Abstract
Background
In literature, the levels of miRNA-146a and miRNA-155 are increased in periodontitis. Limited data are available regarding the expression of miRNA-146a and miR-NA-155 in diseased human peri-implant tissue. Therefore, the objective of this study was to explore the expression of miRNA-146a and miRNA-155 in human gingival peri-implant tissue affected by peri-implantitis.
Methods
After recording the clinical parameters, human peri-implant pocket tissues were harvested from sites diagnosed with peri-implantitis (n = 15 cases) in addition to healthy peri-implant sulcus tissues (n = 15 controls). The levels of miRNA-146a and miRNA-155 were assessed using real-time qPCR.
Results
Cases exhibited a significantly higher mean expression of miRNA-155 (5.2-fold increase) and miRNA-146a (2.8-fold increase) than controls. MiRNA-155 and miRNA-146a demonstrated an appropriate sensitivity (87.5% and 87.5%, respectively) and specificity (73.3% and 66.7%, respectively) in discriminating cases from controls. A moderate correlation (r = 0.544, p = 0.029) was found between miRNA-155 and miRNA-146a levels in the case group.
Conclusions
The expressions of miRNA-146a and miR-NA-155 are different between healthy and peri-implantitis affected tissues. Both miRNAs might potentially able to discriminate healthy from peri-implantitis affected tissues.
Similar content being viewed by others
Background
Peri-implantitis is a biofilm-induced inflammation of the oral mucosa surrounding dental implants. Clinically, it is characterized by increased peri-implant pocketing, bleeding gingiva, and loss of alveolar bone [1, 2]. Peri-implantitis is a widespread disease worldwide; its prevalence is 19.53% at the patient level and 12.53% at the implant level [3]. Treatment of peri-implantitis mostly needs surgical intervention [4]. Unfortunately, the success of peri-implantitis therapy is uncertain, particularly in cases with severe bone loss [5,6,7]. Therefore, early detection of pathological peri-implant bone resorption is of great importance. Nowadays, the role of biomarkers for early identification and accurate prediction of peri-implant diseases is getting much attention [8,9,10].
In peri-implant diseases, local inflammatory responses are generated and maintained in the peri-implant tissue by the interactions of cytokines and chemokines secreted from activated lymphocytes, macrophages, and neutrophils [11,12,13]. Peri-implant bone loss is the consequence of prolonged local inflammation that leads to pathological bone remodeling and, consequently to implant failure [14]. Earlier studies have shown that miRNAs (miRNAs) play a critical role in numerous inflammatory diseases [15, 16] such as periodontitis [17,18,19]. Abnormal expression of these molecules leads to various systemic and oral disease [20,21,22,23]. MiRNAs are small (18–22 base pairs) non-coding RNA molecules [24, 25]. They participate in regulating gene expression [26]. MiRNAs induce degradation or suppression of the targeted messenger RNA molecule after binding to its complementary sequence of the 3-UTR (untranslated coding region) [27,28,29,30]. Among miRNAs, miRNA-146a and miRNA-155 have been reported to be stimulated by Toll-like receptors (TLRs) and proinflammatory cytokines and have a regulatory role in immune reactions [31, 32].
The expression of both miRNA-146a and miRNA-155 have been extensively investigated in periodontitis patients. As compared to subjects with healthy periodontium, periodontitis patients have been reported to show higher expression of miRNA-146a [18, 33, 34]. This finding is further supported by a recent meta-analysis which also has suggested that miRNA-146a might have a potential role in discriminating periodontal health from disease [35]. At the same time, miRNA-155 shows a similar trend as it has been demonstrated to be upregulated in periodontitis compared to periodontal health [29, 33]. However, a contrary finding (downregulation of miRNA-155) has also been reported in periodontitis [34]. This suggests that many miRNAs might demonstrate a dual regulation effect. Such behavior could be explained by the ability of a single miRNA to impact and control many genes [36]. Therefore, more research is needed to determine the significance of this dual regulation effects of miRNAs in the regression and progression of diseases. On the other hand, no data are available about the expression of both above-mentioned miRNAs in peri-implantitis. Only one animal study that have revealed a considerable increase in expression of miRNA-146 [14]. Despite similarities between periodontitis and peri-implantitis conditions with respect to etiology and pathogenesis, more pronounced inflammatory responses are encountered to bacterial challenges in peri-implant tissue [37, 38]. There are distinct molecular and histopathological characteristics of peri-implantitis compared to periodontitis, despite some similarities between the two conditions [39]. Therefore, this study aimed to explore the expression level of miRNA-146a and miRNA-155 in human gingival tissue surrounding dental implants diagnosed with peri-implantitis and health.
