba B, Hernaiz AI, de Ceano-Vivas M, GarcíaLópez-Hortelano M, et al. Comparative study shows that 1 in 7 Spanish children with COVID-19 symptoms were still experiencing issues after 12 weeks. Acta Paediatr. 2022;111(8):1573–82.
Kikkenborg Berg S, Dam Nielsen S, Nygaard U, Bundgaard H, Palm P, Rotvig C, et al. Long COVID symptoms in SARS-CoV-2-positive adolescents and matched controls (LongCOVIDKidsDK): a national, cross-sectional study. Lancet Child Adolesc Health. 2022;6(4):240–8.
Lifestyle Team, NHS Digital. Mental Health of Children and Young People in England 2021 - wave 2 follow up to the 2017 survey [Internet]. 2021 Sep [cited 2022 Jun 10]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2021-follow-up-to-the-2017-survey
Department for Education. Schools, pupils and their characteristics: academic year 2021/22. 2022 June [cited 2022 Oct 19]. Available from: https://explore-education-statistics.service.gov.uk/find-statistics/school-pupils-and-their-characteristics
Acknowledgements
We would like to thank the schools, head teachers, staff, families and children who took part in the SIS study. Members of the COVID-19 Schools Infection Survey 2 Study Group are Elliot McClenahan; Gillian McKay; Jody Phelan; Liang-Yu Lin; Alex Lewin (all from LSHTM) and Alison Judd; Byron Davies; Anisah Saib; James McCrae; Joe Kelly; Ian Diamond; Emma Rourke; Fiona Dawe; Pete Jones (all from ONS).
Funding
This work was funded by the UK Department of Health and Social Care. CWG is supported by a Wellcome Career Development Award (225868/Z/22/Z).
Author information
Authors and Affiliations
Consortia
Contributions
CWG, AL, SC, DS, ST, FL, BF, GI, SNL, TS, PND and PM contributed to study design. AL, DS, ST, FL, BF and CWG analysed data. CWG drafted the manuscript. All authors critically revised the manuscript for important intellectual content and approved the final version for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the UKHSA Research Support and Governance Office (R&D 474) and London School of Hygiene & Tropical Medicine Ethics Review Committee (ref:22657). Informed consent was obtained from parents of children in school years 0–11 and from children in school years 12 to 13. The study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Warren-Gash, C., Lacey, A., Cook, S. et al. Post-COVID-19 condition and persisting symptoms in English schoolchildren: repeated surveys to March 2022. BMC Infect Dis 23, 201 (2023). https://doi.org/10.1186/s12879-023-08203-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08203-1