Materials and methods
Study design
This case-control study was carried out between July 2022 and August 2023. The peri-implant tissue samples were collected from patients attending several private clinics in Baghdad. The study protocol was earlier approved by the ethical committee of the College of Dentistry / University of Baghdad in April 2022 (project No.#534,622). All selected patients signed informed consents which were collected by the study examiner.
Sample size
In this study, the sample size was calculated after conducting a pilot study involving 6 tissue samples; three diseased and three healthy tissue samples. After processing the tissue samples, the estimated mean fold changes of miRNA-155 (primary outcome) were 0.15 ± 0.11 and 0.45 ± 0.44 in healthy and diseased tissues, respectively; the estimated effect size was 0.935. Accordingly, it was found that, at least, a total size of 30 tissue samples (15 for each group) was enough to reject the null hypothesis at a power of 80% and 0.05 probability. G*power 3.1 software was used to calculate the sample size.
Inclusion and exclusion criteria
Tissue samples were collected from patients who were seeking to replace missing teeth with dental implants (control group) and patients already having dental implants diagnosed with peri-implantitis (case group). To include patients in this study, they should be systemically healthy adult (> 18 years). The selection of patients in the control group was based on the adequacy of their bone quality and quantity for implant placement. A minimum of 8.5–13 mm bone length and 4.5–5 mm bone width were the thresholds for selecting patients in this group. In addition, the selected patients should have a minimum 3 mm width of keratinized mucosa. While for case group, patients should have at least one implant with more than one year in function diagnosed with peri-implantitis. The considered implants should have bleeding and/or suppuration on gentle probing, increased probing pocket depth (PPD) compared to previous baseline data and bone loss beyond initial bone remodeling levels. In the absence of previous examination data, the included diagnosed implants should exhibit bleeding and/or suppuration on gentle probing, PPD of ≥ 6 mm and bone levels ≥ 3 mm apical to the most coronal portion of the intraosseous part of the implant [1]. The exclusion criteria included positive history of periodontitis, active infectious diseases, cardio-vascular diseases, type I or type II diabetes and receiving local or systemic anti-inflammatory/antimicrobial treatment 3 months before starting the study.
Clinical examination
The eligible patients were clinically examined to detect any signs of mucosal inflammation, such as redness or edema, and measure PPD and bleeding on probing (BOP) sites followed by digital radiographic imaging to verify the presence of osseous resorption. All clinical parameters were measured by a University of North Carolina-15 (UNC) periodontal probe.
For each site, the periodontal probe was inserted gently into the pockets until feeling resistance then removed. After 15 s, the presence or absence of BOP in the sites were recorded as 1 or 0 respectively [40]. The presence of suppuration in the peri-implant sites was detected through palpation by fingers of oral and facial peri-implant tissues. The presence or absence of suppuration was recorded as 1 or 0 respectively [40]. PPD was measured by periodontal probe as the distance between the margin and bottom of the peri-implant pocket [41].
The bone loss was determined by measuring the length from the bone margin to the platform of the implant on periapical digital x-ray using the true length of the implant fixture as a reference. The x-rays were processed with dental x-ray software to make linear measurements. The actual size of the bone defect at the implant site was obtained by adjusting the implant relative size as following: Linear distance in mm equals (true implant size * mesial or distal length at x-ray / implant size in x-ray). The mesial or distal surface true values were obtained [42]. The width of keratinized gingiva was assessed as previously reported [43]. While, the gingival thickness was assessed using an endodontic reamer (#15) with a rubber stopper. First, the site was anesthetized, and then the reamer was inserted 2 mm apical to the gingival margin at mid-buccal sites. The stopper was adjusted to mark the depth of insertion, and the length of the reamer from the tip to the stopper was measured by a digital caliper [44].
Tissue sampling
All patients in control group had received dental implants (Medentika, Germany). The surgical implant placement was done by one experienced surgeon (M.P) for all patients. Amoxicillin (2 g/day, GlaxoSmithKline, UK) was prescribed for patients for 6 days. Sutures were removed after a period of 7–10 days [45].
After 12 ± 4 weeks healing period, the dental implants were surgically exposed by the same surgeon to replace cover screws by narrow healing abutments. All patients received oral hygiene instructions for full mouth-mouth cleaning including brushing and interdental cleaning twice daily. Subsequently, after one month of healing period, patients came again to clinic in order to collect healthy tissue samples. The peri-implant tissue was examined to confirm the lack of bleeding with gentle probing and the absence of redness to avoid any confusion with mucositis. The clinical parameters were recorded before peri-implant tissue harvesting. In this visit, a circular incision, after giving local anesthesia, was made by the same surgeon using a scalpel blade (15 C, Aesculap AG) or tissue punch. By using tissue forceps and scalpel 1.5 mm of peri-implant gingival tissue was obtained around each abutment. Then, a larger diameter healing abutment was screwed into the implant as shown in Figure S1 [45,46,47]. Patients were re-instructed about oral hygiene measures at this visit.
For patients in the case group, diseased peri-implant tissue samples were harvested as a part of their surgical treatment after recording the clinical parameters. After anesthetizing the area, two parallel incisions, 3 mm apart, were made through the soft tissue (peri-implant pocket sites) using a micro-scalpel blade (MEDESY CO, Italy) until reaching bone at proximal side of the dental implant. The two incisions were joined by a perpendicular incision 4 mm from the implant proximal area. Then specimens, which included the entire supra-crystal soft tissue part of the affected location, were carefully detached using tissue forceps and scalpel (MEDESY CO, Italy) [46, 47].
All tissue samples were rinsed with normal saline, preserved in a 2 ml tube containing DNA/RNA Shield (Zymo Research Europe, Freiberg, Germany) to avoid tissue degradation (preserving DNA/RNA intact). These tubes were immediately saved in a transfer cooling box (at 4 °C) for one hour and then saved at -20 °C in a refrigerator until RNA extraction (after 6 months).
Total RNA extraction and quality control
The saved frozen tubes containing tissue samples were left for 5 min at room temperature, vortexed, and then centrifuged at maximum speed for two minutes. The tissue was accumulated as a pellet at the bottom of the tube after aspirating the shield solution (supernatant layer). For homogenizing the tissue and isolation of total RNA, QIAzol™ Reagent kit was used according to manufactural instructions with the aid of 1.0 mm fused silica beads (BioSpec, USA) as shown in Figure S2.
The total RNA quality and quantity of the homogenized tissue samples was assessed using a spectrophotometer (Nabi-UV/VIS Nano Spectrophotometer Micro-Digital Co., Ltd., Seoul, Korea) [48].
RNA reverse transcription and quantification of miRNAs
The total RNA was converted to complementary DNA (cDNA) using miRNA-specific stem-loop primers (GoScript Reverse Transcription System, Promega, USA) according to the manufacturer instructions. The used primers are listed in Table 1. Quantus-Fluorometer (Promega, USA) was used to estimate the concentration of extracted cDNA. The levels of miRNA-155 and miRNA-146a gene were quantified using GoTaq® qPCR Master Mix (Promega, USA) kits based on the manufacturer instructions by real-time polymerase chain reaction (qPCR) device (Mic-PCR-Cycler, Bio-Molecular, Australia). Briefly, the Real-Time qPCR was started with an initial denaturation step at 95 °C for 5 min, followed by 40 cycles of denaturation at 95 °C for 15 s, annealing at 55 °C for 15 s, and extension at 72 °C for 15 s. The program ends with a final hold step at 4 °C for 10 min. The fluorescence signals were acquired during the annealing step to detect the amplification of the gene.
The 2−∆∆CT method was used to estimate the relative expression of miRNAs [49] as following:
ΔCT = CT gene - CT Housekeeping gene.
ΔΔCT = ΔCT Treated or Control – Average ΔCT Control.
Fold change = 2-ΔΔCT.
Statistical analysis
The data showed in Table S1 were analyzed using SPSS software (V.26; Chicago, IL, USA). The SPSS output draft is shown in Table S2. The normal distribution of numeric variables was detected by exploring their skewness. Each variable showed skewness < -1 or > 1 was considered as non-normally distributed. Mann Whitney U test was used to compare between non-normally distributed variables. On the other hand, Student t-test was used to detect any difference between normally distributed variables. The receiver operator curve [46] was used for checking the reliability criteria and the cutoff values of miRNAs (miR155 and miR146a) in detecting diseased tissue. The considered level of alpha for significance was < 0.05.
Results
Peri-implant tissue samples were harvested from 16 (44.8 ± 11.1 years) and 15 (49.1 ± 9.7 years) volunteers in the case and control groups respectively as shown in Fig. 1. The sex distribution was not statistically different between the groups (p = 0.095). Means of PPD and gingival width were significantly higher in case than control groups (p < 0.001 and p = 0.004, respectively). While no difference was detected in mean gingival thickness between the groups (see Table 2). Means of BOP and bone loss as well as suppuration frequency in the case group are shown in Table 2.
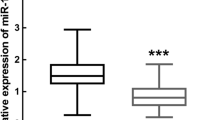
In this study, a significantly (p < 0.05) higher fold change of miRNA-155 (12.5 ± 14.2) was detected in tissue of cases than control group (2.4 ± 3.4). It was estimated that the average fold change of miRNA-155 in case group was 5.2 times higher than controls. Similarly, the fold change of miRNA-146a was found to be significantly (p < 0.05) higher in case group (8.6 ± 11.5) than control group (3.0 ± 4.3). Approximately, the fold change of miRNA-146a in case group was 2.8 times higher than control group as shown in Table 3.
The cut off value of fold change of miRNA-155 to differentiate between healthy and diseased tissues was 2.382 (0.829 area under curve, 87.5% sensitivity and 73.3% specificity). For miRNA-146a, the cut off value of fold change was 1.438 (0.742 area under curve, 87.5% sensitivity and 73.3% specificity) as shown in Fig. 2; Table 4.
In the case group, the mean level of miRNA-155 was found to be moderately associated with miRNA-146a level (r = 0.544, p = 0.029). While, no associations between the miRNAs and other study variables were detected as shown in Table 5.
Discussion
To date, this is the first study which assessed the levels of miRNA-155 and miRNA-146a genes in human diseased-tissue of patients with peri-implantitis. In fact, miRNAs have a regulatory role during the process of inflammation. They degrade or suppress messenger RNA molecules, and influence gene expression. Hence, they play a crucial role in several biological and physiological processes such as cell proliferation, growth, differentiation, and apoptosis [50, 51]. There is increasing evidence that dysregulation of miRNAs could contribute to various human diseases such as cancers, cardiovascular disease, chronic hepatitis, and diabetes [52,53,54,55]. As peri-implantitis is a bacterial induced inflammatory condition [1], therefore it was expected that the levels of both miRNA-155 and miRNA-146a in diseased tissue would be different compared to healthy peri-implant tissue.
In this study, the levels of both miRNA-155 and miRNA-146a were found to be increased in peri-implantitis affected tissue than healthy peer. This finding is not surprising as many studies have reported that miRNA-155 and miRNA-146a are endotoxin-responsive genes [31, 56, 57]. Peri-implantitis is caused by bacterial biofilm accumulated onto implant surfaces. Bacterial components from the accumulated biofilm such as lipopolysaccharides could induce over-expression of these miRNAs in the affected tissues [56, 57]. TLR-4 on inflammatory cells could recognize bacterial components and thereby trigger the high expression of miRNA-146a within tissues [31]. With time during inflammation, miRNA-146a has been reported to be persist in high levels and acts as a key negative regulator of the immune response. MiRNA-146a represses IL-1 receptor-associated kinase 1 and TNF receptor-associated factor 6 protein mRNAs and thus controlling TLR induced proinflammatory cytokine signaling [31]. On the other hand, limited amount of bacterial accumulation is associated with healthy peri-implant tissue [58].Therefore, no induction for miRNAs overproduction is assumed.
In literature, the expression of miR-155 and miR146a have been extensively studied in periodontitis, dissimilar to peri-implantitis, affected tissue [29, 33,34,35]. It is worth to mention that this is the first study investigating the level of miRNA-155 in peri-implantitis. While, there is only one animal study which assessed the level of miRNA 146a in ligature-induced peri-implantitis among canine dogs [14]. This study has reported a contrary outcome as the previous study found that miRNA-146a was down-regulated in peri-implantitis. However, the present study assessed the level of miRNAs in human, not animal, tissue which might not necessarily exhibit the same molecular events occurring during the process of peri-implantitis lesion in animals. Moreover, peri-implantitis lesion was induced in the previous animal study, whereas this study involved volunteers already having peri-implantitis. Furthermore, the previous study used a split-mouth design, while this study investigated sample distributed in parallel groups with possibly less controlling of inter-group confounders. Thus, these, above-mentioned, differences in studied samples might explain the inconsistence in the findings. Therefore, more studies are highly suggested to resolve this disagreement regarding this finding.
MiRNA-155 is an important regulator of TLR-related disorders. The stimulation of cells with bacterial LPS increased the expression of miRNA-155, which worked on NF-B via negative feedback, regulating the release of numerous cytokines and influencing the inflammatory response [31, 59]. Because both miRNA-155 and miRNA-146a have a role in LPS-induced macrophage activation, these variables are frequently examined together. Their expression profiles, however, differed in various tissues. In periodontitis patients, for example, miRNA-146a was found to be overexpressed in inflammatory gingival tissue, while miRNA-155 was downregulated in some reports [34, 60] and upregulated in others [29, 33]. However, it has been reported that the expression of miRNA-155 and miRNA-146a in the GCF of patients with periodontitis was upregulated [33]. No doubt, miRNA-146a and miRNA-155 function in a two-tiered manner. During the initiation of inflammation, miRNA-146a is activated in response to low LPS doses, while miRNA-155 is gradually elevated to full expression and acts as a limiter of proinflammatory gene expression once the miRNA-146a-dependent anti-inflammatory impact is lost [33, 61].
Both miRNA-155 and miRNA-146a expressions showed a considerable discriminating efficacy to differentiate peri-implantitis affected from healthy tissues with accepted levels of sensitivity and specificity. For the diagnosis of periodontitis, similar findings have been reported that the level of both miRNA-146a and miRNA-155 could differentiate between healthy and periodontitis patients with high accuracy based on ROC curves analysis [33]. This, in turn, highlights the possibility of using these miRNAs as potential biomarkers to predict peri-implantitis. MiRNA-146 and miRNA-155 are vital in controlling the immune response and inflammation associated with periodontal disease. Their consistent presence in bodily fluids makes them very promising as diagnostic biomarkers [62]. At the same time, their ability to regulate biological processes presents prospective opportunities for targeting and controlling peri-implantitis and enhancing periodontal health. More research is required to convert these discoveries into practical uses in the medical field, specifically establishing uniform diagnostic standards and improving the methods of administering miRNA-based treatments [35]. In fact, it is not reasonable to use the expression of these miRNAs in tissue for the diagnosis of peri-implant disease. More clinically relevant, it is suggested that the levels of these biomarker in peri-implant gingival fluid might have the same discriminating efficacy. To approve this suggestion, future studies are highly suggested.
The present study showed nonsignificant association between miRNA-146a and mi-RNA-155 levels with bone loss and pocket depth. This might reflect the roles of these miRNAs in regulating the immunological response or maintaining immunological hemostasis in peri-implantitis disease.
As a limitation in this study, plaque index was not recorded. However, BOP was recorded in both groups which provided more objective indicator for the health status of peri-implant tissue. Moreover, it was better to use a split-mouth design in this study. This design provides better control of unexpected inter-group confounding factors. However, strict inclusion and exclusion criteria were used in this study in order to minimize the effects of unexpected inter-group confounders. Furthermore, the unrevealed association between the miRNAs expression and clinical parameters might be attributed to the small sample size considered in this study. However, the sample size was estimated to detect the difference of miRNA-155 expression (as the primary outcome) between the study groups. Future studies with larger sample size are suggested to resolve this issue.
Conclusion
This study demonstrates that the expressions of miRNA-146a and miRNA-155 are different between healthy and peri-implantitis affected tissues. Both miRNAs might potentially able to discriminate the healthy from peri-implantitis affected tissues. Further studies are suggested to investigate the role of these miRNAs within the course of peri-implant tissue inflammation.
Data availability
The datasets supporting the conclusions of this article are included within the article and its additional files.
Abbreviations
- (miRNAs):
-
microRNAs
- (TLRs):
-
Toll-like receptors
- (PPD):
-
probing pocket depth
- (BOP):
-
bleeding on probing
- (qPCR):
-
polymerase chain reaction
References
Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM, Chen S, Cochran D, Derks J, Figuero E. Peri‐implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World workshop on the classification of Periodontal and Peri‐Implant diseases and conditions. J Periodontol. 2018;89:S313–8.
SChWaRZ F, Derks J. monJe a, WanG hl: Peri-implantitis. J Clin Periodontol 2018.
Diaz P, Gonzalo E, Villagra LJG, Miegimolle B, Suarez MJ. What is the prevalence of peri-implantitis? A systematic review and meta-analysis. BMC Oral Health. 2022;22(1):449.
Herrera D, Berglundh T, Schwarz F, Chapple I, Jepsen S, Sculean A, Kebschull M, Papapanou PN, Tonetti MS, Sanz M. Prevention and treatment of peri-implant diseases—the EFP S3 level clinical practice guideline. J Clin Periodontol 2023.
Cha JK, Lee JS, Kim CS. Surgical Therapy of Peri-implantitis with local minocycline: a 6-Month Randomized Controlled Clinical Trial. J Dent Res. 2019;98(3):288–95.
dos Santos Martins BG, Hasse Fernandes JC, Gomes Martins A, de Moraes Castilho R, de Oliveira Fernandes GV. Surgical and Nonsurgical Treatment protocols for Peri-implantitis: an overview of systematic reviews. Int J Oral Maxillofacial Implants 2022, 37(4).
Atarchi AR, Miley DD, Omran MT, Abdulkareem AA. Early failure rate and Associated Risk factors for Dental implants placed with and without Maxillary Sinus Augmentation: a retrospective study. Int J Oral Maxillofacial Implants 2020, 35(6).
Rakic M, Monje A, Radovanovic S, Petkovic-Curcin A, Vojvodic D, Tatic Z. Is the personalized approach the key to improve clinical diagnosis of Peri‐implant conditions? The role of bone markers. J Periodontol. 2020;91(7):859–69.
Menini M, Dellepiane E, Baldi D, Longobardi M, Pera P, Izzotti A. Microarray expression in peri-implant tissue next to different titanium implant surfaces predicts clinical outcomes: a split‐mouth study. Clin Oral Implants Res. 2017;28(9):e121–34.
Chaparro A, Atria P, Realini O, Monteiro LJ, Betancur D, Acuña-Gallardo S, Ramírez V, Bendek MJ, Pascual A, Nart J. Diagnostic potential of Peri‐implant crevicular fluid microRNA‐21‐3p and microRNA‐150‐5p and extracellular vesicles in Peri‐implant diseases. J Periodontol. 2021;92(6):e11–21.
Belibasakis GN. Microbiological and immuno-pathological aspects of peri-implant diseases. Arch Oral Biol. 2014;59(1):66–72.
Carcuac O, Berglundh T. Composition of human peri-implantitis and periodontitis lesions. J Dent Res. 2014;93(11):1083–8.
Alqutaibi AY, Aljohani A, Alduri A, Masoudi A, Alsaedi AM, Al-Sharani HM, Farghal AE, Alnazzawi AA, Aboalrejal AN, Mohamed A-AH. The effectiveness of Cold Atmospheric plasma (CAP) on bacterial reduction in Dental implants: a systematic review. Biomolecules. 2023;13(10):1528.
Wu X, Chen X, Mi W, Wu T, Gu Q, Huang H. MicroRNA sequence analysis identifies microRNAs associated with peri-implantitis in dogs. Biosci Rep. 2017;37(5):BSR20170768.
Öksüz Z, Gragnani L, Lorini S, Temel GÖ, Serin MS, Zignego AL. Evaluation of plasma miR-17-5p, mir-24-3p and miRNA-223-3p Profile of Hepatitis C virus-infected patients after treatment with Direct-Acting Antivirals. J Personalized Med. 2023;13(8):1188.
Lauria G, Curcio R, Tucci P. A Machine Learning Approach for highlighting microRNAs as biomarkers linked to amyotrophic lateral sclerosis diagnosis and progression. Biomolecules. 2023;14(1):47.
Abdulkareem A, Abdulbaqi H, Gul S, Milward M, Chasib N, Alhashimi R. Classic vs. Novel antibacterial approaches for eradicating dental biofilm as adjunct to periodontal debridement: an evidence-based overview. Antibiotics. 2021;11(1):9.
Daily ZA, Al-Ghurabei BH, Al-Qarakhli AMA, Moseley R. MicroRNA-155 (miR-155) as an accurate biomarker of periodontal status and coronary heart disease severity: a case–control study. BMC Oral Health. 2023;23(1):868.
Ibrahem DN, Mahmood MS, BIOLOGICAL THERAPY FOR PATIENTS WITH RHEUMATOID ARTHRITIS AND ITS EFFECT ON PERIODONTAL AND IMMUNOLOGICAL PARAMETERS. Biochem Cell Archives 2021, 21(1).
Al-Juboori SKE, Al-Juboori SI. Hepatocellular Carcinoma Prediction and early diagnosis of Hepatitis B and C viral infection using miR-122 and miR-223 in a sample of Iraqi patients. Baghdad Sci J. 2023;20(4):1520–1520.
Mudhir SH, Al-Jubouri RH, Majeed BAA. The validity of salivary microRNAs (hsa-miR-200a, hsa-miR-125a and hsa-miR-93) as oral squamous cell carcinoma biomarker. J Baghdad Coll Dentistry. 2014;26(3):66–71.
Edan WH, El-Samarrai SK. Significance of salivary miRNA 21 determined by Real Time PCR in patients with squamous cell carcinoma. J Baghdad Coll Dentistry. 2016;28(3):178–80.
Al-Heety RA, Al-Hadithi HS. Association of circulating MicroRNA-142-3p with Graves Disease. Baghdad Sci J. 2021;18(4):1133–1133.
Ferro A, Saccu G, Mattivi S, Gaido A, Herrera Sanchez MB, Haque S, Silengo L, Altruda F, Durazzo M, Fagoonee S. Extracellular vesicles as Delivery vehicles for non-coding RNAs: potential biomarkers for Chronic Liver diseases. Biomolecules. 2024;14(3):277.
Raheem AR, Abdul-Rasheed OF, Khattab OS, Alsammarraie AZ, Al-Aubaidy H, Abid HA. Circulating miRNA-373 and vascular endothelial growth factor as potential biomarkers for early detection of breast Cancer. Indian J Clin Biochem 2024:1–10.
Pagoni M, Cava C, Sideris DC, Avgeris M, Zoumpourlis V, Michalopoulos I, Drakoulis N. miRNA-based technologies in cancer therapy. J Personalized Med. 2023;13(11):1586.
Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. cell 2004, 116(2):281–297.
He L, Hannon GJ. MicroRNAs: small RNAs with a big role in gene regulation. Nat Rev Genet. 2004;5(7):522–31.
Stoecklin-Wasmer C, Guarnieri P, Celenti R, Demmer R, Kebschull M, Papapanou P. MicroRNAs and their target genes in gingival tissues. J Dent Res. 2012;91(10):934–40.
AL-saqabi ANI, Aziz IH. The expression miRNA-195 in a sample of Iraqi breast cancer pa-tients.
Taganov KD, Boldin MP, Chang K-J, Baltimore D. NF-κB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proc Natl Acad Sci. 2006;103(33):12481–6.
Abdulkareem AA, Abdulbaqi HR, Nayyef AK, Saliem SS. Differential expression of toll-like receptor 4 and nuclear factor κB of primary rat oral keratinocytes in response to Stimulation with Fusobacterium nucleatum. World J Dentistry. 2009;9(4):270–4.
Radović N, Nikolić Jakoba N, Petrović N, Milosavljević A, Brković B, Roganović J. Micro RNA-146a and micro RNA‐155 as novel crevicular fluid biomarkers for periodontitis in non‐diabetic and type 2 diabetic patients. J Clin Periodontol. 2018;45(6):663–71.
Xie Y-f, Shu R, Jiang S-y, Liu D-l, Zhang X. Comparison of microRNA profiles of human periodontal diseased and healthy gingival tissues. Int J Oral Sci. 2011;3(3):125–34.
Asa’ad F, Garaicoa-Pazmiño C, Dahlin C, Larsson L. Expression of microRNAs in periodontal and peri-implant diseases: a systematic review and meta-analysis. Int J Mol Sci. 2020;21(11):4147.
Nisha K, Janam P, Harshakumar K. Identification of a novel salivary biomarker mir-143‐3p for periodontal diagnosis: a proof of concept study. J Periodontol. 2019;90(10):1149–59.
Genova T, Chinigò G, Munaron L, Rivolo P, Luganini A, Gribaudo G, Cavagnetto D, Mandracci P, Mussano F. Bacterial and Cellular Response to Yellow-shaded surface modifications for Dental Implant abutments. Biomolecules. 2022;12(11):1718.
Gul SS, Abdulkareem AA, Sha AM, Rawlinson A. Diagnostic accuracy of oral fluids biomarker profile to determine the current and future status of periodontal and peri-implant diseases. Diagnostics. 2020;10(10):838.
Heitz-Mayfield LJA, Lang NP. Comparative biology of chronic and aggressive periodontitis vs. peri-implantitis. Periodontol 2000. 2010;53:167–81.
Figueiredo LC, Bueno-Silva B, Nogueira CFP, Valadares LC, Garcia KMM, Filho GCL, Milanello L, Esteves FM, Shibli JA, Miranda TS. Levels of Gene expression of immunological biomarkers in Peri-implant and Periodontal tissues. Int J Environ Res Public Health. 2020;17(23):9100.
Adibrad M, Shahabuei M, Sahabi M. Significance of the width of keratinized mucosa on the health status of the supporting tissue around implants supporting overdentures. J Oral Implantology. 2009;35(5):232–7.
Calvo-Guirado JL, López‐López PJ, Pérez‐Albacete Martínez C, Javed F, Granero‐Marín JM. Maté Sánchez De Val JE, Ramirez Fernandez MP: Peri‐implant bone loss clinical and radiographic evaluation around rough neck and microthread implants: a 5‐year study. Clin Oral Implants Res. 2018;29(6):635–43.
Isler SC, Uraz A, Kaymaz O, Cetiner D. An evaluation of the relationship between peri-implant soft tissue biotype and the severity of peri-implantitis: a cross-sectional study. Nternational J Oral Maxillofacial Implants. 2019;34(1):187–96.
Padhye NM, Mehta LK, Yadav N. Buccally displaced flap versus sub-epithelial connective tissue graft for peri-implant soft tissue augmentation: a pilot double-blind randomized controlled trial. Int J Implant Dentistry. 2020;6:1–7.
Ghinassi B, Di Baldassarre A, D’Addazio G, Traini T, Andrisani M, Di Vincenzo G, Gaggi G, Piattelli M, Caputi S, Sinjari B. Gingival response to dental implant: comparison study on the effects of new nanopored laser-treated vs. traditional healing abutments. Int J Mol Sci. 2020;21(17):6056.
Canullo L, Penarrocha Oltra D, Pesce P, Zarauz C, Lattanzio R, Penarrocha Diago M, Iezzi G. Soft tissue integration of different abutment surfaces: an experimental study with histological analysis. Clin Oral Implants Res. 2021;32(8):928–40.
Gualini F, Berglundh T. Immunohistochemical characteristics of inflammatory lesions at implants. J Clin Periodontol. 2003;30(1):14–8.
Yadav A, Ramasamy TS, Lin S-C, Chen S-H, Lu J, Liu Y-H, Lu F-I, Hsueh Y-Y, Lin S-P, Wu C-C. Autologous platelet-rich growth factor reduces M1 macrophages and modulates inflammatory microenvironments to promote sciatic nerve regeneration. Biomedicines. 2022;10(8):1991.
Rao X, Huang X, Zhou Z, Lin X. An improvement of the 2ˆ (–delta delta CT) method for quantitative real-time polymerase chain reaction data analysis. Biostatistics Bioinf Biomathematics. 2013;3(3):71.
Shrivastava S, Steele R, Ray R, Ray RB. MicroRNAs: role in hepatitis C virus pathogenesis. Genes Dis. 2015;2(1):35–45.
Ebert MS, Sharp PA. Roles for microRNAs in conferring robustness to biological processes. cell 2012, 149(3):515–524.
Albandar JM. Aggressive periodontitis: case definition and diagnostic criteria. Periodontol 2000. 2014;65(1):13–26.
Vahabi S, Sattari M, Taheraslani M, Bagheban AA. Correlation between interleukin-1β, interleukin-6 and tumor necrosis factor-α and clinical parameters in chronic and aggressive periodontal disease. J Adv Periodontology Implant Dentistry. 2011;3(2):51–6.
Noh MK, Jung M, Kim SH, Lee SR, Park KH, Kim DH, Kim HH, Park YG. Assessment of IL–6, IL–8 and TNF–α levels in the gingival tissue of patients with periodontitis. Experimental Therapeutic Med. 2013;6(3):847–51.
Livak KJ. TD Schmittgen 2001 Analysis of relative gene expression data using real-time quantitative PCR and the 2 – ∆∆CT method. Methods 25 4 402–8.
Nahid MA, Pauley KM, Satoh M, Chan EK. miR-146a is critical for endotoxin-induced tolerance. J Biol Chem. 2009;284(50):34590–9.
Nahid MA, Rivera M, Lucas A, Chan EK, Kesavalu L. Polymicrobial infection with periodontal pathogens specifically enhances microRNA miR-146a in ApoE–/– mice during experimental periodontal disease. Infect Immun. 2011;79(4):1597–605.
Souza AB, Tormena M, Matarazzo F, Araújo MG. The influence of peri-implant keratinized mucosa on brushing discomfort and peri‐implant tissue health. Clin Oral Implants Res. 2016;27(6):650–5.
Ma X, Becker Buscaglia LE, Barker JR, Li Y. MicroRNAs in NF-κB signaling. J Mol Cell Biol. 2011;3(3):159–66.
Xie Yf, Shu R, Jiang Sy L, Dl Z, Xl. Comparison of microRNA profiles of human periodontal diseased and healthy gingival tissues. Int J Oral Sci. 2011;3(3):125–34.
Yuan Y, Zhang H, Huang H. microRNAs in inflammatory alveolar bone defect: a review. J Periodontal Res. 2021;56(2):219–25.
Kagiya T. MicroRNAs: potential biomarkers and therapeutic targets for alveolar bone loss in periodontal disease. Int J Mol Sci. 2016;17(8):1317.
Acknowledgements
The authors would like to acknowledge Dr. AM AL-Anee, Collage of Dentistry, University of Baghdad for his assistance in surgical procedures. Also, the authors express their appreciations to Al-Rafiden dental clinics and Al-Ghadeer training center, Baghdad, Iraq for their technical support.
Funding
This study is self-funded.
Author information
Authors and Affiliations
Contributions
Conceptualization, H.A.; methodology, M.H. and H.A.; software, M.H.; validation, M.H. and H.A.; formal analysis, M.H. and H.A.; investigation, M.H.; resources, M.H.; data curation, M.H. and H.A.; writing—original draft preparation, M.H.; writing—review and editing, H.A.; visualization, M.H. and H.A.; supervision, H.A.; project administration, M.H. and H.A.; funding acquisition, M.H.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study protocol (including all methods used) was reviewed and approved by the ethical committee of the College of Dentistry / University of Baghdad in April 2022 (project No.#534622) in accordance with the ethical guidelines of the Declaration of Helsinki and its revisions for human research. Signed informed consent forms were collected from all patients who participated in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hamed, M.N., Abdulbaqi, H.R. Expression of miRNAs (146a and 155) in human peri-implant tissue affected by peri-implantitis: a case control study. BMC Oral Health 24, 856 (2024). https://doi.org/10.1186/s12903-024-04579-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04579-x